Abstract
Background
The health care for patients having two or more long-term medical conditions is fragmented between specialists, allied health professionals, and general practitioners (GPs), each keeping separate medical records. There are separate guidelines for each disease, making it difficult for the GP to coordinate care. The TrueBlue model of collaborative care to address key problems in managing patients with multimorbidity in general practice previously reported outcomes on the management of multimorbidities. We report on the care plan for patients with depression, diabetes, and/or coronary heart disease that was embedded in the TrueBlue study.
Methods
A care plan was designed around diabetes, coronary heart disease, and depression management guidelines to prompt implementation of best practices and to provide a single document for information from multiple sources. It was used in the TrueBlue trial undertaken by 400 patients (206 intervention and 194 control) from 11 Australian general practices in regional and metropolitan areas.
Results
Practice nurses and GPs successfully used the care plan to achieve the guideline-recommended checks for almost all patients, and successfully monitored depression scores and risk factors, kept pathology results up to date, and identified patient priorities and goals. Clinical outcomes improved compared with usual care.
Conclusion
The care plan was used successfully to manage and prioritise multimorbidity. Downstream implications include improving efficiency in patient management, and better health outcomes for patients with complex multimorbidities.
Keywords: Multimorbidity, care plans, collaborative care, diabetes, heart disease, depression
What this study adds:
-
What is known about this subject?
Medicare-funded care plans generally fail to deal with multiple diseases, track changes over time, omit personalised goals, miss supporting self-management, and don’t provide specific prompts for recommended checks.
-
What new information is offered in this report?
A care-plan template developed from multiple disease guidelines was successfully used to manage multimorbidity, summarising information from multiple sources and involving patient participation in disease management.
-
What are the implications for research, policy, or practice?
GP practices should consider a combined care-plan approach similar to the plan reported here with its automatic prompts to ensure better adherence to the recommended checks.
Background
Multimorbidity, the co-occurrence of multiple medical conditions in an individual,1 is becoming the norm for older people. One-third of 65-year-olds have three or more chronic conditions.2 Patients with multimorbidity have poorer quality of life, greater loss of physical function, and are prescribed multiple drugs with consequent difficulties with adherence. These patients are more likely to be admitted to and have longer stays in hospital.3 They already form the majority of GP workload in primary care, with more than half of patient encounters dealing with managing chronic conditions,4 and this will increase as the population ages.5,6 Recent articles7,8 have highlighted that it is both timely and important to examine practical ways to better manage the healthcare of patients with multimorbidity.
One difficulty is that treatment guidelines are based on research focussed on single diseases that specifically exclude patients with multimorbidity. This can lead to conflicting management guidelines—such as using non-steroidal anti-inflammatory medication for the treatment of osteoarthritis pain9 while avoiding the same medications in the presence of heart failure10—that do not account for the complexities of living with overlapping medical conditions.3 As a result, patients undergo multiple investigations and find their health care fragmented between multiple specialist clinics, allied health providers, and general practice. The location of these services adds an additional travel burden, especially in rural or regional areas. With the fragmentation of health care, important comorbidities can be missed, such as depression, which is overrepresented and underdiagnosed in patients presenting with other chronic diseases.11 Individual preferences are often overlooked with targets being simply medical ones without the patient’s wishes and lifestyle preferences being considered.
The key question for patients with multimorbidity is how high quality and coordinated care can be achieved in healthcare services in the face of such fragmentation of care.12 The TrueBlue model of collaborative care13–16, in a large, multicentre study undertaken in Australia, provided a means to address this question.
The TrueBlue study
Collaborative care has been recognised as a successful systematic approach to the management of depression.17 The TrueBlue model of collaborative care used the principles of chronic disease management18 that call for timetabled reviews, a single case-manager, new roles for practice nurses, a way to exchange information between all members of the healthcare team, and a combined guideline for type 2 diabetes, coronary heart disease (CHD), and depression. The TrueBlue model is described in detail elsewhere;13,15 a brief description is provided here.
Patients were screened for depression by completing the Patient Health Questionnaire 9 (PHQ-9)19 in the waiting room before attending a 45-minute nurse consultation, followed by a 15-minute GP consultation. In each nurse consultation, pathology results, clinical measurements, and lifestyle risks were documented and referrals to allied health, specialist services, or mental-health workers were arranged. Patient priorities, goal setting, and problem solving were key components of the TrueBlue model. Nurses worked with patients during the consultation to enable them to think about their personal priorities and the barriers to and enablers of better lifestyle choices. Nurses used problem-solving techniques to help patients set personal SMART (specific, measurable, attainable, realistic, and time-bound) goals that patients felt were achievable to assist in reducing their risk factors. Nurses reviewed and updated these goals with patients during each subsequent consultation. GP clinical decisions were based on these patient priorities. Importantly, this entire process was repeated every three months by automatically timetabling recall visits. The costs for the nurse time were covered through Australian Medicare rebates for chronic disease management.
Care plans are known to be important in managing chronic disease20 and lead to improved patient outcomes21 and reduced hospitalisation.22 However, typical Australian GP management plans (GPMPs), such as a suggested blank GPMP template,23 do not report the patient’s wishes and lifestyle preferences, focussing instead on medical targets and management goals, nor do they track the achievement or partial achievement of personal lifestyle goals. Such GPMPs only contain a snapshot of information taken at the time of the consultation and do not track the changes over time that allow progress to be easily reviewed. Many such GPMPs are disease-specific and do not incorporate the varied requirements of multiple diseases that follow multiple guidelines. They do not have built-in prompts that guide the clinician through the various guideline-recommended checks. A new care-plan template was designed to address these issues as part of the TrueBlue study to assist in the management of multimorbidity. We report here on the implementation of that care plan, and provide details of its integration into clinical practice.
Methods
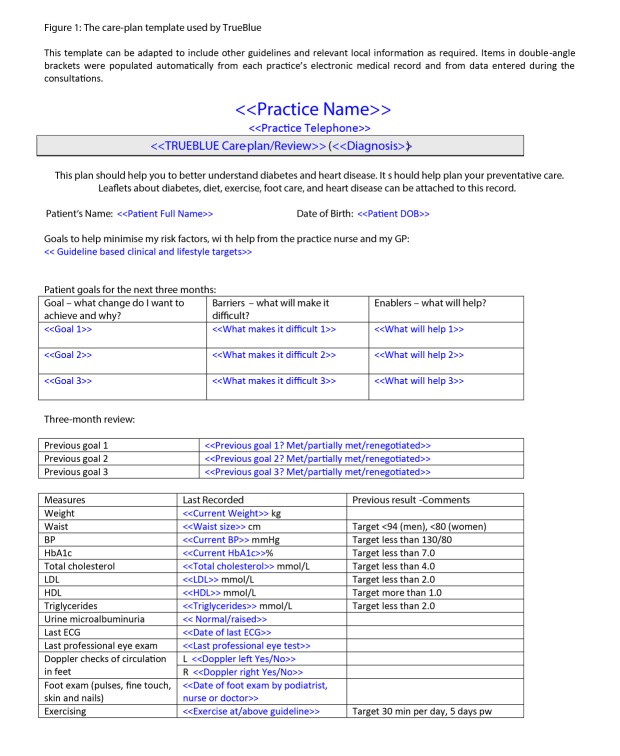
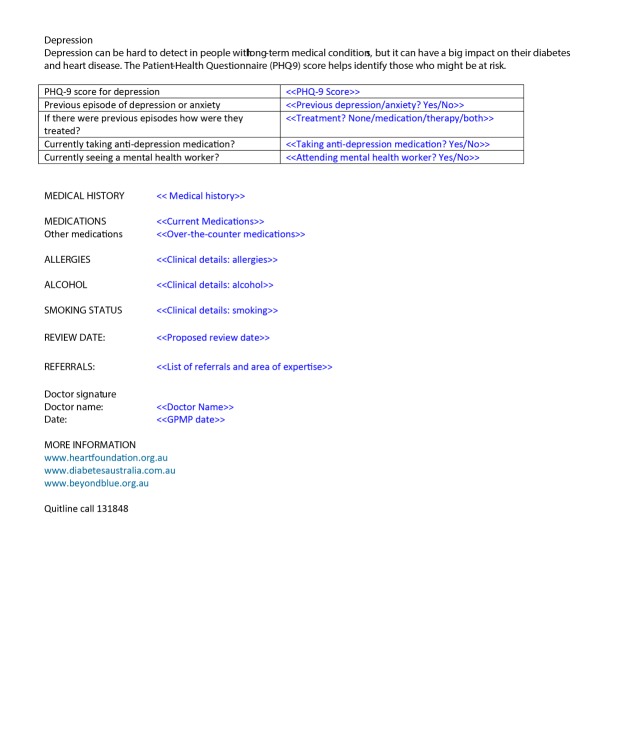
The care-plan template (Figure 1) was specifically developed to acquire all necessary information and provide it in a single document. It was designed around the overlapping management tasks, targets, and lifestyle changes recommended by the National Heart Foundation of Australia, Diabetes Australia, and the MacArthur Foundation for Depression so that it could act as a guide for the clinician through routine scheduling of tests and activities required for each patient.
Figure 1: The care-plan template used by TrueBlue.
The care plan was designed to be capable of summarising clinical data, identifying clinical priorities, recording patient’s personal goals, coordinating the broader healthcare team, and providing de-identified audit data that could be used for research or for feedback to the clinic. It allowed tracking changes over time enabling the clinicians to monitor medication, referrals, adherence to the treatment plan, and attendance at external referrals. The care plan recorded patient’s personal goals and preferences, and the barriers and enablers to achieving these. It allowed depression to be monitored and whether stepped care was occurring through medication management and mental-health worker referrals and attendance. The care plan incorporated an automatic recall visit rather than relying on patients making the next appointment on an ad-hoc basis. Importantly, it incorporated automatic prompts to the health professionals to make sure that all this information was acquired.
The care plan was tested in the D_TECT trial in six rural Australian general practices14 before being used in the TrueBlue randomised trial with usual GP care as a control.15
Results
Four hundred patients (206 in the intervention and 194 in the control) with depression and one or both of diabetes and CHD from 11 general practices in regional and metropolitan settings commenced the TrueBlue trial. Practices ranged from small, single GP practices to large, multi-GP clinics, with five (three intervention, two control) of the practices coming from a regional area and six (two intervention, four control) from a metropolitan area.15 Data collection commenced in 2009 and was completed in 2011. Approximately 72 per cent of patients (142 in the intervention and 147 in the control) completed the study.
Table 1 presents the comparison between the control and intervention groups of the checks recommended by the National Heart Foundation and Diabetes Australia that were included in the combined guideline for CHD, diabetes, and depression management. Near-perfect recording occurred when the care plan was used. The intervention data were those recorded at the end of the 12-month study. The usual-care data from the control group were retrospectively extracted at baseline before their nurses were trained in the TrueBlue model and started using its care plan. Usual-care depression and exercise rates were not available because there was no system for recording exercise rates in usual care and patients were specifically screened for depression as part of their recruitment into the TrueBlue RCT.
Table 1:Comparison between the control and intervention groups for the guideline-recommended checks.
| Control group | TrueBlue | |||||
|---|---|---|---|---|---|---|
| Item recorded | N * | n § | N | n | ||
| Smoking | 114 | 110 | 96% | 142 | 142 | 100% |
| Alcohol | 114 | 42 | 37% | 142 | 107 | 75% |
| Height & weight | 114 | 103 | 90% | 142 | 142 | 100% |
| Blood pressure | 114 | 112 | 0.98 | 142 | 142 | 100% |
| Foot checks | 94 | 34 | 36% | 80 | 80 | 100% |
| Eye checks | 94 | 30 | 32% | 80 | 79 | 99% |
| Renal function | 75 | 64 | 85% | 80 | 80 | 100% |
| Lipids | 114 | 110 | 96% | 142 | 141 | 99% |
| HbA1c | 75 | 67 | 89% | 80 | 80 | 100% |
| Depression† | – | – | – | 142 | 140 | 99% |
| Exercise‡ | – | – | – | 142 | 142 | 100% |
Usual-care depression scores were not available for the control group because patients were screened for depression as part of the recruitment process
Baseline exercise rates were not available for the control group
The total number of patients for whom checks could be performed (N) varies as not all checks were required for patients without diabetes.
n is the number of patients for whom checks were performed
Discussion
The TrueBlue model was successful in its primary aim that patients using its model of care showed a clinically-significant improvement in depression.15 Improved 10-year cardiovascular risk, exercise rates, and referrals to exercise programmes and mental-health workers were also observed. Personal lifestyle goals were set by almost all (96 per cent) of intervention patients. Nurses, GPs, and patients found that the care plan provided a structure for teamwork and communication between the healthcare providers and patients, and the information and prompts within it ensured a comprehensive approach to care16.
The prompts in the care plan ensured that the practice nurses were able to successfully perform the combined-guideline-recommended checks for CHD, diabetes, and depression management, with a near-complete reporting of the recommended checks in the intervention group (Table 1). This contrasts with the reduced level of reporting observed in the usual care undertaken by the control group, especially for eye and foot checks. This may be simply due to control clinics not reporting existing data but our “usual-care” rates are consistent with those reported for blood pressure (93 per cent), renal function (69 per cent), HbA1C (82 per cent), and lipids (90 per cent) observed in a recent study of patients with diabetes24 prior to an audit cycle with training in the management of diabetes.
Rates of depression screening in usual care could not be obtained in the control clinics because their patients were screened and their scores recorded as part of the recruitment phase. However, rates as low as 19 per cent in usual care have been reported.25
Multimorbidity shifts the focus from an index disease to the cumulative combination of many diseases.27 Consequently, patient priorities will be a greater part of the decision-making process. Our care plan ensured that patient priorities and goals were identified for almost all patients.
Care plans can be generated online,26 but there are difficulties because online systems must be general enough to encompass all likely variations in data, leading to complex data entry. Consequently, the care plan used in the TrueBlue study was deliberately incorporated into the letter-writer component of each practice’s clinical software that automatically populated the care plan with existing data from the electronic medical record and additional measures obtained during each patient’s visit. It also generated a table of de-identified data that could be exported to the research team. Automating these tasks made time available to the practice nurses to build therapeutic relationships with their patients.
To allow patients to be more proactive in improving their health, it was important that the care plan be kept short and non-technical with a view to being readable by the patient so that they had an overview of all their medical conditions. However, it was also important that it still remain a useful summary for the patient’s clinical team.
When designing a care plan where multiple guidelines conflict in their advice, GPs will need to use clinical judgement to determine which targets should be followed.5,7 However, a well-constructed care plan developed using clinical judgement can assist GPs to undertake these tasks. GPs will need to use their skills as generalists and their expertise in longitudinal care together with their unique knowledge of each patient’s history to best manage the complexities of multimorbidity.
Several components should be considered when developing the care plan. The following items were found to be necessary to achieve the improvements that were observed in the TrueBlue study:
Multiple guidelines need to be formulated into a single care plan into which practice nurses collate and enter information. GPs will need to use clinical judgement to determine which targets should be followed.
Patient priorities need to be determined and SMART goals developed and written into the care plan to assist GPs to make appropriate clinical decisions. This requires that nurses be trained in effective goal setting and problem solving.
Patient goals and priorities need to be reviewed and updated in the next appointment and the care plan updated.
The care plan should automatically timetable recall visits to ensure ongoing continuity of chronic disease management.
The care plan should assist with case-management tasks by documenting referrals to other healthcare specialists, acting as a communication tool between the healthcare teams, and allowing referrals to be monitored over time.
The care plan should contain automatic prompts so that all recommended checks are performed and data entered into the clinic’s medical records.
The next steps are to extend the care plan and the TrueBlue model of care to cover a broader range of co-existing chronic diseases while still using the practice nurse as case manager and the care plan as the communication tool. Practice nurses will continue to play a central role in collating information from multiple sources and coordinating referrals. The extension of the TrueBlue training package will equip practice nurses to help patients set effective goals and identify priorities. GPs will be assisted with protocols for de-prescribing to reduce the harm from polypharmacy and align medications with identified patient priorities rather than following a range of separate single-disease guidelines. Patients will continue to receive the individualised care plan that provides an overview of all their medical conditions and clearly states their priorities and the steps to be taken to achieve them. Monitoring will be focussed on reducing harms, maintaining function, and achieving the patient’s priority outcomes.
Conclusion
A care plan was designed to contain automatic prompts to ensure that all recommended checks formulated from separate chronic-disease guidelines were performed during the consultation. The care plan was designed to be a patient-readable summary of their medical conditions, while still remaining a suitable summary for the health team of information coming from multiple sources. It involved the participation of patients in the management of their diseases and summarised their priorities. The care plan was used successfully in the management and prioritisation of depression, diabetes, and heart disease during the TrueBlue study.
ACKNOWLEDGEMENTS
The authors wish to thank beyondblue, the National Depression Initiative, for the funding to undertake this study, and the patients, practice nurses, general practitioners, and support staff of the participating clinics in D_TECT (Bordertown Family Medicine, Hamilton Medical Group, Hawkins Medical Clinic, Corangamite Clinic, Warracknabeal Medical Centre, and Robinson St Medical Centre) and TrueBlue (Evans Head Medical Centre, Lennox Head Medical Centre, Keen Street Clinic, Tintenbar Medical Centre, Health on Grange, Warradale Medical Centre, Seaton Medical and Specialist Centre, Woodcroft Medical Centre, and Southcare Medical Centre). We also wish to thank Paresh Dawda and the reviewers for their helpful comments on the manuscript.
Footnotes
PEER REVIEW
Not commissioned. Externally peer reviewed.
CONFLICTS OF INTEREST
The authors declare that they have no competing interests.
FUNDING
Funding was provided by beyondblue, the National Depression Initiative, through grant 172.
ETHICS COMMITTEE APPROVAL
Ethics approval was obtained from Flinders University’s Social and Behavioural Research Ethics Committee, approval number 4164.
Please cite this paper as: Morgan MAJ, Coates MJ, Dunbar JA. Using care plans to better manage multimorbidity. AMJ 2015;8(6): 208–215 http://dx.doi.org/10.4066/AMJ.2015.2377
References
- 1.van den Akker M, Buntinx F. et al. Comorbidity or multimorbidity: what's in a name? A review of literature. Eur J Gen Pract. 1996;2:65–70. [Google Scholar]
- 2.Barnett K, Mercer SW, Norbury M. et al. Epidemiology of multimorbidity and implications for health care, research, and medical education: a cross-sectional study. Lancet. 2012;380:37–43. doi: 10.1016/S0140-6736(12)60240-2. DOI:10.1016/S0140-6736(12)60240-2. [DOI] [PubMed] [Google Scholar]
- 3.Smith SM, Soubhi H, Fortin M. et al. Managing patients with multimorbidity: systematic review of interventions in primary care and community settings. Br Med J. 2012;345:e5205. doi: 10.1136/bmj.e5205. doi: 10.1136/bmj.e5205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Britt H, Miller GC, Charles J. General practice activity in Australia 2009–10. Canberra: AIHW; 2010. General practice series no. 27, 216 p. Cat. no. GEP 27. [Google Scholar]
- 5.Guthrie B, Payne K, Alderson P. et al. Adapting clinical guidelines to take account of multimorbidity. Br Med J. 2012;345:e6341. doi: 10.1136/bmj.e6341. doi: 10.1136/bmj.e6341. [DOI] [PubMed] [Google Scholar]
- 6.Mercer SW, Gunn J, Bower P. et al. Managing patients with mental and physical multimorbidity. Br Med J. 2012;345:e5559. doi: 10.1136/bmj.e5559. doi: 10.1136/bmj.e5559. [DOI] [PubMed] [Google Scholar]
- 7.Roland M, Paddison C. Better management of patients with multimorbidity. Br Med J. 2013;346:f2510. doi: 10.1136/bmj.f2510. doi: 10.1136/bmj.f2510. [DOI] [PubMed] [Google Scholar]
- 8.Harris M, Dennis S, Pillay M. Multimorbidity: negotiating priorities and making progress. Aust Fam Physician. 2013;42(12):850–4. [PubMed] [Google Scholar]
- 9.The Royal Australian College of General Practitioners. Guideline for the non-surgical management of hip and knee osteoarthritis. Melbourne: RACGP; 2009. [cited 2015 June 4]. Available from http://www.racgp.org.au/download/documents/Guidelines/Musculoskeletal/racgp_oa_guideline.pdf. [Google Scholar]
- 10.National Heart Foundation of Australia and Cardiac Society of Australia and New Zealand. Quick reference guide. Diagnosis and management of chronic heart failure. Heart Foundation 2011. [updated 2011 October; cited 2015 June 4]. Available from http://www.heartfoundation.org.au/SiteCollectionDocuments/CHF-QRG-updated-2014.pdf. [Google Scholar]
- 11.Clarke DM, Currie KC. Depression, anxiety and their relationship with chronic diseases: a review of the epidemiology, risk and treatment evidence. Med J Aust. 2009 Apr 6;190(7 Suppl):S54–60. doi: 10.5694/j.1326-5377.2009.tb02471.x. doi: cla10974_fm. [DOI] [PubMed] [Google Scholar]
- 12.Haggerty JL. Ordering the chaos for patients with multimorbidity. Br Med J. 2012;345:e5915. doi: 10.1136/bmj.e5915. doi: 10.1136/bmj.e5915. [DOI] [PubMed] [Google Scholar]
- 13.Morgan M, Dunbar J, Reddy P. et al. The TrueBlue study: Is practice nurse-led collaborative care effective in the management of depression for patients with heart disease or diabetes? BMC Fam Pract. 2009;10:46. doi: 10.1186/1471-2296-10-46. doi: 10.1186/1471-2296-10-46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Morgan MA, Dunbar J, Reddy P. Collaborative care – The role of practice nurses. Aust Fam Physician. 2009 Nov;38(11):925–6. [PubMed] [Google Scholar]
- 15.Morgan MAJ, Coates MJ, Dunbar JA. et al. The TrueBlue model of collaborative care using practice nurses as case managers for depression alongside diabetes or heart disease: a randomised trial. BMJ Open. 2013;3(1):bmjopen2012002171. doi: 10.1136/bmjopen-2012-002171. doi: 10.1136/bmjopen-2012-002171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Schlicht K, Morgan MAJ, Fuller J. et al. Safety and acceptability of practice-nurse-managed care of depression in patients with diabetes or heart disease in the Australian TrueBlue study. BMJ Open. 2013;3:e002195. doi: 10.1136/bmjopen-2012-002195. doi: 10.1136/bmjopen-2012-002195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Archer J, Bower P, Gilbody S. et al. Collaborative care for depression and anxiety problems. Cochrane Database of Systematic Reviews 2012, Issue 10. Art. No. CD006525. doi: 10.1002/14651858.CD006525.pub2. doi: 10.1002/14651858.CD006525.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wagner EH. Chronic disease management: what will it take to improve care for chronic illness? Eff Clin Pract. 1998 Aug-Sep;1(1):2–4. [PubMed] [Google Scholar]
- 19.Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–13. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Blakeman T, Harris M. Enhanced primary care items: their use in diabetes management. Aust Fam Physician [online]. 2001 Dec;30(12):1134–40. [cited 27 Oct 14]; Available from: http://search.informit.com.au/documentSummary;dn=383827242751817;res=IELHEA. [PubMed] [Google Scholar]
- 21.Wickramasinghe LK, Schattner P, Hibbert ME. et al. Impact on diabetes management of General Practice Management Plans, Team Care Arrangements and reviews. Med J Aust. 2013;199(4):261–265. doi: 10.5694/mja13.10161. doi: 10.5694/mja13.10161. [DOI] [PubMed] [Google Scholar]
- 22.Vitry AI, Nguyen TA, Ramsay EN. et al. General practitioner management plans delaying time to next potentially preventable hospitalisation for patients with heart failure. Intern Med J. 2014:1117–23. doi: 10.1111/imj.12512. doi:10.1111/imj.12512. [DOI] [PubMed] [Google Scholar]
- 23.Department of Health. Chronic Disease Management (formerly Enhanced Primary Care) — GP services. Canberra ACT: Australian Government Department of Health; 2014 [updated 2014 April 02; cited 2015 March 24]. Available from: http://www.health.gov.au/internet/main/publishing.nsf/content/95003EE464F100E2CA257BF0001F9F60/$File/PDF. [Google Scholar]
- 24.Barlow J, Krassas G. Improving management of type 2 diabetes – Findings of the Type2Care clinical audit. Aust Fam Physician. 2013 Jan-Feb;42(1/2):57–60. [PubMed] [Google Scholar]
- 25.Wan Q, Harris MF, Jayasinghe UW. et al. Quality of diabetes care and coronary heart disease absolute risk in patients with type 2 diabetes mellitus in Australian general practice. Qual Saf Health Care. 2006;15(2):131–5. doi: 10.1136/qshc.2005.014845. doi: 10.1136/qshc.2005.014845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Jones K, Dunning T, Costa B. et al. The CDM-Net Project: The development, implementation and evaluation of a broadband-based network for managing chronic disease. Int J Family Med. 2012 doi: 10.1155/2012/453450. 2012. doi:10.1155/2012/453450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Newman AB. Comorbidity and Multimorbidity. Newman AB, Cauley JA, editors. The epidemiology of aging. Dordrecht: Springer Science and Business Media; 2012:119–133. doi:10.1007/978-94-007-5061-6_8. [Google Scholar]