Abstract
Purpose:
We compared measurements of central retinal sensitivity on a portable, low-cost tablet device to the established method of microperimetry in age-related macular degeneration (AMD).
Methods:
A customized test designed to measure central retinal sensitivity (within the central 1° radius) on a tablet device was developed using an open-source platform called PsyPad. A total of 30 participants with AMD were included in this study, and all participants performed a practice test on PsyPad, followed by four tests of one eye and one test of the other eye. Participants then underwent standardized microperimetry examinations in both eyes.
Results:
The average test duration on PsyPad was 53.9 ± 7.5 seconds, and no significant learning effect was observed over the examinations performed (P = 1.000). The coefficient of repeatability of central retinal sensitivity between the first two examinations on PsyPad was ±1.76 dB. The mean central retinal sensitivity was not significantly different between PsyPad (25.7 ± 0.4 dB) and microperimetry (26.1 ± 0.4 dB, P = 0.094), and the 95% limits of agreement between the two measures were between −4.12 and 4.92 dB.
Conclusions:
The measurements of central retinal sensitivity can be performed effectively using a tablet device, displaying reasonably good agreement with those obtained using the established method of microperimetry.
Translational Relevance:
These findings highlight the potential of tablet devices as low-cost and portable tools for developing and performing visual function measures that can be easily and widely implemented.
Keywords: iPad, visual function, microperimetry, age-related macular degeneration
Introduction
Measurements of visual function beyond the standard measure of visual acuity (VA) have been performed widely in ocular diseases to provide further insights into disease pathogenesis, and also to provide potential tools for monitoring disease progression and response to treatment.1–6 They have been reported to have potential prognostic value in diseases, such as age-related macular degeneration (AMD), especially before the development of vision-threatening complications or vision loss.7–10 However, such measures are typically performed in controlled clinical or research environments using specialized equipment that can be expensive and often not portable.
Advances in technology have led to the development of portable tablet devices where the resolution and luminance range of the touch-screens could allow visual function measures to be performed.11,12 Previous studies have reported that visual acuity13,14 and contrast sensitivity15,16 measurements can, indeed, be performed reliably on such devices. Recently, an open-source platform that allows visual psychophysics experiments to be performed on an iPad tablet device (Apple, Inc., Cupertino, CA) called PsyPad also was introduced by Turpin et al.17 to allow customized tests to be created, and, thus provide an avenue to develop and evaluate visual function measures with ease.
The development of more effective visual function measures to characterize the disease severity and monitor progression is particularly relevant for AMD, since it is well-established that the standard measurement of VA does not sufficiently detect deficits in the early stages.18,19 Visual acuity often is unaffected until later in the AMD disease process through the development of atrophic changes (which often develop outside the fovea first20) or choroidal neovascularization (CNV). We recently found that the measurement of central retinal sensitivity to luminance increment under mesopic conditions using microperimetry was a more sensitive measure of foveal functional deficit than VA measured under photopic and mesopic conditions.19
The ability to measure central retinal sensitivity under mesopic conditions using a relatively inexpensive, portable tablet device would be highly desirable. Therefore, we sought to compare the measurements of central retinal sensitivity on a tablet device with the established method of microperimetry.
Methods
This study involved a prospective examination of consecutive AMD participants that were currently involved in research studies where microperimetry was performed. It was approved by the Human Ethics Committee of the Royal Victorian Eye and Ear Hospital (RVEEH) and was conducted in adherence with the Declaration of Helsinki. Written informed consent was obtained from all participants following an explanation of all test procedures.
Participants
The inclusion criteria for all participants in this study were being 50 years of age or older and having at least intermediate AMD in both eyes.21 The exclusion criteria for any study eye included the presence of central geographic atrophy, disciform scar involving the fovea, glaucoma, significant cataracts, any corneal pathology that could compromise vision, diabetes, uncontrolled hypertension, amblyopia, neurological or systemic disease affecting vision, or any medication known to affect retinal function. Any participant also was excluded if they had any physical and/or mental impairment preventing them from participating in this study or an inability to sign a consent form.
Procedures
All participants underwent subjective refraction first using a standardized protocol that was performed monocularly using an Early Treatment Diabetic Retinopathy Study refraction chart at 4 m. Pupillary dilation of a minimum of 6 mm then was performed using 1 drop of tropicamide 1% and 1 drop of phenylephrine 2.5%, followed by measurements of central retinal sensitivity using the PsyPad application (app) and then microperimetry. Pupillary dilation was performed in this study to provide consistent testing conditions for the two measures, but is unlikely to be required when measuring luminance increment sensitivity in the foveal region, since previous studies did not find a significant influence of pupil size on these measurements in the foveal region.22,23 Retinal imaging including color fundus photography and spectral-domain optical coherence tomography (SD-OCT) scans then were performed using a Spectralis HRA+OCT (Heidelberg Engineering, Heidelberg, Germany) to allow the diagnosis of AMD to be confirmed, followed by clinical ophthalmic examination.
Measurements of Retinal Sensitivity Using the PsyPad App
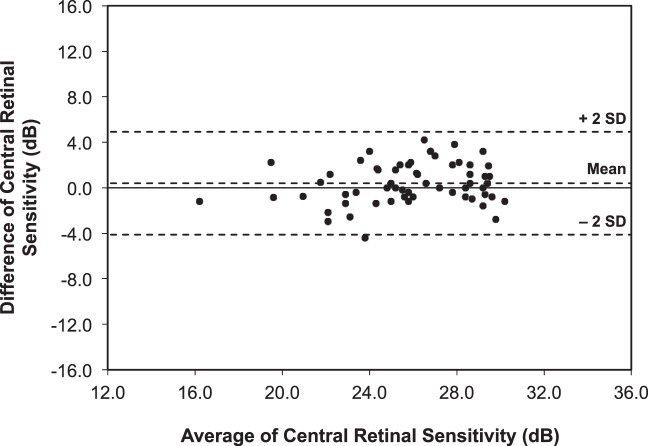
A test designed to measure central retinal sensitivity to luminance increment was developed on PsyPad, a customizable, open-source platform,17 and implemented on an iPad 3 tablet device (Apple, Inc.). PsyPad enables the display of a library of images (png, drawn using custom software) at desired timing and with the implementation of standard thresholding procedures (in this case a staircase, described below). The images included a uniform background (having a luminance of 1.27 cd/m2) and test stimuli that were circular white targets (Goldmann Size III, or 0.43° scaled for a viewing distance of 50 cm) of specific luminance levels at 1 dB increments; the maximum and minimum luminance of the stimuli were set at 317.50 and 1.52 cd/m2, respectively, providing a dynamic range of 31 dB. All image luminance levels were checked with a PR-650 Spectra-Scan Colorimeter (Photo Research, Inc., Chatsworth, CA). Stimuli were presented randomly for 200 msec without any cues at 5 locations within the central 1° radius, inside a red ring with a radius of 3° as a fixation target (Fig. 1). This fixation target differed from that used for microperimetry to minimize the influence of the fixation target on the measurements. The time between a response to the next stimulus presentation was set at a mean ± δ of 1.00 ± 0.25 seconds, where δ is sampled uniformly at random from [−variation, variation]. When no response was registered, the time to the next stimulus presentation following the onset of the stimulus was 1.50 seconds. No false-positive or false-negative trials were included, since the limited number of trials that could be added to this test to maintain a short duration would provide an inaccurate estimation of test reliability. A 4-2 staircase strategy was used to obtain the threshold measurements, with the initial stimuli set at 24 dB. The final threshold estimate was taken as the last-seen presentation after the second reversal had occurred or was terminated following two negative or positive responses to the brightest (floor; 0 dB) or dimmest (ceiling; 31 dB) stimuli, respectively. Central retinal sensitivity was defined as the average threshold estimate of five stimuli in decibels. A grey square (physical size of 36 mm) at the bottom-right corner was designated as an on-screen button for responses; these test parameters are illustrated in Figure 1. All responses were recorded in log files that were sent to a specified server as outlined previously.17
Figure 1.
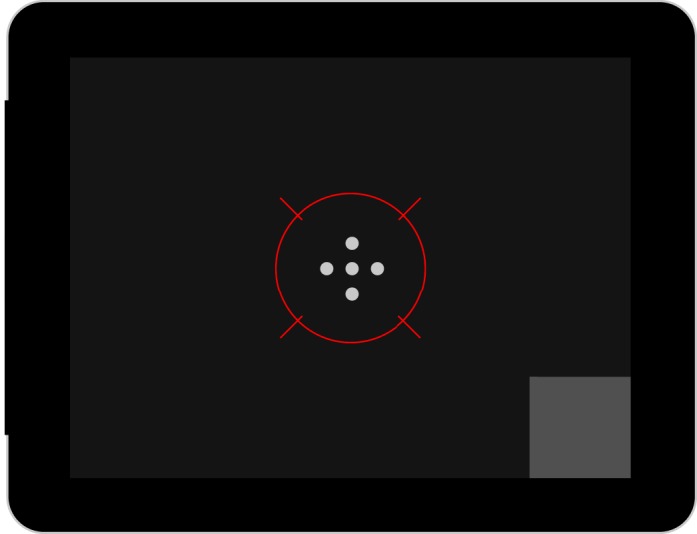
Illustration of the customized test designed on the PsyPad platform to measure central retinal sensitivity (within the central 1° radius) and the location of the five test stimuli are shown. The test stimuli are presented within the fixation target (red ring, 3° in radius) and participants responded to seeing a stimulus by pressing the grey response square at the bottom right hand corner.
PsyPad examinations were performed with participants wearing their distance refractive correction with a +2.00 D near addition included in a trial frame for the viewing distance of 50 cm, in a darkened room with a luminance lower than background luminance of screen, without any formal adaptation to the ambient illumination or background luminance of the screen. Participants were seated at a table in front of the tablet device, which was placed on a reading stand and were adjusted to the correct viewing distance by the examiner; the examiner ensured that the participant was at the correct viewing distance throughout the test and repositioned the participant between examinations if required. Before formal measurement of thresholds, the examiner explained the procedure for performing the examinations (using the illustration shown in Fig. 1), and all participants then performed a short practice examination consisting of 10 stimuli with differing luminance levels to familiarize themselves with the testing procedure (providing approximately 1 to 2 minutes of adaptation to the ambient illumination and background luminance of the screen). Participants then underwent four examinations of the left eye on PsyPad (to examine the test–retest repeatability and if a significant learning effect was present) and one examination of the right eye so both eyes can be used to examine the agreement of the measurements of retinal sensitivity between PsyPad and microperimetry.
Microperimetric Examination
All participants underwent examinations on the Macular Integrity Assessment (MAIA; CenterVue, Padova, Italy) microperimeter using a standardized method outlined previously.24 In short, the MAIA microperimeter performs fundus-tracking using a line scanning laser ophthalmoscope that illuminates the fundus using a superluminescent diode with a central wavelength of 850 nm, using the entire fundus as a reference for fundus tracking at 25 frames per second. A red circle 1° in diameter was used as a fixation target, and Goldman III sized stimuli were presented against a background of 1.27 cd/m2 using a 4-2 staircase threshold strategy. The maximum and minimum luminance of the stimulus was 318 and 1.37 cd/m2, respectively, creating a dynamic range of 36 dB. A custom grid designed to assess the macular region was used and consisted of 37 points located at 0°, 1°, 2.33°, 4°, and 6° (in radius) from fixation. Central retinal sensitivity in this study was defined as the average of microperimetry results from only the central 1° radius, comprising 1 point at 0° and 4 points at 1° radius (as used in a previous study19), and is illustrated in Figure 2. Test reliability was determined by the percentage of false-positive responses (to suprathreshold stimuli at the optic nerve head, which was manually located before the start of the threshold measurements), and any test with false-positive responses of >25% was excluded from this study; this percentage was chosen since there were typically only four to five false-positive trials in each examination. Identical instructions were given to all participants before microperimetric examinations, and each participant underwent two full examinations of the right eye followed by one full examination of the left eye. The first full examination was considered a practice and the subsequent examinations were used for analyses.
Figure 2.
Customized grid on microperimetry with the fixation target represented by the red ring and central retinal sensitivity defined as the average of the five points (lighter grey points) within the central 1° radius.
Statistical Analysis
A one-way analysis of variance (ANOVA) was used to examine whether there were significant differences in examination duration and central retinal sensitivity among the four repeated examinations of the left eye on PsyPad. The coefficients of repeatability (CoRs) of central retinal sensitivity and point-wise retinal sensitivity then were calculated for sequential pairs of these repeated examinations using the method by Bland and Altman,25 and the CoR represents a value for which 95% of the test–retest differences for the same participant are expected to lie.
To examine whether measurements of mean central retinal sensitivity were significantly different using the two methods (PsyPad and by microperimetry), the values were compared using a linear mixed effects model to account for the use of measurements from two eyes per participant, by using eyes nested within participants as the random effect and the type of test (PsyPad or microperimetry) as the fixed effect. The 95% limits of agreement (95% CI) between these two measurements were then determined using a method described by Bland and Altman26 that accounts for the use of multiple measurements per participant, by taking into account the within-subject variance. All statistical analyses were performed using commercially available statistical software (IBM SPSS Statistics, software version 21; IBM/SPSS, Inc., Chicago, IL).
Results
A total of 30 consecutive AMD participants was included in this study, and had an average age of 70.9 ± 8.2 years (range, 51–85 years).
Intrasession Characteristics of Test Parameters on PsyPad
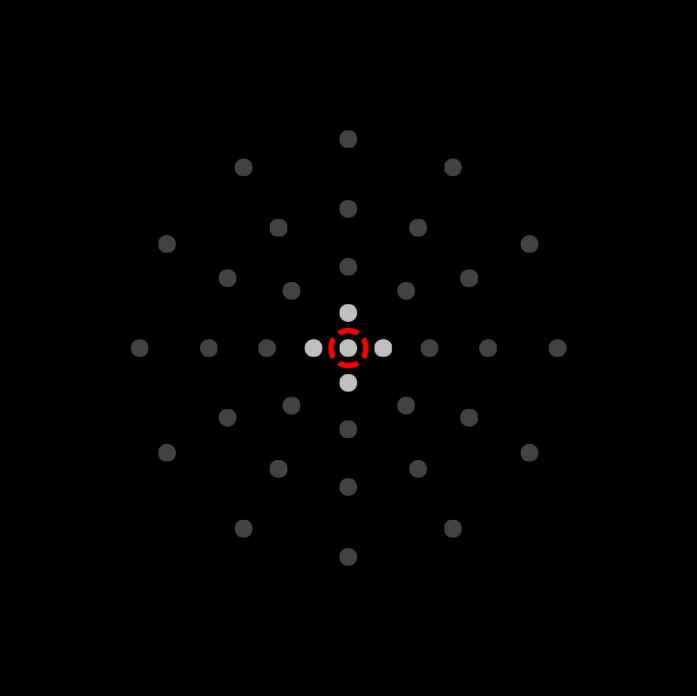
Each test on PsyPad took on average 53.9 ± 7.5 seconds (range, 39–83 seconds), and the average test duration did not differ significantly between each of the five tests performed within the same session (F [4, 145] = 0.253, P = 0.907). There also was no significant difference in mean central retinal sensitivity between any pairs of the four examinations performed on PsyPad in the first eye (P = 1.000, Fig. 3).
Figure 3.
Intrasession changes in mean central retinal sensitivity using PsyPad for participants with AMD, showing no significant differences in the mean central retinal sensitivity between any pair of the four sequential examinations in both groups. Error bars: 95% CI of the mean.
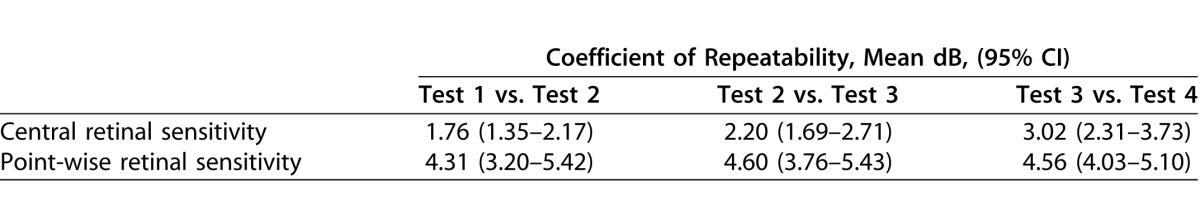
Since there were no significant differences between examinations, the test–retest repeatability could be determined; the CoR of mean central retinal sensitivity and pointwise retinal sensitivity for each sequential PsyPad examination pair (tests 1 vs. 2, tests 2 vs. 3, and tests 3 vs. 4) are shown in the Table.
Table 1.
Coefficients of Repeatability for Sequential PsyPad Examination Pairs
Agreement Between PsyPad and Microperimetry
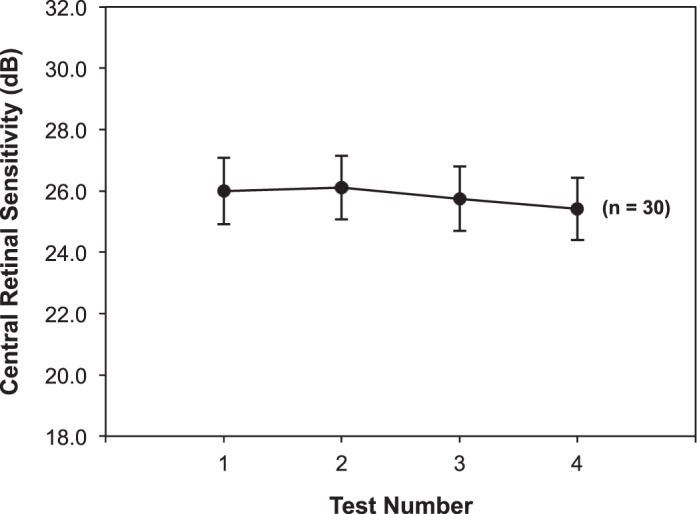
Since there was no significant learning effect, the data of the first PsyPad examination of each eye were used and compared with microperimetry. The mean central retinal sensitivity (±SEM) for all eyes was 25.7 ± 0.4 and 26.1 ± 0.4 dB measured using PsyPad and microperimetry, respectively, and was not significantly different using these two methods (P = 0.094). Bland-Altman plots then were used to examine the agreement between the two methods, and no obvious relationship between the difference and magnitude was observed (Fig. 4). The 95% CIs between the two measures were between −4.12 and 4.92 dB.
Figure 4.
Bland-Altman plot of mean central retinal sensitivity measurements obtained using PsyPad and microperimetry, illustrating the agreement between the two measures (the difference was obtained by subtracting the central retinal sensitivity results of microperimetry from PsyPad). Horizontal dashed lines represent the upper limits of 95% of the mean (+2 SD), mean, and lower limits of 95% of the mean (−2 SD) from top to bottom respectively, and the solid dashed line represents zero.
Discussion
In this study, we sought to design and assess the ability of portable tablet devices to measure central retinal sensitivity compared to those obtained using the established method of microperimetry. We did not find a significant difference between the mean central retinal sensitivity between these two methods and their 95% CIs were between −4.12 and 4.92 dB. These findings highlight the potential for measures of visual function to be developed and implemented in clinical and nonclinical settings with ease using tablet devices.
To ensure that an accurate comparison is performed between the measurements of central retinal sensitivity on PsyPad and microperimetry in this study, we performed four PsyPad examinations on the left eye of each participant to examine intrasession changes in its measurements, since we have observed previously a significant learning effect between the first two microperimetric examinations, even after participants performed a short practice test.24 We had expected that given the short duration of each test, participants would have required a greater number of examinations before becoming familiarized with this test and, thus, exhibit a learning effect over several examinations. Instead, we did not find a significant intrasession learning effect and, therefore, these measurements could be used to compare to those obtained by microperimetry.
The agreement between measurements obtained using the tablet device and microperimetry appears to be reasonably good in context of its effective dynamic range. This ability to obtain measurements on a tablet device that closely represent those obtained under controlled clinical or research settings also has been demonstrated for contrast sensitivity,15,16 another measure requiring low levels of contrast (or small increments of luminance) to be presented. The ability for the tablet device to deliver stimuli with a dynamic range of 31 dB, while limited by the 8-bit range and gamma function of the tablet device display,11 still exceeds the dynamic range (of 20 dB) currently available on commercially-available microperimeters (other than the MAIA microperimeter used in this study),27 which is important in avoiding the floor- and ceiling-effects experienced by such a limited dynamic range.28
A key difference between the measurements of luminance increment sensitivity on the tablet device and microperimetry in this study was the number of locations presented during each examination. We chose to analyze only the central five locations on microperimetry within the central 1° radius (which were embedded within a test involving a total of 37 stimuli) in this study, since we have previously found that these measurements on microperimetry detected a greater degree of functional deficit than visual acuity measures.19 Therefore, we sought to design a test on the PsyPad platform to measure these same locations on a tablet device so that these measurements could be performed rapidly in a clinical setting. Although it would have been ideal to use the same stimulus pattern on both tests to allow the test–retest repeatability of these two measurements to be compared, this was a proof-of-concept study where the measurements on a tablet device were performed on participants who already were involved in research studies that required our standard microperimetry testing. Therefore, future studies will benefit from comparing the two devices using the same stimulus pattern in eyes with normal and abnormal visual function to determine the effectiveness of this test.
There are also a few other potential limitations that are important to consider in this study. Firstly, no supportive equipment, such as a headrest and/or chinrest, was used to enforce the viewing distance and, thus, may have affected the stimulus size or location throughout the test. However, the examiners ensured that the participants were in a comfortable position before commencement of the tests and, thus, we noted anecdotally that there were little changes in the viewing distance throughout the test. Secondly, no false-positive or false-negative trials were included for the PsyPad examinations due to their short duration of the examinations. However, all the participants included in this study were considered to be reliable observers, since no microperimetry examinations were excluded in this study due to poor reliability. In addition, the close agreement between the thresholds obtained by both devices suggests that the absence of false-positive or false-negative trials was unlikely to have a major influence on the findings of this study, although future iterations of this test could include these trials.
As the primary aim of this study was to examine whether measurements of luminance increment sensitivity in the foveal region are similar when obtained with a portable tablet device compared to microperimetry, we excluded participants with foveal vision loss to ensure that fixation was foveal in this pilot study. Therefore, caution must be applied when generalizing these results to eyes with foveal vision loss (such as those with central geographic atrophy or disciform scars involving the fovea), and future studies are required to examine the effectiveness of this test on a portable tablet device for such eyes and whether there are more optimal fixation targets than the one used in this study. Note also that the close agreement between measurements obtained using the two devices in this study does not suggest that fundus tracking is not beneficial for the measurements of luminance increment sensitivity in the wider macular region, since only a small region of the fovea was compared between the two devices.
The ability to develop and perform sensitive measures of visual function on a portable and low-cost tablet device has enormous potential for monitoring ocular diseases. For researchers, platforms like PsyPad allow these visual function measures to be developed, customized and evaluated in clinical settings with greater ease. Clinical studies involving multiple sites that often do not have access to specialized equipment for the measurement of visual function can potentially perform a range of measures easily using a single device. Eye and health care practitioners also can potentially have easy access to a battery of effective clinical visual function tests that can be easily implemented, which is especially useful for the provision of eye care services in developing countries and remote settings. If such tests are robust enough to overcome the potential issues associated with self-testing12 (such as maintenance of the correct viewing distance and recommended ambient illumination), these tests can enable individuals to be more engaged in monitoring their own eye health and, thus, assist in the early detection and prevention of vision loss. We anticipate that such tests also can be implemented on other low-cost devices, including smartphones and computers in the future.
We have now added the library of images used to deliver the visual stimuli in this study onto the PsyPad Public Image Gallery, as well as the staircase configuration used (http://server.psypad.net.au). It is also available in the Demo mode of the PsyPad 2.0 App from this server. This will allow other researchers to use and continue to improve this test, although it should be noted that PsyPad does not provide a clinically ready application.
In summary, we demonstrated in this study that measurements of central retinal sensitivity can be performed effectively using a portable, low-cost tablet device, showing reasonably good agreement with those obtained using the established method of microperimetry. These findings highlight the potential of tablet devices in developing and performing novel measurements of visual function that can be easily and widely implemented.
Acknowledgments
Supported by the Australian Research Council (AMM, FT0990930 and AT, FT0991326), the National Health and Medical Research Council (NH&MRC) Project Grant (1027624), Macular Disease Foundation Australia (MDFA) Research Grant, Bupa Health Foundation (Australia) and The Macular Vision Loss Support Society of Australia, Inc. CERA receives Operational Infrastructure Support from the Victorian Government and is supported by a NHMRC Centre for Clinical Research Excellence Award (#529923).
Andrew Turpin and Allison M, McKendrick contributed equally as senior author.
Disclosure: Z. Wu, None; R.H. Guymer, None; C.J. Jung, None; J.K. Goh, None; L.N. Ayton, None; C.D. Luu, None; D.J. Lawson, None; A. Turpin, None; A.M. McKendrick, None
References
- 1. Hogg RE,, Chakravarthy U. Visual function and dysfunction in early and late age-related maculopathy. Prog Retin Eye Res. 2006; 25: 249–276. [DOI] [PubMed] [Google Scholar]
- 2. Johnson CA. Psychophysical measurement of glaucomatous damage. Surv Ophthalmol. 2001; 45 (suppl 3): S313–S318. [DOI] [PubMed] [Google Scholar]
- 3. Monhart M. What are the options of psychophysical approaches in glaucoma? Surv Ophthalmol. 2007; 52: S127–S133. [DOI] [PubMed] [Google Scholar]
- 4. Neelam K,, Nolan J,, Chakravarthy U,, Beatty S. Psychophysical function in age-related maculopathy. Surv Ophthalmol. 2009; 54: 167–210. [DOI] [PubMed] [Google Scholar]
- 5. Roman AJ,, Schwartz SB,, Aleman TS,, et al. Quantifying rod photoreceptor-mediated vision in retinal degenerations: dark-adapted thresholds as outcome measures. Exp Eye Res. 2005; 80: 259–272. [DOI] [PubMed] [Google Scholar]
- 6. Fishman GA,, Jacobson SG,, Alexander KR,, et al. Outcome measures and their application in clinical trials for retinal degenerative diseases: outline, review, and perspective. Retina. 2005; 25: 772–777. [DOI] [PubMed] [Google Scholar]
- 7. Eisner A,, Klein M,, Zilis J,, Watkins M. Visual function and the subsequent development of exudative age-related macular degeneration. Invest Ophthalmol Vis Sci. 1992; 33: 3091–3102. [PubMed] [Google Scholar]
- 8. Sandberg MA,, Weiner A,, Miller S,, Gaudio AR. High-risk characteristics of fellow eyes of patients with unilateral neovascular age-related macular degeneration. Ophthalmology. 1998; 105: 441–447. [DOI] [PubMed] [Google Scholar]
- 9. Sunness JS,, Rubin GS,, Broman A,, Applegate CA,, Bressler NM,, Hawkins BS. Low luminance visual dysfunction as a predictor of subsequent visual acuity loss from geographic atrophy in age-related macular degeneration. Ophthalmology. 2008; 115: 1480–1488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Luu CD,, Dimitrov PN,, Robman L,, et al. Role of flicker perimetry in predicting onset of late-stage age-related macular degeneration. Arch Ophthalmol. 2012; 130: 690–699. [DOI] [PubMed] [Google Scholar]
- 11. Aslam TM,, Murray IJ,, Lai MY,, Linton E,, Tahir HJ,, Parry NR. An assessment of a modern touch-screen tablet computer with reference to core physical characteristics necessary for clinical vision testing. J Roy Soc Interface. 2013; 10: 20130239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Tahir HJ,, Murray IJ,, Parry NRA,, Aslam TM. Optimisation and assessment of three modern touch screen tablet computers for clinical vision testing. PLoS One. 2014; 9: e95074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Black J,, Jacobs R,, Phillips G,, et al. An assessment of the iPad as a testing platform for distance visual acuity in adults. BMJ Open. 2013; 3. [DOI] [PMC free article] [PubMed]
- 14. Zhang ZT,, Zhang SC,, Huang XG,, Liang LY. A pilot trial of the iPad tablet computer as a portable device for visual acuity testing. J Telemed Telecare. 2013; 19: 55–59. [DOI] [PubMed] [Google Scholar]
- 15. Kollbaum PS,, Jansen ME,, Kollbaum EJ,, Bullimore MA. Validation of an iPad Test of letter contrast sensitivity. Optom Vis Sci. 2014; 91: 291–296. [DOI] [PubMed] [Google Scholar]
- 16. Dorr M,, Lesmes LA,, Lu Z-L,, Bex PJ. Rapid and reliable assessment of the contrast sensitivity function on an iPad. Invest Ophthalmol Vis Sci. 2013; 54: 7266–7273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Turpin A,, Lawson DJ,, McKendrick AM. PsyPad: a platform for visual psychophysics on the iPad. J Vis. 2014; 14: 16. [DOI] [PubMed] [Google Scholar]
- 18. Klein R,, Wang Q,, Klein B,, Moss SE,, Meuer SM. The relationship of age-related maculopathy cataract, and glaucoma to visual acuity. Invest Ophthalmol Vis Sci. 1995; 36: 182–191. [PubMed] [Google Scholar]
- 19. Wu Z,, Ayton LN,, Luu CD,, Guymer RH. Low luminance visual acuity and microperimetry in age-related macular degeneration. Ophthalmology. 2014; 121: 1612–1619. [DOI] [PubMed] [Google Scholar]
- 20. Sunness JS. The natural history of geographic atrophy the advanced atrophic form of age-related macular degeneration. Mol Vis. 1999; 5: 25. [PubMed] [Google Scholar]
- 21. Ferris FL,, III,, Wilkinson C,, Bird A,, et al. Clinical classification of age-related macular degeneration. Ophthalmology. 2013; 129: 844–851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Wood JM,, Wild JM,, Bullimore MA,, Gilmartin B. Factors affecting the normal perimetric profile derived by automated static threshold LED perimetry. I. Pupil size. Ophthalmic Physiol Opt. 1988; 8: 26–31. [PubMed] [Google Scholar]
- 23. Flammer J,, Drance SM,, Fankhauser F,, Augustiny L. Differential light threshold in automated static perimetry: factors influencing short-term fluctuation. Arch Ophthalmol. 1984; 102: 876–879. [DOI] [PubMed] [Google Scholar]
- 24. Wu Z,, Ayton LN,, Guymer RH,, Luu CD. Intrasession test–retest variability of microperimetry in age-related macular degeneration. Invest Ophthalmol Vis Sci. 2013; 54: 7378–7385. [DOI] [PubMed] [Google Scholar]
- 25. Bland M,, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet. 1986; 327: 307–310. [PubMed] [Google Scholar]
- 26. Bland JM,, Altman DG. Agreement between methods of measurement with multiple observations per individual. J Biopharm Stat. 2007; 17: 571–582. [DOI] [PubMed] [Google Scholar]
- 27. Crossland M,, Jackson ML,, Seiple WH. Microperimetry: a review of fundus related perimetry. Optom Rep. 2012; 2: e2. [Google Scholar]
- 28. Chen FK,, Patel PJ,, Xing W,, et al. Test–retest variability of microperimetry using the nidek mp1 in patients with macular disease. Invest Ophthalmol Vis Sci. 2009; 50: 3464–3472. [DOI] [PubMed] [Google Scholar]