Abstract
Dystrophic calcinosis cutis was commonly described in long-term dermatomyositis or systemic sclerosis, being rarely reported in other connective tissue diseases.
We report the case of a 65-years old woman with an only 5-years history of systemic lupus erythematosus, who presents with multiple, impressive subcutaneous calcified masses and biological normal serum calcium and phosphate levels.
Keywords: Calcinosis cutis, subcutaneous calcifications
CASE REPORT
A 65-year-old woman was referred to our department for polyarthralgia and functional impotence for the articulations of elbows, knees and ankles. Five years ago she was diagnosed with systemic lupus erythematosus (SLE), characterized by cutaneous, hematological and vasculitis involvements. Immunologically, she presented anti-dsDNA antibodies and anti-Ro antibodies.
The clinical examination showed small nodules in the fingers and multiple, indurate, various sized subcutaneous deposits in elbows, knees, thighs and gluteal muscles with a preferential periarticular distribution. Also, a ulcerate lesion in the gluteal muscles region, that revealed a chalky material.
Biologically, the serum calcium and phosphate levels were normal. The radiological examination showed large, impressive calcium deposits in elbows (Figure 1), knees, gluteal muscles region and thighs (Figure 2). ❑
Figure 1.
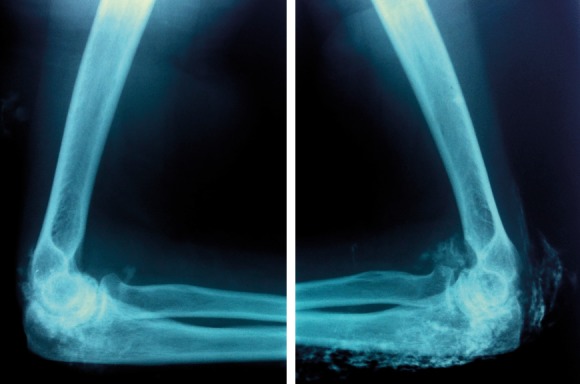
Elbow X-ray.
Figure 2.
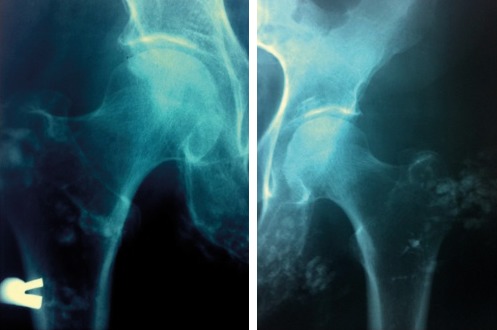
Coxofemoral joint X-ray.
DIFFERENTIAL DIAGNOSES OF SUBCUTANEOUS CALCIFICATIONS
Calcinosis cutis (CC) is an entity characterized by the presence of insoluble calcium salts in the skin and subcutaneous tissue (1).
Boulman et al. reweaving older classifications of CC proposed a characterization taking into account calcium/phosphorus levels and the background disease associated with the presence of CC. They divided the subcutaneous calcifications into five groups: metastatic calcification, tumoral calcification, dystrophic calcification, idiopathic calcification and calciphylaxis (2). Starting from this classification, Guttierez and Wetter spoke also about iatrogenic calcinosis as a separate entity and included tumoral calcinosis, a rare familial disorder into idiopathic calcification group and calciphylaxis, syndrome of vascular calcification into metastatic calcification group (3).
In Table 1 we tried to summarize the main etiologies that participate to the differential diagnosis at a patient with CC. ❑
Table 1.
Classification of calcinosis cutis.
| Dystrophic (normal calcium or phosphorus) |
| Connective tissue diseases Dermatomyositis Systemic sclerosis Mixed CTD Lupus erythematosus Undifferentiated CTD Overlap CTD |
| Metastatic (elevated calcium or phosphorus) |
| Chronic renal failure Hyperparathyroidism Sarcoidosis Milk alkali syndrome Malignancies Hypervitaminosis D |
| Calciphylaxis (abnormal calcium-phosphorus levels) |
| Small vessel vasculopathy |
| Iatrogenic (ab/normal calcium or phosphorus levels) |
| IV calcium-containing solutions Sites of venipuncture |
| Idiopathic (normal calcium or phosphorus) |
| Subepidermal calcified nodules Scrotal calcinosis |
| Tumoral (normal calcium and elevated phosphorus) |
| Familial disorder |
FINAL CLINICAL COMMENTS
CC, a clinical feature associated with CTD, was rarely reported at patients with SLE; until 2010 being only 36 such cases reported in English-language medical published work (4). In a retrospective study involving 78 patients with CC, Balin et al. found only 2 patients with SLE. On the contrary, CC was described in 23 patients with dermatomyositis (DM) and 21 patients with systemic sclerosis (SS) from the same series (5).
CC typically develops in patients with long-standing SLE (6) and might be an incidental radiologic finding because patients with CC and SLE tend to be asymptomatic (7). Local trauma or local ischemia might be involved as precipitating factors (3), the periarticular areas being most often involved (8).
In this paper we describe a rare association for CC, in a patient apparently without a long-standing CTD (only 5 years from the diagnosis of SLE), but with spectacular radiological images of massive calcium subcutaneous deposits (calcinosis cutis universalis).
The efficacy of different medical treatment for CC, like Warfarin, Bisphosphonates, Mynocicline, Ceftriaxone, Diltiazem, Aluminium hydroxide, Probenecid or Intravenous immunoglobulin, was reported only in single cases or small series, no treatment being generally accepted as standard therapy (9). ❑
Abbreviations
- CC
calcinosis cutis
- CTD
connective tissue disease
- DM
dermatomyositis
- SLE
systemic lupus erythematosus
- SS
systemic sclerosis
CONFLICT OF INTEREST
none declared.
FINANCIAL SUPPORT
none declared.
References
- 1.Reiter N, El-Shabrawi L, Leinweber B, et al. Calcinosis cutis: part I. Diagnostic pathway. J Am Acad Dermatol. 2011;65:1–12. doi: 10.1016/j.jaad.2010.08.038. [DOI] [PubMed] [Google Scholar]
- 2.Boulman N, Slobodin G, Rozenbaum M, et al. Calcinosis in rheumatic diseases. Semin Arthritis Rheum. 2005;34:805–12. doi: 10.1016/j.semarthrit.2005.01.016. [DOI] [PubMed] [Google Scholar]
- 3.Gutierrez A Jr, Wetter DA. Calcinosis cutis in autoimmune connective tissue diseases. Dermatol Ther. 2012;25:195–206. doi: 10.1111/j.1529-8019.2012.01492.x. [DOI] [PubMed] [Google Scholar]
- 4.Kim MS, Choi KC, Kim HS, et al. Calcinosis cutis in systemic lupus erythematosus: a case report and review of the published work. J Dermatol. 2010;37:815–8. doi: 10.1111/j.1346-8138.2010.00894.x. [DOI] [PubMed] [Google Scholar]
- 5.Balin SJ, Wetter DA, Andersen LK, et al. Calcinosis cutis occurring in association with autoimmune connective tissue disease: the Mayo Clinic experience with 78 patients, 1996-2009. Arch Dermatol. 2012;148:455–62. doi: 10.1001/archdermatol.2011.2052. [DOI] [PubMed] [Google Scholar]
- 6.Carocha AP, Torturella DM, Barreto GR, et al. Calcinosis cutis universalis associated with systemic lupus erythematosus: an exuberant case. An Bras Dermatol. 2010;85:883–7. doi: 10.1590/s0365-05962010000600016. [DOI] [PubMed] [Google Scholar]
- 7.Park YM, Lee SJ, Kang H, et al. Large subcutaneous calcification in systemic lupus erythematosus: treatment with oral aluminum hydroxide administration followed by surgical excision. J Korean Med Sci. 1999;14:589–92. doi: 10.3346/jkms.1999.14.5.589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Okada J, Nomura M, Shirataka M, et al. Prevalence of soft tissue calcifications in patients with SLE and effects of alfacarcidol. Lupus. 1999;8:456–61. doi: 10.1177/096120339900800608. [DOI] [PubMed] [Google Scholar]
- 9.Reiter N, El-Shabrawi L, Leinweber B, et al. Calcinosis cutis: part II. Treatment options. J Am Acad Dermatol. 2011;65:15–22. doi: 10.1016/j.jaad.2010.08.039. [DOI] [PubMed] [Google Scholar]


