Abstract
Background:
Best's disease is a hereditary form of macular dystrophy that starts in childhood and progresses until visual symptoms occur. In evolution it can be complicated with choroidal neovascularization, condition very rare in children.
We report an important visual improvement in a 8-year-old caucasian girl after successful treatment with one intravitreal bevacizumab injection. There are few cases reported in literature (1-7), and the patient presented here have important particularities: one of the youngest children ever-mentioned with this complication, the third-member of her family with this disease and the first patient who didn't receive a second intravitreal bevacizumab at six weeks after first treatment, even though BCVA was lower than expected. The girl accused decrease of vision in the RE for the past 3-4 months. BCVA at presentation was 1/10. After 6 weeks from the intravitreal treatment, BCVA improved, but not very satisfactory (5/10). Because fundus and OCT aspects were encouraging, we waited another 4 weeks before the second injection. BCVA doubled in this period (8/10). Visual acuity, fundus and OCT aspects stabilized for 18 months of follow-up.
Conclusion:
We note that choroidal neovascular membrane associated with Best's disease can appear at such young children, this fact being very important in the phase of diagnosis, when the clinician should also take in consideration this possibility.
Another important idea underlined here is the long-term efficacy of a single intravitreal anti-VEGF injection and also the no-need for imminent, fast re-treatment when the fundus and OCT aspects are encouraging through the follow-up.
Keywords: Best's disease, Bevacizumab, choroidal neovascular membrane, vitelliform macular dystrophy
BACKGROUND
Best's vitelliform macular dystrophy is a hereditary form of macular dystrophy that starts in childhood and progresses until visual symptoms occur. In evolution it can be associated and complicated with choroidal neovascularization.
Bevacizumab, an anti-vascular endothelial growth factor (VEGF), is a humanized, monoclonal antibody commonly used as an 'off-label' drug for the management of choroidal neovascularization (in age related macular degeneration, pathological myopia, parafoveal idiopathic teleangiectasia).
We report an important visual improvement in a 8-years old Caucasian girl after successful treatment of choroidal neovascularization with only one intravitreal bevacizumab injection. ❑
CASE REPORT
SS, 8-year-old girl came in our department accusing loss of vision and distorted images in the right eye for the past 3-4 months. There were no systemic diseases associated, no pathological personal or heredo-collateral antecedents (excepting the fact that her mother told us she had the same problem, with loss of vision in the both eyes; she received the diagnosis of macular toxoplasmosis sequelae but couldn't show us any written examination, diagnosis or treatment).
The best corrected visual acuity was 1/10 in the right eye and 9/10 in the left eye. Intraocular pressures were good, 16 and 15 mmHg without any treatment (contact tonometry). Full ocular movements, no relative afferent pupillary defect.
At the slit-lamp examination the anterior segment was unremarkable in both eyes.
Fundus examination of the right eye revealed a large, egg yolk-like subfoveal lesion of 1 disk diameter characteristic of Best's disease, associated with a yellowish-grey choroidal neovascular membrane, with subretinal hemorrhage (Figure 1). Left eye shows an egg yolk appearance at the fovea characteristic of Best's disease (vitelliform stage).
Figure 1.
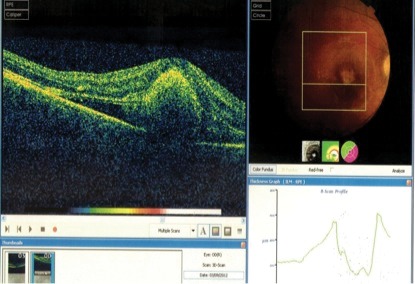
Fundus examination and optical coherence tomography aspect in the right eye. Fundus examination: Large, egg yolk-like subfoveal lesion of 1 disk diameter characteristic of Best's disease, associated with a yellowish-grey choroidal neovascular membrane, with subretinal hemorrhage.
OCT: Cystoid macular edema, CNVM, RPE detachment, subretinal blood.
Right eye fundus flourescenin angiography reveals intense late leakage from the choroidal neovascular membrane and blocked fluorescence corresponding to the subretinal and sub RPE – hemorrhage. In the left eye there is also hypofluorescence due to blockage.
Visual field in the right eye revealed subtle central sensitivity losses and in the left eye was normal.
The electro-oculogram (EOG) was abnormal in both eyes (Arden ratio 1.2).
Optical coherence tomography (OCT) revealed in the right eye cystoid macular edema, CNVM, RPE detachment, subretinal blood (Figure 1) and in the left eye cystoid macular edema, RPE detachment and typical vitelliform changes.
Diagnosis was juvenile Best Macular Dystrophy:
RE: vitelliform stage with sub-RPE choroidal neovascularization and subretinal hemorrhage
LE: vitelliform stage
We have evaluated also the family members. The mother had BCVA: 160/200 in both eyes and the fundus examination revealed Best's disease vitelliform stage in both eyes. Also, the smaller sister, 6 years old was identified with the disease, vitteliform stage. The family was provided with genetic counseling, career counseling and follow-up examinations.
The treatment for the right eye with anti-VEGF agents was discussed with the family and they signed an informed (written) consent.
So the patient received in the right eye an intravitreal injection with bevacizumab 0.05 ml under strict aseptic precautions. The post injection period was uneventful.
After six weeks of follow-up, BCVA in the right eye was 5/10 and the girl was still complaining of distorted image, but lesser than before the injection. BCVA in the left eye was stable.
Fundus examination of the right eye revealed a CNVM in regression, with resolution of subretinal hemorrhage (Figure 2). The left eye fundus was stable.
Figure 2.
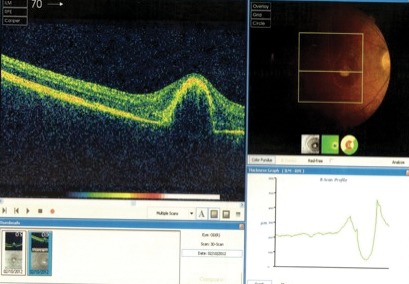
Fundus examination and optical coherence tomography aspect in the right eye after six weeks of follow-up. Fundus examination: CNVM in regression, with resolution of subretinal hemorrhage.
OCT: RPE detachment, with no subretinal haemorrhage and increased fibrosis of CNVM.
The OCT in the right eye revealed RPE detachment, with no subretinal hemorrhage and increased fibrosis of CNVM (Figure 2). Left eye OCT was stable.
We decided to wait another month and see what happens before a re-treatment with bevacizumab.
So, after another four weeks, BCVA in the right eye was 8/10, the left eye was stable, without complains from the patient.
Fundus examination and OCT in both eyes revealed RPE detachment and stagnant Juvenile Best Disease, vitteliform stage, so there was no need for re-treatment with bevacizumab.
After a follow-up of 18 months, BCVA, fundus examination and OCT were stagnant in both eyes, without any complains from the patient. During the entire course of treatment, we did not encounter any drug-related ocular or systemic side effects. ❑
DISCUSSION
Choroidal neovascular membrane is a rare complication of Best's disease in children. As you saw in the case stated before, it can appear at such small ages, in children, this fact being very important in the phase of diagnosis, when the clinician should also take into consideration this possibility.
There are reported in literature other various treatment procedures for CNVM in Best's disease: photodynamic therapy, laser photocoagulation, intravitreal bevacizumab with triamcinolone. The most important limitation of photodynamic therapy with verteporfin is the high cost, as for laser photocoagulation is that it is not suitable for subfoveal CNVM.
As you saw in our case, the child's vision improved a lot after 10 weeks with only one intravitreal bevacizumab and was maintained until 2-year follow-up without any negative events. ❑
CONCLUSION
Intravitreal bevacizumab as a monotherapy is a promising and suitable procedure of treatment in choroidal neovascular membrane, improving the visual acuity and presenting low interventional risks.
We also stress the idea that in achieving a long-term stabilization, there is no-need for imminent, fast re-injection when the BCVA starts improving and the OCT aspect is encouraging.
ACKNOWLEDGMENTS
Written informed consent was obtained from the patient's mother for publication of this case report and any accompanying images. A copy of the written consent is available for review.
Abbreviations
- BCVA
best corrected visual acuity
- CNMV
choirodal neovascular membrane
- OCT
optical coherence tomography
- LE
left eye
- RE
right eye
- RPE
retinal pigment epithelium
CONFLICT OF INTEREST
none declared.
FINANCIAL SUPPORT
This work was supported by the project entitled "CERO - Career profile: Romanian Researcher", (grant number POSDRU/ 159/1.5/S/135760), cofinanced by the European Social Development 2007-2013.
References
- 1.Perol J, Wolff B, Sahel JA, et al. Intravitreal bevacizumab treatment for choroidal neovascularization in Best's disease. J Fr Ophtalmol. 2011;34:281–6. doi: 10.1016/j.jfo.2010.11.021. [DOI] [PubMed] [Google Scholar]
- 2.Cennamo G, Cesarano I, Vecchio EC, et al. Functional and anatomic changes in bilateral choroidal neovascularization associated with vitelliform macular dystrophy after intravitreal bevacizumab. J Ocul Pharmacol Ther. 2012;28:643–6. doi: 10.1089/jop.2011.0250. [DOI] [PubMed] [Google Scholar]
- 3.Taban C, Merticariu A, Melcioiu L, et al. Choroidal neovascular membrane in Best juvenile dystrophy treated with intravitreal bevacizumab. Oftalmologia. 2013;57:42–51. [PubMed] [Google Scholar]
- 4.Chhablani J, Jalali S. Intravitreal bevacizumab for choroidal neovascularization secondary to Best vitelliform macular dystrophy in a 6-year-old child. Eur J Ophthalmol. 2012;22:677–9. doi: 10.5301/ejo.5000095. [DOI] [PubMed] [Google Scholar]
- 5.Mandal S, Sinha S, Venkatesh P, et al. Intravitreal bevacizumab in choroidal neovascularization associated with Best's vitelliformdystrophy. Indian J Ophthalmol. 2011;59:262–3. doi: 10.4103/0301-4738.81034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lee YS1, Kim ES, Kim M, et al. Atypical vitelliform macular dystrophy misdiagnosed as chronic central serous chorioretinopathy: case reports. BMC Ophthalmol. 2012;20:12–25. doi: 10.1186/1471-2415-12-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hussain RN, Shahid FL, Empeslidis T, et al. Use of Intravitreal Bevacizumab in a 9-year-old Child with Choroidal Neovascularization Associated with Autosomal Recessive Bestrophinopathy. Ophthalmic Genet. 2014;29:1–5. doi: 10.3109/13816810.2014.962706. [DOI] [PubMed] [Google Scholar]


