Abstract
Background
Preventing and/or delaying cognitive impairment is a public health priority. To increase awareness of and participation in behaviors that may help maintain cognitive function or reduce risk of impairment, we need to understand public perceptions about risk and protective factors.
Methods
We conducted a scoping review of studies examining the public’s perceptions about risk and protective factors related to cognitive health and impairment published since the 2007 National Public Health Road Map to Maintaining Cognitive Health.
Results
A search of five databases yielded 1,115 documents published between June 2007 and December 2013. Initial review of abstracts identified 90 potentially eligible studies. After full-article review, 30 met inclusion criteria; four additional articles identified in reference lists also met inclusion criteria. Of the 34, 16 studies addressed Alzheimer’s disease (AD) specifically, 15 dementia broadly, 5 mild to moderate cognitive impairment, and 8 normal functioning, with some content overlap. Across studies, respondents reported genetics (n = 14 studies), older age (n = 8), stress (n = 7), brain/head injury (n = 6), and mental illness/brain disease (n = 6) as perceived risk factors for AD and dementia. Protective factors most commonly identified for maintaining cognitive health were intellectual/mental stimulation (n = 13), physical activity (n = 12), healthy diet (n = 10), and social/leisure activities (n = 10).
Conclusions
Studies identified genetics and older age as key perceived risk factors more so than behaviors such as smoking. Individuals perceived that numerous lifestyle factors (e.g. intellectual stimulation, physical activity) could protect against cognitive impairment, AD, and/or dementia. Results can inform national and international education efforts about AD and other dementias.
Keywords: cognition, Alzheimer’s disease, dementia, scoping review, public perceptions, risk factors, protective factors
Introduction
Cognitive status in older adulthood can range from optimal cognition to mild impairment to dementia including AD (Department of Health and Human Services, 2010). Hebert et al. (2013) estimated the prevalence of AD in the US in 2010 to be 4.7 million people, and projected that this number would triple to 13.8 million by 2050, with 7 million of those aged 85 years or older.
By 2050, the total annual cost for dementia care is projected to be $1.2 trillion, including a six-fold increase in government spending (Alzheimer’s Association, 2014). Dementia care also exacts a tremendous emotional and physical toll on informal, unpaid caregivers (Ivey et al., 2013). Associated healthcare costs for caregivers are estimated at approximately $9.3 billion (Alzheimer’s Association, 2014).
Due to their tremendous human and financial burden, cognitive impairment, AD, and other dementias have reached the forefront of the public health agenda (Albert et al., 2007; Anderson and McConnell, 2007a; 2007b; Department of Health and Human Services, 2010; Centers for Disease Control and Prevention, 2011; Department of Health and Human Services, 2012; Alzheimer’s Association and Centers for Disease Control and Prevention, 2013; Alzheimer’s Disease International, 2014). In June 2007, the Centers for Disease Control and Prevention (CDC) and the Alzheimer’s Association published The Healthy Brain Initiative: A National Public Health Road Map to Maintaining Cognitive Health as the first call to action and coordinated approach to move cognitive health promotion into public health practice (Alzheimer’s Association and Centers for Disease Control and Prevention, 2007). The definition of cognitive health from the National Institutes of Health Cognitive and Emotional Health Project, which influenced the formation of The Healthy Brain Initiative, is used in this review:
“cognitive health as it pertains to the older adult should be defined not just as the absence of disease, but rather as the development and preservation of the multidimensional cognitive structure that allows the older adult to maintain social connectedness, an ongoing sense of purpose, and the abilities to function independently, to permit functional recovery from illness or injury, and to cope with residual functional deficits” (Hendrie et al., 2006, p. 13).
In 2013, the Alzheimer’s Association and CDC released the Road Map, The Healthy Brain Initiative: The Public Health Road Map for State and National Partnerships, 2013–2018 (Alzheimer’s Association and Centers for Disease Control and Prevention, 2013), outlining 35 specific actions within four public health domains designed to help state and local agencies and their partners employ effective public health practices relating to cognitive health and impairment. Two domains relevant to this review are: Monitor and Evaluate – actions that encourage “national organizations and agencies to develop standardized questions that can be used at the national, state, and local levels to track awareness and perceptions about cognitive health and impairment, including decline in cognitive functioning,” and Educate and Empower – actions that “identify and promote culturally appropriate strategies designed to increase public awareness about dementia, including Alzheimer’s disease, to reduce conflicting messages, decrease stigma, and promote early diagnosis.” This review paper will inform the 2013 Road Map’s call to actions by identifying and synthesizing the current literature regarding the public’s perceptions about protective factors related to cognitive health and risk factors related to cognitive impairment, AD, and other dementias.
Methods
A scoping review “provides a preliminary assessment of the potential size and scope of available research literature. It aims to identify the nature and extent of research evidence (usually including ongoing research)” (Grant and Booth, 2009, p. 31). Scoping reviews are conducted for various purposes (e.g. to examine the extent of research activity, to determine the need for a systematic review) (Arksey and O’Malley, 2005); the current review was undertaken to summarize and disseminate knowledge about public perceptions of risk and protective factors associated with cognitive health and impairment. The scoping methodology of Arksey and O’Malley (2005) was applied, incorporating modifications of Levac and colleagues (2010).
Search strategy
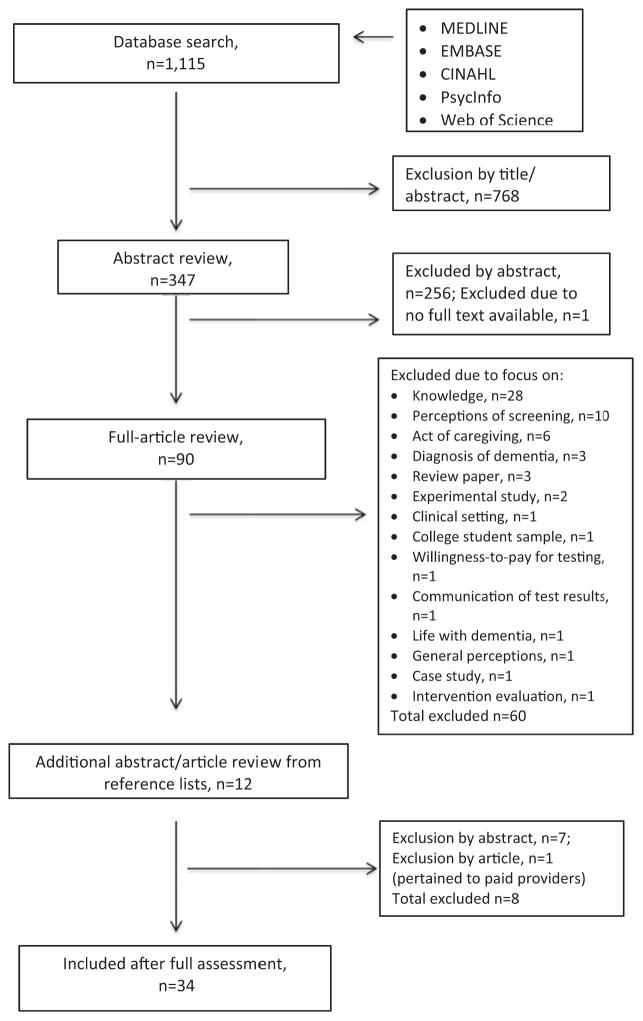
A librarian trained in conducting systematic reviews performed the search. The online database search of MEDLINE, EMBASE, CINAHL, PsycInfo, and Web of Science included search specifications and text searches specific to each journal but generally involved the following terms: cognition disorders OR dementia OR Alzheimer disease OR memory disorders in combination with: attitude OR attitude to health OR health knowledge, attitudes, practice. The terms cognition OR cognitive OR dementia OR Alzheimer were also combined with attitude OR belief OR perception OR knowledge. The process included three interrelated steps (See Figure 1): abstract reviews, full-article reviews, and reviewers’ examination of reference lists from full articles to identify articles for possible inclusion.
Figure 1.
Flowchart of scoping review process.
Inclusion and exclusion criteria
Inclusion criteria required an empirical research study involving adults residing in the community and published in English between June 1, 2007 and December 31, 2013. Studies had to provide qualitative or quantitative data on perceptions of risk and/or protective factors related to cognitive functioning. The initial review date in 2007 was selected to reflect the inclusion of studies prior to that date in preparation of the 2007 Road Map. Because this review was designed to further understand the perceptions of the general adult population, we excluded articles focused only on the perceptions of children, college students, and healthcare providers and trainees.
Data extraction and synthesis
Twelve research team members (including the 11 authors) reviewed and abstracted information from 90 full articles (the full article from one abstract could not be located), posting their reviews to an online abstraction tool developed and pilot tested by the team using six model articles. The final online tool contained 20 questions, 5 of which were open ended (available upon request). After the initial full-article abstraction, articles were re-distributed for a secondary review by a different co-author as a quality check. Two authors (DF, KB) arbitrated any disagreements among reviewers and made final decisions. Article reference lists were also reviewed for potentially relevant articles. All data abstracted from the articles were summarized into a Microsoft Excel spreadsheet.
Results
Selection of studies
After the two-round full-article review process, 60 of the 90 articles were excluded (28 pertained only to knowledge regarding cognition or dementia, 10 to cognitive screening, 6 to the act of caregiving, and 3 to the diagnosis of dementia; 3 were review papers, 2 experimental studies, and 8 were excluded due to other exclusion criteria). During full-article reviews, we identified 12 additional potentially relevant abstracts from article reference lists. Two of the authors (DF, KB) reviewed these abstracts and excluded 7 of the 12. Two other co-authors (LB, SB) reviewed the 5 full-text articles using the online tool and excluded 1 (pertained to perceptions of paid providers of care). Thus, based on this extensive review process, a total of 34 articles were determined to fit inclusion criteria for this scoping review because they examined the public’s perceptions about protective factors related to cognitive health and risk factors related to cognitive impairment, AD, and other dementias.
Overview of studies
Included studies were conducted in 8 countries (22 United States, 4 Australia, 3 United Kingdom, 1 Brazil, 1 Germany, 1 Ireland, 1 Italy, and 1 South Korea). Of the 34 studies, sample sizes ranged from 9 (in-depth interviews) to 4,728 (national survey) individuals. Most studies included men and women. One study of caregivers included only women (Gray et al., 2009); one study included all male clergy (Stansbury et al., 2010a; 2010b); and one study did not report participant gender (Beard et al., 2009). An equal number of studies (n = 17 each) assessed perceptions of the general public aged 18 years or older and of adults over the age of 50 years.
Studies focused on AD (n = 16), dementia broadly (n = 15), mild to moderate cognitive impairment (n = 5), and/or normal cognitive functioning (n = 8). Most studies were quantitative based on written surveys or online questionnaires based on investigator-developed tools or questions adapted from published measures (n = 22). Qualitative studies involved focus groups and/or interviews and used open-ended questions and probing techniques to examine participants’ perceptions regarding risk and protective factors (n = 12).
The specific risk and protective factors investigated in this set of studies and identified by study participants are presented in Tables 1 and 2. Studies examining risk factors related to cognitive impairment are summarized in Table 1. Genetics/heredity (n = 14 studies) and older age (n = 8) were the most consistently cited risk factors among study respondents. Additionally, participants also identified risk factors such as stress, mental illness, brain/head injury in 6 or more studies. Studies examining protective factors related to cognitive health are summarized in Table 2. Protective factors most commonly reported as maintaining cognitive health were intellectual stimulation/mental activity (n = 13), physical activity (n = 12), healthy diet (n = 10), and social/leisure activities (n = 10). In studies published between 2008 and 2011, few lifestyle factors were cited as protective against AD and/or dementia. A more recent study demonstrated that adults from the general population perceived that numerous factors could potentially protect people from AD and dementia (Friedman et al., 2013). Key study findings are described in the following sections.
Table 1.
Cognitive impairment risk factors commonly investigated across studies and study participants’ perceptions about risk factors* (n = 18 studies)
| FIRST AUTHOR AND YEAR |
GENETICS/ HEREDITY |
OLDER AGE |
STRESS
|
BRAIN/ HEAD INJURY |
MENTAL ILLNESS/ DISEASE |
LONELINESS/ ISOLATION |
POOR DIET |
OTHER DISEASES |
ALCOHOL/ SMOKING |
PERSONALITY/ ATTITUDE |
“GOD’S WILL” (NO CURE) |
MENTAL INACTIVITY |
PHYSICAL INACTIVITY |
STROKE
|
ENVTL. TOXINS |
HYPER- TENSION |
ILLICIT DRUG USE |
|||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| I* | A* | I | A | I | A | I | A | I | A | I | A | I | A | I | A | I | A | I | A | I | A | I | A | I | A | I | A | I | A | I | A | I | A | |
| Moscarillo et al., 2007† | + | + | ||||||||||||||||||||||||||||||||
| Sullivan et al., 2007 | + | + | + | - | ||||||||||||||||||||||||||||||
| Yeo et al., 2007 | + | + | + | - | + | + | + | - | + | - | + | - | + | + | ||||||||||||||||||||
| Blay and Piza Peluso Ede, 2008 | + | − | + | − | + | − | + | + | + | + | + | − | + | − | + | + | ||||||||||||||||||
| Otilingam and Gatz, 2008 | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | − | + | − | ||||||||||||||||
| Park et al., 2008 | + | − | + | + | + | + | − | + | − | + | − | |||||||||||||||||||||||
| Beard et al., 2009‡ | + | |||||||||||||||||||||||||||||||||
| Connell et al., 2009 | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | ||||||||||||||||||
| Low and Anstey, 2009 | + | + | + | + | + | − | + | + | + | + | − | + | − | + | + | + | − | |||||||||||||||||
| Wu et al., 2009‡ | + | + | + | |||||||||||||||||||||||||||||||
| Lee et al., 2010 | + | + | − | + | + | + | + | − | + | + | + | + | + | + | + | − | ||||||||||||||||||
| Stansbury et al., 2010a‡ | + | + | + | + | ||||||||||||||||||||||||||||||
| Stansbury et al., 2010b‡ | + | + | + | + | + | |||||||||||||||||||||||||||||
| Anderson et al., 2011 | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | ||||||||||||||||
| Low et al., 2011 | + | − | + | + | + | + | + | + | + | + | + | − | + | + | + | − | + | − | + | − | ||||||||||||||
| Riva et al., 2012 | + | + | + | − | ||||||||||||||||||||||||||||||
| Ayalon 2013 | + | + | + | + | ||||||||||||||||||||||||||||||
| Laditka et al., 2013‡ | + | + | + | + | + | |||||||||||||||||||||||||||||
| Number of Studies | 12 | 14 | 5 | 8 | 8 | 7 | 7 | 6 | 7 | 6 | 3 | 5 | 5 | 4 | 3 | 4 | 5 | 3 | 5 | 3 | 2 | 2 | 3 | 2 | 4 | 2 | 3 | 2 | 4 | 1 | 1 | 1 | 1 | 1 |
+/+ = Factor investigated in study and agreed upon or identified by participants.
+/− = Factor investigated in study but not agreed upon or identified by participants.
/+ = Factor identified by participants in qualitative (inductive) study.
Factors categorized as “Agreed upon/Identified” may not have been cited by all subgroups within a single study.
One risk factor was examined on survey; inductive, qualitative analysis was conducted for the focus group component of study.
Participants were not asked to select factors from a list; inductive, qualitative analysis.
Table 2.
Cognitive health protective factors commonly investigated across studies and study participants’ perceptions about protective factors (n = 17 studies)
| FIRST AUTHOR AND YEAR |
INTELLECTUAL STIMULATION/ MENTAL ACTIVITY |
PHYSICAL ACTIVITY |
HEALTHY DIET |
SOCIAL/ LEISURE ACTIVITIES |
LIMIT ALCOHOL |
PRESCRIPTION MEDICATION/ MEDICAL INTERVENTION |
VITAMINS/ SUPPLEMENTS |
HEALTHY WEIGHT |
LIMIT STRESS |
POSITIVE ATTITUDE |
AVOID ILLICIT DRUGS |
AVOID SMOKING |
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| I* | A* | I | A | I | A | I | A | I | A | I | A | I | A | I | A | I | A | I | A | I | A | I | A | |
| Low et al., 2007 | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | |||||||||
| McIlvane et al., 2008 | + | + | + | + | + | − | + | − | + | − | + | − | + | + | ||||||||||
| Yeo et al., 2007† | + | − | + | − | ||||||||||||||||||||
| Beard et al., 2009‡ | + | + | + | + | ||||||||||||||||||||
| Connell et al., 2009 | + | + | + | + | + | + | + | − | + | − | + | + | ||||||||||||
| Gray et al., 2009 | + | − | + | − | + | − | + | + | + | − | ||||||||||||||
| Laditka et al., 2009‡ | + | + | ||||||||||||||||||||||
| Low et al., 2009 | + | + | + | + | + | + | + | + | + | − | + | − | + | − | + | − | + | − | + | − | ||||
| Wilcox et al., 2009§ | + | + | + | + | ||||||||||||||||||||
| Wu et al., 2009‡ | + | + | + | + | + | |||||||||||||||||||
| Anderson et al., 2011 | + | + | + | + | ||||||||||||||||||||
| Friedman et al., 2011§ | + | + | + | + | + | + | ||||||||||||||||||
| Price et al., 2011§ | + | + | ||||||||||||||||||||||
| Laditka et al., 2012‡ | + | + | + | + | + | + | + | |||||||||||||||||
| Luck et al., 2012 | + | + | + | + | + | + | + | + | + | |||||||||||||||
| Ayalon 2013 | + | + | + | + | + | + | + | + | ||||||||||||||||
| Friedman et al., 2013 | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | − | ||||||
| Number of Studies | 10 | 13 | 11 | 12 | 8 | 10 | 6 | 10 | 3 | 4 | 6 | 3 | 8 | 3 | 1 | 2 | 4 | 2 | 2 | 2 | 1 | 1 | 2 | 1 |
+/+ = Factor investigated and agreed upon or identified by participants.
+/− = Factor investigated but not agreed upon or identified by participants.
/+ = Factor identified by participants in qualitative (inductive) study.
Factors categorized as ‘Agreed upon/Identified’ may not have been cited by all subgroups within a single study.
Protective factors examined in study; numeric perception results not presented.
Participants were not asked to select factors from a list; inductive, qualitative analysis.
Qualitative study, however, analysis focused on perceptions about specific factors.
Perceptions of diverse older adults and cross-cultural studies
A subset of articles included in this review (n = 8) reported results from the “Healthy Brain Study,” a multi-state US focus group study that examined ethnically (African American, white, American Indian, Chinese American, Vietnamese American, and Latino) and geographically (rural and urban) diverse groups’ perceptions about cognitive health. Older participants (n = 396) attributed memory loss to stress, chronic diseases (e.g. diabetes, stroke), head injury, and genetics (Laditka et al., 2013). Specifically among rural older adults in a separate analysis, 67 participants identified chronic diseases, additives and processed foods, and genetics as causes of memory loss by both men and women; women also identified stress as a potential risk factor (Wu et al., 2009). Regarding strategies for reducing the risk of cognitive decline, older men and women agreed that mental stimulation (e.g. reading and puzzles) (Laditka et al., 2009; Wu et al., 2009; Friedman et al., 2011), positive attitude (Wu et al., 2009, Friedman et al., 2011), social interaction (Laditka et al., 2009; Wu et al., 2009; Friedman et al., 2011), and healthy diet (Wu et al., 2009) were important. An analysis by gender revealed that women also noted social involvement and structured leisure activities, including group exercise, as protective factors (Wu et al., 2009). Friedman et al. (2011) found that African Americans and whites more commonly suggested that mental activities (e.g. puzzles) were useful compared with other racial/ethnic groups.
In a qualitative analysis from this larger “Healthy Brain Study” that focused specifically on perceptions of adults aged 55 years or older regarding the link between physical activity and cognitive health, some participants indicated they were aware of the association, others were not, and still others were skeptical of the relationship (Price et al., 2011). Participants provided a wide range of frequency and duration recommendations for physical activity, but most commonly suggested 30 minutes of physical activity between 3 and 7 days per week (Price et al., 2011). In an analysis of physical activity and cognition perceptions by racial/ethnic group, participants (n = 396) from all groups (i.e. white, Chinese, Vietnamese, Hispanic, African American, and American Indian) believed that physical activity can keep the brain healthy; walking in particular was mentioned by all groups. Diet and nutrition were also mentioned as protective factors, albeit less frequently (Wilcox et al., 2009).
Perceptions about cognitive health and impairment among various racial/ethnic groups were examined in an additional five studies (Otilingam and Gatz, 2008; Lee et al., 2010, Stansbury et al., 2010a; 2010b; Rovner et al., 2013). In a survey study with 209 South Korean American adults aged 40 years or older, most participants reported that not keeping the mind active (80%), social and physical inactivity due to living alone or in isolation (75%), problems with brain chemistry (71%), stress (62%), introverted or passive personality (61%), or the South Korean concept of han (i.e. unresolved personal/family issues or hardships; 56%) can lead to dementia (Lee et al., 2010). A study of 255 Asian Indian Americans found that loneliness (35.2%), stress (34.7%), older age (32.0%), mental illness (29.6%), head injury (27.4%), genetics (24.7%), alcohol (19.4%), and smoking (17.1%) were considered “very important” in determining whether a person develops dementia (Otilingam and Gatz, 2008). In a sample of 271 older African Americans, most reported (68%) they could take steps to prevent AD, although specific strategies were not investigated (Rovner et al., 2013). Additionally, almost half (49.3%) reported that developing AD was “God’s will.” Two studies using in-depth interviews with nine African American clergy found that respondents identified diet, age, genetics, and chronic illnesses (e.g. diabetes, hypertension) as potential risk factors for AD (Stansbury et al., 2010a; 2010b). All study participants described AD as incurable and stated that believing in “God’s will” would provide comfort while dealing with the disease (Stansbury et al., 2010b).
In other research comparing racial and ethnic perceptions about AD, both African Americans and whites cited genetics (75.4%) and old age (51.5%) as primary risk factors for AD (Connell et al., 2009). African Americans were significantly more likely than whites to report stress, exposure to toxins, mental illness, drinking too much alcohol, smoking too much, head injury, and old age as factors likely to increase risk. Between one-half and one-third of the 301 respondents reported keeping mentally active (58.1%), lowering stress (44.9%), keeping physically active (42.9%), and eating a healthy diet (35.9%) as behaviors believed to protect against AD; African American participants were more likely than whites to report each of these strategies (Connell et al., 2009). In another study of racial and ethnic differences in perceptions with 1,230 adults (Ayalon, 2013), the majority of respondents across racial and ethnic groups rated the following as “very important” or “somewhat important” to a person’s risk of developing AD: stress (55.6% white, 77.2% Latino, 82.5% African American) and genetics (90.7% white, 87.0% Latino, 84.0% African American). In terms of factors protecting against AD, over 80% of respondents regardless of the racial or ethnic group rated the following as “very important” or “somewhat important”: mental activity, physical activity, and healthy diet; however, whites were the most likely to report mental activity as protective whereas Latinos the least likely (95.2% vs. 84.4%) (Ayalon, 2013).
Low and colleagues (2011) conducted a survey of third generation Australians and compared their perceptions to three other ethnic groups (Chinese, Greek, and Italian) (n = 1,701). They found that 30%–43% of groups reported not knowing what caused dementia. Additionally, 28%–42% reported they did not know that dementia was associated with old age. Participants from different ethnic minorities suggested factors such as stress (e.g. 21% of Greek respondents), and loneliness (e.g. 15% of Chinese respondents) as plausible causes, whereas third generation Australians were more likely to suggest brain disease (27%) as the cause compared to other groups (Low et al., 2011).
Other earlier research conducted in Australia by Low and Anstey (2007; 2009) examined 17 behaviors believed to be related to risk-reduction in dementia. Low and Anstey (2007) subjected the 17 behaviors to factor analysis, which resulted in three sets of dementia risk-reduction factors: lifestyle (i.e. cardiovascular health, reducing stress, and improving intake of liquids), activity (i.e. physical, psychosocial, and mental), and nutrition (i.e. intake of specific nutritional chemicals, use of vitamin and nutritional supplements, and of non-aluminum cookware). Low and Anstey (2009) subsequently examined perceived risk and protective factors. Over 80% of participants, aged 18 years or older (n = 2,000), reported that genetics, old age, brain disease, and stroke or mini-stroke were related to increased risk of dementia. The most commonly reported protective factors were mental activity (38.8%), healthy diet (31.0%), physical activity (30.2%), and social engagement (13.9%).
In a study of 500 adults aged 18–65 years in Brazil, respondents “agreed” that the main causes of AD were drug use (93.2%), isolation (90.2%), and brain problems (89.0%) (Blay and Piza Peluso Ede, 2008). In a study of 2,767 older adults aged 60–84 years in South Korea, participants reported that being older was the most commonly perceived risk factor for AD (59.6%) followed by head trauma (33.6%) (Park et al., 2008). In a sample of 562 older adults aged 56–96 years residing in the United Kingdom (UK), 51% reported that family history, 38% head injury, 23% hypertension, 19% smoking, and 6% poor education as risk factors for dementia (Yeo et al., 2007). Potential protective factors were reportedly assessed but no data were provided. In another sample of 312 adults, aged 17–82 years, living in the UK were surveyed about risk factors for developing AD and about 75% of participants reported that they were not aware that hypertension or hypercholesterolemia may increase one’s risk (Hudson et al., 2012).
A study of 1,002 adults aged 18–92 years residing in Germany examined perceptions about activities that might protect against dementia. Brain/memory training (47.4%) and mental activities (33.9%) were the largest categories that participants reported might protect against dementia whereas active lifestyle, taking prescription medications, physical activity, social contact, and healthy diet were reported by less than 19% of the respondents (Luck et al., 2012). Bowes and colleagues (2012) studied 402 adults aged 50–65 years from the UK and assessed reported participation in mentally stimulating activities (e.g. reading, word puzzles, and new “brain-training” technology) as well as reasons for participating in these activities. Among respondents who mentioned each activity, they found that between 1.9% and 16.1% reported engaging in these activities to prevent memory loss or the onset of dementia or AD.
Perceptions of special populations: caregivers and family members
This “Healthy Brain Study” also included an examination of caregiver perceptions. Specifically, 25 Filipino Americans who cared for individuals with dementia viewed a healthy diet and engagement in social, mental, leisure, and physical activities as beneficial to cognitive health (Laditka et al., 2012). Avoiding smoking, alcohol, and drugs were also viewed as ways to protect cognitive health. In an analysis exploring caregiver versus patient perceptions (patient perceptions not reported here), 68 caregivers noted the potential cognitive benefits of eating well, being physically and mentally active, and staying socially involved, but they cautioned that these approaches do not “prevent” decline. They also discussed the role of genetics and family history as risk factors for AD (Beard et al., 2009). Other research studies included in this review also examined caregiver perceptions (Sullivan et al., 2007; McIlvane et al., 2008, Gray et al., 2009, Riva et al., 2012). In a study of 236 caregivers, Gray and colleagues (2009) reported that Hispanic/Latino and Chinese caregivers living in the US were more likely than their white counterparts to believe that medical interventions were effective in reducing, preventing, and delaying AD. In an Australian study by Sullivan and colleagues (2007), 13 caregivers of people with AD were more likely than 20 non-caregivers to believe persons with a close relative with AD have an increased risk of AD and that the cause of AD is unknown. Non-caregivers also believed that nutrition played no role in AD (Sullivan et al., 2007). In an Italian study of 1,111 survey respondents, the majority of both caregivers (54%) and non-caregivers (63%) felt that genetics were a risk factor for AD (Riva et al., 2012). Further, 21% of respondents reported that depression was a risk factor and less than 7% reported lower education was a risk factor.
Another study focused specifically on caregivers of individuals with mild cognitive impairment (McIlvane et al., 2008). The majority of the 29 caregivers believed that mental activity (71%), physical exercise (64%), and staying optimistic (54%) may prevent the progression of mild impairment to AD. Medication was not commonly identified (McIlvane et al., 2008). A separate study that assessed perceptions of a sample of adults (n = 51 telephone interview; 2 focus groups with 16 participants in total) with a family history of AD (Moscarillo et al., 2007) also reported that most individuals (72.9%) believed that their family history increased their risk.
Perceptions by age group
Eight studies indicated differences in perceptions by age group (Low and Anstey, 2007; Park et al., 2008; Low and Anstey, 2009; Lee et al., 2010; Anderson et al., 2011; Bowes et al., 2012; McParland et al., 2012; Riva et al., 2012 ). Anderson et al. (2011) compared perceptions between college-age younger adults (n = 82) and community-dwelling older adults (n = 57). Although many comparisons were made, we focus on summary findings related to perceived risks or “causes” of AD and protective factors between the two groups. When comparing older and younger participants’ lists of “causes of AD,” significant differences were found between older and younger participants in genetics/heredity (16.9% older vs. 26.4% younger), lifestyle (31.5% vs. 16.9%), aging (4.5% vs. 10.6%), other (10.6% vs. 5.9%), and brain dysfunction (1.1% vs. 11.1%). Concerning strategies to prevent AD, significant differences were found between older and younger adults on the number of strategies listed per person, with older adults listing twice the number of strategies as younger adults. Older adults were more likely than younger adults to cite social activities (10.3% vs. 2.0%) and less likely to indicate “there is nothing you can do” (4.3% vs. 28.4%).
Several studies examined age differences along with other demographic factors reported previously. Low and Anstey (2007), for example, compared four age groups (18–24, 35–49, 50–64, and 65+) examining differences in perceptions about the protective aspects of three domains against AD, including health and lifestyle, activity, or nutrition subscales. They reported the age groups 18–34 and 65+ years had significantly higher scores on all three subscales compared to the other age groups (35–49 and 50–64). Using logistic regression, Low and Anstey (2009) found that respondent age was significantly associated with suggesting the following risk factors (brain disease, stroke, stress, laziness) and protective factors (mental activity, physical activity, reducing alcohol and drug intake) for dementia. McParland and colleagues (2012) also examined age differences and protective factors for AD. They studied adults aged 18 years of older in Ireland and reported that adults aged 65 years and older were significantly more likely than 18–24 year olds (46% vs. 16%, respectively) to support the statement that a healthy diet and physical activity could protect people from AD. Riva and colleagues (2012) examined the effect of age on various AD perceptions among caregivers and non-caregivers. Of specific interest was that younger adults (18–40 years;) and middle-aged (41–64 years) compared with older adults (65+ years) agreed that genetics were a risk factor for AD, this was found regardless of reported status as caregivers.
Finally, three studies found differences in perceptions by age specifically among middle-aged and older or only older respondents. Lee and colleagues (2010) studied South Korean American respondents aged 40–79 years and found that the younger adults were more likely to report physical/environmental and cognitive/social factors were causes of dementia compared to older adults. Using a multivariate logistic regression analysis, Park and colleagues (2008) found that among adults aged 60–84 years in South Korea, being older was associated with worse knowledge of risk factors for AD. Bowes and colleagues (2012) found that the reported use of “brain-training technologies” for mental activity decreased with age and was not used by 65 year olds. They also found that the use of word puzzles increased with age among those between the aged of 50–65 years.
Perceptions of control of risk and protective factors
Two studies reported on perception about control and preventing or reducing the risk of cognitive impairment. In a sample of African American, Hispanic, and white adults (n = 1,176) aged 35 years or older, 53.1% agreed with a statement that nothing can be done to “maintain a healthy memory and reduce the chances of getting Alzheimer’s disease,” and 74.4% (more African Americans and Hispanics than whites) reported not making changes to their diet or lifestyle to avoid AD (Connell et al., 2007). After having 140 middle-aged and older adults read a vignette about a person with symptoms of cognitive impairment, VonDras (2009) found that participants perceived only modest personal control in preventing future symptoms. Finally, one study of 1,204 adults in Ireland revealed that the majority (64%) did not believe that diet and exercise could protect against dementia. Participants suggested medication to treat AD but did not mention drugs as a way to reduce risk (McParland et al., 2012). In contrast, a recent national survey study (n = 4,728) revealed that US consumers believed that multiple factors – including intellectual stimulation (86.6%), physical activity (82.6%), healthy diet (82.5%), social activity (64.1%), vitamins/supplements (64.1%), avoiding smoking (51.8%), and prescription medication (31.4%) – could prevent or delay cognitive impairment (Friedman et al., 2013).
Discussion
This is the first review of published studies summarizing the public’s perceptions about risk and protective factors related to cognitive functioning since the 2007 National Public Health Road Map to Maintaining Cognitive Health. The current investigation indicates that the general public, regardless of nationality, race/ethnicity, or gender, identified well-established risk factors for cognitive impairment, such as genetics, along with lifestyle factors, such as physical or social activities and healthy diet, as factors that may reduce the risk of dementia or AD.
Within the scientific community, there is ongoing debate about the role of lifestyle factors in reducing the risk of AD and other dementias. An expert panel recently concluded that the level of evidence is considered insufficient to support the use of lifestyle interventions in prevention efforts (Daviglus et al., 2011); however, a recent meta-analysis by Norton and colleagues (2014) reported that around a third of ADs cases worldwide might be attributable to potentially modifiable risk factors such as smoking, physical inactivity, and midlife obesity. As the number of older adults continues to increase, there is a need for evidence-informed communication about prevention research and findings. Importantly, the reduction of key risk factors such as not smoking and the promotion of factors such as physical activity are well recognized as critical to healthy aging.
Although population level interventions may need to be implemented at the earliest stage possible (from a scientific perspective), if they are to have a chance at reducing incidence of cognitive impairment, our findings still highlight the need for the acceleration of scientific research and subsequent dissemination efforts to provide the public with accurate information about the current evidence regarding reducing risks for cognitive impairment. Focused research regarding effective and relevant behavior change strategies specific to cognitive health promotion will also be required.
Strengths and limitations
This scoping review provides insight into public perceptions about risk and protective factors related to cognitive health and impairment. The study has several strengths. First, the methodology ensured that every abstract was examined by at least two reviewers, with a third reviewer available for adjudication. Similarly, two separate reviewers read each article for a decision on inclusion and abstraction. Second, an international focus was purposefully maintained by including studies from many countries (although only articles in English were reviewed). Third, qualitative studies were included and the summaries presented in narrative or descriptive form. Finally, this review draws upon the experience of a research team that has developed and refined a standardized literature review process over ten years of collaborating within a highly productive research network. The team included relevant disciplines of public health, nursing, medicine, psychology, and communications.
There are several limitations of this review. Although all studies reviewed reported participants’ perceptions, the methods and reporting styles varied from study to study. Therefore, readers should be cautious when interpreting comparisons. We also cannot generalize results from this review because inferences about the data collected in each of the studies were driven by the research questions and measures in each of the studies. Future work would benefit from more systematic examination of perceptions across settings as well as different cultural group’s perceptions about established, probable, possible, and unlikely risk factors associated with cognitive impairment, AD, and other dementias, as well as their views about which factors may be modifiable. Another limitation is the diversity of methods and evaluation tools used across studies and how these approaches may have resulted in different responses to questions about cognition-related perceptions. Although most studies were not eligible due to the population studied, we did not include psychological, experimental, or interventional studies. This review focused on public perceptions of cognitive health and impairment rather than whether or not these perceptions were modifiable through experimental conditions or interventions. Even though the exclusion of experimental/interventional studies serves the study purpose, it is acknowledged that these studies may include important findings relevant to perceptions of cognitive health and impairment. Finally, studies focused only on knowledge and screening were excluded even though there may be overlap between perceptions and knowledge, and some screening-based studies might also contribute to an overall understanding of public perceptions of cognitive health and impairment. Research focused on knowledge and how to potentially improve the public’s knowledge and behaviors is needed but was beyond the scope of this review.
Implications for future research
This study provides an identification and compilation of the literature concerning the general public’s perceptions of factors that may increase the risk of or decrease the occurrence of cognitive impairment, AD, and other dementias. The scoping review examined the body of work produced since the 2007 National Public Health Road Map to Maintaining Cognitive Health. Given the nature of the studies exploring these issues, we were able to document the diversity of findings but found no consistent patterns of risk or protective perceptions across studies. This is not surprising given that the current evidence base is limited by a lack of common definitions, measures, and instruments across studies, as found in this scoping review. As a result, this review underscores the need to develop, validate, and disseminate measures that can be employed across studies to better assess and track changes in public perceptions over time and across locations and cultures. Future studies may also benefit from greater attention to distinguishing between different types of perceptions such as general attitudes versus perceptions about individual risk factors. Without the use of common definitions and measures we will continue to be limited to descriptions of individual studies but will not advance the field to our ultimate goal to create communication strategies that can promote evidence-based messages designed for populations or different population groups though effective communication channels.
Implications for practice
The findings from this study are in alignment with key actions in the 2013 Road Map (Alzheimer’s Association and Centers for Disease Control and Prevention, 2013) and the 2014 World Alzheimer Report (Alzheimer’s Disease International, 2014). Understanding the public’s perceptions about cognitive health and impairment will enable better identification and promotion of culturally appropriate strategies to increase public awareness and develop effective communications related to cognitive health, impairment, AD, and other dementias. Although evidence is regarded currently as insufficient to promote particular lifestyle interventions for cognitive health, research in progress could eventually yield a strong evidence base for specific recommendations. In the interim, knowledge exists regarding some factors, e.g. smoking, that increase risk and others, e.g. physical activity, that promote overall health and may decrease risk of impairment (Alzheimer’s Disease International, 2014). A fuller understanding of the range of public perceptions about risk and protective factors for cognitive health and impairment will prepare us to more effectively create messages to reach communities most in need of information about these critical public health issues. Moreover, it is important to counter misinformation using research-based messages and to consider how best to reduce stigma and its potential impact on behaviors such as information seeking. Working in partnership with researchers and practitioners can help translate knowledge into practice in a timely manner that will be crucial given the escalation of cognitive impairment prevalence with population aging.
Acknowledgments
This research is the result of work conducted by the Centers for Disease Control and Prevention (CDC) Healthy Aging Research Network. The CDC Healthy Aging Research Network is a Prevention Research Centers program funded by the CDC Healthy Aging Program. The research was supported in part by cooperative agreements from CDC’s Prevention Research Centers Program: U48-DP-001908, U48-DP-001938, U48-DP-001944, U48-DP-001936, and U48-DP-001911.
We are grateful to Elaine Kurtovich (University of California, Berkeley) for her assistance with abstract reviews and article abstractions and William Thomas (CDC) for his expertise in searching the literature.
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the CDC.
Footnotes
Conflict of interest
None.
Description of authors’ roles
D.B. Friedman, K. Becofsky, and L.A. Anderson designed the study with input from all authors. D.B. Friedman and K. Becofsky supervised the data collection. D.B. Friedman, K. Becofsky, L.A. Anderson, L.L. Bryant, and R.H. Hunter were the main writers of the paper, however, all of the remaining authors (S.L. Ivey, B. Belza, R.G. Logsdon, S. Brannon, A.E. Vandenberg, and S.Y. Lin) contributed to the writing and editing of manuscript sections (especially for the Discussion section to which all 11 authors contributed content). All of the 11 authors were involved in the review of abstracts and in the abstraction of data from full articles that were included in this review paper. K. Becofsky was responsible for compiling and summarizing results from the review under the supervision of D.B. Friedman.
References
- Albert MS, et al. The healthy brain and our aging population: translating science to public health practice. Alzheimer’s & Dementia. 2007;3:S3–S5. doi: 10.1016/j.jalz.2007.01.016. [DOI] [PubMed] [Google Scholar]
- Alzheimer’s Association. Alzheimer’s Disease Facts and Figures. Chicago, IL: Alzheimer’s Association; 2014. [DOI] [PubMed] [Google Scholar]
- Alzheimer’s Association and Centers for Disease Control and Prevention. The Healthy Brain Initiative: the Public Health Road Map for State and National Partnerships, 2013–2018. Chicago, IL: Alzheimer’s Association; 2013. [Google Scholar]
- Alzheimer’s Disease International. World Alzheimer Report 2014: Dementia and Risk Reduction. An Analysis of Protective and Modifiable Factors [Online] London, England: Alzheimer’s Disease International; 2014. [Accessed 21 September 2014]. Available at: http://www.alz.co.uk/research/WorldAlzheimerReport2014.pdf. [Google Scholar]
- Anderson LA, McConnell SR. Cognitive health: an emerging public health issue. Alzheimer’s & Dementia. 2007a;3:S70–S73. doi: 10.1016/j.jalz.2007.01.018. [DOI] [PubMed] [Google Scholar]
- Anderson LA, McConnell SR. The healthy brain and our aging population: translating science to public health practice. Alzheimer’s & Dementia. 2007b;3:S1–S2. doi: 10.1016/j.jalz.2007.01.017. [DOI] [PubMed] [Google Scholar]
- Anderson LN, McCaul KD, Langley LK. Common-sense beliefs about the prevention of Alzheimer’s disease. Aging & Mental Health. 2011;15:922–931. doi: 10.1080/13607863.2011.569478. [DOI] [PubMed] [Google Scholar]
- Arksey H, O’Malley L. Scoping studies: towards a methodological framework. International Journal of Social Research Methodology. 2005;8:19–32. [Google Scholar]
- Ayalon L. Re-examining ethnic differences in concerns, knowledge, and beliefs about Alzheimer’s disease: results from a national sample. International Journal of Geriatric Psychiatry. 2013;28:1288–1295. doi: 10.1002/gps.3959. [DOI] [PubMed] [Google Scholar]
- Beard RL, Fetterman DJ, Wu B, Bryant L. The two voices of Alzheimer’s: attitudes toward brain health by diagnosed individuals and support persons. The Gerontologist. 2009;49(Suppl 1):S40–S49. doi: 10.1093/geront/gnp083. [DOI] [PubMed] [Google Scholar]
- Blay SL, de Piza Peluso ET. The public’s ability to recognize Alzheimer disease and their beliefs about its causes. Alzheimer’s Disease and Associated Disorders. 2008;22:79–85. doi: 10.1097/WAD.0b013e31815ccd47. [DOI] [PubMed] [Google Scholar]
- Bowes A, McCabe L, Wilson M, Craig D. ‘Keeping your brain active’: the activities of people aged 50–65 years. International Journal of Geriatric Psychiatry. 2012;27:253–261. doi: 10.1002/gps.2708. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. The CDC Healthy Brain Initiative: Progress 2006–2011. Atlanta, GA: Centers for Disease Control and Prevention; 2011. [Google Scholar]
- Centers for Disease Control and Prevention and the Alzheimer’s Association. The Healthy Brain Initiative: a National Public Health Road Map to Maintaining Cognitive Health. Chicago, IL: Alzheimer’s Association; 2007. [Google Scholar]
- Connell CM, Scott Roberts J, McLaughlin SJ. Public opinion about Alzheimer disease among blacks, hispanics, and whites: results from a national survey. Alzheimer’s Disease and Associated Disorders. 2007;21:232–240. doi: 10.1097/WAD.0b013e3181461740. [DOI] [PubMed] [Google Scholar]
- Connell CM, Scott Roberts J, McLaughlin SJ, Akinleye D. Racial differences in knowledge and beliefs about Alzheimer disease. Alzheimer’s Disease & Associated Disorders. 2009;23:110–116. doi: 10.1097/WAD.0b013e318192e94d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daviglus ML, et al. Risk factors and preventive interventions for Alzheimer disease: state of the science. Archives of Neurology. 2011;68:1185–1190. doi: 10.1001/archneurol.2011.100. [DOI] [PubMed] [Google Scholar]
- Department of Health and Human Services. [Accessed 1 February 2013];Healthy People 2020: Dementias, Including Alzheimer’s Disease. 2010 [Online]. Available at: http://www.healthypeople.gov/2020/topicsobjectives2020/overview.aspx?topicid=7.
- Department of Health and Human Services. [Accessed 30 January 2013];National Plan to Address Alzheimer’s Disease. 2012 [Online]. Available at: http://aspe.hhs.gov/daltcp/napa/natlplan.shtml.
- Friedman DB, et al. Ethnically diverse older adults’ beliefs about staying mentally sharp. International Journal of Aging & Human Development. 2011;73:27–52. doi: 10.2190/AG.73.1.b. [DOI] [PubMed] [Google Scholar]
- Friedman DB, et al. Beliefs and communication practices regarding cognitive functioning among consumers and primary care providers in the United States, 2009. Preventing Chronic Disease. 2013;10:E58. doi: 10.5888/pcd10.120249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant MJ, Booth A. A typology of reviews: an analysis of 14 review types and associated methodologies. Health Information & Libraries Journal. 2009;26:91–108. doi: 10.1111/j.1471-1842.2009.00848.x. [DOI] [PubMed] [Google Scholar]
- Gray HL, Jimenez DE, Cucciare MA, Tong HQ, Gallagher-Thompson D. Ethnic differences in beliefs regarding Alzheimer disease among dementia family caregivers. American Journal of Geriatric Psychiatry. 2009;17:925–933. doi: 10.1097/JGP.0b013e3181ad4f3c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hebert LE, Weuve J, Scherr PA, Evans DA. Alzheimer disease in the United States (2010–2050) estimated using the 2010 census. Neurology. 2013;80:1778–1783. doi: 10.1212/WNL.0b013e31828726f5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hendrie HC, et al. The NIH cognitive and emotional health project. Report of the critical evaluation study committee. Alzheimer’s & Dementia. 2006;2:12–32. doi: 10.1016/j.jalz.2005.11.004. [DOI] [PubMed] [Google Scholar]
- Hudson JM, Pollux PM, Mistry B, Hobson S. Beliefs about Alzheimer’s disease in Britain. Aging & Mental Health. 2012;16:828–835. doi: 10.1080/13607863.2012.660620. [DOI] [PubMed] [Google Scholar]
- Ivey SL, et al. Experiences and concerns of family caregivers providing support to people with dementia: a cross-cultural perspective. Dementia (London) 2013;12:806–820. doi: 10.1177/1471301212446872. [DOI] [PubMed] [Google Scholar]
- Laditka SB, et al. Attitudes about aging well among a diverse group of older Americans: implications for promoting cognitive health. The Gerontologist. 2009;49(Suppl 1):S30–S39. doi: 10.1093/geront/gnp084. [DOI] [PubMed] [Google Scholar]
- Laditka SB, et al. How do older people describe others with cognitive impairment? A multi-ethnic study in the United States. Ageing & Society. 2013;33:369–392. [Google Scholar]
- Laditka SB, et al. Beliefs about promoting cognitive health among Filipino Americans who care for persons with dementia. International Journal of Aging & Human Development. 2012;75:273–296. doi: 10.2190/AG.75.3.d. [DOI] [PubMed] [Google Scholar]
- Lee SE, Diwan S, Yeo G. Causal attributions of dementia among Korean American immigrants. Journal of Gerontological Social Work. 2010;53:743–759. doi: 10.1080/01634372.2010.515290. [DOI] [PubMed] [Google Scholar]
- Levac D, Colquhoun H, O’Brien KK. Scoping studies: advancing the methodology. Implementation Science. 2010;5:69. doi: 10.1186/1748-5908-5-69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Low LF, Anstey KJ. The public’s perception of the plausibility of dementia risk factors is not influenced by scientific evidence. Dementia & Geriatric Cognitive Disorders. 2007;23:202–206. doi: 10.1159/000099038. [DOI] [PubMed] [Google Scholar]
- Low LF, Anstey KJ. Dementia literacy: recognition and beliefs on dementia of the Australian public. Alzheimer’s & Dementia. 2009;5:43–49. doi: 10.1016/j.jalz.2008.03.011. [DOI] [PubMed] [Google Scholar]
- Low LF, et al. Recognition, attitudes and causal beliefs regarding dementia in italian, greek and chinese australians. Dementia & Geriatric Cognitive Disorders. 2011;30:499–508. doi: 10.1159/000321667. [DOI] [PubMed] [Google Scholar]
- Luck T, et al. Attitudes of the German general population toward early diagnosis of dementia–results of a representative telephone survey. PLoS ONE. 2012;7:e50792. doi: 10.1371/journal.pone.0050792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McIlvane JM, Popa MA, Robinson B, Houseweart K, Haley WE. Perceptions of Illness, coping, and well-being in persons with mild cognitive impairment and their care partners. Alzheimer’s Disease & Associated Disorders. 2008;22:284–292. doi: 10.1097/WAD.0b013e318169d714. [DOI] [PubMed] [Google Scholar]
- McParland P, Devine P, Innes A, Gayle V. Dementia knowledge and attitudes of the general public in Northern Ireland: an analysis of national survey data. International Psychogeriatrics. 2012;24:1600–1613. doi: 10.1017/S1041610212000658. [DOI] [PubMed] [Google Scholar]
- Moscarillo TJ, et al. Knowledge of and attitudes about Alzheimer disease genetics: report of a pilot survey and two focus groups. Community Genetics. 2007;10:97–102. doi: 10.1159/000099087. [DOI] [PubMed] [Google Scholar]
- Norton S, Matthews FE, Barnes DE, Yaffe K, Brayne C. Potential for primary prevention for Alzheimer’s disease: an analysis of population-based data. The Lancet. 2014;13:788–794. doi: 10.1016/S1474-4422(14)70136-X. [DOI] [PubMed] [Google Scholar]
- Otilingam PG, Gatz M. Perceptions of dementia among Asian Indian Americans. AAPI Nexus: Asian Americans & Pacific Islanders Policy, Practice and Community. 2008;6:45–66. [Google Scholar]
- Park MH, et al. Awareness of putative risk factors for Alzheimer’s disease among elderly Koreans. Acta Neuropsychiatrica. 2008;20:20–24. doi: 10.1111/j.1601-5215.2007.00230.x. [DOI] [PubMed] [Google Scholar]
- Price AE, Corwin SJ, Friedman DB, Laditka SB, Colabianchi N, Montgomery KM. Older adults’ perceptions of physical activity and cognitive health: implications for health communication. Health Education & Behavior. 2011;38:15–24. doi: 10.1177/1090198110369764. [DOI] [PubMed] [Google Scholar]
- Riva M, Caratozzolo S, Zanetti M, Vicini Chilovi B, Padovani A, Rozzini L. Knowledge and attitudes about Alzheimer’s disease in the lay public: influence of caregiving experience and other socio-demographic factors in an Italian sample. Aging-Clinical & Experimental Research. 2012;24:509–516. doi: 10.3275/8366. [DOI] [PubMed] [Google Scholar]
- Rovner BW, Casten RJ, Harris LF. Cultural diversity and views on Alzheimer disease in older African Americans. Alzheimer’s Disease & Associated Disorders. 2013;27:133–137. doi: 10.1097/WAD.0b013e3182654794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stansbury KL, Harley DA, Brown-Hughes T. African-American urban clergy’s literacy of Alzheimer’s disease. Social Work in Mental Health. 2010a;8:254–266. [Google Scholar]
- Stansbury KL, Marshall GL, Harley DA, Nelson N. Rural African American clergy: an exploration of their attitudes and knowledge of Alzheimer’s disease. Journal of Gerontological Social Work. 2010b;53:352–365. doi: 10.1080/01634371003741508. [DOI] [PubMed] [Google Scholar]
- Sullivan K, Muscat T, Mulgrew K. Knowledge of Alzheimer’s disease among patients, carers, and noncarer adults: misconceptions, knowledge gaps, and correct beliefs. Topics in Geriatric Rehabilitation. 2007;23:137–148. [Google Scholar]
- VonDras D. Lay appraisal of cognitive impairment symptoms and related prevention beliefs in a community-dwelling sample of midlife and older adults. Journal of Applied Gerontology. 2009;28:342–368. [Google Scholar]
- Wilcox S, et al. Perceptions and beliefs about the role of physical activity and nutrition on brain health in older adults. The Gerontologist. 2009;49(Suppl 1):S61–S71. doi: 10.1093/geront/gnp078. [DOI] [PubMed] [Google Scholar]
- Wu B, Goins RT, Laditka JN, Ignatenko V, Goedereis E. Gender differences in views about cognitive health and healthy lifestyle behaviors among rural older adults. The Gerontologist. 2009;49:S72–S78. doi: 10.1093/geront/gnp077. [DOI] [PubMed] [Google Scholar]
- Yeo LH, Horan MA, Jones M, Pendleton N. Perceptions of risk and prevention of dementia in the healthy elderly. Dementia & Geriatric Cognitive Disorders. 2007;23:368–371. doi: 10.1159/000101338. [DOI] [PubMed] [Google Scholar]