Abstract
Evidence from clinical trials should contribute to informed decision making and a learning health care system. People frequently, however, find participating in clinical trials meaningless or disempowering. Moreover, people often do not incorporate trial results directly into their decision making. The lack of patient centeredness in clinical trials may be partially addressed through trial design. For example, Bayesian adaptive trials designed to adjust in a pre-specified manner to changes in clinical practice could motivate people and their health care providers to view clinical trials as more applicable to real-world clinical decisions. The way in which clinical trials are designed can transform the evidence generation process to be more patient centered, providing people with an incentive to participate or continue participating in clinical trials. In order to achieve the transformation to patient-centeredness in clinical trial decisions, however, there is a need for transparent and reliable methods and education of trial investigators and site personnel.
Keywords: patient-centered, trial design, pragmatic, Bayesian, adaptive, RCT
Introduction
Activated and engaged people are empowered to meaningfully participate in their health care.i When it comes to research, however, people generally participate passively in the learning process; participants usually are involved in clinical trials merely as human subjects rather than as engaged stakeholders. A more patient-centered approach to participant involvement in outcomes research has been proposed, which would lead to the empowerment of participants throughout the research process.ii Study design elements of clinical trials intended for regulatory approval of drugs and health care technologies, however, traditionally do not reflect a patient-centered approach.
Meaningful participant involvement to help produce and disseminate relevant evidence for decision making is made more difficult when the clinical trial experience falls short of the participant’s initial expectations. Individuals may feel comfortable with their participation initially, but may become unsure of their involvement later as they progress through the trial. For instance, although participants in cancer trials are satisfied with their medical care, they are disappointed not to learn more about their disease through their involvement in research, and they find that trial participation takes more time and effort than they thought it would.iii As a result, the application of a patient-centered approach requires more than identifying people who are willing to participate in trials. Many people are, at least in theory, willing to participate in research if the study is convenient and if they are informed of study results.iv
There is no single answer to addressing the divide between expectations and the reality of clinical trial participation. Therefore, improvements to ensure participants are truly providing informed consent must be implemented to address participant-related factors (e.g. mistrust of medical research, hard to reach groups, lack of resources), contextual factors (e.g. cultural traditions), and research-related factors (e.g. likelihood of receiving placebo, risk of harm, inconvenience of protocol).v
Patient-Centeredness through Clinical Trial Design
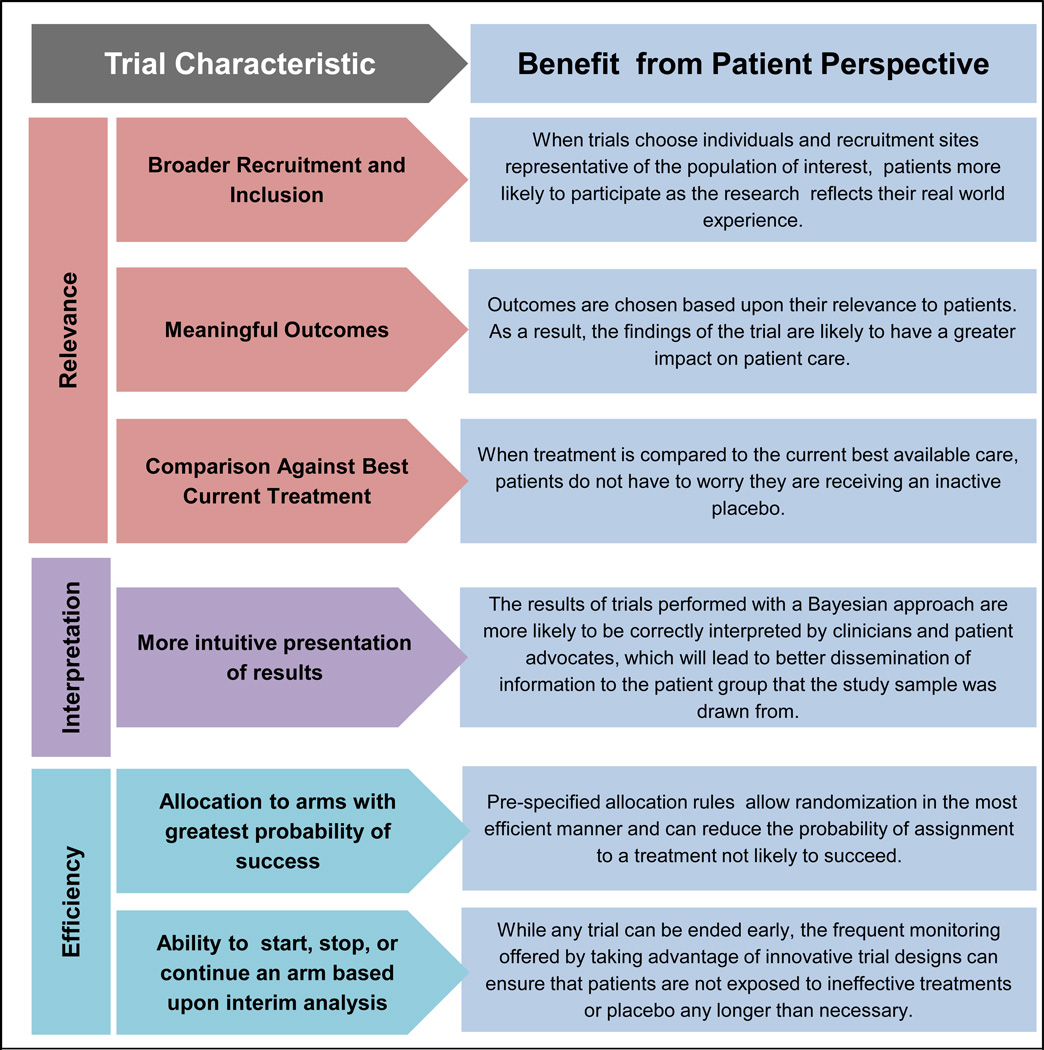
Patient centered outcomes research (PCOR) is designed to “help people and their caregivers communicate and make informed health care decisions, allowing their voices to be heard in assessing the value of health care options”.vi People increasingly want to be informed, empowered, and engaged with their medical management.vii This attitude would carry over to clinical trial participation if many of the concerns regarding the fact that trials are not “patient centered” could be addressed. Providing better information to participants and incorporating alternative trial designs are ways to minimize these concerns. In this commentary, we discuss the potential for pragmatic, Bayesian, and adaptive trial designs to enhance patient centeredness within a clinical trial setting. There are characteristics specific to pragmatic, Bayesian, and adaptive clinical trials that offer potential improvements to the clinical trial process, which frequently is neither patient centered (in terms of the evidence generated, population studied) nor patient friendly (in terms of meeting information needs). The goal is to consider the viewpoint of participants, rather than trialists or other stakeholders, and to supplement the wealth of literature on these trial designs that document the benefits to other, non-participant, stakeholders. Figure 1 illustrates these characteristics and their corresponding benefits in terms of relevance, transparency, and efficiency from the perspective of the patient.
Figure 1.
Means by which trials designs can promote recruitment and retention in clinical trials by improving the patient experience.
Pragmatic Trials
Traditional trials recruit highly selected patients seen in specialist environments and meet rigorous inclusion/exclusion criteria such as being free of comorbidities, which might confound the results of the experiment. By contrast, pragmatic trials support the generation of evidence that might be considered more relevant to the real-world decision making of participants than traditional trials.viii Pragmatic trials recruit from a variety of clinical settings and include study participants that reflect the real world population impacted by the condition the treatment aims to address. This means that the participants most likely to benefit from a treatment will be represented in the study and the effect observed in the trial more closely represents what a typical person could expect to experience. Pragmatic trials frequently also support the utilization of outcome measures that are more relevant to participants. Incorporating outcomes that are meaningful to participants increases the likelihood that once the results of a study are made available, people will benefit from the knowledge gained. For example, if a study only examines changes in laboratory values or clinical indicator, it will be unable to help a person decide if a treatment is right for them if that individual is concerned with quality of life issues. Where nothing prevents patient-reported outcomes from being used in traditional trials, historically these types of measures were relatively uncommon or perceived as less important than laboratory values. This is also not to suggest that pragmatic, Bayesian and adaptive trials are prohibited from using laboratory values and clinical indicators; they are simply in a position to support the use of outcomes relevant from a patient perspective. Individuals participating in a pragmatic clinical trial likely will receive the current gold standard of care or the innovative treatment; no patient receives an inactive comparator (placebo) unless there truly are no comparator interventions in use, such as in trials where there is no equipoise between no therapy and the experimental therapy. Consequently, the study results will more accurately inform decisions in the real world where people and their clinicians typically have to make a choice between therapeutic options.
Bayesian Statistics in Trials
Traditional clinical trials provide the statistical likelihood of rejecting a null hypothesis that a treatment is no better than placebo. Bayesian statistics takes an approach that more closely resembles clinical decision making. Physicians use the knowledge gained from individuals they have treated previously as well as from a specific person’s prior visits. Widespread access to the internet has also increased opportunities for people to incorporate the health care experiences of individuals similar to themselves in addition to their own prior health care experiences when choosing which treatment options to pursue or abandon.ix The application of the Bayesian approach to clinical trials is accomplished by quantifying the knowledge surrounding the treatment based upon previously available evidence.x The result of this quantification is called the prior distribution. The prior distribution describes the level of uncertainty associated with the treatment effect among the clinical trial participant and can be updated periodically as data is generated in the trial, much as a patient’s opinion of an intervention can change over the course of treatment. At any pre-specified time during the trial, inference can be drawn from updated or “posterior” beliefs, which present a decision maker with the probability that a hypothesis is true. This dynamic process of building from a foundation of what is already known, learning from new evidence, and updating outcome probability reflects a more real world approach to medical decision making.
Trials utilizing Bayesian methods produce results that are also more easily interpreted than the results from traditional trials based upon frequentist statistics. P-values and confidence intervals from frequentist statistics are designed for statistical inference and are not necessarily applicable to patient-centered clinical decision making. For example, the range between the upper and lower 95% confidence intervals does not predict the next patient’s treatment effect with 95% probability. The interpretation of this confidence interval is that if the experiment is repeated many times, 95% of the confidence intervals generated accordingly will cover the true treatment effect. In contrast, Bayesian methodology offers a direct interpretation for the probability of treatment effects.10 The more intuitive interpretability of Bayesian results, as compared with those presented by traditional frequentist trials, reduces the likelihood of misinterpretation by people and their physicians. As a result, trial findings may be more effectively diffused into routine community practice.
Adaptive Trials
Adaptive trial designs allow features of the trial to change as evidence accrues during the trial. These changes can include the number of participants required for the trial, the process for randomizing participants into different treatments, modifying null hypotheses, and the integration of trials from different phases. Moreover, the target population can also be modified as a trial goes on if a particular subgroup of participants seems to respond or not respond to treatments. Thus, the trials described can improve participant safety over traditional trials by decreasing the likelihood that participants will be exposed to ineffective treatments or placebo any longer than necessary. While traditional trials are always stopped when significant safety concerns arise they do not typically conclude based upon evidence of futility. With adaptive trial designs, the evaluation of the comparative effectiveness for different treatments can be performed during the trial instead of waiting until the end as in traditional clinical trials. This is especially beneficial when the disease state of interest is rare or the trial seeks results from a subgroup of participants that were underrepresented in recruitment. The advantage for rare diseases, when recruiting over a long period of time, is that using new information, such as biomarkers, is especially important as these diseases are often very serious. In the case of an ineffective trial arm, newly enrolled patients can be randomized into the remaining treatments for which equipoise still exists. This process can also improve relevance as it ensures that participants enrolled are receiving clinically appropriate treatments by allowing the entrance of new therapeutic options that become available after the trial is underway.
The nature of Bayesian statistics makes it an ideal modeling tool for adaptive trials. While it is entirely possible to have an adaptive trial without using a Bayesian approach, the continuous learning process offered by Bayesian statistics is a key component behind the increased popularity of the adaptive trial design.xi Adaptive clinical designs allow researchers to modify clinical trials partway through the study by considering information about the treatment effect that has become apparent as the trial progresses. These modifications are based upon rules specified prior to the initiation of the trial and can include: 1) the ability to conclude the trial based upon interim analyses; 2) adjusting sample size; 3) deleting or adding a treatment arm or extending an existing one; and 4) stopping the trial due to evidence of efficacy, futility, or safety.xii The combination of Bayesian principles and the structure of adaptive trials enable adaptations to occur following pre-specified updating as the data accrue and are analyzed in conjunction with the prior evidence.10 Examples of trial adaptations include, but are not limited to, adding an additional arm to reflect changes in clinical practice that occurred following the onset of the trial or utilizing a new biomarker that better predicts the likelihood of a patient responding in order to more effectively allocate patients.
Potential Impact on Trial Recruitment and Retention
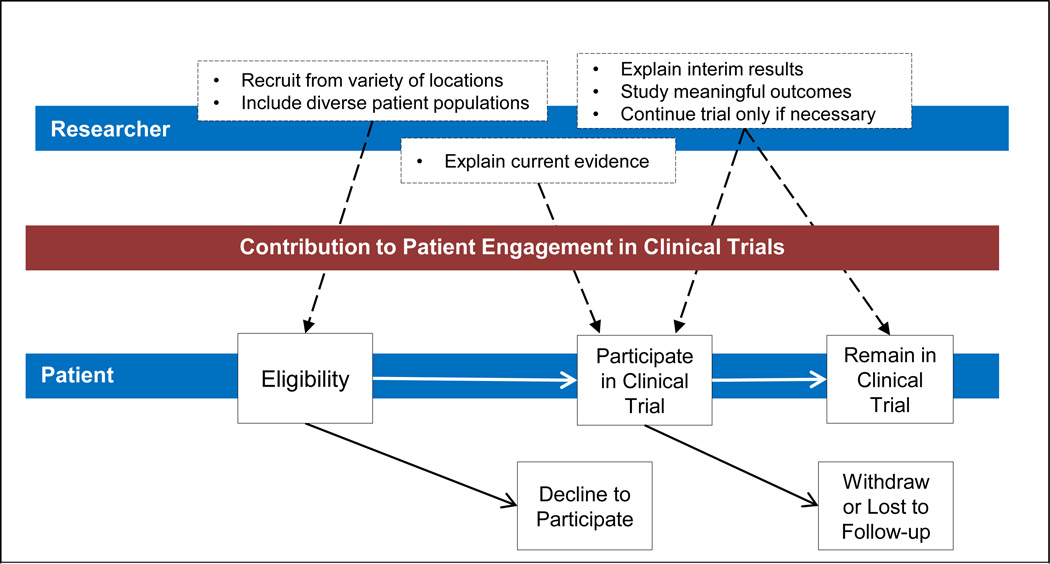
In the words of the Director of the National Institutes of Health: “If clinical trials are to be successful, it is critical that more people get involved”.xiii Through the application of these trial methods, researchers can improve the quality of care and safety for participants in clinical trials and as a result, improve trial recruitment and retention. Figure 2 presents a framework describing the stages at which researchers can incorporate a more patient-centered approach to improve recruitment and retention. Pragmatic, Bayesian, and adaptive trials can improve enrollment by expanding the eligible population for trials based upon prior knowledge. Additionally, where prior information indicates that a trial population should be more narrowly focused, the improved targeted enrollment criteria have the potential to motivate people and physicians to participate as the trial more closely mirrors their unique health care experience. The number of people making the decision to begin and/or continue participating at a given point can be increased if researchers effectively communicate to participants that the trial is not continuing unnecessarily; if results have been found, either of efficacy or futility, the trial will conclude. It is also worth noting that if an a priori stopping rule is imbedded in the study design, the risk of premature stopping, which can occur in traditional trials due to mistakenly lower power calculations, can be mitigated or completely eliminated. Using an approach that allows the inclusion of a broad participant population can provide decision makers with the regulatory approval and evidence necessary to make effective decisions regarding the use of a treatment in subpopulations, such as the elderly, who may be underrepresented in traditional clinical trials.
Figure 2.
A diagram showing points in the clinical trial process (illustrated as dashed lines) where trial design and statistical approaches can impact patient recruitment and retention.
Limitations of our Proposed Approach
The trial designs discussed here offer many advantages from a patient-centered perspective; however, these designs are not without limitations. For example, pragmatic trials, as opposed to traditional, “explanatory” trials, are designed to reflect real world practice, yet there is ambiguity over what constitutes “real world”. Moreover, there is a trade-off to achieving the objectives of pragmatic clinical and adaptive trials including logistical complications attributable to data management and study design as well as potentially exposing manufacturers to a higher level of business risk. Cost and logistical concerns extend to trials that use Bayesian inference. As the FDA discusses in their 2010 Guidance for the Use of Bayesian Statistics in Medical Device Clinical Trials, a Bayesian approach requires a significant investment in the planning and model-building stages, as well as the involvement of experts in statistics/computation.xiv Furthermore, the way in which the informative priors are generated must be “clinically and statistically” justified, a process that can be resource intensive.20 Adaptive trials require the analysis of interim results with which to make decisions. Certain innovative products or therapeutic areas that cannot offer interim results would be unable to utilize adaptive methodology. Another limitation to the adaptive trial design is the difficulty in creating a balance between the needs of patients and the need to generate strong evidence of efficacy for a new therapy. Oncology trials present a real world instance where researchers would encounter this challenge. A patient-centered approach to trial design would support allowing cross-over to the experimental treatment if it shows a superior progression-free survival. This attenuates, however, the chances of showing superiority in overall survival, which is often required for regulatory approval and adoption by payers. The results from all three trial designs must be interpreted carefully as the conclusions drawn from these studies could be very different from those made had the trial been conducted using traditional methodology.8,20
Uptake of Patient-Centeredness in Trial Design
Applying these trial designs to study treatment options among individuals with rare conditions, such as amyotrophic lateral sclerosis (ALS) or Huntington's disease may serve as the first step to widespread implementation of patient-centered trials. Trials for rare conditions inherently face small sample sizes and are continuously looking for ways to improve the ability to detect treatment differences, such as expanding a trial to several different countries.xv Bayesian and adaptive trials offer alternatives for circumstances when researchers are faced with this scenario.xvi,xvii,xviii The additional benefit offered by Bayesian and adaptive approaches for participants in rare condition trials is that patients will not remain in a trial for an extended period of time without good reason. If an effect is found, all individuals with the condition could potentially benefit sooner than under a traditional trial. In the event a treatment is determined to offer no benefit, participants can be either allocated into an arm with more potential or, if the entire trial has been ended early, funneled into another study where their participation can help address a question where uncertainty is still present.
Conclusion
The way in which a clinical trial is designed, in theory, provides an opportunity to empower participants in the research process. Deciding which approaches truly achieve the objective of patient-centered research, however, requires further research to determine the impact on participation, incorporation of trial results into patient-centered decision making, and ultimately health outcomes. Until trials routinely use more patient-centered methodology, it is uncertain if the conceptual advantages described in this article will translate into actual gains for patient-centered health care. Making trials more patient-centered requires more than merely designing and implementing more pragmatic, Bayesian and adaptive trials. To maximize the likelihood that a trial is patient centered, trial designs should involve informed participants and patient advocates in the study design. This approach could be supplemented by an online system that lets participants know about the progress of the trial. In addition, participants should be informed of interim findings and provided an understandable summary of the trial findings.
Challenges associated with the adoption of alternative trial designs exist in respects to implementation and balancing patient-centeredness with the need for high-quality evidence. Unless we overcome these obstacles and transform the way in which clinical trials are conducted, we will be unable to accomplish the patient-centered portion of Healthcare Reform. Adopting more patient-centered approaches, such as using pragmatic, Bayesian, and adaptive designs, is only one piece of the puzzle; continuous participant engagement and feedback, and addressing the information needs of diverse populations are other mechanisms necessary to improve trial recruitment and retention.
Acknowledgments
Financial Support
NIH/NHLBI - [1RC4HL106363-01] “Do Bayesian Adaptive Trials Offer Advantages for CER?”
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- i.A New Definition of Patient Engagement: What is Engagement and Why is it Important? [Internet] Washington DC: Center for Advancing Health; 2010. [cited 2012 Oct 14]. Available from: http://www.cfah.org/pdfs/CFAH_Engagement_Behavior_Framework_current.pdf. [Accessed Month day, year]. [Google Scholar]
- ii.Mullins CD, Abdulhalim AM, Lavallee DC. Continuous patient engagement in comparative effectiveness research. JAMA. 2012;307:1587–1588. doi: 10.1001/jama.2012.442. [DOI] [PubMed] [Google Scholar]
- iii.Verheggen FW, Nieman FH, Reerink E, Kok GJ. Patient satisfaction with clinical trial participation. Int J Qual Health Care. 1998;10:319–330. doi: 10.1093/intqhc/10.4.319. [DOI] [PubMed] [Google Scholar]
- iv.Sood A, Prasad K, Chhatwani L, et al. Patients' attitudes and preferences about participation and recruitment strategies in clinical trials. Mayo Clin Proc. 2009;84:243–247. doi: 10.4065/84.3.243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- v.Gul RB, Ali PA. Clinical trials: the challenge of recruitment and retention of participants. J Clin Nurs. 2010;19:227–233. doi: 10.1111/j.1365-2702.2009.03041.x. [DOI] [PubMed] [Google Scholar]
- vi.Patient-Centered Outcome Research Institute (US) Patient-Centered Outcomes Research [Internet] Washington (DC): [cited 2012 Oct 04]. Available from: http://www.pcori.org/what-we-do/pcor/. [Accessed Month day, year]. [Google Scholar]
- vii.Davis K, Schoenbaum SC, Audet AM. A 2020 vision of patient-centered primary care. J Gen Intern Med. 2005;20:953–957. doi: 10.1111/j.1525-1497.2005.0178.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- viii.Roland M, Torgerson DJ. Understanding controlled trials: What are pragmatic trials? BMJ. 1998;316:285. doi: 10.1136/bmj.316.7127.285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- ix.Nakamura C, Bromberg M, Bhargava S, et al. Mining online social network data for biomedical research: a comparison of clinicians' and patients' perceptions about amyotrophic lateral sclerosis treatments. J Med Internet Res. 2012;14:e90. doi: 10.2196/jmir.2127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- x.Berry DA. Bayesian clinical trials. Nat Rev Drug Discov. 2006;5:27–36. doi: 10.1038/nrd1927. [DOI] [PubMed] [Google Scholar]
- xi.Jones D. Adaptive trials receive boost. Nat Rev Drug Discov. 2010;9:345–348. doi: 10.1038/nrd3174. [DOI] [PubMed] [Google Scholar]
- xii.Dragalin V. Adaptive Designs: Terminology and Classification. [cited 2012 Oct 4];Drug Inf J [Internet] 2006 40:425–435. Available from: http://www.diahome.org/Tools/Content.aspx?type=eopdf&file=%2fproductfiles%2f8357%2fdiaj_14478%2Epdf. [Accessed Month day, year]. [Google Scholar]
- xiii.Collins F. From the NIH Director: The Importance of Clinical Trials. NIH MedlinePlus. 2011;6:2–3. [Google Scholar]
- xiv.U. S. Food and Drug Administration, Center for Devices and Radiological Health. Guidance for the use of Bayesian statistics in medical device clinical trials - guidance for industry and FDA staff [Internet] [Cited 2013 Nov 07]; Available from: http://www.fda.gov/downloads/MedicalDevices/DeviceRegulationandGuidance/GuidanceDocuments/ucm071121.pdf. [Accessed Month day, year].
- xv.Marina N, Bielack S, Whelan J, et al. International collaboration is feasible in trials for rare conditions: the EURAMOS experience. Cancer Treat Res. 2009;152:339–353. doi: 10.1007/978-1-4419-0284-9_18. [DOI] [PubMed] [Google Scholar]
- xvi.Kesselheim AS, Gagne JJ. Strategies for Post-market Surveillance of Drugs for Rare Diseases. Clinical Pharmacology & Therapeutics. Accepted article preview online 05 November 2013; Has this been published yet?. [Google Scholar]
- xvii.Gupta S, Faughnan ME, Tomlinson GA, Bayoumi AM. A framework for applying unfamiliar trial designs in studies of rare diseases. J Clin Epidemiology. 2011;64:1085–1094. doi: 10.1016/j.jclinepi.2010.12.019. [DOI] [PubMed] [Google Scholar]
- xviii.Chow SC, Chang M. Adaptive design methods in clinical trials - a review. Orphanet J Rare Dis. 2008;3:11. doi: 10.1186/1750-1172-3-11. Available from: http://www.ojrd.com/content/3/1/11. [Accessed Month day, year]. [DOI] [PMC free article] [PubMed] [Google Scholar]