Abstract
Obesity and its associated comorbidities are among the most prevalent and challenging conditions confronting the medical profession in the 21st century. A major metabolic consequence of obesity is insulin resistance, which is strongly associated with the deposition of triglycerides in the liver. Hepatic steatosis can either be a benign, noninflammatory condition that appears to have no adverse sequelae or can be associated with steatohepatitis: a condition that can result in end-stage liver disease, accounting for up to 14% of liver transplants in the US. Here we highlight recent advances in our understanding of the molecular events contributing to hepatic steatosis and nonalcoholic steatohepatitis.
Nonalcoholic fatty liver disease (NAFLD) is a clinicopathological term that encompasses a disease spectrum ranging from simple triglyceride accumulation in hepatocytes (hepatic steatosis) to hepatic steatosis with inflammation (steatohepatitis), fibrosis, and cirrhosis (1). NAFLD is the most frequent cause of abnormal liver function tests (LFTs) in the US (2, 3), affecting approximately 30 million Americans. Excess hepatic triglyceride accumulation is associated with various drugs, nutritional factors, and multiple genetic defects in energy metabolism. However, the most common disorder associated with hepatic steatosis is insulin resistance (3). As such, it has been proposed that NAFLD be included as a component of the metabolic syndrome (4).
Day et al. (5) initially proposed a “two-hit” model to explain the progression of NAFLD. The “first hit” constitutes the deposition of triglycerides in the cytoplasm of the hepatocyte. The disease does not progress unless additional cellular events occur (the “second hit”) that promote inflammation, cell death, and fibrosis, which are the histologic hallmarks of nonalcoholic steatohepatitis (NASH). Recent studies in animal models of NAFLD have provided new insights into the molecular and physiologic alterations that constitute the first and second hits in the progression of NAFLD to end-stage liver disease and will be the focus of this review.
Epidemiology
The prevalence of NAFLD in the general population is estimated to be between 14% and 24% (6–8). NAFLD used to be almost exclusively a disease of adults. However, the estimated prevalence of the disorder has increased markedly in all segments of the population and now extends to children. The rising prevalence of obesity and type 2 diabetes in the population is likely responsible for the burgeoning number of individuals with hepatic steatosis (9, 10).
The progression of NAFLD to cirrhosis may differ significantly among ethnic groups. Hispanics with NAFLD appear to progress to NASH and cirrhosis more frequently than either blacks or whites. In contrast to Hispanics, blacks may be at reduced risk for the development of NASH and end-stage liver disease (11, 12).
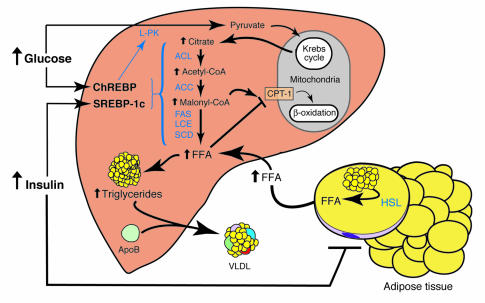
Development of hepatic steatosis
As summarized in Figure 1, a series of molecular and physiologic alterations occur in the setting of insulin resistance that results in the accumulation of triglycerides in liver. The conventional explanation for hepatic triglyceride accumulation is that obesity and insulin resistance result in increased release of FFAs from adipocytes. Increased adipocyte mass and increased hydrolysis of triglycerides through increased hormone-sensitive lipase activity contribute to elevated plasma levels of FFAs (reviewed in ref. 13). The rate of hepatic FFA uptake is unregulated and therefore directly proportional to plasma FFA concentrations (14).
Figure 1.
Metabolic alterations resulting in hepatic triglyceride accumulation in insulin-resistant states. Insulin resistance is manifested by hyperinsulinemia, increased hepatic glucose production, and decreased glucose disposal. In adipocytes, insulin resistance increases hormone-sensitive lipase (HSL) activity, resulting in elevated rates of triglyceride lipolysis and enhanced FFA flux to the liver. FFAs can either be oxidized in the mitochondria to form ATP or esterified to produce triglycerides for storage or incorporation into VLDL particles. In liver, hyperinsulinemia induces SREBP-1c expression, leading to the transcriptional activation of all lipogenic genes. Simultaneously, hyperglycemia activates ChREBP, which transcriptionally activates L-PK and all lipogenic genes. The synergistic actions of SREBP-1c and ChREBP coordinately activate the enzymatic machinery necessary for the conversion of excess glucose to fatty acids. A consequence of increased fatty acid synthesis is increased production of malonyl-CoA, which inhibits CPT-1, the protein responsible for fatty acid transport into the mitochondria. Thus, in the setting of insulin resistance, FFAs entering the liver from the periphery, as well as those derived from de novo lipogenesis, will be preferentially esterified to triglycerides. ACL, ATP citrate lyase; CPT-1, carnitine palmitoyl transferase-1; FAS, fatty acid synthase; LCE, long-chain fatty acyl elongase.
FFAs taken up by the liver are metabolized by one of two pathways: oxidation to generate ATP or esterification to produce triglycerides, which are either incorporated into VLDL particles for export or stored within the hepatocyte. As discussed below, defects in one or both of these pathways can lead to hepatic steatosis.
Molecular mediators of lipogenesis and their role in hepatic steatosis
A central metabolic function of the liver is to maintain plasma glucose levels regardless of the nutritional state of the animal. In the setting of energy excess, glucose is converted to fatty acids via the conversion of glucose to pyruvate, which enters the Krebs cycle in the mitochondria (Figure 1). Citrate formed in the Krebs cycle is shuttled to the cytosol where it is converted to acetyl-CoA by ATP citrate lyase. Acetyl-CoA carboxylase 1 (ACC1) then converts acetyl-CoA to malonyl-CoA, which is used by fatty acid synthase to form palmitic acid (C16:0). Palmitic acid is then either desaturated by stearoyl-CoA desaturase (SCD) to palmitoleic acid, or further elongated by the long chain fatty acyl elongase to form stearic acid (C18:0), which also can be desaturated to form oleic acid (C18:1) (15). These fatty acids are used to synthesize triglycerides — the primary source of energy storage and transport. Humans (16) and mice (17) with hepatic steatosis accumulate excess oleic acid, the end-product of de novo fatty acid synthesis. This suggests that fatty acid synthetic rates are increased in the insulin-resistant liver.
De novo synthesis of fatty acids in liver is regulated independently by insulin and glucose (18, 19). Insulin’s ability to activate lipogenesis is transcriptionally mediated by the membrane-bound transcription factor, sterol regulatory element–binding protein-1c (SREBP-1c) (20, 21). SREBP-1c is one of three SREBP isoforms that belong to the basic helix-loop-helix-leucine zipper (bHLH-Zip) family of transcription factors (22). In the nucleus, SREBP-1c transcriptionally activates all genes required for lipogenesis (15, 23). Importantly, the overexpression of SREBP-1c in transgenic mouse livers leads to the development of a classic fatty liver due to increased lipogenesis (24). We (25), and others (26, 27) have demonstrated that increased rates of hepatic fatty acid synthesis contribute to the development of fatty livers in rodent models of insulin-resistant diabetes and obesity.
Hyperinsulinemia and elevated hepatic glucose production are hallmarks of insulin resistance (28). It might be anticipated that SREBP-1c would not be activated in states of insulin resistance. Surprisingly, even in the presence of profound insulin resistance, insulin stimulates hepatic SREBP-1c transcription, resulting in increased rates of de novo fatty acid biosynthesis (25). The contribution SREBP-1c makes to triglyceride accumulation in insulin-resistant livers has been explored in ob/ob mice. Ob/ob mice are severely obese and insulin resistant due to a mutation in the leptin gene and, as a consequence, these mice have hepatic steatosis (29). Inactivation of the Srebp-1 gene in the livers of ob/ob mice results in an approximately 50% reduction in hepatic triglycerides (30). Thus, SREBP-1 plays a significant role in the development of hepatic steatosis in this animal model of insulin resistance.
SREBP-1c also activates ACC2 (23), an isoform of ACC that produces malonyl-CoA at the mitochondrial membrane (31). Increases in malonyl-CoA result in decreased oxidation of fatty acids due to inhibition of carnitine palmitoyl transferase-1 (CPT-1), which shuttles fatty acids into mitochondria (32). The critical role of ACC2 in hepatic fatty acid metabolism was revealed in mice that harbored the genetic deletion of the Acc2 gene. The Acc2 knockout mice were resistant to obesity, owing to increased activity of CPT-1, resulting in an increased rate of fatty acid oxidation (33, 34). Adenoviral-mediated expression of malonyl-CoA decarboxylase, an enzyme that degrades malonyl-CoA, also results in increased fatty acid β oxidation and reduced hepatic triglyceride stores (35).
Carbohydrate (glucose)-mediated stimulation of lipogenesis is transcriptionally mediated by a second bHLH-Zip transcription factor, designated carbohydrate response element binding protein (ChREBP) (36). Glucose activates ChREBP by regulating the entry of ChREBP from the cytosol into the nucleus and by activating the binding of the transcription factor to DNA (37). Glucose stimulates ChREBP to bind to an E-box motif in the promoter of liver-type pyruvate kinase (L-PK), a key regulatory enzyme in glycolysis. L-PK catalyzes the conversion of phosphoenolpyruvate to pyruvate, which enters the Krebs cycle to generate citrate, the principal source of acetyl-CoA used for fatty acid synthesis. Recently, ChREBP knockout mice have been developed and characterized (38). As predicted from in vitro studies, the expression of L-PK was reduced by approximately 90% in livers of ChREBP knockout mice. An unexpected finding was that the mRNA levels of all fatty acid synthesis enzymes also were reduced by approximately 50% (38). This suggests that ChREBP can independently stimulate the transcription of all lipogenic genes. Thus, activation of L-PK stimulates both glycolysis and lipogenesis, thereby facilitating the conversion of glucose to fatty acids under conditions of energy excess. Whether inactivation of ChREBP will attenuate the development of fatty livers in insulin-resistant states is currently under investigation; however, it seems likely that excessive stimulation of lipogenesis by ChREBP stimulation would be important only after the development of hyperglycemia.
A third transcription factor that participates in the development of hepatic steatosis in rodents is PPAR-γ. PPAR-γ is a member of the nuclear hormone receptor superfamily that is required for normal adipocyte differentiation (39). Normally, PPAR-γ is expressed at very low levels in the liver; however, in animal models with insulin resistance and fatty livers, the expression of PPAR-γ is markedly increased (40, 41). Previous studies have demonstrated that SREBP-1c can transcriptionally activate PPAR-γ, and it has been suggested that SREBP-1c may activate PPAR-γ by stimulating production of an activating ligand for the nuclear receptor (42, 43).
The importance of PPAR-γ expression in the development of fatty livers has been demonstrated by the development of liver-specific gene deletions of Ppar-γ in two different insulin-resistant mouse models, the ob/ob mouse and the lipodystrophic transgenic mouse, named AZIP/F-1. AZIP-F-1 mice are insulin resistant due to a near absence of white adipose tissue and leptin deficiency (41). The genetic deletion of hepatic PPAR-γ in livers of either ob/ob (44) or AZIP-F-1 (45) mice markedly attenuates the development of hepatic steatosis, independent of the presence of hyperinsulinemia or hyperglycemia.
The precise molecular events mediated by PPAR-γ that promote triglyceride deposition in the liver have not been fully defined. It is also not known whether PPAR-γ expression is increased in human livers with steatosis.
AMP-activated protein kinase and hepatic steatosis
AMP-activated protein kinase (AMPK) is a heterotrimeric protein that serves as a sensor of cellular energy levels (46). AMPK is activated by increased cellular AMP levels, a marker of decreased cellular energy stores. Activated AMPK stimulates ATP-producing catabolic pathways, such as fatty acid β oxidation, and inhibits ATP-consuming processes, such as lipogenesis, directly by phosphorylating regulatory proteins and indirectly by affecting expression levels of genes in these pathways (46).
The fatty acid composition of liver can also influence the amount of triglyceride that accumulates by altering AMPK activity. The genetic deletion of SCD-1, an enzyme responsible for the synthesis of monounsaturated fatty acids, protects against the development of fatty livers and insulin resistance in mice (47, 48). In the absence of SCD-1, AMPK is activated (49), resulting in phosphorylation and inhibition of both ACC (50) and ChREBP (51) as well as a reduction in the expression levels of SREBP-1c (52).
The antidiabetic drug metformin also activates hepatic AMPK (52). Treatment of ob/ob mice with metformin markedly reduced hepatic steatosis (53), and its administration to humans with NASH improved LFT numbers and decreased liver size (54). A second class of antidiabetic drugs, the thiazolidinediones, are principally recognized as drugs that activate PPAR-γ; however, recent data suggest that they also can activate AMPK (55, 56). Pilot studies in humans using pioglitazone (57, 58) and rosiglitazone (59) have demonstrated the efficacy of these agents in reducing hepatic fat, presumably as a consequence of the molecular events summarized in Figure 2.
Figure 2.
Consequences of hepatic AMPK activation. The pharmacologic agents, metformin and thiazolidinediones (TZDs), activate AMPK in the liver. In addition, the deletion of SCD results in AMPK activation through an undetermined mechanism. The activation of AMPK reduces lipogenesis through three independent mechanisms. Activated AMPK phosphorylates and inhibits the activity of ACC, which reduces malonyl-CoA formation. ChREBP is phosphorylated by activated AMPK, which inhibits its entry into the nucleus, thus suppressing L-PK and lipogenic gene expression. SREBP-1c expression is reduced by activated AMPK through undefined mechanisms. The cumulative result of AMPK activation, whether by drugs or through the deletion of SCD, is a reduction in fatty acid synthesis, decreased malonyl-CoA concentrations, and increased CPT-1 activity, resulting in increased fatty acid oxidation.
Taken together, these studies suggest that increased hepatic lipogenesis is an important metabolic abnormality underlying the pathogenesis of hepatic steatosis in insulin-resistant livers. Increased lipogenesis may actually cause dual metabolic alterations that lead to increased hepatic triglyceride content. The first alteration is direct — through the increased synthesis of triglycerides. The second is indirect — through increased production of malonyl-CoA, which inhibits CPT-1 and fatty acid entry into the mitochondria, thus reducing β oxidation and enhancing fatty acid and triglyceride accumulation (Figure 1).
It is important to note that the concept that endogenous fatty acid synthesis contributes significantly to hepatic steatosis is based on data from the studies of mice. Stable-isotope studies in humans suggest that de novo hepatic fatty acid synthesis contributes only modestly to the amount of triglycerides synthesized in liver (60). Although there is evidence that de novo hepatic fatty acid synthesis is increased in humans with insulin resistance (61), the overall importance of this pathway in the development of hepatic steatosis remains to be determined.
Disease progression: steatosis to NASH
According to the two-hit hypothesis, hepatic steatosis is a prerequisite for subsequent events that lead to liver injury (5). Despite the high prevalence of NAFLD and its potential for serious sequelae, the underlying etiological factors that determine disease progression to cirrhosis remain poorly understood. Studies to clearly define the molecular and physiologic changes that mediate the presumed transition from hepatic steatosis to NASH have been limited by several factors. First, no animal models incorporate all features of human steatohepatitis. Second, the available noninvasive techniques to study hepatic metabolism in humans are limited. Third, liver biopsies are required to identify individuals with NASH, precluding large population-based studies. Therefore, our current understanding of the mechanisms by which hepatic steatosis progresses to NASH is based almost exclusively on correlative data from animal models. How well these animal models reflect the human pathophysiology of NASH is not known.
NASH is histologically similar to alcohol-induced steatohepatitis, a disease that can progress to cirrhosis and liver failure. Many of the factors implicated in the development of alcoholic steatohepatitis are also associated with NASH. These factors can be grouped into two broad categories: factors causing an increase in oxidative stress and factors promoting expression of proinflammatory cytokines. Although there is considerable evidence implicating cytokines in the development of NASH, the focus here will be on the potential role of lipid-induced cellular injury in the development of NASH.
Oxidative stress
Oxidative stress results from an imbalance between pro-oxidant and antioxidant chemical species that leads to oxidative damage of cellular macromolecules (62). The predominant pro-oxidant chemicals in fatty livers are singlet oxygen molecules, superoxide anions, hydrogen peroxide, and hydroxyl radicals: molecules collectively referred to as reactive oxygen species (ROS). As depicted in Figure 3, the oxidation of fatty acids is an important source of ROS in fatty livers (63–66). Some of the consequences of increased ROS include depletion of ATP and nicotinamide dinucleotide, DNA damage, alterations in protein stability, the destruction of membranes via lipid peroxidation, and the release of proinflammatory cytokines (62, 67). Increased production of ROS in the presence of excess FFAs has been validated in animal models of NASH (66, 68). Human livers with NASH have increased levels of by-products of lipid peroxidation, providing further evidence of an increase in oxidative stress in this condition (69).
Figure 3.
Mechanisms of lipid-induced cellular injury in NAFLD. ROS are formed through oxidative processes within the cell. In the mitochondria, impaired MRC activity leads to the formation of superoxide anions and hydrogen peroxide. The accumulation of fatty acids in the cytosol increases fatty acid oxidation in peroxisomes and the ER. The initial reaction in peroxisomal β oxidation is catalyzed by acyl-CoA oxidase (AOX) that forms hydrogen peroxide through the donation of electrons to molecular oxygen. Microsomal w oxidation is catalyzed by cytochrome P450 (CYP) enzymes 2E1, 4A10, and 4A14, which form ROS through flavoprotein-mediated donation of electrons to molecular oxygen. PUFAs are extremely susceptible to lipid peroxidation by ROS. By-products of PUFA peroxidation are aldehydes, such as HNE and MDA. These aldehydes are themselves cytotoxic and can freely diffuse into the extracellular space to affect distant cells. ROS and aldehydes induce oxidative stress and cell death via ATP and NAD depletion, DNA and protein damage, and glutathione depletion. Additionally, they induce inflammation through the production of proinflammatory cytokines, leading to neutrophil chemotaxis. Within the extracellular space, HNE and MDA are themselves potent chemoattractants for neutrophils. Finally, ROS and products of lipid peroxidation can lead to fibrosis by activating hepatic stellate cells, which synthesize collagen and perpetuate the inflammatory response.
Mitochondrial dysfunction
Mitochondrial β oxidation is the dominant oxidative pathway for the disposition of fatty acids under normal physiologic conditions but can also be a major source of ROS (70). Several lines of evidence suggest that mitochondrial function is impaired in patients with NASH. Ultrastructural mitochondrial abnormalities have been documented in patients with NASH (71). Similar mitochondrial lesions are found in liver biopsy specimens from patients treated with 4,4′-diethylaminoethoxyhexestrol, a drug that inhibits mitochondrial respiratory chain (MRC) activity and mitochondrial β oxidation (72). Prolonged treatment with this agent is associated with hepatic steatosis and steatohepatitis that is histologically indistinguishable from NAFLD in humans (72). The ultrastructural mitochondrial defects in patients with NAFLD may be indicative of defective oxidative-phosphorylation, inasmuch as these patients also have reduced MRC activity (73) and impaired ATP synthesis after a fructose challenge (74). MRC dysfunction can directly lead to the production of ROS. If electron flow is interrupted at any point in the respiratory chain, the preceding respiratory intermediates can transfer electrons to molecular oxygen to produce superoxide anions and hydrogen peroxide (65, 66).
As the oxidative capacity of the mitochondria becomes impaired, cytosolic fatty acids accumulate. Alternative pathways in the peroxisomes (β oxidation) and in microsomes (w oxidation) are activated, resulting in the formation of additional ROS (72, 75, 76). In the initial step of peroxisomal β oxidation, hydrogen peroxide is formed by the action of acyl-CoA oxidase, which donates electrons directly to molecular oxygen (64). Microsomal w oxidation of fatty acids, catalyzed primarily by cytochrome P450 enzymes 2E1, 4A10, and 4A14, forms ROS through flavoprotein-mediated donation of electrons to molecular oxygen (63). Additionally, dicarboxylic acids, another product of microsomal fatty acid w oxidation, can impair mitochondrial function by uncoupling oxidative-phosphorylation (77). Protonated dicarboxylic acids cycle from the inner to the outer mitochondrial membrane, resulting in dissipation of the mitochondrial proton gradient without concomitant ATP production (78). The cumulative effect of extramitochondrial fatty acid oxidation is a further increase in oxidative stress and mitochondrial impairment.
Lipid peroxidation
ROS are relatively short-lived molecules that exert local effects (79). However, they can attack polyunsaturated fatty acids (PUFAs) and initiate lipid peroxidation within the cell (79), which results in the formation of aldehyde by-products such as trans-4-hydroxy-2-nonenal (HNE) and malondialdehyde (MDA). These molecules have longer half-lives than ROS and have the potential to diffuse from their site of origin to reach distant intracellular and extracellular targets, thereby amplifying the effects of oxidative stress. The formation of HNE and MDA occurs only through the peroxidation of PUFAs (79), which are preferentially oxidized owing to decreased carbon-hydrogen bond strength in methylene groups between unsaturated carbon pairs (80). As the number of double bonds in PUFAs increase, their rate of peroxidation increases exponentially (81). Mitochondria have a substantial concentration of phospholipids containing docosahexaenoic, which may be essential for functional assembly of the MRC (82). Peroxidation of these mitochondrial membrane components could lead to further diminution of MRC activity and increased cellular oxidative stress. Additionally, the peroxidation of PUFAs has also been shown to enhance postendoplasmic reticulum presecretory proteolysis of ApoB, thereby attenuating VLDL secretion in rodents (83). The reduction in VLDL secretion may further contribute to triglyceride accumulation in the liver.
In addition to the deleterious effects of lipid peroxidation on organelle function, aldehydes formed through peroxidation of PUFAs also are detrimental to cellular homeostasis. They impair nucleotide and protein synthesis, deplete the natural antioxidant glutathione, increase production of the proinflammatory cytokine TNF-α, promote influx of inflammatory cells into the liver, and activate stellate cells, leading to collagen deposition, fibrosis, and the perpetuation of the inflammatory response (reviewed in refs. 79, 84). These effects have the potential to directly induce hepatocyte death and necrosis, inflammation, and liver fibrosis: all of the histologic hallmarks of NASH.
Conclusions
Over the past 5 years, substantial progress has been made in identifying the molecular and physiologic changes that cause hepatic steatosis. The transcription factors that control hepatic lipid metabolism have been identified. The elucidation of these physiologic alterations that lead to hepatic steatosis in mice now permit directed studies in humans using newer techniques such as mass isotopomer distribution analysis to measure fluxes through involved metabolic pathways. The major unresolved question is the nature of the relationship between hepatic steatosis and NASH. Although there is abundant evidence to suggest that increased liver triglycerides lead to increased oxidative stress in the hepatocytes of animals and humans (16, 63, 66, 68, 69), an unequivocal cause-and-effect relationship between hepatic triglyceride accumulation, oxidative stress, and the progression of hepatic steatosis to NASH remains to be established in humans. Longitudinal studies also are needed to define the true natural history of NAFLD and to delineate the key components of NAFLD progression. Thus the combined efforts of clinician-investigators and basic scientists will be required to advance our understanding of the progression of this disease. Elucidation of the molecular mechanisms underlying the development of NASH will facilitate the development of specific interventions aimed at preventing the progression of NAFLD.
Acknowledgments
Support for the research cited from the authors’ laboratory was provided by grants from the NIH (HL-20948 and HL-38049) and the Perot Family Foundation. J.D. Horton is a Pew Scholar in the biomedical sciences. J.D. Browning is supported by a post-doctoral fellowship award from the American Liver Foundation and NIH training grant T32-DK-07745. The authors wish to thank Jonathan Cohen, Helen Hobbs, and Joseph Goldstein for critical reading of the manuscript.
Footnotes
Nonstandard abbreviations used: acetyl-CoA carboxylase (ACC); AMP-activated protein kinase (AMPK); basic helix-loop-helix-leucine zipper (bHLH-Zip); carbohydrate response element binding protein (ChREBP); carnitine palmitoyl transferase-1 (CPT-1); diethylaminoethoxyhexestrol (DEAEH); liver function test (LFT); liver-type pyruvate kinase (L-PK); malondialdehyde (MDA); mitochondrial respiratory chain (MRC); nonalcoholic fatty-liver disease (NAFLD); nonalcoholic steatohepatitis (NASH); polyunsaturated fatty acid (PUFA); reactive oxygen species (ROS); stearoyl-CoA desaturase (SCD); trans-4-hydroxy-2-nonenal (HNE).
Conflict of interest: The authors have declared that no conflict of interest exists.
References
- 1.Neuschwander-Tetri B, Caldwell S. Nonalcoholic steatohepatitis:summary of an AASLD single topic conference. Hepatology. 2003;37:1202–1219. doi: 10.1053/jhep.2003.50193. [DOI] [PubMed] [Google Scholar]
- 2.Clark JM, Brancati FL, Diehl AM. The prevalence and etiology of elevated aminotransferase levels in the United States. Am. J. Gastroenterol. 2003;98:960–967. doi: 10.1111/j.1572-0241.2003.07486.x. [DOI] [PubMed] [Google Scholar]
- 3.Angulo P. Nonalcoholic fatty liver disease. N. Engl. J. Med. 2002;346:1221–1231. doi: 10.1056/NEJMra011775. [DOI] [PubMed] [Google Scholar]
- 4.Marchesini G, et al. Nonalcoholic fatty liver disease a feature of the metabolic syndrome. Diabetes. 2001;50:1844–1850. doi: 10.2337/diabetes.50.8.1844. [DOI] [PubMed] [Google Scholar]
- 5.Day CP, James OFW. Steatohepatitis: a tale of two “hits”? Gastroenterology. 1998;114:842–845. doi: 10.1016/s0016-5085(98)70599-2. [DOI] [PubMed] [Google Scholar]
- 6.Nomura H, et al. Prevalence of fatty liver in a general population in Okinawa, Japan. Jpn. J. Med. 1988;27:142–149. doi: 10.2169/internalmedicine1962.27.142. [DOI] [PubMed] [Google Scholar]
- 7.Hilden M, Christoffersen P, Juhl E, Dalgaard JB. Liver histology in a “normal” population — examination of 503 consecutive fatal traffic casualties. Scand. J. Gastroenterol. 1977;12:593–597. doi: 10.3109/00365527709181339. [DOI] [PubMed] [Google Scholar]
- 8.Bellentani S, et al. Prevalence of and risk factors for hepatic steatosis in northern Italy. Ann. Intern. Med. 2000;132:112–117. doi: 10.7326/0003-4819-132-2-200001180-00004. [DOI] [PubMed] [Google Scholar]
- 9.Flegal KM, Ogden CL, Wei R, Kuczmarski RL, Johnson CL. Prevalence of overweight in US children: comparison of US growth charts from the Centers for Disease Control and Prevention with other reference values for body mass index. Am. J. Clin. Nutr. 2001;73:1086–1093. doi: 10.1093/ajcn/73.6.1086. [DOI] [PubMed] [Google Scholar]
- 10.Rashid M, Roberts EA. Nonalcoholic steatohepatitis in children. J. Pediatr. Gastroenterol. Nutr. 2000;30:48–52. doi: 10.1097/00005176-200001000-00017. [DOI] [PubMed] [Google Scholar]
- 11.Browning JD, Kumar KS, Saboorian MH, Thiele DL. Ethnic differences in the prevalence of cryptogenic cirrhosis. Am. J. Gastroenterol. 2004;99:292–298. doi: 10.1111/j.1572-0241.2004.04059.x. [DOI] [PubMed] [Google Scholar]
- 12.Caldwell SH, Harris DM, Patrie JT, Hespenheide EE. Is NASH underdiagnosed among African Americans? Am. J. Gastroenterol. 2002;97:1496–1500. doi: 10.1111/j.1572-0241.2002.05795.x. [DOI] [PubMed] [Google Scholar]
- 13.Lewis GF, Carpentier A, Adeli K, Giacca A. Disordered fat storage and mobilization in the pathogenesis of insulin resistance and type 2 diabetes. Endocr. Rev. 2002;23:201–229. doi: 10.1210/edrv.23.2.0461. [DOI] [PubMed] [Google Scholar]
- 14.Wahren J, Sato Y, Ostman J, Hagenfeldt L, Felig P. Turnover and splanchnic metabolism of free fatty acids and ketones in insulin-dependent diabetics at rest and in response to exercise. J. Clin. Invest. 1984;73:1367–1376. doi: 10.1172/JCI111340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Horton JD, Goldstein JL, Brown MS. SREBPs: activators of the complete program of cholesterol and fatty acid synthesis in the liver. J. Clin. Invest. 2002;109:1125–1131. doi:10.1172/JCI200215593. doi: 10.1172/JCI15593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Araya J, et al. Increase in long-chain polyunsaturated fatty acid n-6/n-3 ratio in relation to hepatic steatosis in patients with non-alcoholic fatty liver disease. Clin. Sci. (Lond). 2004;106:635–643. doi: 10.1042/CS20030326. [DOI] [PubMed] [Google Scholar]
- 17.Shimomura I, Shimano H, Korn BS, Bashmakov Y, Horton JD. Nuclear sterol regulatory element-binding proteins activate genes responsible for the entire program of unsaturated fatty acid biosynthesis in transgenic mouse liver. J. Biol. Chem. 1998;273:35299–35306. doi: 10.1074/jbc.273.52.35299. [DOI] [PubMed] [Google Scholar]
- 18.Koo S-H, Dutcher AK, Towle HC. Glucose and insulin function through two distinct transcription factors to stimulate expression of lipogenic enzyme genes in liver. J. Biol. Chem. 2001;276:9437–9445. doi: 10.1074/jbc.M010029200. [DOI] [PubMed] [Google Scholar]
- 19.Stoeckman AK, Towle HC. The role of SREBP-1c in nutritional regulation of lipogenic enzyme gene expression. J. Biol. Chem. 2002;277:27029–27035. doi: 10.1074/jbc.M202638200. [DOI] [PubMed] [Google Scholar]
- 20.Shimomura I, et al. Insulin selectively increases SREBP-1c mRNA in the livers of rats with streptozotocin-induced diabetes. Proc. Natl. Acad. Sci. U. S. A. 1999;96:13656–13661. doi: 10.1073/pnas.96.24.13656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Foretz M, Guichard C, Ferre P, Foufelle F. Sterol regulatory element binding protein-1c is a major mediator of insulin action on the hepatic expression of glucokinase and lipogenesis-related genes. Proc. Natl. Acad. Sci. U. S. A. 1999;96:12737–12742. doi: 10.1073/pnas.96.22.12737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Brown MS, Goldstein JL. The SREBP pathway: regulation of cholesterol metabolism by proteolysis of a membrane-bound transcription factor. Cell. 1997;89:331–340. doi: 10.1016/s0092-8674(00)80213-5. [DOI] [PubMed] [Google Scholar]
- 23.Horton JD, et al. Combined analysis of oligonucleotide microarray data from transgenic and knockout mice identifies direct SREBP target genes. Proc. Natl. Acad. Sci. U. S. A. 2003;100:12027–12032. doi: 10.1073/pnas.1534923100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Shimano H, et al. Isoform 1c of sterol regulatory element binding protein is less active than isoform 1a in livers of transgenic mice and in cultured cells. J. Clin. Invest. 1997;99:846–854. doi: 10.1172/JCI119248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Shimomura I, Bashmakov Y, Horton JD. Increased levels of nuclear SREBP-1c associated with fatty livers in two mouse models of diabetes mellitus. J. Biol. Chem. 1999;274:30028–30032. doi: 10.1074/jbc.274.42.30028. [DOI] [PubMed] [Google Scholar]
- 26.Martin RJ. In vivo lipogenesis, and enzyme levels in adipose tissue and liver tissues from pair-fed genetically obese and lean rats. Life Sci. 1974;14:1447–1453. doi: 10.1016/0024-3205(74)90155-6. [DOI] [PubMed] [Google Scholar]
- 27.Memon RA, Grunfeld C, Moser AH, Feingold KR. Fatty acid synthesis in obese insulin resistant diabetic mice. Horm. Metab. Res. 1994;26:85–87. doi: 10.1055/s-2007-1000778. [DOI] [PubMed] [Google Scholar]
- 28.Lam TKT, et al. Mechanisms of the free fatty acid-induced increase in hepatic glucose production. Am. J. Physiol. Endocrinol. Metab. 2003;284:E863–E873. doi: 10.1152/ajpendo.00033.2003. [DOI] [PubMed] [Google Scholar]
- 29.Halaas JL, et al. Weight-reducing effects of the plasma protein encoded by the obese gene. Science. 1995;269:543–546. doi: 10.1126/science.7624777. [DOI] [PubMed] [Google Scholar]
- 30.Yahagi N, et al. Absence of sterol regulatory element-binding protein-1 (SREBP-1) ameliorates fatty livers but not obesity or insulin resistance in Lepob/Lepob mice. J. Biol. Chem. 2002;277:19353–19357. doi: 10.1074/jbc.M201584200. [DOI] [PubMed] [Google Scholar]
- 31.Abu-Elheiga L, et al. The subcellular localization of acetyl-CoA carboxylase 2. Proc. Natl. Acad. Sci. U. S. A. 2000;97:1444–1449. doi: 10.1073/pnas.97.4.1444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.McGarry JD, Mannaerts GP, Foster DW. A possible role for malonyl-CoA in the regulation of hepatic fatty acid oxidation and ketogenesis. J. Clin. Invest. 1977;60:265–270. doi: 10.1172/JCI108764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Abu-Elheiga L, Matzuk MM, Abo-Hashema KAH, Wakil SJ. Continuous fatty acid oxidation and reduced fat storage in mice lacking acetyl-CoA carboxylase 2. Science. 2001;291:2613–2616. doi: 10.1126/science.1056843. [DOI] [PubMed] [Google Scholar]
- 34.Abu-Elheiga L, Oh W, Kordari P, Wakil SJ. Acetyl-CoA carboxylase 2 mutant mice are protected against obesity and diabetes induced by high-fat/high-carbohydrate diets. Proc. Natl. Acad. Sci. U. S. A. 2003;100:10207–10212. doi: 10.1073/pnas.1733877100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.An J, et al. Hepatic expression of malonyl-CoA decarboxylase reverses muscle, liver and whole-animal insulin resistance. Nat. Med. 2004;10:268–274. doi: 10.1038/nm995. [DOI] [PubMed] [Google Scholar]
- 36.Yamashita H, et al. A glucose-responsive transcription factor that regulates carbohydrate metabolism in the liver. Proc. Natl. Acad. Sci. U. S. A. 2001;98:9116–9121. doi: 10.1073/pnas.161284298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kawaguchi T, Osatomi K, Yamashita H, Kabashima T, Uyeda K. Mechanism for fatty acid “sparing” effect on glucose-induced transcription. Regulation of carbohydrate-responsive element-binding protein by Amp-activated protein kinase. J. Biol. Chem. 2002;277:3829–3835. doi: 10.1074/jbc.M107895200. [DOI] [PubMed] [Google Scholar]
- 38.Iizuka, K., Bruick, R.K., Liang, G., Horton, J.D., and Uyeda, K. 2004. Deficiency of carbohydrate response element binding protein (ChREBP) reduces lipogenesis as well as glycolysis. Proc. Nat. Acad. Sci. U. S. A. In press. [DOI] [PMC free article] [PubMed]
- 39.Tontonoz P, Hu E, Spiegelman BM. Stimulation of adipogenesis in fibroblasts by PPAR gamma 2, a lipid-activated transcription factor. Cell. 1994;79:1147–1156. doi: 10.1016/0092-8674(94)90006-x. [DOI] [PubMed] [Google Scholar]
- 40.Edvardsson U, et al. Rosiglitazone (BRL49653), a PPARgamma-selective agonist, causes peroxisome proliferator-like liver effects in obese mice. J. Lipid. Res. 1999;40:1177–1184. [PubMed] [Google Scholar]
- 41.Chao L, et al. Adipose tissue is required for the antidiabetic, but not for the hypolipidemic, effect of thiazolidinediones. J. Clin. Invest. 2000;106:1221–1228. doi: 10.1172/JCI11245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kim JB, Wright HM, Wright M, Spiegelman BM. ADD1/SREBP-1 activates PPAR gamma through the production of endogenous ligand. Proc. Natl. Acad. Sci. U. S. A. 1998;95:4333–4337. doi: 10.1073/pnas.95.8.4333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Fajas L, et al. Regulation of peroxisome proliferator-activated receptor gamma expression by adipocyte differentiation and determination factor 1/sterol regulatory element binding protein 1: implications for adipocyte differentiation and metabolism. Mol. Cell. Biol. 1999;19:5495–5503. doi: 10.1128/mcb.19.8.5495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Matsusue K, et al. Liver-specific disruption of PPARgamma in leptin-deficient mice improves fatty liver but aggravates diabetic phenotypes. J. Clin. Invest. 2003;111:737–747. doi:10.1172/JCI200317223. doi: 10.1172/JCI17223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Gavrilova O, et al. Liver peroxisome proliferator-activated receptor gamma contributes to hepatic steatosis, triglyceride clearance, and regulation of body fat mass. J. Biol. Chem. 2003;278:34268–34276. doi: 10.1074/jbc.M300043200. [DOI] [PubMed] [Google Scholar]
- 46.Hardie DG. Minireview: The AMP-activated protein kinase cascade: the key sensor of cellular energy status. Endocrinology. 2003;144:5179–5183. doi: 10.1210/en.2003-0982. [DOI] [PubMed] [Google Scholar]
- 47.Cohen P, et al. Role for stearoyl-CoA desaturase-1 in leptin-mediated weight loss. Science. 2002;297:240–243. doi: 10.1126/science.1071527. [DOI] [PubMed] [Google Scholar]
- 48.Ntambi JM, et al. Loss of stearoyl-CoA desaturase-1 function protects mice against adiposity. Proc. Natl. Acad. Sci. U. S. A. 2002;99:11482–11486. doi: 10.1073/pnas.132384699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Dobrzyn P, et al. Stearoyl-CoA desaturase 1 deficiency increases fatty acid oxidation by activating AMP-activated protein kinase in liver. Proc. Natl. Acad. Sci. U. S. A. 2004;101:6409–6414. doi: 10.1073/pnas.0401627101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Hardie DG, Scott JW, Pan DA, Hudson ER. Management of cellular energy by the AMP-activated protein kinase system. FEBS Lett. 2003;546:113–120. doi: 10.1016/s0014-5793(03)00560-x. [DOI] [PubMed] [Google Scholar]
- 51.Kawaguchi T, Takenoshita M, Kabashima T, Uyeda K. Glucose and cAMP regulate the L-type pyruvate kinase gene by phosphorylation/dephosphorylation of the carbohydrate response element binding protein. Proc. Natl. Acad. Sci. U. S. A. 2001;98:13710–13715. doi: 10.1073/pnas.231370798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Zhou G, et al. Role of AMP-activated protein kinase in mechanism of metformin action. J. Clin. Invest. 2001;108:1167–1174. doi:10.1172/JCI200113505. doi: 10.1172/JCI13505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Lin HZ, et al. Metformin reverses fatty liver disease in obese, leptin-deficient mice. Nat. Med. 2000;6:998–1003. doi: 10.1038/79697. [DOI] [PubMed] [Google Scholar]
- 54.Marchesini G, et al. Metformin in non-alcoholic steatohepatitis. Lancet. 2001;358:893–894. doi: 10.1016/s0140-6736(01)06042-1. [DOI] [PubMed] [Google Scholar]
- 55.Fryer LG, Parbu-Patel A, Carling D. The anti-diabetic drugs rosiglitazone and metformin stimulate AMP-activated protein kinase through distinct signaling pathways. J. Biol. Chem. 2002;277:25226–25232. doi: 10.1074/jbc.M202489200. [DOI] [PubMed] [Google Scholar]
- 56.Saha AK, et al. Pioglitazone treatment activates AMP-activated protein kinase in rat liver and adipose tissue in vivo. Biochem. Biophys. Res. Commun. 2004;314:580–585. doi: 10.1016/j.bbrc.2003.12.120. [DOI] [PubMed] [Google Scholar]
- 57.Bajaj M, et al. Pioglitazone reduces hepatic fat content and augments splanchnic glucose uptake in patients with type 2 diabetes. Diabetes. 2003;52:1364–1370. doi: 10.2337/diabetes.52.6.1364. [DOI] [PubMed] [Google Scholar]
- 58.Promrat K, et al. A pilot study of pioglitazone treatment for nonalcoholic steatohepatitis. Hepatology. 2004;39:188–196. doi: 10.1002/hep.20012. [DOI] [PubMed] [Google Scholar]
- 59.Neuschwander-Tetri BA, et al. Improved nonalcoholic steatohepatitis after 48 weeks of treatment with the PPAR-gamma ligand rosiglitazone. Hepatology. 2003;38:1008–1017. doi: 10.1053/jhep.2003.50420. [DOI] [PubMed] [Google Scholar]
- 60.Hellerstein MK, Schwarz JM, Neese RA. Regulation of hepatic de novo lipogenesis in humans. Annu. Rev. Nutr. 1996;16:523–557. doi: 10.1146/annurev.nu.16.070196.002515. [DOI] [PubMed] [Google Scholar]
- 61.Diraison F, Dusserre E, Vidal H, Sothier M, Beylot M. Increased hepatic lipogenesis but decreased expression of lipogenic gene in adipose tissue in human obesity. Am. J. Physiol. Endocrinol. Metab. 2002;282:E46–E51. doi: 10.1152/ajpendo.2002.282.1.E46. [DOI] [PubMed] [Google Scholar]
- 62.Robertson G, Leclercq I, Farrell GC. Nonalcoholic steatosis and steatohepatitis: II. Cytochrome P-450 enzymes and oxidative stress. Am. J. Physiol. Gastrointest. Liver Physiol. 2001;281:G1135–G1139. doi: 10.1152/ajpgi.2001.281.5.G1135. [DOI] [PubMed] [Google Scholar]
- 63.Lieber CS. CYP2E1: from ASH to NASH. Hepatol. Res. 2004;28:1–11. doi: 10.1016/j.hepres.2003.08.001. [DOI] [PubMed] [Google Scholar]
- 64.Mannaerts GP, Van Veldhoven PP, Casteels M. Peroxisomal lipid degradation via beta- and alpha-oxidation in mammals. Cell Biochem. Biophys. 2000;32:73–87. doi: 10.1385/cbb:32:1-3:73. [DOI] [PubMed] [Google Scholar]
- 65.Garcia-Ruiz C, Colell A, Morales A, Kaplowitz N, Fernandez-Checa JC. Role of oxidative stress generated from the mitochondrial electron transport chain and mitochondrial glutathione status in loss of mitochondrial function and activation of transcription factor nuclear factor-kappa B: studies with isolated mitochondria and rat hepatocytes. Mol. Pharmacol. 1995;48:825–834. [PubMed] [Google Scholar]
- 66.Hensley K, et al. Dietary choline restriction causes complex I dysfunction and increased H(2)O(2) generation in liver mitochondria. Carcinogenesis. 2000;21:983–989. doi: 10.1093/carcin/21.5.983. [DOI] [PubMed] [Google Scholar]
- 67.Bergamini CM, Gambetti S, Dondi A, Cervellati C. Oxygen, reactive oxygen species and tissue damage. Curr. Pharm. Des. 2004;10:1611–1626. doi: 10.2174/1381612043384664. [DOI] [PubMed] [Google Scholar]
- 68.Yang S, et al. Mitochondrial adaptations to obesity-related oxidant stress. Arch. Biochem. Biophys. 2000;378:259–268. doi: 10.1006/abbi.2000.1829. [DOI] [PubMed] [Google Scholar]
- 69.Seki S, et al. In situ detection of lipid peroxidation and oxidative DNA damage in non-alcoholic fatty liver diseases. J. Hepatol. 2002;37:56–62. doi: 10.1016/s0168-8278(02)00073-9. [DOI] [PubMed] [Google Scholar]
- 70.Reddy JK, Mannaerts GP. Peroxisomal lipid metabolism. Annu. Rev. Nutr. 1994;114:343–370. doi: 10.1146/annurev.nu.14.070194.002015. [DOI] [PubMed] [Google Scholar]
- 71.Caldwell SH, et al. Mitochondrial abnormalities in non-alcoholic steatohepatitis. J. Hepatol. 1999;31:430–434. doi: 10.1016/s0168-8278(99)80033-6. [DOI] [PubMed] [Google Scholar]
- 72.Berson A, et al. Steatohepatitis-inducing drugs cause mitochondrial dysfunction and lipid peroxidation in rat hepatocytes. Gastroenterology. 1998;114:764–774. doi: 10.1016/s0016-5085(98)70590-6. [DOI] [PubMed] [Google Scholar]
- 73.Perez-Carreras M, et al. Defective hepatic mitochondrial respiratory chain in patients with nonalcoholic steatohepatitis. Hepatology. 2003;38:999–1007. doi: 10.1053/jhep.2003.50398. [DOI] [PubMed] [Google Scholar]
- 74.Cortez-Pinto H, Zhi Lin H, Qi Yang S, Odwin Da Costa S, Diehl AM. Lipids up-regulate uncoupling protein 2 expression in rat hepatocytes. Gastroenterology. 1999;116:1184–1193. doi: 10.1016/s0016-5085(99)70022-3. [DOI] [PubMed] [Google Scholar]
- 75.Johnson EF, Palmer CN, Griffin KJ, Hsu MH. Role of the peroxisome proliferator-activated receptor in cytochrome P450 4A gene regulation. FASEB J. 1996;10:1241–1248. doi: 10.1096/fasebj.10.11.8836037. [DOI] [PubMed] [Google Scholar]
- 76.Kersten S, et al. Peroxisome proliferator-activated receptor alpha mediates the adaptive response to fasting. J. Clin. Invest. 1999;103:1489–1498. doi: 10.1172/JCI6223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Tonsgard JH, Getz GS. Effect of Reye’s syndrome serum on isolated chinchilla liver mitochondria. J. Clin. Invest. 1985;76:816–825. doi: 10.1172/JCI112039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Hermesh O, Kalderon B, Bar-Tana J. Mitochondria uncoupling by a long chain fatty acyl analogue. J. Biol. Chem. 1998;273:3937–3942. doi: 10.1074/jbc.273.7.3937. [DOI] [PubMed] [Google Scholar]
- 79.Esterbauer H, Schaur RJ, Zollner H. Chemistry and biochemistry of 4-hydroxynonenal, malonaldehyde and related aldehydes. Free Radic. Biol. Med. 1991;11:81–128. doi: 10.1016/0891-5849(91)90192-6. [DOI] [PubMed] [Google Scholar]
- 80.Gardner HW. Oxygen radical chemistry of polyunsaturated fatty acids. Free Radic. Biol. Med. 1989;7:65–86. doi: 10.1016/0891-5849(89)90102-0. [DOI] [PubMed] [Google Scholar]
- 81.Wagner BA, Buettner GR, Burns CP. Free radical-mediated lipid peroxidation in cells: oxidizability is a function of cell lipid bis-allylic hydrogen content. Biochemistry. 1994;33:4449–4453. doi: 10.1021/bi00181a003. [DOI] [PubMed] [Google Scholar]
- 82.Infante JP, Huszagh VA. Secondary carnitine deficiency and impaired docosahexaenoic (22:6n-3) acid synthesis: a common denominator in the pathophysiology of diseases of oxidative phosphorylation and beta-oxidation. FEBS Lett. 2000;468:1–5. doi: 10.1016/s0014-5793(00)01083-8. [DOI] [PubMed] [Google Scholar]
- 83.Pan M, et al. Lipid peroxidation and oxidant stress regulate hepatic apolipoprotein B degradation and VLDL production. J. Clin. Invest. 2004;113:1277–1287. doi:10.1172/JCI200419197. doi: 10.1172/JCI19197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Yamauchi T, et al. Globular adiponectin protected ob/ob mice from diabetes and apoE-deficient mice from atherosclerosis. J. Biol. Chem. 2003;278:2461–2468. doi: 10.1074/jbc.M209033200. [DOI] [PubMed] [Google Scholar]