Abstract
Introduction:
Negative-pressure wound therapy is a therapeutic technique that uses a vacuum dressing in order to promote healing in acute or chronic wounds. The continued vacuum draws out fluid from the wound and increases blood flow to the area.
The aim of this study was to establish the effectiveness of negative pressure therapy increasing this way the chances of rehabilitation after knee prosthesis infections.
Material and method:
11 patients with septic complications after total knee joint replacement were involved into this study, from the Department of Orthopaedic and Traumatology of Bucharest Emergency University Hospital. In all of the cases negative pressure wound treatment was applied. The surgical approach was chosen according to the surgeon's preferences or along the pre-existing surgical approach.
Results and discussions:
Time from the knee arthroplasty to the clinical and biological manifestation of septic complications was about 35 days with limits between 21 and 42 days. In most cases we managed to keep the implant, the outcome obviously being conditioned by using the negative pressure. Knee infections are still a hazardous problem in orthopedic surgery. Negative-pressure system increased the granulation tissue formation and the local blood flow and enhanced the bacterial clearance function.
Conclusions:
The clinical outcome in our cases indicates that the Negative-Pressure Wound Therapy can be a valuable contribution to the treatment of knee joint infections.
Keywords: vacuum-assisted closure, negative-pressure wound therapy, infection, knee prosthesis
INTRODUCTION
Negative pressure wound therapy (NPWT) or Vacuum-assisted Closure (VAC) has become a widely applied treatment of simple or complex soft tissue defects, either in acute or chronic conditions (1,2). One of the most unlikely complications of joint replacements in Orthopedics is the septic evolution which remains a major challenge for surgeons. The use of negative pressure therapy aims to improve wound management of infected and dehisced wounds after joint replacements. One of the main advantages of NPWT is that it doesn't require daily dressings, which can be uncomfortable for some patients.
The main two physiological mechanisms which occurs during NPWT is: decrease of edema with fluid removal and the removal of soluble inflammatory molecules which may affect the healing process (3,4). Chen et al in an experimental study showed that NPWT not only decreases edema but induces angiogenesis, and blood flow in the affected wound, which explains the dramatic response to this therapy in diseases like diabetes or venous ulcer in which microcirculation is affected (5).
The aim of our study was to present the dramatic outcome of NPWT after joint replacements surgery, offering new possibilities in treatment for septic complications in orthopedics. ❑
MATERIAL AND METHOD
11 patients were treated, between 2010-2013, in the Orthopedic Department of Bucharest Emergency University Hospital with a history of knee replacements, complicated with septic evolution at an interval of 21-42 days postoperatively which manifested in dehisced wound or implant exposure. Near routine laboratory examination, inflammatory markers like C-reactive protein, erythrocyte sedimentation rate, white blood cells and fibrinogen were collected for all patients. Before the application of NPWT every patient underwent mechanical and chemical debridement of the wound with antiseptic solutions like hydrogen peroxide solution and povidone iodine.
In the large skin defects that couldn't be closed in the first attempt the procedure supposed the use of high cellularity sponges that were inserted in the wound margins after being shaped to a correct size (Figure 1), which blocks the penetration of the devitalized tissue and blood clots in the vacuum system of the device. The entire area surrounding the surgical wound was covered with adhesive foil which delimits the aspiration area strictly to the level of the defect. Wounds, which were prepared with surgical and chemical debridement and had achieved primary suture were covered with several layers of a particular gauze soaked in saline and only after then was applied the isolating wound foil. Above this foil was installed the drainage connected to the vacuum system which created negative pressure (Figure 2). ❑
Figure 1.

A Skin defect, exposing the patella; B High cellularity sponges.
Figure 2.

Negative pressure therapy.
RESULTS
The average interval, elapsed since joint replacement surgery to onset of sepsis, was 35 days with limits between 21 and 42 days. Sex ratio was: 7 males and 4 females, age between 25 and 78 years old.
9 patients out of 11 showed a good biological status without severe associated pathologies. The other 2 patients aged 71 and 76 years old respectively presented associated severe pathologies disease including diabetes and chronic venous insufficiency. The result of laboratory tests showed elevated markers of inflammation for all of patients and significantly higher in the two older patients with associated pathology. In 6 cases, the patients underwent primary arthroplasty for osteoarthritis of the knee. In 3 cases of bone tumor, reconstruction was achieved using modular prosthesis. In 2 cases, the patients underwent revision surgery of the primary implant. Average negative pressure was -125 mmHg, this therapy being applied immediately after the draining surgical intervention. The average duration of NPWT was 12.6 (SD ±3.80) days with a range between 6 and 18 days. In all patients, preoperative fluid samples were collected from the wound and from the infected tissue area, which were sent to microbiological exam for culture and antibiotic sensitivity.
In 5 cases with primary knee implant and positive microbiological results, healing was achieved after rigorous surgical and chemical debridement, specific antibiotic therapy followed by negative pressure therapy. In these 5 cases the removal of the prosthetic implants was not necessary (Figure 3). In the other 6 cases, due to the late diagnosis and the presence of an active fistula, the removal of the prosthesis was necessary in order to treat the infection.
Figure 3.

6 weeks follow-up aspect, after NPWT.
In 2 cases with modular prosthesis reconstruction after segmental resection with late septic manifestation (5-7 years) postoperatively, healing was achieved after debridement of the wound followed by negative pressure therapy (Figures 4). In the 3rd case of tumor prosthesis reconstruction with early sepsis, prosthesis had to be removed and temporarily replaced with an orthopedic antibiotic-impregnated cemented spacer was necessary (Figure 5).
Figure 4.
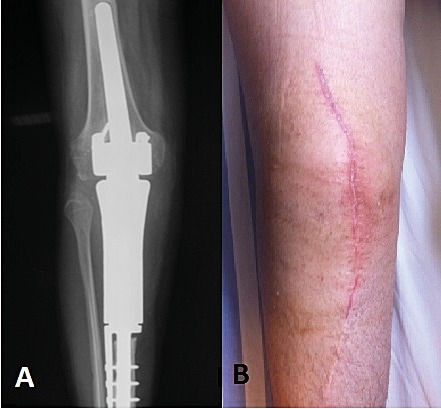
A. Modular knee prosthesis; B. 6 weeks follow-up.
Figure 5.
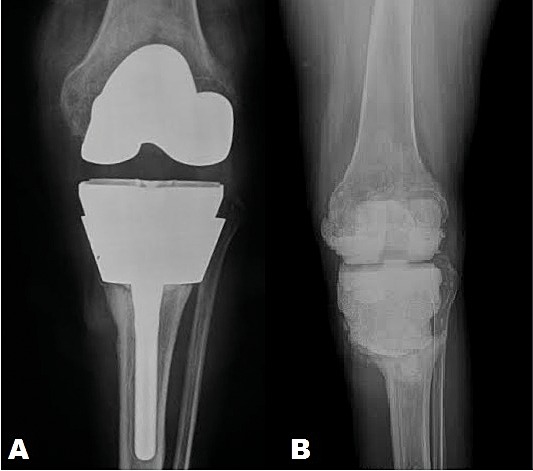
A. X-ray showing prosthetic implant with septic loosening of the components; B. X-ray after implant removal showing an antibiotic impregnated cement spacer.
In the 2 cases of revision arthroplasty, patients developed postoperative hematomas, due to the curative anticoagulant therapy for cardiac diseases. The microbiological results of the infected tissue samples confirmed the presence of Staphylococcus Aureus. In both cases, specific surgical maneuvers were performed followed by NPWT. ❑
DISCUSSION
Negative pressure wound therapy has proven to be highly effective in septic complications of knee replacements surgery with hospital and, in some extreme conditions, home applicability. One of the major advantages of this technique is that it replaces the 2-3 usual dressings per day for complex wounds, which sometimes are painful and uncomfortable for the patient, with a dressing for every 3-4 days (6-8). Microscopic studies showed that the collagen fiber orientation after NPWT is more physiological than in normal wound therapy with daily dressing. Several studies showed that the main efficacy of NPWT is the mechanical effect, which reduces the edema, changes the biological pressure in the infected tissue and reduces inflammatory cytokines. It reduces the number of bacteria and stimulates angiogenesis with the activation of vascular endothelial growth factor (VEGF) (9). A recent experimental study on rats by Li XQ et al showed that in diabetic conditions angiogenesis is promoted by the use of NPWT with an increase of Angiopoietin 1 (Ang-1) and a decrease of Angiopoietin 2 (Ang-2) in the affected area as an inhibitor of Ang-1 (10). These physiological changes in NPWT may be the explanation of the dramatic outcome of contaminated skin damages, diabetes and chronic venous insufficiency. Another interesting recent study by Zhu J. et a showed that continuous suction at -125 mmHg promote fracture healing, inducing bone formation and reducing bone resorption, by the induce of periosteum-derived mesenchymal stem cells (P-MSCs)in the negative pressure area (11). This may explain the good results of NPWT in the treatment of open fractures and also in maintaining the stability of orthopedic implants in septic complications.
However this procedure of wound treatment has been widely applied in different surgical specialties, the selection of patients for the application of negative pressure therapy should be carefully made, paying attention at the followings:
Tolerability of pain in order to make 2-3 dressings a week
Wound position to perform wound debridement and proper insulation
Mental and cognitive status of the patient to accept the device and mobilization with precautions
The procedure is counter-indicated in patients with coagulopathies to exclude the risk of bleeding (12,13).
One of the main complications of NPWT is bleeding which can be severe in cases of vascular grafts and anticoagulant therapy. There are some cases reported in the literature with the worsening of infection (14). If a vacuum cannot be developed due to skin and tissue lesions or necrosis, and then the Negative-pressure wound therapy should not be used for infection management of the underlying implant.
The creation of a therapy concept is essential with respect to the treatment strategies of septic surgery and the causes of the infection. These circumstances led to application of guidelines in order to the correct use of NPWT (15).
Our study was in line with the main findings of other research papers and highlights the good outcome of wound healing with NPWT in orthopedic infections in patients with other associated diseases like diabetes, chronic venous insufficiency, etc. ❑
CONCLUSION
NPWT can be used to treat both early and late infected wounds with large defects of the skin and to manage wounds that underwent primary suture. However early diagnosis and treatment is crucial for implant salvage and for a better outcome of the therapy.
NPWT can be applied in different age groups and in different pathologies, paying attention to contraindications.
In all of our patients, NPWT shortened and decreased the costs of hospitalizations. The patients were compliant to the treatment, the dressing being changed every 3 or 4 days, while a classical dressing required daily changes. ❑
ACKNOWLEDGMENTS
The authors of the article entitled "NEGATIVE PRESSURE, A "SOLUTION" IN THE TREATMENT OF INFECTED KNEE PROSTHESIS?" would like to thank the Orthopedics, Plastic and Reconstructive surgery and Radiology team for their help and support. The authors would also like to thank the Microbiology lab for their collaboration and help.
CONFLICT OF INTEREST
none declared.
FINANCIAL SUPPORT
none declared.
References
- 1.Orgill DP, Bayer LR. Update on negative-pressure wound therapy. Plast Reconstr Surg. 2011;127:105S–115. doi: 10.1097/PRS.0b013e318200a427. [DOI] [PubMed] [Google Scholar]
- 2.Isc E, Canter HI, Dadac M, et al. The efficacy of negative pressure wound therapy on chemotherapeutic extravasation ulcers: An experimental study; Indian J Plast Surg. 2014;47:394–400. doi: 10.4103/0970-0358.146611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Morykwas MJ, Simpson J, Punger K, et al. Vacuum-assisted closure: State of basic research and physiologic foundation. Plast Reconstr Surg. 2006;117:121–126. doi: 10.1097/01.prs.0000225450.12593.12. [DOI] [PubMed] [Google Scholar]
- 4.Dowsett C, Davis L, Henderson V, et al. The economic benefits of negative pressure wound therapy in community-based wound care in the NHS. International Wound Journal. 2012;9:544–552. doi: 10.1111/j.1742-481X.2011.00913.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chen SZ, Li J, Li XY, et al. Effects of vacuum-assisted closure on wound microcirculation: An experimental study. Asian J Surg. 2005;28:211–217. doi: 10.1016/S1015-9584(09)60346-8. [DOI] [PubMed] [Google Scholar]
- 6.Othman D. Negative pressure wound therapy literature review of efficacy, cost effectiveness, and impact on patients' quality of life in chronic wound management and its implementation. United Kingdom Plast Surg Int. 2012;2012:374398–374398. doi: 10.1155/2012/374398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dunn R, Hurd T, Chadwick P, et al. Factors associated with positive outcomes in 131 patients treated with gauze-based Negative Pressure Wound Therapy. Int J Surg. 2011;9:258–62. doi: 10.1016/j.ijsu.2010.12.005. [DOI] [PubMed] [Google Scholar]
- 8.Ubbink DT1, Westerbos SJ, Nelson EA, et al. A systematic review of topical negative pressure therapy for acute and chronic wounds. Br J Surg. 2008;95:685–692. doi: 10.1002/bjs.6238. [DOI] [PubMed] [Google Scholar]
- 9.Chen KD, Li YS, Kim M, et al. Mechanotransduction in response to shear stress. Roles of receptor tyrosine kinases, integrins, and Shc. J Biol Chem. 1999;274:18393–18400. doi: 10.1074/jbc.274.26.18393. [DOI] [PubMed] [Google Scholar]
- 10.Li XQ, Hu DH, Liu Y, et al. Influence of negative pressure wound therapy on the angiogenesis of wounds in diabetic rats. Zhonghua Shao Shang Za Zhi. 2013;29:442–447. [PubMed] [Google Scholar]
- 11.Zhu J, Yu A, Qi B, et al. Effects of Negative Pressure Wound Therapy on Mesenchymal Stem Cells Proliferation and Osteogenic Differentiation in a Fibrin Matrix. 2014;9:1–9. doi: 10.1371/journal.pone.0107339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mouës CM, Heule F, Hovius SE, et al. A review of topical negative pressure therapy in wound healing: sufficient evidence? American Journal of Surgery. 2011;201:544–556. doi: 10.1016/j.amjsurg.2010.04.029. [DOI] [PubMed] [Google Scholar]
- 13.Bourée M, Kozianka J, Die VAC, et al. Therapie in der Allgemeinchirugie. European Society ACA. 2003;191:35–38. [Google Scholar]
- 14.Putnis S, Khan WS, Wong JML. Negative Pressure Wound Therapy – A Review of its Uses in Orthopaedic Trauma. The Open Orthopaedics Journal. 2014;8:142–147. doi: 10.2174/1874325001408010142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.US food and drug administration – Class II special controls guidance document: Non-powered suction apparatus device intended for negative pressure wound therapy (NPWT). http:// www.fda.gov/downloads/MedicalDevices/DeviceRegulationandGuidanc e/GuidanceDocuments/UCM233279.pdf (Accessed: 10th March, 2014).


