Abstract
Background
Chronic prostatitis/chronic pelvic pain syndrome (CP/CPPS) afflicts 2–10% of adult men. Available therapies offer little or no proven benefit. Because acupuncture represents an attractive “natural” therapy, we compared the efficacy of acupuncture to sham acupuncture for CP/CPPS
Methods
Participants met US National Institutes of Health (NIH) consensus criteria for CP/CPPS, aged ≥ 20 years old, with total score ≥ 15 on the NIH-Chronic Prostatitis Symptom Index (NIH-CPSI) and symptoms for at least 3 of the preceding 6 months were randomized 1:1 to acupuncture or sham acupuncture. Treatment consisted of twice weekly 30-minute sessions for 10 weeks (20 sessions total), without needle stimulation, herbs or adjuvants. The primary response criterion was a six-point decrease from baseline to week 10 in NIH-CPSI total score (range 0–43).
Results
Thirty-two (73%) of 44 participants responded in the acupuncture group compared to 21 (47%) of 45 sham group participants (relative risk [RR] 1.81, 95% confidence interval [CI], 1.3–3.1, p=0.02,). Long-term responses 24 weeks after completing therapy without additional treatment occurred in 14 (32%) of 44 acupuncture group participants and in 6 (13%) of 45 sham group participants (RR 2.39, 95% CI, 1.0–5.6, p=0.04).
Conclusion
After 10 weeks of treatment, acupuncture proved almost twice as likely as sham to improve CP/CPPS symptoms. Participants receiving acupuncture were 2.4 fold more likely to experience long-term benefit than participants receiving sham acupuncture.
Keywords: acupuncture, sham acupuncture, chronic prostatitis, chronic pelvic pain, traditional Chinese medicine
Chronic prostatitis/chronic pelvic pain syndrome (CP/CPPS) represents the most common prostatitis syndrome, with a 2–10% prevalence among adult men worldwide, and an 8.7% prevalence in Northern Malaysia 1. Characteristic pelvic pains, often with urinary symptoms, cause considerable morbidity. There is no consensus on the etiology and no treatment has proven effective in high-quality trials 2. Previously, we showed that our population had similar demographic and clinical characteristics to the NIH cohort 3.
Acupuncture is popular for conditions not managed effectively by orthodox approaches. Data suggest that acupuncture provides benefit for chronic pain, including uncontrolled series suggesting efficacy for CP/CPPS 4. We report the first randomized, blinded comparison of acupuncture with sham acupuncture for CP/CPPS.
Materials and Methods
Availability of traditional Chinese practitioners and Western consultants in the same facility provided an opportunity to conduct a randomized clinical trial.
Participants met NIH CP/CPPS consensus criteria 5. Requirements included: age ≥20 years, NIH-CPSI total score ≥15 (scale 0-to-43) on both baseline visits, and symptoms for ≥3 within the preceding 6 months. Each participant had a medical history, physical examination, cultures, uroflowmetry and residual urine determination. Exclusion criteria included: bacterial prostatitis, urinary tract infection within 1 year, any traditional or alternative medical therapy within 6 weeks, or any consensus CP/CPPS exclusion criterion. The University of Science Malaysia-Penang Hospital Committee and University of Washington Institutional Review Board approved the protocol.
Design
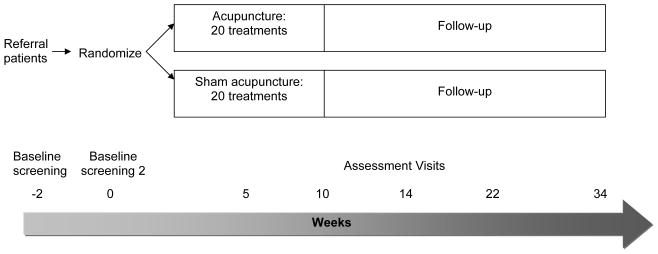
Following written informed consent, participants were assigned 1:1 to acupuncture or sham acupuncture following a computer-generated random, variable block design with biweekly treatment for 20 total sessions (Figure 1). A nurse observed each session to assure that interaction between participants and acupuncturists was limited to needle placement and withdrawal. Symptoms were assessed at baseline, weeks 5, 10, 14, 22 and 34.
Figure 1. Flow Diagram for Comparison of Acupuncture with Sham Acupuncture Treatment for Chronic Prostatitis/Chronic Pelvic Pain Syndrome.
*
Participants were randomly assigned 1:1 to either acupuncture or sham acupuncture using a computer-generated random number table (QuickCalcs, Graphpad Software). Participants received acupuncture or sham acupuncture for 20 total sessions over 10 weeks, with follow-up assessments at weeks 5, 10, 14, 22 and 34. Each participant had a minimum of 27 physician visits, including two baseline screening visits (2 weeks apart), 20 visits for treatment with acupuncture or sham acupuncture and a post-therapy visit, 4, 12 and 24 weeks after completing the treatment protocol.
Interventions
Lam Wah Ee Hospital acupuncturists (each with ≥2,800 training hours in China), faculty from Xiamen and Fujian Universities (China), and Western-trained physicians fluent in Chinese reviewed the Chinese and Western literature to develop a protocol with a minimal number of acupoints.
Acupuncture
Four acupoints were prepared with 70% alcohol pads then sterile, disposable stainless steel needles (Suzhou HuanQiu Acupuncture Medical Supplies, Suzhou, China) were placed perpendicularly (Table 1). Treatments lasted 30 minutes with participants supine.
Table 1.
Comparison of Acupuncture with Sham Acupuncture Treatment for Chronic Prostatitis/Chronic Pelvic Pain Syndrome
| Treatment | Acupuncture | Sham Acupuncture |
|---|---|---|
| Points used | 4 | 4 |
| No of needles used | 6 | 6 |
| No of sessions | 2 weekly sessions for 10 weeks | 2 weekly sessions for 10 weeks |
| Duration | 30 minutes | 30 minutes |
| Needle Stimulation | None | None |
| Needle diameter | 0.3mm | 0.3mm |
| Needle length | 40mm – 60mm depending on location of acupuncture point | 25mm for all points |
| Location of points | CV1-GuanYuan | Needling performed 15mm to the left of actual acupuncture points |
| CV4-Huiyin | ||
| SP6-Sanyinjiao | CV1, CV4, SP6 or SP9 | |
| SP9-Yinlingquan | ||
| Depth of needling | CV4–60mm | 15mm or less for all points |
| CV1–50mm | ||
| SP6 & SP9-40mm |
Acupuncture and sham acupuncture were similar in all variables except for the location and depth of needling.
Sham acupuncture included the same number, duration and frequency of sessions as the acupuncture group at non-acupoints (superficial and 15mm to the left of each corresponding acupoint).
Outcomes
Primary endpoint was a six-point NIH-CPSI total score from baseline to week 10, based on a consensus of expert opinion and data from a multi-center trial 5.
Secondary outcomes included: complete resolution, NIH-CPSI total score at weeks 5, 14, 22 and 34, NIH-CPSI subscales, Global Response Assessment, Brief Pain Inventory (Short Form), International Prostate Symptom Score, and International Index of Erectile Function. Combined, the primary and secondary endpoints addressed all recommended outcome domains for chronic pain trials 6.
To test blinding, participants were asked, “Which therapy do you think you received?” after 10 and 20 treatments. Long-term responders were defined as responders at week 10 who met the primary criterion at week 34 without additional therapy.
Analyses
Setting significance at 0.05 with 80% power, 86 participants were required, assuming response in 75% of acupuncture and 35% of sham participants with 20% dropouts. We used intention-to-treat-analysis, replacing missing data by the last-observation-carried-forward. Two-way repeated measures analysis of variance (ANOVA) compared NIH-CPSI total scores (Prism software 4.0b, GraphPad Software, San Diego, CA).
Results
Participants
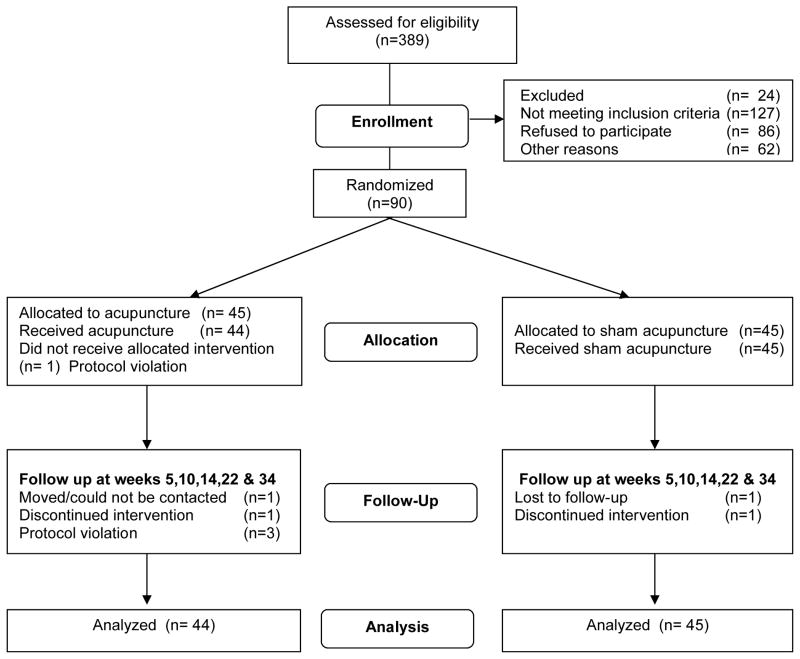
Between February 1, 2004 and July 30, 2005, 343 patients were screened to enroll 90 participants (Figure 2). Treatment groups were similar at baseline (Table 2).
Figure 2. Double-blind, Randomized Clinical Trial Comparing Acupuncture with Sham Acupuncture Therapy for Chronic Prostatitis/Chronic Pelvic Pain Syndrome.
CONSORT diagram. Participants with chronic prostatitis/chronic pelvic pain syndrome were randomized to receive either acupuncture (n = 44) or sham acupuncture (n = 45) therapy. Of the 89 participants, 82 (92.1%) completed all 20 treatment sessions over 10-weeks, 79 (88.8%) completed the 14-week follow-up, 63 (70.8%) the 22-week follow-up and 59 (66.3%) completed the 34-week follow-up.
Table 2.
Baseline Demographic and Clinical Characteristics of 89 Participants with Chronic Prostatitis/Chronic Pelvic Pain Syndrome
| Characteristic1 | Acupuncture (N = 44) | Sham Acupuncture (N = 45) | p-value* |
|---|---|---|---|
| Age, mean years (± 1 standard deviation, SD)† | 40.9 (11.0) | 42.8 (9.4) | 0.06 |
| Duration of symptoms, mean months (SD)† | 22.4 (28.4) | 27.5 (26.9) | 0.80 |
| Living status, N (%)† | |||
| Alone | 14 (31.8) | 7 (15.6) | 0.08 |
| Partnered | 30 (68.2) | 38 (84.4) | |
| Employment status, N (%)† | |||
| Employed | 41 (93.2) | 38 (84.4) | 0.35 |
| Unemployed | 0 (0) | 1 (2.2) | |
| Retired | 3 (6.8) | 6 (13.3) | |
| Treatment history, N (%)† | |||
| 0 treatment | 12 (27.3) | 9 (20.0) | 0.42 |
| 1 or more treatment | 32 (72.7) | 36 (80.0) | |
| Pelvic pain location/type, N (%)§ | |||
| Area between rectum + testicle | 20 (45.5) | 18 (40.0) | 0.10 |
| Testicles | 8 (18.2) | 11 (24.4) | 0.47 |
| Tip of penis, not related to urination | 24 (54.5) | 21 (46.7) | 0.46 |
| Below the waist in the pubic or bladder area | 33 (75.0) | 30 (66.7) | 0.39 |
| Pain or burning during urination | 25 (56.8) | 24 (53.3) | 0.74 |
| Pain or discomfort during/after sexual climax | 16 (36.4) | 15 (33.3) | 0.76 |
| Other significant medical conditions, No. (%)† | |||
| None | 12 (27.3) | 9 (20.0) | 0.46 |
| 1 or more | 32 (72.7) | 36 (80.0) | |
| National Institutes of Health-Chronic Prostatitis Symptom Index2, mean (SD) | |||
| Total score (range 0–43, ≥15 to enter study) | 24.8 (6.2) | 25.2 (5.8) | 0.73 |
| Pain subscale (range 0–21) | 11.4 (3.4) | 11.5 (2.9) | 0.85 |
| Urinary subscale (range 0–10) | 4.1 (3.7) | 4.3 (3.7) | 0.78 |
| Quality of life subscale (range 0–12) | 9.3 (1.6) | 9.4 (1.8) | 0.77 |
| International Prostate Symptom Score3, mean (SD) | |||
| Total (range 0–35) | 8.2 (6.0) | 9.3 (7.8) | 0.82 |
| Quality of life subscale (range 0–6) | 3.4 (1.9) | 3.7 (2.0) | 0.53 |
| Brief Pain Inventory (short form)4, mean (SD) | |||
| Pain intensity (range 0–10) | 3.6 (1.9) | 3.6 (1.5) | 0.88 |
| Pain disability (range 0–10) | 3.2 (1.8) | 3.0 (1.7) | 0.54 |
| International Index of Erectile Function5, mean (SD, range 0–25) | 17.6 (7.7) | 19.2 (6.9) | 0.30 |
All participants recruited were of Asian race/ethnicity.
A battery of survey instruments was used to assess all recommended domains for a chronic pain study19. The National Institutes of Health-Chronic Prostatitis Symptom Index was used to assess symptoms associated with chronic prostatitis. Participants were required to have a total score >15 at each of the two baseline visits. The primary criterion for response was a six point drop in NIH-CPSI total score from baseline to the 10 week visit.
The International Prostate Symptom Score was used to assess the lower urinary tract symptoms.
Brief Pain Inventory-Short Form assessed the severity of pain as well as pain interference with activities of daily living.
The International Index of Erectile Function-5 is used to measure sexual function.
Participants may experience one or more of these symptoms
P-values based on two sample t-tests.
Chi-square tests were used
Primary outcome
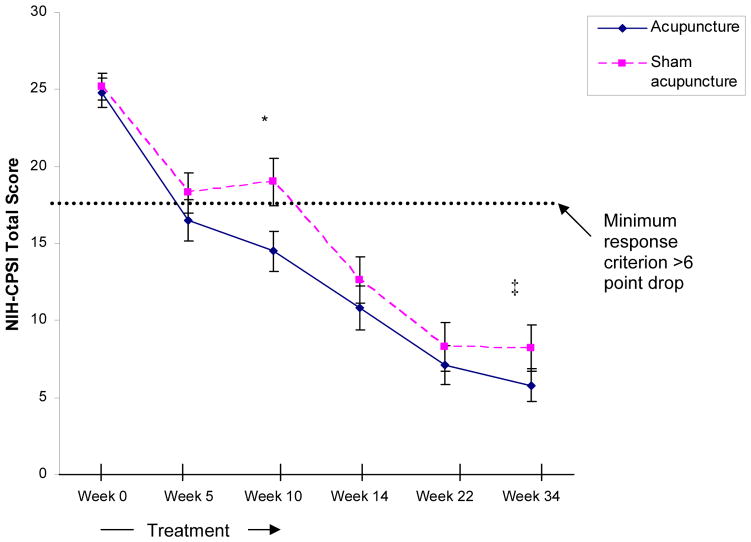
Of 44 acupuncture participants, 32 (72.7%) responded compared to 21 (46.7%) of 45 sham participants (relative risk [RR] 1.81, 95% confidence interval [CI], 1.3–3.1, Fisher’s exact test p=0.02, Figure 3). After 10 weeks, the acupuncture group improved 4.5 points more on average than the sham group (Figure 3, Mann-Whitney p=0.03). The median decrease in NIH-CPSI total score was 15.0 (range 0–33, 95% CI, 13.1–17.0) among the 32 acupuncture responders compared to 10.0 (range 0–32, 95% CI, 12.1–18.0) among the 21 sham responders (not significant). No demographic or clinical characteristic was associated with response.
Figure 3. Mean NIH-CPSI Total Score comparing Acupuncture with Sham Acupuncture in 89 Men with Chronic Prostatitis/Chronic Pelvic Pain Syndrome.
Mean NIH-CPSI total scores of 89 chronic prostatitis/chronic pelvic pain patients treated with 20 sessions of either acupuncture (n = 44) or sham acupuncture (n = 45) therapy over 10-weeks. Error bars represent the standard error of mean. To enter into the study, each participant had a minimum NIH-CPSI total score of at least 15 (range 0-to-43) on both baseline visits (indicated as the average in the baseline value). The primary criterion for response was at least a 6 point decrease from baseline to week 10 (end of therapy).
There was no significant difference between the NIH-CPSI total scores in the acupuncture and sham acupuncture groups at baseline, week 5 (early during therapy) or weeks 14, 22 and 34 (post-therapy) evaluations.
*Of 44 participants in the acupuncture group, 32 (72.7%) met the primary response criterion (at least a 6 point decrease in NIH-CPSI total score from baseline to week 10), compared to 21 (46.7%) of 45 participants in the sham acupuncture group (Fisher’s exact test p=0.02).
‡At week 34, 14 (31.8%) of 44 acupuncture group participants had long-term responses (with no additional treatment) compared to 6 (13.3%) of 45 sham acupuncture group participants (R.R. 2.39, CI 1.0–5.6, Fisher’s Exact test p=0.04).
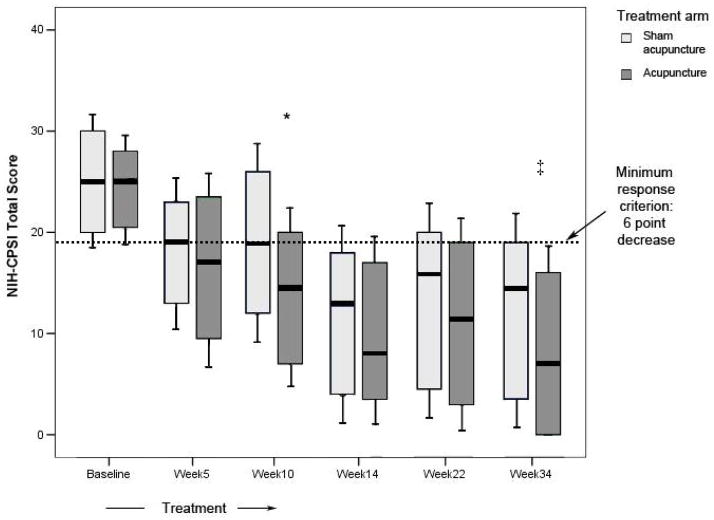
Figure 3. Box-Whiskers Plot Comparing Acupuncture with Sham Acupuncture in 89 Men with Chronic Prostatitis/Chronic Pelvic Pain Syndrome.
Box-and whiskers plot comparing NIH-CPSI total scores of 89 chronic prostatitis/chronic pelvic pain patients treated with 20 sessions of either acupuncture (n = 44) or sham acupuncture (n = 45) therapy over 10-weeks. Within each box, the bold line represents the median, upper and lower bounds of the box represent the 25th and 75th percentiles, respectively. Error bars represent the standard deviation. To enter into the study, each participant had a minimum NIH-CPSI total score of at least 15 (range 0-to-43) on both baseline visits (indicated as the average in the baseline value). The primary criterion for response was at least a 6 point decrease from baseline to week 10 (end of therapy).
*Of 44 participants in the acupuncture group, 32 (72.7%) met the primary response criterion (at least a 6 point decrease in NIH-CPSI total score from baseline to week 10), compared to 21 (46.7%) of 45 participants in the sham acupuncture group (Fisher’s exact test p=0.02).
There was no significant difference between the NIH-CPSI total scores in the acupuncture and sham acupuncture groups at baseline, week 5 (early during therapy) or weeks 14, 22 and 34 (post-therapy) evaluations.
‡At week 34, 14 (31.8%) of 44 acupuncture group participants had long-term responses (with no additional treatment) compared to 6 (13.3%) of 45 sham acupuncture group participants (R.R. 2.39, CI 1.0–5.6, Fisher’s Exact test p=0.04).
Secondary outcomes
After 10 weeks, 18 (40.9%) of 44 acupuncture participants experienced complete resolution compared to 10 (22.2%) of 45 sham participants (RR 1.51, 95% CI, 1.0–2.3, p=0.07). Both groups had NIH CPSI total scores decrease from baseline (ANOA p<0.001, Figure 3). Twenty-nine (65.9%) acupuncture participants and 18 (40.0%) sham participants reported ≥50% improvement in Global Response Assessment scores (Fisher’s exact test p=0.02), including 11 (25.0%) acupuncture and 6 (13.3%) sham group participants reporting ≥75% improvement (Fisher’s exact test p=0.19, Table 3).
Table 3.
Outcomes after 10 weeks of Acupuncture or Sham Acupuncture Therapy for 89 Men with Chronic Prostatitis/Chronic Pelvic Pain Syndrome
| Outcome | Acupuncture (n=44) | Sham Acupuncture (n=45) | p-value* |
|---|---|---|---|
| National Institutes of Health-Chronic Prostatitis Symptom Index, median (standard deviation, SD) | |||
| Total score (range 0–43, primary response criterion = 6 points decrease) | 14.5 (8.7) | 19.0 (10.3) | 0.03 |
| Pain subscale (range 0–21) | 7.0 (4.5) | 8.0 (4.8) | 0.12 |
| Urinary subscale (range 0–10) | 0 (2.9) | 2.0 (3.2) | 0.04 |
| Quality of life subscale (range 0–12) | 3.5 (5.5) | 8.0 (3.8) | 0.02 |
| International Prostate Symptom Score, median (SD) | |||
| Total (range 0–35) | 3.5 (5.5) | 6.0 (6.4) | 0.13 |
| Quality of life subscale (range 0–6) | 2.0 (2.0) | 3.0 (2.0) | 0.23 |
| Brief Pain Inventory (short form), median (SD) | |||
| Pain intensity (range 0–10) | 1.9 (2.0) | 2.3 (1.7) | 0.07 |
| Pain disability (range 0–10) | 0.9 (1.7) | 1.7 (1.5) | 0.31 |
| International Index of Erectile Function, median (SD, range 0–25) | 22.5 (7.5) | 23.0 (6.7) | 0.63 |
| Global response assessment†, N (%) | |||
| ≥50% improvement | 29 (65.9) | 18 (40.0) | 0.02 |
| ≥75% improvement | 11 (25.0) | 6 (13.3) | 0.19 |
Both groups of patients received 10 weeks of acupuncture or sham acupuncture therapy (20 total sessions).
P value based on Mann-Whitney U test.
P-value based on Fisher Exact test
Adverse events occurred in 13 participants, 8 (18.1%) in the acupuncture group (6 hematomas and 2 with pain at needling sites) and 5 (11.1%) in the sham group (1 hematoma, 3 with pain at needling sites, and 1 with acute urinary retention, Fisher’s exact test, p=0.38). All adverse events resolved quickly.
Credibility
At week 5, 33 (75%) of 44 acupuncture and 36 (80%) of 45 sham participants thought they were receiving acupuncture (Fisher’s Exact test p=0.62). At week 10, 42 (95%) acupuncture and 37 (82%) sham participants thought they were receiving acupuncture (Fisher’s Exact test p=0.20).
Long-term responses
At week 14, all 18 initial acupuncture responders continued to respond compared to 7 of 10 initial sham acupuncture responders (Fisher’s exact test p=0.037). At weeks 22 and 34, 14 (78%) of 18 initial acupuncture responders continued to respond compared to 6 (60%) of 10 initial sham responders (Fisher’s exact test p=0.40). Thus, 14 (32%) of 44 acupuncture participants had long-term responses compared to 6 (13%) of 45 sham acupuncture participants (R.R. 2.39, 95% CI, 1.0–5.6, p=0.04).
Discussion
Acupuncture proved almost twice as effective as sham acupuncture for CP/CPPS. After 10 weeks, 32 (73%) acupuncture participants responded compared to 21 (48%) sham acupuncture participants (p=0.02). Overall, 18 acupuncture participants experienced complete resolution after 10 weeks, compared to 10 sham participants (p=0.07). Although 32% of acupuncture participants had long-term responses 20 weeks after completing therapy, this was 2.4 times better than the 13% response rate among sham-acupuncture participants (p = 0.04). Mild adverse events occurred in 18% of acupuncture and 11% of sham participants. Thus, acupuncture represents safe and effective therapy for CP/CPPS.
Acupuncture fits with the theory that neurobehavioral factors are important in CP/CPPS. In uncontrolled series, behavioral and physical therapies improved CP/CPPS 7. In traditional Chinese medicine, CP/CPPS reflects “deficient qi” (“energy of life”). We selected three acupoints deemed highly effective to restore qi (CV-1, CV-4, and SP-6) and another acupoint (SP-9) considered effective for voiding dysfunction.
This trial follows controlled acupuncture trial recommendations 8. However, traditional practitioners modify therapy based on individual responses, add acupoints, manipulate needles and add adjuvants, especially herbs. Practitioners confirm therapeutic effects by “de-qi” (“arrival of energy”), indicated by tingling, numbness, etc. with each needle placement. Our results might prove less optimal than traditional practitioners’ results.
We selected sham acupuncture rather than a placebo therapy to assure blinding. We did not manipulate or stimulate needles because this is difficult to standardize. “De-qi’ was not achieved deliberately to assure blinding. Complimentary therapies were not used. We minimized interactions between practitioners and participants. Sham points were 15 mm away from the acupuncture points. These measures assured credibility, since three-quarters of the sham group thought they had received acupuncture.
The sham group had a 48% response rate, with 22% experiencing complete resolution. In acupuncture theory, sham points may prove beneficial, although not as beneficial as acupoints. Each participant had 27 scheduled physician visits plus 5 phone calls. Each visit lasted ≥45 minutes, including 30 minutes needle retention. The high response rate to sham acupuncture might reflect this intense attention. These observations might also reflect the natural history of CP/CPPS. Drug studies for CP/CPPS report substantial placebo response rates 5,9.
More than one-third of eligible patients enrolled, including one-quarter who had no previous medical therapy (Figure 2). Thus, our population may mirror patients in primary care or general urology practices, in contrast to the heavily-pretreated referral patients in previous trials 5.
This study had several strengths. We offered Western and Eastern medicine in the same facility. Evaluation, entry and exclusion criteria adhered to consensus recommendations 5,10. We employed standard outcomes validated in our population 11. Interventions were developed following literature review and expert consultation, then administered by optimally trained practitioners. We had an adequate sample size and excellent follow-up.
This study had important limitations. Personal attention likely increased response rates to both treatments. The high-intensity protocol limited enrollment. Outcomes may differ in other populations. Controls did not include a waiting list group. Sample size limited power for subgroup analyses. The protocol might be deemed inadequate by some acupuncturists.
In summary, acupuncture proved almost twice as effective as sham acupuncture for treating CP/CPPS; 73% of acupuncture participants and 47% of sham participants met the primary response criterion. Although the long-term response rate was 2.4-fold higher for acupuncture than for sham acupuncture, most participants did not experience complete resolution. These results are more encouraging than other interventions evaluated in randomized, controlled, clinical trials. Studies are indicated to determine whether longer treatment courses, different techniques or combination of acupuncture with other therapies can improve outcomes for CP/CPPS patients.
Acknowledgments
Funding source: NIH, Bethesda, Maryland, grants DK065266 and DK38955,
Footnotes
Registration: www.clinicaltrails.gov, identifier NCT00260637.
Role of sponsor. The sponsor had no role in study design, data collection, analysis or interpretation.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Krieger JN, Riley DE, Cheah PY, Liong ML, Yuen KH. Epidemiology of prostatitis: new evidence for a world-wide problem. World J Urol. 2003;21(2):70–4. doi: 10.1007/s00345-003-0329-0. [DOI] [PubMed] [Google Scholar]
- 2.McNaughton C, Mac Donald R, Wilt T. Interventions for chronic abacterial prostatitis. Cochrane Database Syst Rev. 2001;(1):CD002080. doi: 10.1002/14651858.CD002080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lee SW, Cheah PY, Liong ML, Yuen KH, Schaeffer AJ, Propert K, et al. Demographic and clinical characteristics of chronic prostatitis: prospective comparison of the University of Sciences Malaysia Cohort with the United States National Institutes of Health Cohort. J Urol. 2007;177(1):153–7. doi: 10.1016/j.juro.2006.08.098. discussion 158. [DOI] [PubMed] [Google Scholar]
- 4.Chen R, Nickel JC. Acupuncture ameliorates symptoms in men with chronic prostatitis/chronic pelvic pain syndrome. Urology. 2003;61(6):1156–9. doi: 10.1016/s0090-4295(03)00141-9. discussion 1159. [DOI] [PubMed] [Google Scholar]
- 5.Alexander RB, Propert KJ, Schaeffer AJ, Landis JR, Nickel JC, O’Leary MP, et al. Ciprofloxacin or tamsulosin in men with chronic prostatitis/chronic pelvic pain syndrome: a randomized, double-blind trial. Ann Intern Med. 2004;141(8):581–9. doi: 10.7326/0003-4819-141-8-200410190-00005. [DOI] [PubMed] [Google Scholar]
- 6.Turk DC, Dworkin RH, Allen RR, Bellarmy N, Brandenburg N, Carr DB, et al. Core outcome domains for chronic pain clinical trials: IMMPACT recommendations. Pain. 2003;106:337–345. doi: 10.1016/j.pain.2003.08.001. [DOI] [PubMed] [Google Scholar]
- 7.Anderson RU, Wise D, Sawyer T, Chan C. Integration of myofascial trigger point release and paradoxical relaxation training treatment of chronic pelvic pain in men. J Urol. 2005;174(1):155–60. doi: 10.1097/01.ju.0000161609.31185.d5. [DOI] [PubMed] [Google Scholar]
- 8.MacPherson H, White A, Cummings M, Jobst K, Rose K, Niemtzow R, et al. Standards for reporting interventions in controlled trials of acupuncture: the STRICTA recommendations. Acup Med. 2002;20(1):22–25. doi: 10.1136/aim.20.1.22. [DOI] [PubMed] [Google Scholar]
- 9.Cheah PY, Liong ML, Yuen KH, Teh CL, Khor T, Yang JR, et al. Terazosin therapy for chronic prostatitis/chronic pelvic pain syndrome: a randomized, placebo controlled trial. J Urol. 2003;169(2):592–6. doi: 10.1097/01.ju.0000042927.45683.6c. [DOI] [PubMed] [Google Scholar]
- 10.Krieger JN, Nyberg L, Nickel JC. Consensus definition and classification of prostatitis. JAMA. 1999;282:236–237. doi: 10.1001/jama.282.3.236. [DOI] [PubMed] [Google Scholar]
- 11.Cheah PY, Liong ML, Yuen KH, Lee S, Yang JR, Teh CL, et al. Reliability and Validity of the National Institutes of Health - Chronic Prostatitis Symptom Index in a Malaysian Population. World J Urol. 2006;24(1):79–87. doi: 10.1007/s00345-005-0037-z. [DOI] [PubMed] [Google Scholar]