Abstract
Background
Once a disease of developed countries, type 2 diabetes mellitus (T2DM) has become widespread worldwide. For people with T2DM, achievement of therapeutic outcomes demands the rational and quality use of medicine.
Aims
The primary aim of this study was to examine the prevalence of diabetes and prescribing patterns of anti-diabetic medications in Australia and Malaysia.
Methods
The most recent, publicly available, statistical reports (2004–2008) on the use of medicines published in Australia and in Malaysia were evaluated. Defined daily doses (DDDs/1,000 population/day) were derived from the reports and used to rank and compare individual drug use.
Results
There was an increasing trend in the prevalence of diabetes in Australia, although there is a greater predicted increase in prevalence for Malaysia. While drugs used for the treatment of diabetes were not the most highly used drugs in Australia, their use increased during the study period, from 42.64 to 48.61 DDD/1,000/day. Anti-diabetic drugs were the most frequently dispensed class of drugs in Malaysia. Although the total consumption of anti-diabetic drugs in Malaysia decreased between 2006 and 2007 (from 40.30 to 39.72), this was followed by a marked increase to 46.69 in 2008. There was a marked reduction in the dispensing of insulin in Malaysia from 2004 to 2007 (7.77 to 3.23).
Conclusion
The use of drugs to treat diabetes does not reflect the usage patterns found in Australia. Effective drug use reviews are required to ensure impartial access in middle- and low-income countries.
Keywords: Utilisation, drugs, diabetes, Malaysia, Australia, insulin, metformin
What this study adds:
-
What is known about this subject?
Worldwide there is an emerging focus on treatment of diabetes and associated complications. Dispensing trends reflect drug usage and treatment of medical conditions.
-
What new information is offered in this study?
This paper highlights the differences between Australia and Malaysia in the drugs used to treat diabetes, and their concordance with national and international treatment guidelines.
-
What are the implications for research, policy, or practice?
Effective drug usage reviews are needed for diabetes management protocol in developing countries, and for the development of educational interventions, review of treatment guidelines, and education of prescribers and patients.
Background
Diabetes mellitus is a chronic, progressive disorder that affects millions of people worldwide.1 Once a disease of developed countries, type 2 diabetes mellitus (T2DM) is now in every country.2 Global estimates published in 2010 reported the world prevalence as 6.4 per cent, affecting 285 million adults (aged 20–79 years); the incidence is predicted to rise to 7.7 per cent and 439 million by 2030.3 The predicted increase in patients with diabetes is nearly twice the annual growth of the total world adult population.3
Both the incidence and prevalence of diabetes are escalating, particularly in developing and newly industrialised nations, and also among disadvantaged people in developed countries; these populations are said to be at highest risk of having diabetes.3 By 2030, the increase in the number of adults with diabetes over the preceding decade is estimated to be 20 per cent in developed and 69 per cent in developing countries, respectively.3 Malaysia, situated in Southeast Asia, is one of the most prominent developing, middle-income countries;4 it was also among the top 10 countries for diabetes prevalence in 2010 and is predicted to remain so until 2030.3 Diabetes prevalence among the adult population in Malaysia (>18 years) has increased significantly over recent years from 11.6 per cent in 20065,6 to 22.9 per cent in 2013.7
Diabetes is the fastest growing chronic disease in Australia and the AusDiab Follow-up Study (2010) estimated the total number of Australians with diabetes and pre-diabetes at 3.2 million,8 or 14.3 per cent of the population at the time. This is a marked increase since 1995, when self-report census data indicated that 2.4 per cent of Australians (430,700 people) had been diagnosed with diabetes at some time during their lives. The figure increased to 3.6 per cent in 2004–05,9 and to 3.8 per cent (an estimated 818,200 people) in 2007–08.10 In 2011–12, 4.0 per cent of the Australian population (875,400 people) reported having some type of diabetes; however, the prevalence of diabetes remained stable between 2007–08 and 2011–12 (both 4.0 per cent).11 Diabetes is expected to become the leading contributor to disease burden in Australia by 2023.12
Dispensing trends reflect the use of drugs and therefore the treatment of medical conditions.13 The primary aim of this descriptive study was to examine the prevalence of diabetes and prescribing patterns of anti-diabetic medications in Australia and Malaysia, to evaluate prescribing trends and their concordance with national and international treatment guidelines. This comparison was made between a developed country with adequate health resources and an increasing prevalence of diabetes (Australia), and a middle-income developing country with a high prevalence of diabetes (Malaysia). The underpinning research question was: How does the use of drugs to treat diabetes differ between Australia and Malaysia? The findings potentially serve as a means of improving the quality use of medicine, enhancing therapeutic outcomes, and indicating over- or under-consumption of medicines in both countries.
Method
Assessing the prevalence of diabetes in Australia and Malaysia
The prevalence of diabetes in this paper is presented using estimates reported by Shaw et al.,3 where the authors derived prevalence estimates for Australia from the Australian Diabetes, Obesity and Lifestyle Study,14 and the National Diabetes Service Scheme, Diabetes Australia.15
The prevalence of diabetes in Malaysia is based on figures published in the National Health and Morbidity Survey (NHMS) reports.5,7 NHMS is a nationwide survey of self-reported data that include medicine use, dietary habits, various disease states, and demographics, which were first published in 1986 and is now published every 10 years.5,7 Although we focused on both types (type 1 and 2) of diabetes in this study, about 90 per cent of all cases of diabetes in both countries are T2DM.3
Assessing diabetes-related medicines use
Publicly available Australian and Malaysian reports containing statistics on medicine use for each year from 2004 to 2008 (inclusive) were used; the focus for this paper was anti-diabetic drugs.16,17 The published reports from both countries adopted the same unit (DDD/1,000 population/day) to describe medicine usage which facilitated comparison between the two countries. Dispensing databases are compiled from claims data and essentially such data are designed for administrative purposes; however, the large size of such databases makes them suitable for drug utilisation studies despite their lack of clinical information. To facilitate international comparison, drugs are classified according to the World Health Organization (WHO) Anatomical Therapeutic Chemical (ATC) classification system, and Defined Daily Doses (DDDs) can be used to rank and compare individual drugs.18 The DDD is the international unit of drug use established by the Nordic Council on Medicines and the WHO, and is assumed to be an average dose of the drug per day for adults for its main indication.19,20
Medicines use data, Australia
The Australian Statistics on Medicines (ASM) is an annual government publication produced by the Drug Utilisation Sub-Committee (DUSC) of the Pharmaceutical Benefits Advisory Committee, and was first published in 1997. The “...comprehensive and valid statistics on the Australian use of medicines...” is published in the public domain “...for use by interested parties...”.17 The reports contain analyses of retrospective data of subsided medicines prescribed by registered general practitioners (GP) in community practice in Australia. For example, the report published in 2013 contained data from 2010. These reports provide information about medicines that are subsidised by the Australian government for its citizens under the Pharmaceutical Benefits Scheme (PBS) or the Repatriation Pharmaceutical Benefits Scheme (RPBS); the latter is specifically for war veterans and their dependents.17 Dispensing data are collected electronically from two sources, namely, Medicare Australia records through the PBS/RPBS and the DUSC survey of community pharmacies;17 both sources are compiled from databases based on electronic claims data.
Medicines use data, Malaysia
The Ministry of Health in Malaysia publishes statistics on medicines using retrospective data derived from the Ministry of Health (public institutions), as well as from private hospitals, university and armed forces, (private) GP prescribing, and (private) pharmacy dispensing.16 The medicines provided through public hospitals or clinics are dispensed free of charge to Malaysian citizens and reports are therefore restricted to “prescription” medicines,16 while prescription medicines dispensed in community pharmacies are paid for in full by the patient. The first Malaysian Statistics on Medicine (MSM) report published in 2013 contains data from 2008.16 The major anti-diabetic drug classes included for comparison were insulin and analogues, biguanides, sulfonylureas, alpha glucosidase, thiazolidinediones, and dipeptidyl peptidase 4 inhibitors. Descriptive analyses presented in the tables and figures in this paper were carried out using Microsoft Excel (Microsoft Corp., Palo Alto, CA). Descriptive statistics were used to analyse frequency, percentage, and mean.
Results
Diabetes prevalence
The population characteristics of Malaysia (a developing country) and Australia (a developed country) for the period of this study were similar.21,22 There was an increasing trend in the percentage prevalence of diabetes in both countries; however, it was 1.5 times higher in Malaysia (10.9) than Australia (7.2).3
Drugs used to treat diabetes
Although the increase in the use of drugs used to treat diabetes in Australia was steady, in Malaysia it declined pointedly in 2005 (35.90 DDDs/1,000/day), with a smaller reduction in 2007 (from 40.39 in 2006 to 39.72 DDDs/1,000/day in 2007), which was followed by a marked increase in 2008 to 46.69 DDDs/1,000/day (Figure 1).
Figure 1: Anti-diabetic drug use in Australia and Malaysia, 2004–2008, according to DDD/1,000/day.
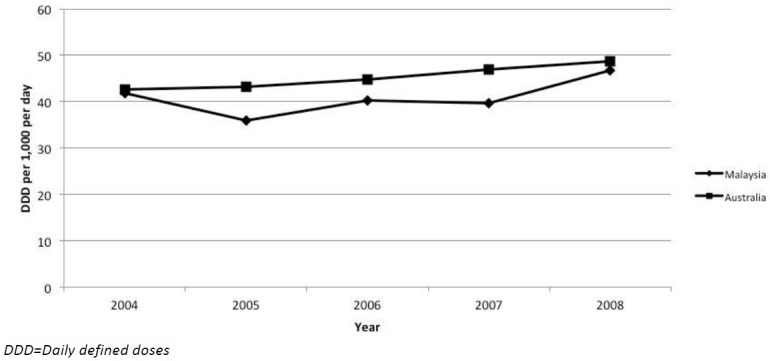
In Australia, the overall use of anti-diabetic drugs increased between 2004 (42.64 DDDs/1,000/day) and 2008 (48.61 DDDs/1,000/day), although the most frequently dispensed therapeutic drug class during the study period (2004–2008) included drugs to treat hyperlipidaemia and cardiovascular diseases.17 The two most frequently dispensed subgroups to treat diabetes in Australia were sulfonylureas and biguanides (2004–2008; Table 1), although there was a decrease in the use of sulfonylureas over the study period (14.35 in 2004, to 11.55 DDDs/1,000/day in 2008). The biguanide (metformin) was the most frequently used oral anti-diabetic drug in Australia from 2004 to 2008, and while the use of the sulfonylurea (glibenclamide) was relatively low, the use of glibenclamide as well as gliclazide declined between 2004 and 2008.
Table 1: Comparison of anti-diabetic medication use in Australia and Malaysia, 2004–2008.
| Therapeutics groups | 2004 | 2005 | 2006 | 2007 | 2008 | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| Malaysia | Australia | Malaysia | Australia | Malaysia | Australia | Malaysia | Australia | Malaysia | Australia | |
| Total antidiabetics use | 41.93 | 42.64 | 35.90 | 43.25 | 40.30 | 44.80 | 39.72 | 46.99 | 46.69 | 48.61 |
| Insulin and analogues | 7.77 | 13.49 | 3.81 | 13.93 | 3.29 | 14.57 | 3.23 | 15.70 | 3.71 | 16.66 |
| Birguanides (meformin) | 11.74 | 13.72 | 11.98 | 14. 34 | 13.15 | 15.46 | 14.28 | 16.24 | 13.55 | 17.16 |
| Sulfonylureas | 21.15 | 14. 35 | 19.16 | 13.31 | 22.08 | 12.84 | 20.45 | 11.98 | 27.75 | 11.55 |
| Alpha glucosidase inhibitors (Acarbose) | 0.38 | 0.25 | 0.49 | 0.22 | 0.45 | 0.18 | 0.83 | 0.17 | 0.71 | 0.16 |
| Thiazolidinediones | 0.57 | 0.81 | 0.21 | 1.46 | 0.20 | 2.31 | 0.44 | 2.87 | 0.21 | 2.81 |
| Dipeptidyl peptidase 4 inhibitors (Sitagliptin) | - | - | - | - | - | - | 0.02 | - | 0.09 | 0.14 |
| Others, exel. insulin | 0.27 | 0.006 | 0.15 | 0.003 | 0.07 | 0.005 | 0.08 | 0.01 | 0.04 | 0.005 |
Note: Comparisons are based on DDD/1,000/day (daily defined doses)
In contrast, the most frequently dispensed drugs in Malaysia were sulfonylureas, used for the treatment of diabetes. Nationally, the drug glibenclamide was ranked first among the top 40 drugs between 2004 (14.49 DDDs/1,000/day) and 2006 (15.53 DDDs/1,000/day). Glibenclamide was replaced in subsequent years by metformin (14.28 DDDs/1,000/day in 2007) and gliclazide (18.80 DDDs/1,000/day in 2008) (Figure 2).
Figure 2:Use of the top five anti-diabetic drugs in Australia and Malaysia, 2004–2008.
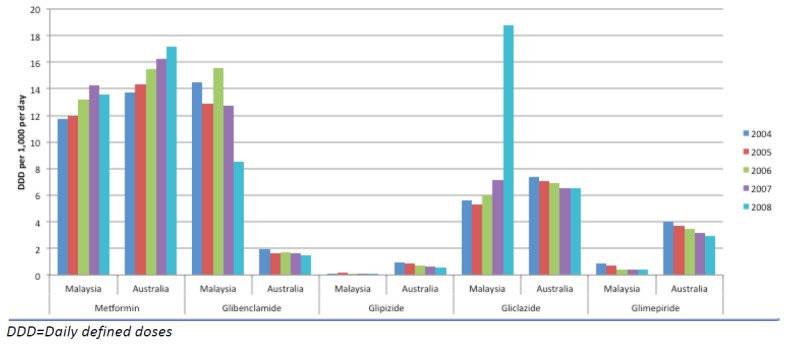
The use of the alpha glucosidase inhibitor acarbose increased more than two-fold In Malaysia between 2004 and 2007 (from 0.38 to 0.83 DDDs/1,000/day) followed by a decrease to 0.71 DDDs/1,000/day (2008). The thiazolidinediones (rosiglitazone and pioglitazone) were used less frequently in Malaysia in 2008 (0.21) compared to Australia (2.81 DDDs/1,000/day respectively; Table 1), although the use of rosiglitazone in Malaysia almost doubled from 2006 to 2007 (0.20 to 0.43 DDDs/1,000/day; Figure 2).
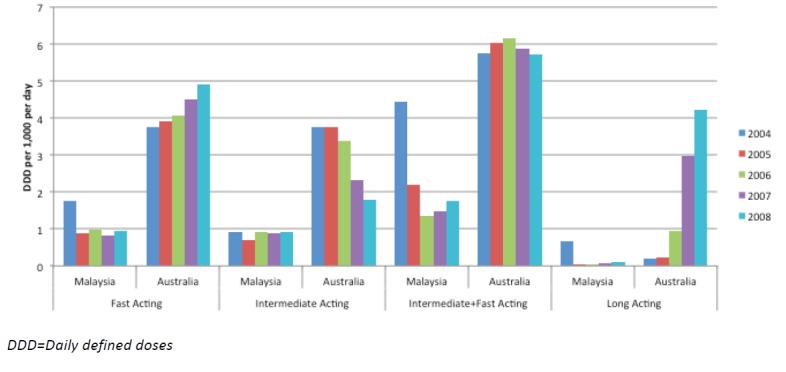
Insulin use in Australia was substantially higher than in Malaysia. Despite a small decrease in insulin use in Australia between 2004 and 2008, the overall increase from 13.49 to 16.66 during the study period (Table 1) was not reflected in Malaysia (Figure 3). Insulin dispensing decreased by 50 per cent in Malaysia from 2004 to 2007 (7.78 to 3.23 DDDs/1,000/day), followed by a small increase to 3.71 DDDs/1,000/day in 2008 (Figure 4). The most widely used insulin in both countries was premixed insulin and analogues (intermediate + fast-acting).
Figure 3:Insulin use in Australia and Malaysia, 2004–2008, according to DDD/1,000/day.
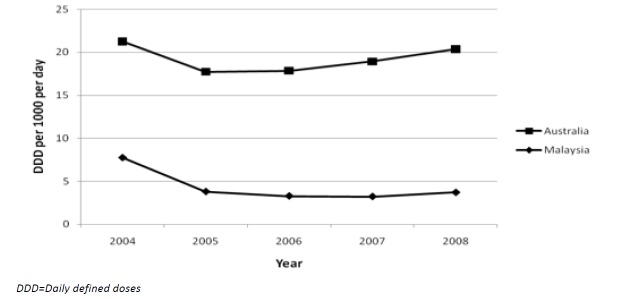
Figure 4: Use of different types of insulin and analogues in Australia and Malaysia, 2004–2008.
Discussion
There were similar trends of increasing diabetes prevalence between the two countries but marked differences in the use of anti-diabetic drugs.3,16,17 The total consumption of drugs used to treat diabetes in Malaysia decreased between 2004 and 2007 and was followed by a marked increase in 2008, while in Australia their use steadily increased during the same period (2004–2008).
Based on global estimates, the prevalence of diabetes in Malaysia is significantly higher than Australia, a difference that is predicted to continue to widen by 2030.3 The increasing prevalence among adults aged ≥18 years in Malaysia has been reported elsewhere;5,7,23 we observed that the prevalence was steeper in Malaysia than Australia. The situation in Malaysia is alarming and as the prevalence of diabetes is expected to increase, the number of patients with diabetes—diagnosed and undiagnosed, treated, and untreated—is expected to rise proportionately. Previous studies in Malaysia using NHMS III data reported that diabetes was most prevalent among Malaysians of Indian origin (37.9 per cent) and among people aged between 45–75 years of age (>20 per cent);5,7 however, it was comparable between genders and geographical locations.7 The incidence of diabetes in Australia was also reported to increase at around 45 years of age and by 2008, was highest among patients aged 75 years and over.10 However, a few years later (2011–12), the age group with the highest incidence of diabetes had decreased to 65–74 years.17 Regarding gender, just more than half (52 per cent) of all diabetic cases (T1DM and T2DM) in Australia occurred among women in 1995,9 while many years later (2011–12), more men in Australia reported having diabetes (4.3 per cent) than women (3.6 per cent).17
Despite the high prevalence of diabetes among people living in Malaysia, the use of drugs to treat diabetes was not as high as expected due to high prevalence of diabetes. It has also been reported that less than one-quarter of patients achieve their target HbA1c level (< 7 per cent),24 which suggests that there may be a large number of people with untreated diabetes in Malaysia or diabetics who do not take appropriate medication.5 Perhaps surprisingly, while the 10 most frequently dispensed drugs in Malaysia included those to treat diabetes,16 in Australia the most frequently dispensed drugs were drugs to treat cardiovascular conditions.17 Despite the fact that there were no anti-diabetic drugs included among the 10 most frequently dispensed drugs in Australia, it is interesting that their use was higher than in Malaysia, at 4.35 DDD/1,000/day, on average.
The two most frequently dispensed drug classes in Malaysia were biguanides and sulfonylureas. In Australia, the most frequently used anti-diabetic drugs were biguanides and insulins. The increased use of metformin in Malaysia indicates (improved) adherence to prescribing guidelines, which recommend metformin as first-line oral medication, particularly for obese individuals.25,26 The introduction of the fixed-dose combination of metformin and sulfonylurea may be associated with improved patient compliance and hence, use.16,26 In Australia, metformin use followed a similar increasing trend during the study period. Thiazolidinedione usage in Malaysia decreased during 2005 and 2006, but then increased in 2007, when pioglitazone was introduced,16 and the use of rosiglitazone almost doubled in 2007 in Malaysia while its use remained constant in Australia.17 With the current controversy surrounding the use of rosiglitazone,27 it is expected that the decreasing trend in Malaysia and Australia is likely to continue.
Surprisingly, the use of insulin in Malaysia decreased by 50 per cent during the study period, from 7.78 (2004) to 3.71 DDD/1,000/day (2008), although there was an encouraging increase of 0.48 DDD/1,000/day between 2007 and 2008. By comparison, despite a decrease from 2004 to 2005, insulin use in Australia increased overall and was substantially higher than in Malaysia.
Due to the progressive failure of insulin secretion, therapy has to be increased over time.28,29 Patients with T2DM who do not achieve optimal glycaemic control with oral anti-diabetic drugs (HbA1c <7.0 per cent) may require insulin therapy, and should start insulin therapy as soon as possible if HbA1c >9.0 per cent and blood glucose levels >15mmol/L.30,31 The early use of insulin in the treatment of T2DM is not without controversy both in terms of micro-vascular and macro-vascular complications.32 However, studies included in the National Institute for Health and Care Excellence (NICE) guidelines suggest that combination treatment with insulin and metformin, or insulin and a sulfonylurea, show significantly lower HbA1ac levels compared to insulin monotherapy.29 Results from clinical trials have led to international management guidelines emphasising the importance of blood glucose control to reduce vascular complications in people with diabetes.33–35
A number of potential barriers to and lower acceptance of insulin use among Malaysian patients have been identified. These include lack of knowledge (e.g., fear of injections, glucose monitoring, patient ignorance, lack of awareness about the importance of diabetes treatment),5,16,36 negative side effects (e.g., insulin-related hypoglycaemia),16,36 patients’ preference (e.g., oral medication, alternative medicines),16,37,38 and cost of treatment.36 The affordability or availability of drugs may also be a factor as it has been reported that essential drugs are expensive in Malaysia and are not available in all areas such as the far-eastern region where the logistics of transporting medicines is challenging.39
Due to the increasing burden of chronic diseases in Malaysia, the Malaysian government has increased the spending on health-related issues; however, under-treatment, under-diagnosis, non-adherence, and the use of traditional medicines may lead to sub-optimal use of anti-diabetic agents. We suggest that a crucial step may have been overlooked: robust screening strategies should be conducted in urban and rural areas, to identify patients at risk of, and suffering from, undiagnosed diabetes. To control, delay, or prevent complications associated with diabetes effective prescribing through targeted training and professional development of healthcare professionals, and patient education on appropriate treatment, must be promoted by the authorities responsible for coordinating services, resources, and facilities.
This study had several limitations. The variability in anti-diabetic medicine use in Malaysia suggests that there may be some problem with sampling procedures, response rates, and hence the quality of the data during the period 2004–2008. Although reports from both countries presented the data in the same unit (DDD/1,000/day), the data sources are very different; Malaysian data are not as comprehensive as Australian data, although this improved over the study period. For example, in Malaysia there were only 32 participating private pharmacies in 2004; this increased to 814 in 2008.16 It is also possible that only essential and accessible sources were included in the collection of data. It is known that Australian reports may underestimate the use of under-co-payment medicines (i.e., non-subsidised medicines, which are therefore not included in the claims databases) by up to 20 per cent.17 Finally, this drug utilisation study is based on reports of dispensing data and the drugs may not necessarily have been consumed.16,17
Conclusion
This comparative study highlights differing prescribing trends between Malaysia and Australia. Although there is an increasing trend in the prevalence of people with diabetes in both countries, the use of drugs to treat diabetes in Malaysia does not reflect the patterns of anti-diabetic drug use in Australia. Insulin is considered to be the most appropriate form of treatment for certain types or stages of diabetes and more research into the low use of insulin in Malaysia is required. It will therefore be necessary to lay a firm foundation for the development of educational interventions, review of treatment guidelines, and education of prescribers and patients to increase the acceptance of insulin therapy. Moreover, effective drug use review to promote rational medicine use should be included in the diabetes management protocol in Malaysia.
Footnotes
PEER REVIEW
Not commissioned. Externally peer reviewed.
CONFLICTS OF INTEREST
The authors declare that they have no competing interests.
Please cite this paper as: Hasan SS, Clavarino AM, Mamun AA, Kairuz T. A comparative drug utilisation study of the treatment of diabetes in Malaysia and Australia. AMJ 2015;8(6):179–188 http//dx.doi.org/10.4066/AMJ.2015.2330
References
- 1.Gallwitz B. Implications of postprandial glucose and weight control in people with type 2 diabetes: understanding and implementing the International Diabetes Federation guidelines. Diabetes Care. 2009;32(2):S322–5. doi: 10.2337/dc09-S331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hu FB. Globalization of diabetes: the role of diet, lifestyle, and genes. Diabetes Care. 2011;34(6):1249–57. doi: 10.2337/dc11-0442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Shaw JE, Sicree RA, Zimmet PZ. Global estimates of the prevalence of diabetes for 2010 and 2030. Diabetes Res Clin Pract. 2010;87:4–14. doi: 10.1016/j.diabres.2009.10.007. [DOI] [PubMed] [Google Scholar]
- 4.United Nations, Population Division, World Population Prospects: The 2006 Revision. United Nations (Ed.). Geneva, 2007 [Google Scholar]
- 5.Letchuman GR, Wan Nazaimoon WM. et al. Prevalence of diabetes in the Malaysian National Health Morbidity Survey III 2006. Med J Malaysia. 2010;65:173–9. [PubMed] [Google Scholar]
- 6.Zaini A. Where is Malaysia in the midst of the Asian epidemic of diabetes mellitus? Diabetes Res Clin Pract. 2000;50:23–8. doi: 10.1016/s0168-8227(00)00175-3. [DOI] [PubMed] [Google Scholar]
- 7.Wan Nazaimoon WM, Md Isa SH, Wan Mohamad WB. et al. Prevalence of diabetes in Malaysia and usefulness of HbA1c as a diagnostic criterion. Diabet Med. 2013;30(7):825–8. doi: 10.1111/dme.12161. [DOI] [PubMed] [Google Scholar]
- 8.Diabetes in Australia Updates [Internet]. [Accessed 2014 Jul 12]. Available from: http://www.diabetesaustralia.com.au/Understanding-Diabetes/Diabetes-in-Australia. [Google Scholar]
- 9.Australian Bureau of Statistics: National Health Survey; Diabetes (1995), cat 4371.0. [Google Scholar]
- 10.Australian Bureau of Statistics: National Health Survey: Summary of Results, 2007–2008 (Reissue), cat, 4364.0 [Google Scholar]
- 11.Australian Bureau of Statistics: Australian Health Survey; Diabetes Mellitus, 2011–12, cat 4364.0.55.001 [Google Scholar]
- 12.Australia Health: Authoritative information and statistics to promote better health and wellbeing [Internet] [Accessed 2013 Oct 08]. Available from: http://www.aihw.gov.au/publication-detail/?id=6442468376. [Google Scholar]
- 13.Schneeweiss S, Avron J. A review of uses of health care utilization databases for epidemiologic research on therapeutics. J Clin Epidemiol. 2005;58:323–7. doi: 10.1016/j.jclinepi.2004.10.012. [DOI] [PubMed] [Google Scholar]
- 14.Dunstan DW, Zimmet PZ, Welborn TA. et al. The rising prevalence of diabetes and impaired glucose tolerance: the Australian Diabetes, Obesity and Lifestyle Study. Diabetes Care. 2002;25(5):829–83. doi: 10.2337/diacare.25.5.829. [DOI] [PubMed] [Google Scholar]
- 15.National Diabetes Service Scheme, Diabetes Australia [Internet]. [Accessed 2014 Jan 21]. Available from: http://ndss.com/au/en/Australian-Diabetes-Map/Map/ [Google Scholar]
- 16.Malaysian statistics on medicine use [Internet]; 2004 to 2008. [Accessed 2014 Jun 01]. Available from: http://www.pharmacy.gov.my/v2/en/documents/malaysian-statistics-medicines.html. [Google Scholar]
- 17.Australian Government Department of Health and Ageing. Australian Statistics on Medicines [Internet]; 1997 to 2008. Available from: http://www.pbs.gov.au/info/browse/statistics. [Google Scholar]
- 18.WHO Collaborating Centre for Drug Statistics Methodology. Guidelines for ATC Classification and DDD Assignment 2009. [Google Scholar]
- 19.Australian Government Department of Health and Ageing 2004. Australian Statistics on Medicines 2001–2002. Canberra: Australian Government Publishing Service [Google Scholar]
- 20.Nordic Council on Medicines. Nordic Statistics on Medicines 1987–1989. NLN publication number 3, Uppsala, Sweden, 1990. [Google Scholar]
- 21.Australian Bureau of Statistics: Australian Demographic Statistics (2011), cat 3101.0 [Google Scholar]
- 22.Department of Statistics Malaysia: Malaysian Demographics Statistics [Internet]. [Accessed 2014 Jan 21]. Available from: http://www.statistics.gov.my/portal/index.php?option=com_content&id=1215&Itemid=89&lang=en. [Google Scholar]
- 23.Institute for Public Health (IPH) 2011. National Health and Morbidity Survey 2011 (NHMS 2011) Vol. II: Non-Communicable Diseases. 2011 188 Pages. [Google Scholar]
- 24.Mafauzy M, Hussein Z, Chan SP. The stauts of diabetes control in Malaysia: results of DiabCare 2008. Med J Malaysia. 2011;66(3):175–81. [PubMed] [Google Scholar]
- 25.International Diabetes Federation. Diabetes Atlas Third Edition. Brussels: IDF [Internet]. [Accessed 2013 Nov 10]. Available from: http://www.euphix.org/object_document/o4858n27165.html. [Google Scholar]
- 26.Clinical Practice Guidelines Task Force. Clinical Practice Guidelines Management of Type 2 Diabetes Mellitus (3rd Edition). Ministry of Health Malaysia 2004 [Google Scholar]
- 27.Nissen SE, Reed R, Wolski K. Effect of rosiglitazone on the risk of myocardial infaction and death from cardiovascular causes. N Engl J Med. 2007;356:2457–71. doi: 10.1056/NEJMoa072761. [DOI] [PubMed] [Google Scholar]
- 28.DeWitt DE, Dugdale DC. Using new insulin strategies in the outpatient treatment of diabetes: clinical applications. JAMA. 2003;289(17):2265–9. doi: 10.1001/jama.289.17.2265. [DOI] [PubMed] [Google Scholar]
- 29.The National Collaborating Centre for Chronic Conditions. Type 2 diabetes: National clinical guideline for management in primary and secondary care (updated NICE guidelines-2008) [Google Scholar]
- 30.Macisaac RJ, Jerums G, Weekes AJ. et al. Patterns of glycaemic control in Australian primary care (NEFRON 8). Intern Med J. 2009;39:512–8. doi: 10.1111/j.1445-5994.2008.01821.x. [DOI] [PubMed] [Google Scholar]
- 31.Deed G, Barlow J, Kuo I. Early and tight glycaemic control: the key to managing type 2 diabetes. Aust Fam Physician. 2012;41(9):681–684. [PubMed] [Google Scholar]
- 32.Chiasson JL. Early insulin use in type 2 diabetes. Diabetes Care. 2009;32(2):S270–4. doi: 10.2337/dc09-S321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.International diabetes federation: clinical guidelines task force (2005). Global guideline for type 2 diabetes. [Accessed 2014 Jan 21]. Available from: http://www.idf.org/webdata/docs/IDF%20GGT2D.pdf. [Google Scholar]
- 34.Stratton IM, Adler AI, Neil HA. et al. Association of glycaemic with macrovascular and microvascular complications of type 2 diabetes (UKPDS 35): prospective observational study. BMJ. 2000;321(7258):405–12. doi: 10.1136/bmj.321.7258.405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.UK Prospective Diabetes Study (UKPDS) Group. Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33) Lancet. 1998;352:837–53. [PubMed] [Google Scholar]
- 36.Lee YK, Ng CJ, Lee PY. et al. What are the barriers faced by patients using insulin? A qualitative study of Malaysian health care professionals’ views. Patient Prefer Adherence. 2013;7:103–9. doi: 10.2147/PPA.S36791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hasan SS, Ahmed SI, Bukhari NI. et al. Use of complementary and alternative medicine among patients with chronic diseases at outpatient clinics. Complement Ther Clin Pract. 2009;15:152–7. doi: 10.1016/j.ctcp.2009.02.003. [DOI] [PubMed] [Google Scholar]
- 38.Hasan SS, Loon WCW, Ahmadi K. et al. Reasons, perceived efficacy and factors associated with complementary and alternative medicine use among Malaysian patients with diabetes mellitus. British Journal of Diabetes Vascular Disease. 2011;11(2):92–8. [Google Scholar]
- 39.Babar ZUD, Ibrahim MIM, Singh H. et al. Evaluating drug prices, availability, affordability, and price components: Implications for access to drugs in Malaysia. PLoS Med. 2007;4(3):466–75. doi: 10.1371/journal.pmed.0040082. [DOI] [PMC free article] [PubMed] [Google Scholar]


