Abstract
Background:
Acute exacerbation of chronic obstructive pulmonary disease (AECOPD) is a common cause of hospitalization and mortality. Recent studies have shown the usefulness of eosinopenia in predicting the outcomes of patients admitted to the intensive care unit. This study examined the association of eosinopenia with the outcomes of patients with AECOPD.
Methods:
This is a prospective study. Patients with AECOPD were divided into two cohorts: patients with eosinopenia and those without eosinopenia. Duration of hospitalization, need of mechanical ventilation, in-hospital mortality, rehospitalization, or death within 30 days after discharge were compared between the two cohorts. Eosinopenia was defined as eosinophil count of >40 cells/mm3.
Results:
Among 100 patients with AECOPD, 44 were eosinopenic and 56 were non-eosinopenic. Duration of hospitalization of patients with eosinopenia was 12.38 ± 9.85 days and that of patients without eosinopenia was 7.35 ± 5.68 days (p = 0.001). In all, 16 (36%) patients with eosinopenia and seven (12%) patients without eosinopenia needed mechanical ventilation (p = 0.005). In-hospital mortality rate among eosinopenic and noneosinopenic patients was 37.5% (12/44) and 7.6% (4/56), respectively (p = 0.006). Among 100 patients with AECOPD, 16 died in the hospital. Of these, 12 (27.27%) were eosinopenic and 4 (7.6%) were noneosinopenic (p = 0.006). The mean eosinophil count of patients who died in the hospital (n = 16) was 44.00 cells/ml whereas that of survivors (n = 84) was 107.41 cells/ml (p = 0.022).
Conclusion:
We conclude that a significant relationship exists between eosinopenia and outcomes of patients with AECOPD. Thus, eosinopenia can be a useful, easy-to-measure, and inexpensive biomarker for predicting the prognosis of patients with AECOPD.
Keywords: COPD, eosinopenia, outcome, mortality, duration of hospitalization
INTRODUCTION
Global Initiative for Chronic Obstructive Lung Disease (GOLD) stated that chronic obstructive pulmonary disease (COPD) is the fourth leading cause of death in the world and is going to be the third cause of death by 2020 (1, 2). The American Thoracic Society (ATS) and the European Respiratory Society (ERS)(3) stated that although this disease mainly involves the lungs it has specific systemic complications with increase in systemic inflammatory markers (4, 5).
Acute exacerbations of COPD (AECOPD) has a 10% mortality rate at admission and one third of the patients die within a year after hospitalization (6).
Some biomarkers were studied for prediction of outcomes in AECOPD. However, there is little information about the real relationship between para-clinical markers and clinical outcomes like duration of hospitalization, need to intensive care and mortality (7-9). Some biological and hematological parameters such as copeptin, C-reactive protein (including hs-CRP), and procalcitonin, have been used to determine the prognosis in AECOPD (8, 10). Although these tests helped to find out that COPD is a systemic disease, these tests are not available in every medical centers and require extra-cost.
The simplest test which is usually ordered for every admitted patient is a complete blood count (CBC). In this test eosinophilia is identified as a marker of allergy and parasitic disease, but recently, eosinopenia was showed as a sensitive and specific marker for sepsis in intensive care unit (ICU) patients (11). It is recently used for prediction of prognosis in adult (12) and pediatric (13) ICUs. In addition, there are studies that reported occurrence of eosinopenia after burning or injury which lasts up to a few days (14-16).
In this study, we aimed to evaluate the usefulness of eosinopenia for prediction of outcomes in AECOPD. ❑
MATERIALS AND METHODS
This study was performed in Imam Khomeini hospital of Urmia, Iran. It was approved by ethical committee of Urmia University of Medical Science.
Patients who hospitalized because of AECOPD were enrolled into two cohorts according to admission day CBC, with eosinopenia and without eosinopenia. We excluded the patients who used systemic corticosteroids during the last 30 days, patients with asthma, new infiltration on chest X-ray during hospitalization, heart failure, and other diseases that could change the level of eosinophils.
A physician not in charge of patient's management collected the data and followed the course of treatment and outcomes. Data like sex, age, smoking, white blood cell (WBC) count, pH of arterial blood sample and spirometry were recorded. Outcome parameters such as duration of hospitalization, mechanical ventilation and death in hospital were collected. Discharged patients were followed up by phone after 30 days about poor outcomes (mortality and re-hospitalization.
Data were analyzed by SPSS software (Chicago, version18.USA). T-test is used to compare means. Mortality and re-hospitalization after discharge were compared with using Fisher's exact test. P value less than 0.05 was considered statistically significant.
Eosinopenia was defined as eosinophil count less than 40/mm3 on admission day. COPD diagnosis was based on GOLD criteria (1) and the diagnosis of AECOPD was based on acute increase of dyspnea, cough and sputum, and sputum purulence severe enough to require medical care in hospital (17). ❑
RESULTS
One hundred patients with AECOPD (44 with eosinopenia and 56 without eosinopenia) were evaluated. Table 1 shows characteristics and outcomes of the two groups. There was no significant differences between the two groups for sex, age, current smoking, WBC count, arterial pH, and spirometric data (p value for all variables >0.05).
Table 1.
Comparison of patients with eosinopenia and without eosinopenia.
| Eosinopenic patients n=44 | Noneosinopenic patients n=56 | P value | |
|---|---|---|---|
| Sex Male n (%) Female n (%) |
29 (66%) 15 (34%) |
40 (71%) 16 (29%) |
0.25 |
| Mean age ± SD | 70.04±10.28 | 71.46±10.35 | 0.8 |
| Smoking n (%) | 32 (73%) | 42 (75%) | 0.65 |
| WBC cells/mm3 | 10033.85 ± 906.89 | 8415.35 ± 4212 | 0.06 |
| pH | 7.42± 0.7 | 7.42 ±0.8 | 0.38 |
| FEV1 % of predicted mean± SD | 33.00 ± 17.30 | 41.53 ± 21.65 | 0.21 |
| FVC % of predicted mean± SD | 38.71 ± 20.53 | 43.55 ± 19.10 | 0.84 |
| FEV1/FVC ratio mean± SD | 0.56 ± 0.20 | 0.55 ± 0.18 | 0.60 |
| Outcome variables | |||
| Duration of hospitalization mean ± SD | 12.38 ±9.85 | 7.35± 5.65 | 0.001 |
| Mechanical ventilation n (%) | 16 (36%) | 7 (12%) | 0.005 |
| Death in hospital n (%) | |||
| Discharge from hospital n (%) | 12 (27.27%) | ||
| 32 (72.73%) | 4 (7.6%) | ||
| 52 (92.4%) | 0.006 | ||
| Re-hospitalization among discharged patients n (% of discharged) | 9 of 32 (28%) | 2 of 52 (3.8%) | 0.04 |
WBC= white blood cell, FEV1= Forced Expiratory Volume in one second, FVC= Forced Vital Capacity
There were significant differences in outcomes (death in hospital, need for mechanical ventilation, and duration of hospitalization) between the two cohort groups with p value for all variables less than 0.05).
Within 30 days after discharge, 9 (28%) of 32 discharged eosinopenic group were re-hospitalized for AECOPD and four of them were died, while only two (3.57%) of the patients with normal eosinophil count needed hospitalization again and one of them died (p value: 0.04).
Mean ± SD of eosinophil count in patients that died in hospital (n=16) was 44±35.8 cell/mm3, while in patients discharged alive (n=84) was 107.41± 40.74 cell/mm3, p value of 0.022 (Figure 1). ❑
Figure 1.
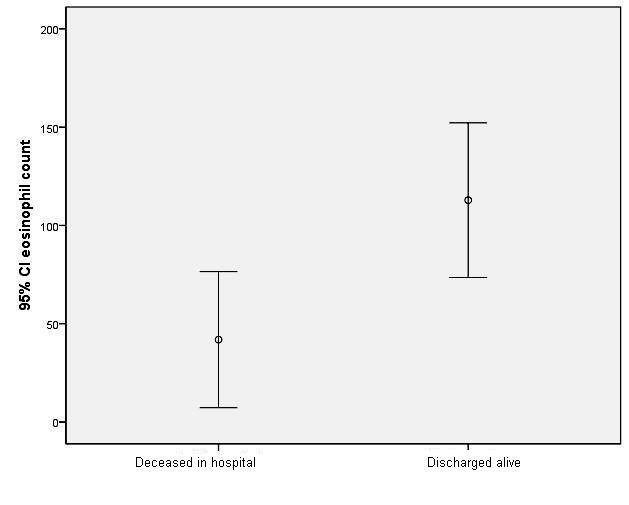
Boxplots showing the mean eosinophil count and comparison between the two grups of patients discharged alive or deceased in hospital.
DISCUSSION
Our findings showed that eosinopenia had a significant relationship with duration of hospitalization, need for mechanical ventilation, and death in the hospital, re-hospitalization and mortality within 30 days after discharge in patients with AECOPD.
Eosinophils consist 0-7% of peripheral blood cells and its production is regulated by granulocyte–macrophage colony-stimulating factor, interleukin-3 and interleukin-5 (18, 19).
Clinicians consider eosinophilia for suspicion of allergic and parasitic disease. Infectious and non-infectious stimuli of acute inflammation markedly suppress eosinophilia. Decrease in eosinophil count during sepsis and inflammatory process is because of destruction of the cells in peripheral tissues, suppression of the migration of mature eosinophils from the bone marrow, localization in inflammatory sites and suppression of formation in bone marrow (19). Eosinopenia also occurs with acute stress, which is mediated by adrenal glucocorticoids and epinephrine (20).
Relation between eosinopenia and poor prognosis and mortality of patients may be related to the presence of bacterial infections, and eosinopenia is a marker of infection.
Abidi et al (12) showed that there was a strong relationship between bacterial infection and eosinopenia in severe patients. They suggested that eosinopenia could differentiate between sepsis and inflammatory response. Others suggested that eosinopenia is more predictive of death than of an infection because it can develop from acute severe stress of infectious or noninfectious, both of which are associated with mortality (13, 21).
Although, some studies like the study of Smithson et al (22) could not find a relation between eosinopenia and infection in intensive care units. Setterberg et al (23) indicated that lack of eosiniphil in the peripheral blood sample could not be a valuable marker of infection.
To our knowledge and search in accessible data bases, only one study by Holland et al (24) evaluated the value of eosinopenia in AECOPD. They studied 65 patients with AECOPD, 42 patients with normal eosinophil count and 23 patients with eosinopenia, and showed a significant relationship between eosinopenia and duration of hospitalization and mortality. They indicated that eosinophil count was an independent marker to determine the severity of disease in patients with AECOPD. However they stated that their study was retrospective and they had no information about receiving corticosteroid, so decrease in eosinophil count could be due to corticosteroids effect. In our prospective study, we excluded the patients that had received systemic corticosteroid, so systemic corticosteroids cannot act as confounding factor. ❑
CONCLUSION
Eosinophil count could be a useful easy-to-measure, inexpensive biomarker to determine the severity and predict the prognosis of patients with acute exacerbation of COPD
CONFLICT OF INTEREST
none declared.
FINANCIAL SUPPORT
This work was supported by a grant from Urmia University of Medical Sciences.
References
- 1.Global initiative for chronic obstructive lung disease (gold): Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease (updated 2014). Available from: http://www.goldcopd.org/uploads/users/files/GOLD_Report2014_Feb07.pdf accessed on 04-June-2014
- 2.Rabe KF, Hurd S, Anzueto A, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: Gold executive summary. Am J Respir Crit Care Med. 2007;176:532–555. doi: 10.1164/rccm.200703-456SO. [DOI] [PubMed] [Google Scholar]
- 3.Celli BR, MacNee W. Standards for the diagnosis and treatment of patients with copd: A summary of the ats/ers position paper. Eur Respir J. 2004;23:932–946. doi: 10.1183/09031936.04.00014304. [DOI] [PubMed] [Google Scholar]
- 4.Wouters EF, Creutzberg EC, Schols AM. Systemic effects in copd. Chest. 2002;121:127S–130S. doi: 10.1378/chest.121.5_suppl.127s. [DOI] [PubMed] [Google Scholar]
- 5.Agusti AG, Noguera A, Sauleda J, et al. Systemic effects of chronic obstructive pulmonary disease. Eur Respir J. 2003;21:347–360. doi: 10.1183/09031936.03.00405703. [DOI] [PubMed] [Google Scholar]
- 6.McCrory DC, Brown C, Gelfand SE, et al. Management of acute exacerbations of copd: A summary and appraisal of published evidence. Chest. 2001;119:1190–1209. doi: 10.1378/chest.119.4.1190. [DOI] [PubMed] [Google Scholar]
- 7.Gompertz S, O'Brien C, Bayley DL, et al. Changes in bronchial inflammation during acute exacerbations of chronic bronchitis. The European respiratory journal: official journal of the European Society for Clinical Respiratory Physiology. 2001;17:1112–1119. doi: 10.1183/09031936.01.99114901. [DOI] [PubMed] [Google Scholar]
- 8.Stolz D, Stulz A, Muller B, et al. Bal neutrophils, serum procalcitonin, and c-reactive protein to predict bacterial infection in the immunocompromised host. Chest. 2007;132:504–514. doi: 10.1378/chest.07-0175. [DOI] [PubMed] [Google Scholar]
- 9.Stolz D, Christ-Crain M, Morgenthaler NG, et al. Copeptin, c-reactive protein, and procalcitonin as prognostic biomarkers in acute exacerbation of copd. Chest. 2007;131:1058–1067. doi: 10.1378/chest.06-2336. [DOI] [PubMed] [Google Scholar]
- 10.Tofan F, Rahimi-Rad MH, Rasmi Y, et al. High sensitive c-reactive protein for prediction of adverse outcome in acute exacerbation of chronic obstructive pulmonary disease. Pneumologia. 2012;61:160–162. [PubMed] [Google Scholar]
- 11.Shaaban H, Daniel S, Sison R, et al. Eosinopenia: Is it a good marker of sepsis in comparison to procalcitonin and c-reactive protein levels for patients admitted to a critical care unit in an urban hospital? Journal of critical care. 2010;25:570–575. doi: 10.1016/j.jcrc.2010.03.002. [DOI] [PubMed] [Google Scholar]
- 12.Abidi K, Belayachi J, Derras Y, et al. Eosinopenia, an early marker of increased mortality in critically ill medical patients. Intensive care medicine. 2011;37:1136–1142. doi: 10.1007/s00134-011-2170-z. [DOI] [PubMed] [Google Scholar]
- 13.Kim YH, Park HB, Kim MJ, et al. Prognostic usefulness of eosinopenia in the pediatric intensive care unit. Journal of Korean medical science. 2013;28:114–119. doi: 10.3346/jkms.2013.28.1.114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hardy JD. The role of the adrenal cortex in the postoperative retention of salt and water. Annals of surgery. 1950;132:189–197. doi: 10.1097/00000658-195008000-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sevitt S. The spleen and blood eosinopenia. Journal of clinical pathology. 1955;8:42–46. doi: 10.1136/jcp.8.1.42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Evans EI, Butterfield WJ. The stress response in the severely burned: An interim report. Annals of surgery. 1951;134:588–613. doi: 10.1097/00000658-195110000-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Anthonisen NR, Manfreda J, Warren CP, et al. Antibiotic therapy in exacerbations of chronic obstructive pulmonary disease. Ann Intern Med. 1987;106:196–204. doi: 10.7326/0003-4819-106-2-196. [DOI] [PubMed] [Google Scholar]
- 18.Hogan SP, Rosenberg HF, Moqbel R, et al. Eosinophils: Biological properties and role in health and disease. Clinical and experimental allergy: journal of the British Society for Allergy and Clinical Immunology. 2008;38:709–750. doi: 10.1111/j.1365-2222.2008.02958.x. [DOI] [PubMed] [Google Scholar]
- 19.Bass DA, Gonwa TA, Szejda P, et al. Eosinopenia of acute infection: Production of eosinopenia by chemotactic factors of acute inflammation. The Journal of clinical investigation. 1980;65:1265–1271. doi: 10.1172/JCI109789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Spreng M. Possible health effects of noise induced cortisol increase. Noise & health. 2000;2:59–64. [PubMed] [Google Scholar]
- 21.Levinson AT, Casserly BP, Levy MM. Reducing mortality in severe sepsis and septic shock. Seminars in respiratory and critical care medicine. 2011;32:195–205. doi: 10.1055/s-0031-1275532. [DOI] [PubMed] [Google Scholar]
- 22.Smithson A, Perello R, Nicolas JM. Is eosinopenia a reliable marker of sepsis? Critical care. 2009;13:409–409. doi: 10.1186/cc7877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Setterberg MJ, Newman W, Potti A, et al. Utility of eosinophil count as predictor of bacteremia. Clinical infectious diseases: an official publication of the Infectious Diseases Society of America. 2004;38:460–461. doi: 10.1086/380846. [DOI] [PubMed] [Google Scholar]
- 24.Holland M, Alkhalil M, Chandromouli S, et al. Eosinopenia as a marker of mortality and length of stay in patients admitted with exacerbations of chronic obstructive pulmonary disease. Respirology. 2010;15:165–167. doi: 10.1111/j.1440-1843.2009.01651.x. [DOI] [PubMed] [Google Scholar]


