Abstract
Primary breast lymphoma (PBL) is a rare entity accounting for less than 1% of all breast malignancies. Diagnostic criteria for primary Hodgkin's lymphoma of the breast are: the presence of sufficient tissue for diagnosis, close interaction between mammary tissue and lymphomatous infiltrate and no evidence or prior diagnosis of widespread lymphoma. Our case illustrates an unusual presentation of Hodgkin's lymphoma of the breast: clinically as inflammatory breast cancer and core biopsy as granulomatous mastitis, the final diagnosis requiring surgical biopsy. Current information regarding this entity is scant, mainly build upon its rarity. In this paper we assess the clinical presentation, the step-by-step diagnosis, the treatment and the importance of immunohistochemistry in this uncommon condition.
Keywords: primary breast lymphoma, extranodal Hodgkin's lymphoma, immunohistochemistry
INTRODUCTION
Primary breast lymphoma (PBL) is a rare entity accounting for 1.7-2.2% of extranodal lymphomas and 0.4-0.5% of breast malignancies (1). More than 70% of PBL are of B- cell lineage (2,3). The definition of PBL comprises only tumors being in stage I (lymphoma limited to the breast) and stage II (lymphoma limited to the breast and axillary lymph nodes) and not tumors originating from non-breast sites. Wiseman and Liao (4) proposed several criteria, before making a diagnosis of primary malignant lymphoma of the breast. These include proper pathological samples, close association of mammary tissue and lymphomatous infiltrate and absence of disseminated lymphoma at the time of diagnosis. Also the presence of ipsilateral axillary nodes is acceptable if they occur simultaneously with the primary lesion.
Breast involvement in Hodgkin's lymphoma is extremely rare, with primary breast Hodgkin's lymphoma even rarer. A primary breast Hodgkin's lymphoma involving the axilla has a very low incidence (0.04%-0.5%) and a good prognosis despite its clinical and pathological features (5). We report an interesting case of primary Hodgkin's lymphoma of the breast presenting as a left breast mass with posterior and axillary extensions. ❑
CASE REPORT
A 54-year-old woman was referred to our hospital in July 2014 for two painful, solid, nodular left breast lesions, measuring 4x3 and 2x1 cm. This patient describes one month history of these lesions. Clinical examination revealed inflammation and ulceration of the overlying skin, "peau d'orange" changes, diffuse axillary erythema and enlarged axillary lymph nodes (Figure 1).
Figure 1.

Clinical picture with two mamelonated breast lumps with enlarged lymph nodes extending to the axilla. Note the edematous and erythematous overlying skin suggesting a preliminary diagnosis of inflammatory breast cancer.
The thoracic CT scan revealed that the skin lumps were part of a left 5x4 cm breast mass with adjacent left axillary lymphadenopathy. Standard blood results were within normal limits, excepting mild elevated WBC. CEA and CA 15-3 were measured and proved to be within normal limits.
The patient was scheduled for a core biopsy which proved to be inconclusive. However, the paraffin embedded tissue revealed a marked inflammatory granulomatous reaction with lymphocytes, plasma cells, neutrophils, epithelioid histiocytes, multinucleated giant cells, necrotic debris and marked cytological atypia, consistent with granulomatous mastitis, although it couldn't completely exclude a malignant origin.
Based on these findings the patient received anti-inflammatory medication for two weeks and later she was scheduled for lumpectomy with axillary lymphadenectomy.
The gross specimen was a tissue fragment of 12x8.8x7.4 cm with overlying skin flap measuring 12x7.5x0.6 cm. The nodules originally described on clinical examination were 4.5/6/4.6 cm and 1.4/1.8/3.3 and at 1,6 cm from one another. On cut section we discovered a heterogeneous, gray-white, non-encapsulated mass, with hemorrhagic and necrotic areas and focal fibrous areas. Ill-defined margins of the tumor invaded the deep surgical resection limit. Microscopic examination of the breast showed a nodular lymphoid malignant proliferation that infiltrates the overlying skin and the adjacent mammary tissue (lateral and deep into the superficial fibers of the pectoralis major muscle). The background showed prominent broad fibroblast-poor collagen bands that separated the lymphoid tissue into nodules consistent with the nodular sclerosis – variant of classic Hodgkin's lymphoma.
The normal architecture of the breast was replaced by a mixed population of small-medium lymphocytes with scant basophilic cytoplasm, round nuclei and conspicuous nucleoli. We also observed a mixed proliferation of eosinophiles, plasma cells, giant pleomorphic Reed-Sternberg cells (Figure 2), pop-corn-like cells, Hodgkin cells and anaplastic multinucleated giant cells.
Figure 2.
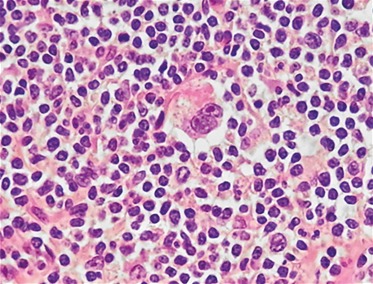
Lacunar Reed-Sternberg cell with bilobed nucleus and prominent eosinophilic nucleoli (center) and numerous Hodgkin cells. (lower left) H.E. 20X.
Immunohistochemical investigations were performed to assess the phenotype and provide a definitive diagnosis. Antibody suppliers and used dilutions are summarized in Table 1. The neoplastic cells showed positivity for CD 30 (Figure 3), CD 15 and weak positivity for PAX 5. Paraffin section immunostaining for CD20/L26 and CD 3 proved negative. The small reactive lymphocytes showed positivity for PAX 5, CD20/L26 and CD3 in rosettes around tumoral cells. The postoperative recovery was uneventful and the patient was referred to the Department of Haematology for further treatment. ❑
Table 1.
Antibodies used in the present study.
| Antibody specificity | Clone | Antibody supplier | Dilution (in 200μl) |
|---|---|---|---|
| PAX 5 | Mouse monoclonal | Biocare | 1:50 |
| CD30 (KI-1) | Mouse monoclonal | Biocare | 1:250 |
| CD15 (cocktail MMA+BY87 | Mouse monoclonal | Biocare | 1:100 |
| CD20 (Ab-1; L-26) | Mouse monoclonal | Biocare | 1:75 |
| CD3 (EP 41) | Mouse monoclonal | Biocare | 1:59 |
Figure 3.
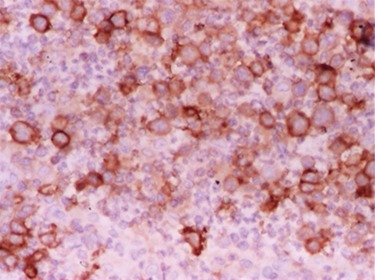
Strong CD30 membrane positivity in Reed– Sternberg cells. Anti-CD30/ peroxidase conjugate and DAB chromogen, 20X.
DISCUSSION
Primary Hodgkin's lymphoma of the breast is a rare neoplasm, while secondary breast involvement with diffuse disease is more common, thus a differential diagnosis is mandatory. The most important factors in assessing primary or secondary breast lymphomas are close association between mammary tissue and lymphocytic infiltrate and no history of widespread lymphoma. Key aspects in diagnosing PBL are computerized tomographic scans - thoracic and abdominal - as well as patient history and past hematologic investigations (5).
Another important clinical differential diagnosis of PBL is with inflammatory invasive breast carcinoma, as presented in our case, because of their similar mammographic appearance, aside from a possible infiltrative margin in breast carcinoma, thus being difficult to diagnose (6). Our differential diagnosis also included granulomatous mastitis and pseudolymphoma based on clinical presentation, macroscopic appearance and excisional biopsy. The first suspicion was perpetuated by the marked inflammatory reaction.
Hodgkin's lymphoma is rarely found in the breast (7). Mammary infiltration is often the result of direct extension from axillary or mediastinal lymph nodes (8,9), part of regional disease with discontinuous axillary node involvement (10,11) or a manifestation of systemic disease (12). Wood and Coltman reviewed 354 reported cases of extranodal Hodgkin's lymphomas published prior to 1973, and found eight that also involved the breast (13). Most patients were women and almost all ultimately developed systemic disease. Recurrent Hodgkin's lymphomas presenting as a breast mass have also been reported (14,15). In one series of cases, 4 women with recurrent tumor limited to the breast were found amongst 2365 patients with Hodgkin's disease (16). Two other patients had breast lesions at the time of diagnosis. Nodular sclerosis and mixed cellularity variants of Hodgkin's disease were reported in the breast (17).
Because the extensive surgical treatment may delay chemotherapy, it is not indicated as first line of therapy for PBL (18). For this reason, a correct diagnosis is critical. Unfortunately, in our case the core biopsy was inconclusive and surgical approach was requested. A combination of CHOP chemotherapy (cyclophosphamid, doxorubicin, vincristine and prednisolone) and field radiotherapy is considered the best treatment for Hodgkin's lymphoma regardless of primary site of presentation (19,20,21). Rituximab, which is a monoclonal antibody against CD20, is not commonly used to treat Hodgkin's lymphoma due to the lack of CD20 surface antigens in most cases (22,23). The precise diagnosis in mandatory, underlying the critical role of the pathologist due to the fact that the chemotherapy regimens for PBL and breast cancer are different. ❑
CONCLUSION
Primary lymphoma of the breast appears to be a rare disease and primary Hodgkin's lymphoma is even rarer. Few clinical, pathological, therapeutic and prognostic features of the disease have been discussed in previous studies mainly because of the rarity of this tumor. Because the PBL benefits mostly from chemotherapy and radiation with surgery as a secondary role, the correct diagnosis is critical. This report presents a challenging case of primary Breast Hodgkin's lymphoma masquerading an inflammatory breast cancer and granulomatous mastitis. Surgical biopsy and immuno histochemistry guided diagnosis and allowed further treatment, improving the prognosis of this patient.
ACKNOWLEDGMENTS
We would like to thank Dr. Gabriel Becheanu and Dr. Ana-Maria Pop for providing us the IHC images for this case.
CONFLICT OF INTEREST
none declared.
FINANCIAL SUPPORT
This paper is partly supported by the Sectorial Operational Programme Human Resources Development (SOPHRD), financed by the European Social Fund and the Romanian Government under contract number POSDRU 141531.
References
- 1.Park YH, Kim SH, Choi SJ, et al. Primary malignant lymphoma of the breast: clinicopathological study of nine cases. Leuk Lymphoma. 2004;45:327–30. doi: 10.1080/10428190310001597892. [DOI] [PubMed] [Google Scholar]
- 2.Liu MT, Hsieh CY, Wang AY, et al. Primary breast lymphoma: a pooled analysis of prognostic factors and survival in 93 cases. Ann Saudi Med. 2005;25:288–93. doi: 10.5144/0256-4947.2005.288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ryan G, Martinelli G, Kuper-Hommel M, et al. Primary diffuse large B-cell lymphoma of the breast: Prognostic factors and outcomes of a study by the International Extranodal Lymphoma Study Group. Ann Oncol. 2008;19:233–41. doi: 10.1093/annonc/mdm471. [DOI] [PubMed] [Google Scholar]
- 4.Wiseman C, Liao KT. Primary lymphoma of the breast. Cancer. 1972;29:1705–12. doi: 10.1002/1097-0142(197206)29:6<1705::aid-cncr2820290640>3.0.co;2-i. [DOI] [PubMed] [Google Scholar]
- 5.Gualco G, Bacchi CE. B cell and T-cell lymphomas of the breast: clinical-pathological features of 53 cases. Int Surg Pathol. 2008;16:407–13. doi: 10.1177/1066896908316784. [DOI] [PubMed] [Google Scholar]
- 6.Jennings WC, Baker RS, Murray SS, et al. Primary breast lymphoma: the role of mastectomy and the importance of lymph node status. Ann Surg. 2007;245:784–9. doi: 10.1097/01.sla.0000254418.90192.59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lin Y, Guo XM, Shen KW, et al. Primary breast lymphoma: long-term treatment outcome and prognosis. Leuk Lymphoma. 2006;47:2102–9. doi: 10.1080/10428190600679064. [DOI] [PubMed] [Google Scholar]
- 8.Shehata WM, Pauke TW, Schleuter JA. Hodgkin's disease of the breast. A case report and review of the literature. Breast. 1985;11:19–21. [Google Scholar]
- 9.Schouten JT, Weese JL, Carbone PP. Lymphoma of the breast. Ann Surg. 1981;194:749–753. doi: 10.1097/00000658-198112000-00015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Meis JM, Butler JJ, Osborne BM. Hodgkin's disease involving the breast and chest wall. Cancer. 1986;57:1859–1865. doi: 10.1002/1097-0142(19860501)57:9<1859::aid-cncr2820570927>3.0.co;2-o. [DOI] [PubMed] [Google Scholar]
- 11.Corrigan C, Sewell C, Martin A. Recurrent Hodgkin's disease in the breast. Diagnosis of a case by fine needle aspiration and immunocytochemistry. ActaCytol. 1990;34:669–672. [PubMed] [Google Scholar]
- 12.Rosen PP, Hoda SA, Brogi E, et al. Wolters Kluwer Health/Lippincott Williams & Wilkins; Philadelphia: 2014. Rosen's breast pathology, Fourth edition; pp. 975–976. [Google Scholar]
- 13.Wood NL, Coltman CA Jr. Localized primary extranodal Hodgkin's disease. Ann Intern Med. 1973;78:113–118. doi: 10.7326/0003-4819-78-1-113. [DOI] [PubMed] [Google Scholar]
- 14.Duman BB, Sahin B, Guvenç B, et al. Lymphoma of the breast in a male patient. Med Oncol. 2011;28:490–3. doi: 10.1007/s12032-010-9675-0. [DOI] [PubMed] [Google Scholar]
- 15.La Mantia E, Cantile M, Liguori G, et al. Breast systemic follicular lymphoma in a man: a case report. J Med Case Rep. 2012;6:217–217. doi: 10.1186/1752-1947-6-217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Talwalkar SS, Miranda RN, Valbuena JR, et al. Lymphomas involving the breast: a study of 106 cases comparing localized and disseminated neoplasms. Am J SurgPathol. 2008;32:1299–309. doi: 10.1097/PAS.0b013e318165eb50. [DOI] [PubMed] [Google Scholar]
- 17.Shao YB, Sun XF, He YN, et al. Clinicopathological features of thirty patients with primary breast lymphoma and review of the literature. Med Oncol. 2015 Feb;32(2):448–448. doi: 10.1007/s12032-014-0448-z. [DOI] [PubMed] [Google Scholar]
- 18.Radkani P, Joshi D, Paramo JC1, et al. Primary breast lymphoma: 30 years of experience with diagnosis and treatment at a single medical center. JAMA Surg. 2014 Jan;149(1):91–3. doi: 10.1001/jamasurg.2013.2283. [DOI] [PubMed] [Google Scholar]
- 19.Horning SG, Weller E, Kim K, et al. Chemotherapy with or without radiotherapy in limited stage diffuse aggressive non-Hodgkin's lymphoma: Eastern Cooperative Oncology Group Study 1484. J ClinOncol. 2004;22:3032–8. doi: 10.1200/JCO.2004.06.088. [DOI] [PubMed] [Google Scholar]
- 20.Pfreundschuh M, Trumper L, Osterborg A, et al. CHOP-like chemotherapy plus rituximab versus CHOP-like chemotherapy alone in young patients with good-prognosis diffuse large B-cell lymphoma: a randomised controlled trial by the MabThera International Trial (MInT) Group. Lancet Oncol. 2006;7:379–91. doi: 10.1016/S1470-2045(06)70664-7. [DOI] [PubMed] [Google Scholar]
- 21.Yarhold JR, Jelliffee AM, Hudson V, et al. The response of treatment of nodular sclerosing Hodgkin's disease with extranodal involvement. Clin Radiol. 1982;33:141–144. doi: 10.1016/s0009-9260(82)80038-x. [DOI] [PubMed] [Google Scholar]
- 22.Saini KS, Azim HA, Cocorocchio E, et al. Rituximab in Hodgkin lymphoma: Is the target always a hit? Cancer Treat Rev. 2011;37:385–90. doi: 10.1016/j.ctrv.2010.11.005. [DOI] [PubMed] [Google Scholar]
- 23.Hosein PJ, Maragulia JC, Salzberg MP, et al. A multicentre study of primary breast diffuse large B-cell lymphoma in the rituximab era. Br J Haematol. 2014;165:358–63. doi: 10.1111/bjh.12753. [DOI] [PMC free article] [PubMed] [Google Scholar]


