Abstract
This self-report and observational study explores the relationship between perceptions of different kinds of teasing experiences and psychosocial functioning in an overweight treatment-seeking adolescent population. Participants were 96 adolescents enrolled in a residential weight-loss camp program. Prior to the start of treatment, participants’ weight status was measured by trained program staff, and participants’ perceptions of teasing experiences and psychosocial functioning were assessed through self-report questionnaires. Controlling for body mass index, more frequent and upsetting weight-related teasing experiences were associated with worse psychological functioning. Adolescents most distressed by weight-related teasing exhibited lower self-esteem and higher depressive symptoms regardless of reported frequency of weight-related teasing. Competence-related teasing was also associated with more worries about weight, greater depressive symptoms, and more negative anti-fat attitudes. Weight-related teasing, but not competence-related teasing, was associated with lower levels of program and social involvement for heavier adolescents.
Keywords: overweight, peers, teasing, self-esteem
Introduction
The prevalence of overweight and at-risk-for-overweight among children and adolescents has increased dramatically in recent years (Eaton et al., 2006; Hedley et al., 2004; Heinberg, Thompson, & Mateson, 2001), making it the most common health problem facing United States’ youth (Strauss & Pollack, 2001). In addition to experiencing physical problems associated with excess weight, overweight youth are often the victims of bias and stereotyping, particularly by peers (Kraig & Keel, 2001; Latner & Stunkard, 2003; Neumark-Sztainer et al., 2002). Overweight adolescents may be par-ticularly susceptible to weight-related teasing (WRT). Marked physical changes during adolescence make appearance a prominent focus of peer interactions (Janssen, Craig, Boyce, & Pickett, 2004) at the same time that social relationships increase in importance (Puhl & Latner, 2007). The combination of these two normative developmental changes serves to make adolescents especially vulnerable to the negative consequences of peer stigmatization.
Weight and Teasing
Greatly contributing to the challenges overweight youth face is society’s increasing intolerance of obesity. Perceptions of overweight figures as ‘unacceptable’ remain relatively constant across ages, with adults becoming only slightly more tolerant than children (Rand & Wright, 2000). In Richardson’s (1970, 1971) studies of developmental trends in rankings of preference, obese children were less liked than a wheelchair-bound or facially disfigured child. A 2003 replication of this study found that stigmatization of overweight by children has increased and obese youth remain the least preferred in a group of handicapped children (Latner & Stunkard, 2003). Moreover, while acceptance of functional impairments increased with rater age, acceptance of obesity decreased (Sigelman, Miller, & Whitworth, 1986). Not surprisingly, overweight teens are more socially isolated and receive significantly fewer friendship nominations from peers than normal-weight teens (Strauss & Pollack, 2003).
Overweight adolescents are also more frequently the victims of negative social interactions (Baum & Forehand, 1984), including both relational and overt aggression (Janssen et al., 2004; Lagerspetz, Bjorkqvist, Berts, & King, 1982). Although all forms of peer victimization are problematic, teasing is often considered the most harmful because of the lasting psychological injury from repeated experiences (Keltner, Capps, Kring, Young, & Heerey, 2001). Teasing content is often directed at physical appearance because of its salience (Mooney, Creeser, & Blatchford, 1991), and WRT is a common occurrence for overweight youth (Eisenberg, Neumark-Sztainer, & Story, 2003; Hayden-Wade et al., 2005). Although some work has demonstrated that overweight girls report more weight-based victimization, and are more bothered by teasing than are overweight boys (Eisenberg et al., 2003; Neumark-Sztainer et al., 2002), other work has found no gender differences (Kraig & Keel, 2001).
The prevalence of weight-based teasing is disturbing given its strong connection to various negative psychosocial factors, including body image dissatisfaction, eating disturbance, and depression (Eisenberg et al., 2003; Fabian & Thompson, 1989; Thompson, Cattarin, Fowler, & Fisher, 1995). Teasing history mediates the impact overweight status has on body image (Lunner et al., 2000; Thompson et al., 1995). WRT has also been linked with social maladjustment and low appearance self-esteem (Young-Hyman, Schlundt, Herman-Wenderoth, & Bozylinski, 2003), and teens who reported being teased about their weight also reported considering and attempting suicide more often than non-teased peers (Eisenberg et al., 2003). Moreover, the impact of teasing appears to last beyond the actual teasing incidents. Women who reported having had more prevalent and distressing appearance-related teasing experiences during their youth held more disturbed body images as adults (Cash, 1995).
Teasing and Internalized Attitudes
Overweight individuals of all ages also appear to internalize the negative stereotypes they receive via teasing and dislike other overweight individuals as much as non-overweight individuals do (Cramer & Steinwert, 1998; Crandall, 1994; Crandall & Biernat, 1990; Davison & Birch, 2004; Kraig & Keel, 2001; Puhl & Latner, 2007; Quinn & Crocker, 1999; Tiggemann & Rothblum, 1988). This is concerning because the negative effects of weight-related stigmatization may be particularly damaging for those who hold strong anti-fat beliefs (Friedman et al., 2005). Overweight adults who endorse stronger anti-fat beliefs report lower self-esteem than those who endorse weaker anti-fat beliefs (Crandall & Biernat, 1990). A recent study of obese, treatment-seeking adults also found that while frequency of stigmatizing experiences was not directly related to anti-fat beliefs, participants’ anti-fat beliefs were associated with psychological distress and moderated the relationship between stigmatization and body image (Friedman et al., 2005). Anti-fat attitudes might be especially problematic for overweight youth. If children internalize negative stereotypes of the overweight they receive via teasing experiences, they may incorporate this stigmatized identity—with all its negative associations—as a significant part of their own developing identity.
Teasing and Behavior
Ironically, differential socialization based on physical appearance may begin to lend a kernel of truth to the negative stereotypes of the overweight. Children who receive more favorable reactions from others may become more comfortable in social settings, have more positive social opportunities from which to learn, and may develop better social skills. This effect has been seen in overweight girls, as Allon (1976) found that girls’ perceptions of social isolation and strained relationships due to their weight influenced their daily interactions with normal-weight peers. Additionally, both behavioral observations and self-report surveys suggest that overweight children not only receive but also dispense more negative social interactions than normal-weight peers (Baum & Forehand, 1984; Janssen et al., 2004). Obese children tend to be rated as less socially competent, have more behavior problems, and exhibit more social isolation than clinic-referred normal-weight children (Banis et al., 1988). In one study, close to 50 percent of children seeking weight loss treatment had elevated scores on the social problems subscale of the child behavior checklist (Epstein, Myers, & Anderson, 1996).
Teasing experiences have also been linked to lower rates of physical activity, less social sports enjoyment and a preference for sedentary, isolative activities (Faith, Leone, Ayers, Heo, & Pietrobelli, 2002; Storch et al., 2007), which may ultimately lead to a vicious cycle of further weight gain, increased aversion to physical activity, and even further isolative inactivity (Hayden-Wade et al., 2005). Reduction in activity among overweight youth may reflect attempts to avoid further teasing (Sallis, Alcaraz, McKenzie, & Hovell, 1999). At a deeper level, this reduced activity may indicate that overweight youth have internalized negative stereotypes about the overweight and their ability to effectively control their weight. Indeed, in one study it was found that beliefs about one’s ability to engage in a healthy lifestyle were related to teens having healthier attitudes and lifestyle choices (Melnyk et al., 2006).
The purpose of the current study was to further investigate the relationships between peer teasing and psychosocial functioning, attitudes, and behavior. A treatment-seeking group of overweight adolescents was targeted for several reasons. Firstly, despite the fact that this unique population has insight into the experience of overweight in adolescence, it has been largely overlooked in favor of school-based samples. Although only a small percentage of overweight youth seek treatment, they are a group that is particularly affected by the negative consequences of overweight. Secondly, a large portion of the research linking stigmatization to negative outcomes has been with treatment-seeking adults (e.g., Friedman et al., 2005). In order to determine whether these findings hold true for youth as well, it would be important to begin with a similar group. Adolescents seeking weight loss in a camp setting would likely be most equivalent to residential treatment-seeking obese adults.
The current study supplements the research on the effects of teasing on overweight youth in several important ways. Firstly, we examine whether WRT and competency-related teasing (CRT) have similar effects on psychosocial functioning. Previous teasing research has focused on WRT and has not examined whether teasing that does not specifically target weight evidences similar outcomes. This important distinction between different types of teasing in relation to psychological well-being may have implications for how peer mistreatment is addressed when dealing with overweight youth. Based on the reviewed research, we hypothesize that while both types of teasing experiences will be frequent and upsetting for overweight youth, the effects of WRT on psychosocial functioning will be especially pronounced.
Secondly, the negative effects of teasing within this population may be due to both the frequency of teasing experiences and the distress adolescents feel about these experiences. The current study separates these two aspects to examine their unique effects. We anticipate that participants who are most distressed by teasing will show lower levels of psychosocial functioning regardless of the frequency of teasing, while adolescents least distressed by teasing will show a dose–response relationship (i.e., more teasing = worse functioning).
Finally, we investigate how weight-based stigmatization affects personal beliefs about overweight individuals in a treatment-seeking adolescent population. Given the relationships found between stigmatizing experiences, anti-fat attitudes, and body image in overweight treatment-seeking adults (Friedman et al., 2005), we anticipated that participants who report greater anti-fat attitudes will display more problematic psychosocial functioning. Additionally, we propose that the relationship between WRT and psychosocial functioning will be moderated by anti-fat attitudes. We also explore the relationship between teasing and social behavior.
Method
Participants
Participants were 96 adolescents (70 females, 26 males) who were part of a larger longitudinal project designed, in part, to assess the immediate and long-term effects of a residential summer weight-loss program on adolescents’ and preadolescents’ self-concept, body esteem, self-esteem, weight-loss success, and lifestyle change. The research was conducted over two summers at a residential program, and for those participants enrolled for both summers, only the data from their first year of participation was included in this analysis. Analysis of the cohorts from the two summers revealed no differences that were significant at the p < .05 level in demographic composition, initial body weight (t = .13), initial body mass index (BMI), calculated by dividing a person’s weight in kilograms by height in meters squared (kg/m2), (t = −.27), weight loss during treatment (t = −.84), or BMI change during treatment (t = −.93). As a result, the cohorts were combined for all statistical analyses. The campers ranged in age from 12 to 18 years of age (M = 13.7 years, SD = 1.5) and 76 percent were White, 11.5 percent were Black, and 7.3 percent were Hispanic. Although participants were from a range of socioeconomic backgrounds, the sample was predominantly middle class. The mean BMI at the start of camp was 34.9 (range 23.6–49.0, SD = 5.6), and campers lost an average of 16.56 lbs (SD = 9.17) and had a decrease of nearly 3 BMI points (M = 2.90, SD = 1.35).
Procedure
Participants were identified through their registration at the summer weight loss camp. Initial recruitment for camp participation was done through publicly available brochures targeting this population, as well as summer camp databases, the Internet, and camp and health fairs. Research-specific recruitment consisted of informational mailings, follow-up phone conversations, and in-person meetings (at camp check-in) with the parents of enrolled campers. All registered camp participants between the ages of 12 and 18 were recruited for this study if there was parental endorsement of the adolescents’ ability to read independently in English and a willingness to comply with study procedures. The first contact with participants was initiated via mail and included a description of the study and its procedures and consent forms for the parents or guardians to provide written consent for their adolescent’s participation. After consent had been obtained, a one hour research session was conducted at the camp within the youth participants’ first full two days, and the study and its procedures were described fully and youth assent was obtained at that time. The campers also completed a demographics form and questionnaire forms addressing self-esteem, body esteem, depressive symptoms, attitudes regarding weight and the overweight, feelings about their own weight, and perceptions of teasing. All participants’ heights and weights were recorded upon camp check-in. Program staff also completed weekly assessments of adolescents’ levels of participation and social involvement during the program.
Measures
Adolescent Characteristics
Participant characteristics were assessed through a demographics form that included questions about age, gender, race, grade in school, and living situation.
Weight Status
Camp nursing and nutrition staff trained in methods of obtaining accurate anthropometric measures obtained height and weight from participants upon camp intake. Participants were weighed and measured in athletic apparel without shoes. These data were then used to calculate BMI (kg/m2). For adults, an ideal BMI is between 20 and 25; above 25 is considered overweight and above 30 is considered obese. For children, classifications of overweight status are based on National Growth Charts and the percentile in which a child falls based on age. Children are typically described as being ‘at risk for overweight’ if their BMI is within the 85th–94.99th percentile (adjusted for gender and age), and ‘overweight’ if their BMI is at the 95th percentile or higher. Although these percentile-based categories of weight are important for identifying physical health risks among children, it is not clear from existing research as to what extent percentile-based cutoffs are meaningful for understanding weight stigma or psychosocial functioning in youth (Puhl & Latner, 2007). Therefore, our analyses used the standard equation of BMI rather than percentile-based category identifications. Moreover, while some of the children in this sample may technically fall below the ‘overweight’ or ‘at risk’ percentile classifications, the fact that they are seeking weight loss treatment indicates that their weight status is problematic in their lives in some way, and campers’ perceptions of their weight status were also assessed through a single question on the camper demographic form (‘How would you describe your own weight: smaller than average, about average, somewhat bigger than average, much bigger than average’).
Self-esteem
Adolescent self-esteem was measured using the Rosenberg scale, a 10-item measure with a four-point response scale (strongly agree to strongly disagree), assessing overall feelings about the self (Rosenberg, 1965). The Rosenberg self-esteem scale is perhaps the most widely used self-esteem measure in social science research. It was originally developed on an adolescent sample and has been validated with numerous populations.
Body Esteem
Adolescents’ body esteem was assessed by the body esteem scale (Mendelson & White, 1982), a measure of physical-appearance self-concept—how individuals value their appearance and body. The body esteem scale is a 24-item scale with a two-item response set (yes/no) that assesses overall, non-specific body esteem (e.g., ‘I like what I look like in pictures’, ‘I’m proud of my body’) and has been found to be suitable for use with all age ranges, including young children (Mendelson & White, 1982). Responses for all items were summed to create a total body esteem score.
Depressive Symptoms
The Center for Epidemiologic Studies depression scale (Radloff, 1977) was used to measure participants’ depressive symptoms. The Center for Epidemiologic Studies depression scale was originally developed for use with adults but has proven reliable and valid in previous research with adolescents (Radloff, 1991). The Center for Epidemiologic Studies depression scale consists of 20 items that were selected for inclusion from previously validated depression scales and are considered to represent the major components of depressive symptomatology as identified from clinical literature and analytic studies. Respondents rate their experience of 20 symptoms on a four-point scale (rarely to most or all of the time).
Anti-fat Attitudes
To measure adolescents’ attitudes about the overweight and being overweight, Crandall’s (1994) anti-fat attitudes questionnaire was administered. The measure was renamed ‘attitudes about weight and dieting’ for this study to eliminate the potential negative impact the original title might have on this particular population. The anti-fat attitude consists of 13 items rated on a 10-point Likert-type scale (strongly disagree to strongly agree) and has been validated in an overweight population (Crandall, 1994).
Feelings and Concerns about Weight
Campers’ feelings about their weight were assessed with a questionnaire specifically developed for this study that consisted of five items (‘My weight is the thing that makes me the most unhappy’, ‘I worry that I won’t be able to do everything I want to do because of my weight’, ‘I worry that my weight will… affect my relationships when I am older’, ‘… prevent me from being happy’, ‘… prevent me from being successful’) rated on a five-point Likert-type scale (strongly disagree to strongly agree). These five items were summed to produce a measure of participants’ worries about weight, and an analyses of this five-item scale indicated acceptable reliability (α= .85).
Teasing
Adolescents’ perceptions of teasing were assessed with Thompson’s (1999) perception of teasing scale. The 26-item perception of teasing scale first asks respondents to indicate on a five-point Likert scale how often they have experienced 13 specific forms of teasing (1 = never to 5 = very often) and then asks them to rate how upset they were by each specific form of teasing (1 = not upset; 5 = very upset). Eight questions represent instances of WRT and included items such as: ‘People made fun of you because you were heavy’ and ‘People pointed at you because you were overweight’. Five questions represent instances of CRT and included such items as: ‘People laughed at you because you didn’t understand something’ and ‘People made fun of you because you were afraid to do something’. The WRT and CRT questions are separately summed to form scales assessing prevalence of and distress related to each form of teasing. The perception of teasing scale has shown high convergence with other measures of teasing and exhibits acceptable internal consistency and reliability (Thompson et al., 1995).
Participation and Social Involvement
At the end of each week of the program, and prior to the weekly ‘weigh-in’, camp staff rated individual adolescents’ levels of program participation and social involvement. These ratings were obtained through a verbal consensus of each camper’s residential staff group, which consisted of two camp counselors. These counselor raters were unaware of campers’ other psychosocial scores. Using a five-point scale (not at all to extremely), counselors rated campers on two areas: activity involvement (One item: ‘How involved has this camper been with the camp activities this week’) and sociability (One item: ‘How sociable has this camper been with the other campers/staff this week’).
Body Concern
To address questions of participants’ global concerns about weight, a composite index of ‘body concern’ was created and consisted of participants’ scores on the body esteem scale, ‘feelings and concerns about weight’, and the anti-fat attitudes scale. It was believed that compiling these measures would yield a different perspective on adolescents’ feelings about these issues that might be less impacted by socially desirable reporting on the individual measures.
Analytic Strategy
Simple comparisons were conducted using t-tests for hypotheses regarding differences in the prevalence of and distress related to the two types of teasing (WRT and CRT) and gender differences in teasing experiences. Regression analyses were used to investigate the relationships between BMI and teasing, teasing and anti-fat attitudes, and anti-fat attitudes and psychosocial functioning. Simple slopes analyses were performed to look at two-way interactions between the variables of interest corresponding to our hypotheses. For interpretation of significant interaction effects including the graphs included in this article, we graphed the results using representative values of the independent variables (+/− 1 SD).
Results
Experiences of Teasing
Table 1 contains descriptive statistics of the major variables of interest, and Table 2 displays inter-correlations between the variables. Overall, participants reported experiencing frequent teasing and were upset by these experiences. Independent samples t-tests indicated there were no significant gender differences in reported prevalence of either form of teasing or in reported level of distress related to teasing. All participants reported having experienced some form of WRT, and 93 percent reported being distressed by these teasing experiences. A repeated measures t-test showed that participants reported significantly more frequent WRT than CRT (t (91) = 9.3, p < .001). Additionally, participants were significantly more upset by WRT experiences than by CRT experiences (t(85) = 11.01, p < .001). Regression analyses were conducted to assess how frequency of teasing was related to distress about teasing. Controlling for participant BMI, frequency of teasing was significantly associated with distress about teasing such that more frequent teasing was related to higher levels of distress (WRT: β = .82, t(87) = 13.17, p < .001; CRT: β = .70, t(85) = 9.07, p < .001).
Table 1.
Descriptive Statistics
| Range | Mean | SD | |
|---|---|---|---|
| Body mass index | 23.57–49.04 | 34.86* | 5.63 |
| Age | 12–18 | 13.69 | 1.47 |
| Frequency of weight-related teasing | 8–40 | 18.38 | 8.29 |
| Distress related to weight-related teasing | 1–40 | 18.47 | 10.00 |
| Frequency of competence-related teasing | 5–25 | 11.21 | 4.53 |
| Distress related to competence-related teasing | 2–25 | 8.94 | 5.27 |
| Perception of own weight status | 1–4 | 3.32 | .55 |
| Self-esteem | 15–40 | 29.03** | 5.93 |
| Body esteem | 0–19 | 6.42* | 4.66 |
| Worries about weight | 5–25 | 16.62 | 5.37 |
| Depression | 19–65 | 36.48 | 10.72 |
| Anti-fat attitudes | 22–42 | 33.05 | 3.59 |
| Program participation, week 1 | 1–5 | 3.92 | 1.07 |
| Program participation, week 2 | 1–5 | 3.82 | .90 |
| Camp social involvement, week 1 | 2–5 | 3.94* | 1.03 |
| Camp social involvement, week 2 | 1–5 | 4.07 | .95 |
Note:
p < .05 (significantly different by gender);
p < .10 (marginally significant difference by gender).
Table 2.
Correlations among Variables
| Age | Gender | BMI | PWT | UWT | PCT | UCT | SE | BES | DEP | AFA | WOR | PAR1 | PAR2 | SOC1 | |
| Age | |||||||||||||||
| Gender | .05 | ||||||||||||||
| BMI | .22* | −.23* | |||||||||||||
| PWT | .01 | −.11 | .10 | ||||||||||||
| UWT | −.04 | −.05 | −.02 | .82*** | |||||||||||
| PCT | −.05 | −.07 | −29** | .46*** | .35*** | ||||||||||
| UCT | −.09 | −.03 | −.23* | .47*** | .60*** | .70*** | |||||||||
| SE | −.24* | −.17 | −.21 | −.30** | −.26** | −.10 | −.11 | ||||||||
| BES | −.11 | −.24* | −.18 | −.33** | −.34** | −.24* | −.30** | .55*** | |||||||
| DEP | .14 | .08 | .24* | .28** | .17 | .06 | .13 | −.63*** | −.39*** | ||||||
| AFA | .13 | .03 | −.10 | .14 | .06 | .32** | .16 | −.34** | −.24* | .24* | |||||
| WOR | .24* | .09 | .19 | .44*** | .46*** | .19 | .39*** | −.46*** | −.41*** | .43*** | .24* | ||||
| PAR1 | −.13 | −.07 | −.11 | −.13 | −.07 | .14 | .06 | .16 | .02 | −.24* | −.01 | −.08 | |||
| PAR2 | −.09 | .04 | −.41*** | −.19 | −.12 | .24* | .06 | .03 | .05 | −.22* | −.03 | −.04 | .59*** | ||
| SOC1 | −.18 | −.25* | −.03 | −.04 | .02 | .15 | .10 | .14 | −.07 | −.28** | −.01 | −.10 | .46*** | .40*** | |
| SOC2 | −.12 | −.04 | −.06 | −.08 | .05 | .15 | .10 | .04 | −.01 | −.12 | −.10 | −.01 | .30** | .57*** | .54*** |
p < .05;
p < .01;
p < .001.
BMI = body mass index; PWT = prevalence of weight-related teasing; UWT = upset over weight-related teasing; PCT = prevalence of competence-related teasing; UCT = upset over competence-related teasing; SE = self-esteem; BES = body esteem; DEP = depressive symptoms; AFA = anti-fat attitudes; WOR = worries about weight; PAR1 = participation in camp activities in week 1; PAR2 = participation in camp activities in week 2; SOC1 = social involvement in week 1; SOC2 = social involvement in week 2.
We anticipated BMI would be associated with participants’ experiences of WRT but found that BMI was not significantly associated with either frequency or feelings of distress about WRT. However, participants’ BMI was significantly related to the frequency of CRT (β = −.29, t (85) = −2.79, p < .01). As participants’ BMI increased, prevalence of CRT decreased. See Table 3 for a summary of the regression analyses in this section.
Table 3.
Regression Analysis Summary for Experiences of Teasing
| Dependent variable | Predictor | β | R2 |
| Frequency of weight-related teasing |
.01 | ||
| Body mass index | .10 | ||
| Weight-related teasing distress | .66 | ||
| Frequency of weight-related teasing |
.82*** | ||
| Body mass index | −.07 | ||
| Frequency of competence-related teasing |
.08 | ||
| Body mass index | −.29** | ||
| Competence-related teasing distress |
.48 | ||
| Frequency of competence-related teasing |
.68*** | ||
| Body mass index | −.04 |
p < .01;
p < .001.
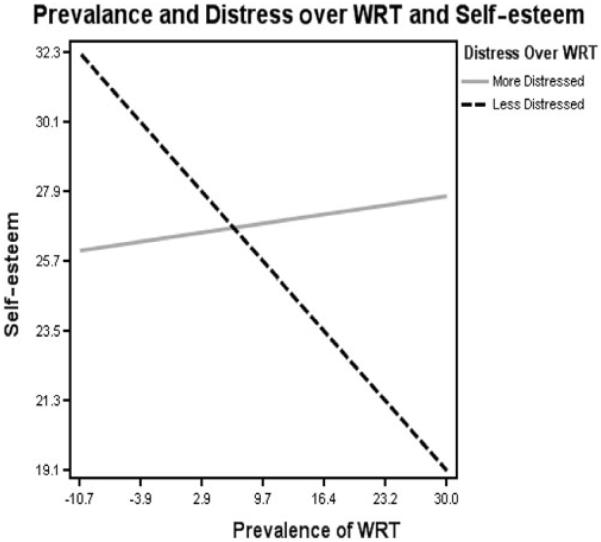
Teasing and Functioning
Regression analyses were conducted to investigate the relationships between teasing and psychosocial functioning. Because previous research with this population found significant correlations between participants’ pretreatment BMI and their psychosocial functioning across domains (Quinlan, Costanzo, & Hoy, 2005), BMI was controlled for in all regression analyses. There was a significant interaction between frequency of WRT and distress related to WRT for participants’ self-esteem and depressive symptoms (self-esteem: β = −.30, t(80) = 2.55, p < .05; depressive symptoms: β = −.35, t(79) = −2.99, p < .01). Simple slopes analyses revealed that those adolescents most distressed by teasing exhibited lower self-esteem and higher depressive symptoms regardless of the reported frequency of teasing. For adolescents less distressed by teasing experiences, increased frequency of teasing was associated with worse functioning (i.e., lower self-esteem and higher depressive symptoms). Figure 1 presents this interaction graphically. Additionally, participants who were more upset by WRT worried more about their weight (β = .37, t(80) = 2.19, p < .05). No significant interactions were found for body esteem or participants’ worries about weight.
Figure 1.
Interaction between Prevalence of and Distress Related to Weight-related Teasing and Participant Self-esteem.
Parallel analyses investigating the effects of CRT showed a significant interaction between frequency of and upset related to CRT for participants’ depressive symptoms (β = −.31, t(77) = −2.14, p < .05). For participants who were more distressed by CRT experiences, increased frequency of CRT was associated with greater depression scores. However, for participants who were less distressed by CRT, increased CRT frequency was associated with decreased depressive symptoms. Additionally, distress over CRT was positively associated with participants’ worries about their weight (β = .45, t(78) = 3.05, p < .01). No other significant interaction or main effects were found for self-esteem, body esteem, or participants’ worries about their weight. Table 4 presents regression weights (b) for the main and interaction effects between prevalence of and distress about teasing experiences and psychosocial functioning.
Table 4.
Regression Analysis Summary for Teasing and Functioning
| Dependent variable | Predictor | β | R2 | ΔR2 |
|---|---|---|---|---|
| Self-esteem | ||||
| WRT | ||||
| Step 1 | .102 | |||
| BMI | −.20 | |||
| WRT frequency | −.13 | |||
| WRT distress | −.13 | |||
| Step 2 | .169 | .067 | ||
| BMI | −.16 | |||
| WRT frequency | −.20 | |||
| WRT distress | −.21 | |||
| WRT frequency × distress | .30* | |||
| CRT | ||||
| Step 1 | .079 | |||
| BMI | −.27* | |||
| CRT frequency | −.14 | |||
| CRT distress | −.07 | |||
| Step 2 | .100 | .021 | ||
| BMI | −.29* | |||
| CRT frequency | −.16 | |||
| CRT distress | −.19 | |||
| CRT frequency × distress | .19 | |||
| Depression | WRT | |||
| Step 1 | .100 | |||
| BMI | .21* | |||
| WRT frequency | .28 | |||
| WRT distress | −.08 | |||
| Step 2 | .191 | .091 | ||
| BMI | .17 | |||
| WRT frequency | .36* | |||
| WRT distress | .01 | |||
| WRT frequency × distress | −.35** | |||
| CRT | ||||
| Step 1 | .100 | |||
| BMI | .30* | |||
| CRT frequency | −.01 | |||
| CRT distress | .19 | |||
| Step 2 | .150 | .050 | ||
| BMI | .33* | |||
| CRT frequency | .03 | |||
| CRT distress | .38* | |||
| CRT frequency × distress | −.31* | |||
| Body Esteem | ||||
| WRT | ||||
| Step 1 | .127 | |||
| BMI | −.17 | |||
| WRT frequency | −.03 | |||
| WRT distress | −.29 | |||
| Step 2 | .134 | .007 | ||
| BMI | −.16 | |||
| WRT frequency | −.06 | |||
| WRT distress | −.31 | |||
| WRT frequency × distress | .09 | |||
| CRT | ||||
| Step 1 | .160 | |||
| BMI | −.27* | |||
| WRT frequency | −.21 | |||
| WRT distress | −.20 | |||
| Step 2 | .160 | .00 | ||
| BMI | −.27* | |||
| CRT frequency | −.21 | |||
| CRT distress | −.19 | |||
| CRT frequency × distress | −.01 | |||
| Weight worries | ||||
| WRT | ||||
| Step 1 | .231 | |||
| BMI | .17 | |||
| WRT frequency | .14 | |||
| WRT distress | .33 | |||
| Step 2 | .252 | .021 | ||
| BMI | .15 | |||
| WRT frequency | .18 | |||
| WRT distress | .37* | |||
| WRT frequency × distress | −.16 | |||
| CRT | ||||
| Step 1 | .201 | |||
| BMI | .26* | |||
| CRT frequency | .01 | |||
| CRT distress | .43* | |||
| Step 2 | .207 | .006 | ||
| BMI | .27* | |||
| CRT frequency | .02 | |||
| CRT distress | .49* | |||
| CRT frequency × distress | −.11 |
p < .05;
p < .01.
WRT = weight-related teasing; CRT = competence-related teasing; BMI = body mass index.
Teasing and Anti-fat Attitudes
The next set of analyses assessed relationships between teasing experiences and anti-fat attitudes, controlling for BMI. WRT frequency and distress about both WRT and CRT were unrelated to anti-fat attitudes; however, frequency of CRT was significantly associated with anti-fat attitudes (β = .32, t(88) = 3.11, p < .01). Participants with higher anti-fat attitudes had lower levels of self-esteem (β = −.35, t(84) = −3.76, p < .001), lower levels of body esteem (β = −.22, t(83) = −2.27, p < .05) and higher levels of depressive symptoms (β = .22, t(83) = 2.55, p < .05), and they were worried more about their own weight (β = .20, t(82) = 2.33, p < .05). However, anti-fat attitudes did not act as a moderator of the relationship between teasing and psychosocial functioning for either WRT or CRT. Table 5 presents regression weights (b) for the main and interaction effects between frequency of and distress related to teasing and anti-fat attitudes.
Table 5.
Regression Analysis Summary for Teasing and Anti-fat Attitudes
| Dependent variable | Predictor | β | R2 | ΔR2 |
|---|---|---|---|---|
| Anti-fat attitudes | ||||
| WRT | ||||
| BMI | −.12 | .046 | ||
| WRT frequency | .31 | |||
| WRT distress | −.21 | |||
| CRT | ||||
| BMI | −.04 | .114 | ||
| CRT frequency | .32** | |||
| CRT distress | −.17 | |||
| Self-esteem | ||||
| WRT | ||||
| Step 1 | .236 | |||
| BMI | −.22* | |||
| WRT frequency | −.23* | |||
| AFA | −.35** | |||
| Step 2 | .236 | .000 | ||
| BMI | −.22* | |||
| WRT frequency | −.23* | |||
| AFA | −.35** | |||
| WRT frequency × AFA | .00 | |||
| CRT | ||||
| Step 1 | .193 | |||
| BMI | −.27* | |||
| CRT frequency | −.09 | |||
| AFA | −.36** | |||
| Step 2 | .193 | .000 | ||
| BMI | −.27* | |||
| CRT frequency | −.09 | |||
| AFA | −.36** | |||
| CRT frequency × AFA | −.01 | |||
| Depression | ||||
| WRT | ||||
| Step 1 | .181 | |||
| BMI | .24* | |||
| WRT frequency | .24* | |||
| AFA | .22* | |||
| Step 2 | .191 | .010 | ||
| BMI | .24* | |||
| WRT frequency | .21 | |||
| AFA | .23* | |||
| WRT frequency × AFA | .10 | |||
| CRT | ||||
| Step 1 | .139 | |||
| BMI | .31** | |||
| CRT frequency | .13 | |||
| AFA | .22* | |||
| Step 2 | .141 | .002 | ||
| BMI | .31** | |||
| CRT frequency | .12 | |||
| AFA | .23* | |||
| CRT frequency × AFA | .04 | |||
| Body esteem | ||||
| WRT | ||||
| Step 1 | .160 | |||
| BMI | −.17 | |||
| WRT frequency | −.26* | |||
| AFA | −.22* | |||
| Step 2 | .163 | .003 | ||
| BMI | −.17 | |||
| WRT frequency | −.24* | |||
| AFA | −.22* | |||
| WRT frequency × AFA | −.05 | |||
| CRT | ||||
| Step 1 | .161 | |||
| BMI | −.27* | |||
| CRT frequency | −.28* | |||
| AFA | −.18 | |||
| Step 2 | .163 | .002 | ||
| BMI | −.27* | |||
| CRT frequency | −.27* | |||
| AFA | −.19 | |||
| CRT frequency × AFA | −.05 | |||
| Weight worries | ||||
| WRT | ||||
| Step 1 | .242 | |||
| BMI | .17 | |||
| WRT frequency | .39*** | |||
| AFA | .20* | |||
| Step 2 | .247 | .005 | ||
| BMI | .17 | |||
| WRT frequency | .41*** | |||
| AFA | .18 | |||
| WRT frequency × AFA | −.08 | |||
| CRT | ||||
| Step 1 | .131 | |||
| BMI | .27* | |||
| CRT frequency | .21 | |||
| AFA | .19 | |||
| Step 2 | .132 | .001 | ||
| BMI | .27* | |||
| CRT frequency | .20 | |||
| AFA | .19 | |||
| CRT frequency × AFA | .02 |
p < .05;
p < .01;
p < .001.
WRT = weight-related teasing; CRT = competence-related teasing; BMI = body mass index; AFA = anti-fat attitudes.
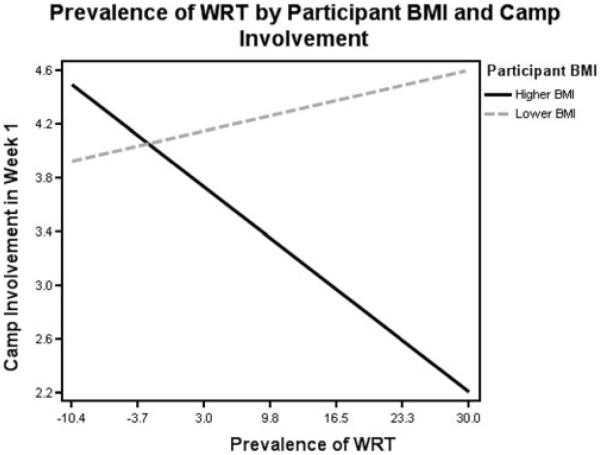
Teasing and Behavior
We next examined the effects of teasing experiences on participants’ involvement in camp activities. The frequency of WRT was significantly related to camp involvement in weeks 1 and 2, but this effect differed by BMI (week 1: β = −.27, t(83) = −2.60, p < .01; week 2: β = −.21, t(81) = −2.14, p < .05). For participants with lower BMI scores, there was no effect of the frequency of WRT on involvement in camp activities. For participants with higher BMI scores, more frequent WRT was associated with less involvement in camp activities (see Figure 2). There was a similar interaction between frequency of WRT and BMI related to social involvement at camp in weeks 1 and 2 (week 1: β = −.27, t(83) = −2.56, p < .05; week 2: β = −.22, t(81) = −2.01, p < .05). For participants with lower BMIs, greater reported frequency of WRT was associated with higher social involvement at camp. For participants with higher BMI scores, more frequent WRT was associated with less social involvement at camp.
Figure 2.
Interaction between Weight-related Teasing Prevalence and Body Mass Index and Involvement with Camp Activities.
The amount of distress about WRT was also differentially related to camp involvement in the first week of camp, depending on the participant’s BMI (week 1: β = −.29, t(81) = −2.75, p < .01). For participants with lower BMI, the more upset the participant was about WRT, the more involved they were in camp in week 1. For participants with higher BMI scores, this relationship was reversed such that the more upset they were about WRT, the less involved they were at camp. Distress over WRT was also related to social involvement in camp during weeks 1 and 2 and differed, depending on the participant’s BMI (week 1: β = −.28, t(81) = −2.56, p < .01; week 2: β = −.24, t(79) = −2.11, p < .05). For lighter participants, the more upset they were about WRT experiences, the more socially involved they were at camp, while for heavier partici-pants the opposite was true.
CRT frequency and distress were not significantly related to camp involvement or social participation. Table 6 presents regression weights (β) for the main and interac-tion effects related to camp involvement and social interaction.
Table 6.
Regression Analysis Summary for Teasing and Behavior
| Dependent variable | Predictor | β | R2 | ΔR2 |
|---|---|---|---|---|
| Camp involvement week 1 | ||||
| WRT frequency | ||||
| Step 1 | .026 | |||
| BMI | −.09 | |||
| WRT frequency | −.12 | |||
| Step 2 | .099 | .073 | ||
| BMI | −.10 | |||
| WRT frequency | −.16 | |||
| WRT frequency × BMI | −.27* | |||
| WRT distress | ||||
| Step 1 | .020 | |||
| BMI | −.13 | |||
| WRT distress | −.06 | |||
| Step 2 | .103 | .083 | ||
| BMI | −.13 | |||
| WRT distress | −.11 | |||
| WRT distress × BMI | −.29** | |||
| CRT frequency | ||||
| Step 1 | .028 | |||
| BMI | −.07 | |||
| CRT frequency | .13 | |||
| Step 2 | .051 | .023 | ||
| BMI | −.02 | |||
| CRT frequency | .17 | |||
| CRT frequency × BMI | .16 | |||
| CRT distress | ||||
| Step 1 | .009 | |||
| BMI | −.08 | |||
| CRT distress | −.04 | |||
| Step 2 | .017 | .008 | ||
| BMI | −.10 | |||
| CRT distress | .01 | |||
| CRT distress × BMI | −.09 | |||
| Camp involvement week 2 | ||||
| WRT frequency | ||||
| Step 1 | .200 | |||
| BMI | −.39*** | |||
| WRT frequency | −.18 | |||
| Step 2 | .242 | .042 | ||
| BMI | −.40*** | |||
| WRT frequency | −.21* | |||
| WRT frequency × BMI | −.21* | |||
| WRT distress | ||||
| Step 1 | .192 | |||
| BMI | −.42*** | |||
| WRT distress | −.14 | |||
| Step 2 | .206 | .014 | ||
| BMI | −.42*** | |||
| WRT distress | −.16 | |||
| WRT distress × BMI | −.12 | |||
| CRT frequency | ||||
| Step 1 | .184 | |||
| BMI | −.37** | |||
| CRT frequency | .13 | |||
| Step 2 | .185 | .001 | ||
| BMI | −.36** | |||
| CRT frequency | .14 | |||
| CRT frequency × BMI | .04 | |||
| CRT distress | ||||
| Step 1 | .146 | |||
| BMI | −.39** | |||
| CRT distress | −.05 | |||
| Step 2 | .151 | .005 | ||
| BMI | −.40*** | |||
| CRT distress | −.07 | |||
| CRT distress × BMI | −.08 | |||
| Social involvement week 1 | ||||
| WRT frequency | ||||
| Step 1 | .002 | |||
| BMI | −.04 | |||
| WRT frequency | −.03 | |||
| Step 2 | .075 | .073 | ||
| BMI | −.04 | |||
| WRT frequency | −.07 | |||
| WRT frequency × BMI | −.27* | |||
| WRT distress | ||||
| Step 1 | .004 | |||
| BMI | −.05 | |||
| WRT distress | .03 | |||
| Step 2 | .078 | .074 | ||
| BMI | −.06 | |||
| WRT distress | −.01 | |||
| WRT distress × BMI | −.28* | |||
| CRT frequency | ||||
| Step 1 | .024 | |||
| BMI | .01 | |||
| CRT frequency | .16 | |||
| Step 2 | .028 | .004 | ||
| BMI | −.01 | |||
| CRT frequency | .14 | |||
| CRT frequency × BMI | −.07 | |||
| CRT distress | ||||
| Step 1 | .011 | |||
| BMI | .03 | |||
| CRT distress | .11 | |||
| Step 2 | .053 | .042 | ||
| BMI | −.01 | |||
| CRT distress | .04 | |||
| CRT distress × BMI | −.22 | |||
| Social involvement week 2 | ||||
| WRT frequency | ||||
| Step 1 | .013 | |||
| BMI | −.05 | |||
| WRT frequency | −.10 | |||
| Step 2 | .060 | .047 | ||
| BMI | −.06 | |||
| WRT frequency | −.13 | |||
| WRT frequency × BMI | −.22* | |||
| WRT distress | ||||
| Step 1 | .003 | |||
| BMI | −.05 | |||
| WRT distress | .02 | |||
| Step 2 | .056 | .053 | ||
| BMI | −.05 | |||
| WRT distress | −.02 | |||
| WRT distress × BMI | −.24* | |||
| CRT frequency | ||||
| Step 1 | .022 | |||
| BMI | −.02 | |||
| CRT frequency | .14 | |||
| Step 2 | .033 | .011 | ||
| BMI | .01 | |||
| CRT frequency | .17 | |||
| CRT frequency × BMI | .11 | |||
| CRT distress | ||||
| Step 1 | .008 | |||
| BMI | .05 | |||
| CRT distress | .08 | |||
| Step 2 | .009 | .001 | ||
| BMI | .05 | |||
| CRT distress | .07 | |||
| CRT distress × BMI | −.04 | |||
p < .05;
p < .01;
p < .001.
WRT = weight-related teasing; CRT = competence-related teasing; BMI = body mass index.
Discussion
This study investigated the relationships between peer teasing and psychosocial functioning, attitudes, and behavior in an overweight, treatment-seeking adolescent sample and further assessed whether weight-related and competency-related teasing evidence similar relationships with functioning. As expected, all participants reported having experienced some form of teasing, with WRT being both more frequent and more distressing than CRT. Despite some research showing that females face more appearance-based or weight-based discrimination, and are more upset by teasing (Eisenberg et al., 2003; Neumark-Sztainer et al., 2002), we found no gender differences. However, there were likely not enough males in this sample to adequately find gender differences that may exist. Also contrary to our hypotheses, adolescents’ weight was not related to reports of WRT frequency or distress, but was related to CRT. Heavier adolescents reported experiencing less CRT and were less distressed by such teasing. One possible explanation is that teasing targets the most obvious ‘weakness’, and for heavier adolescents, weight (rather than competence) is this mark. Conversely, perhaps individuals are most aware of, and distressed by, teasing related to their greatest weakness, and attacks on other domains are therefore less noticeable or distressing in comparison.
This study further supports the belief that excess weight in adolescence is associated with significant psychological risks related to problematic social interactions. Regardless of actual BMI, adolescents’ reports of WRT experiences were significantly and negatively related to multiple psychosocial domains. Although teasing frequency and distress were highly correlated, and it is difficult to untangle the individual contributions of each, it appears that both uniquely affect psychosocial functioning. For adolescents most distressed by WRT, infrequent teasing seemed to be as harmful as frequent teasing, while for least distressed adolescents, a lower frequency exacted a lesser toll on self-esteem and depressive symptoms.
There was also a significant, and unexpected, interaction between CRT frequency and distress and participants’ depressive symptoms. For adolescents most distressed by CRT, more frequent teasing was associated with greater depression scores; however, for adolescents less distressed by CRT, more frequent teasing was associated with decreased depressive symptoms. This is opposite to the WRT findings and may be due to the least distressed participants having developed protective mechanisms to deal with their weight. These overweight adolescents may have learned to draw their sense of self from other domains, such as academic or interpersonal competence, and therefore must protect these domains in order to maintain a positive view of the self. The reported decrease in depressive symptoms despite the increased frequency of CRT may reflect a strong form of this protective system.
Additionally, contrary to our hypotheses, while CRT was not significantly related to self-esteem or depressive symptoms, it was related to body esteem, weight-worries, and anti-fat attitudes. Perhaps this non-WRT was significantly, and negatively, associated with weight-specific feelings precisely because such teasing does not overtly target appearance. Overweight individuals are prejudiced against other overweight individuals as much as non-overweight individuals are (e.g., Crandall, 1994), suggesting they internalize anti-fat messages. However, no direct relationship was found between weight-specific stigmatization and overweight adults’ anti-fat beliefs (Friedman et al., 2005). These current findings suggest teasing that does not overtly target weight is most successful at transmitting common anti-fat stereotypes. Overweight individuals may be so accustomed to negative weight-related comments that they have developed ready defenses against them. But they may be less defended against competence-specific teasing and thus begin to acknowledge, and believe, the popular negative fat stereotypes (i.e., stupid, lazy, clumsy) that are often central to CRT. It may be this internalization of the negative overweight identity that explains the connection between weight-related stigma and psychosocial functioning.
Related to this, Friedman et al. (2005) reported that anti-fat attitudes were an important component in the relationship between weight stigmatized identity and body image. Similarly, we found that teasing, a form of stigmatizing experience, was largely unrelated to anti-fat attitudes, but that individuals holding more anti-fat attitudes evidenced worse psychosocial functioning. However, in this study, anti-fat attitudes did not moderate the relationship between stigmatizing experiences and psychosocial functioning. This difference between adult and adolescent samples may point to some interesting developmental hypotheses. Peer social acceptance is at the forefront of adolescent experience, and therefore, any stigmatizing social experience may be harmful to functioning in overweight adolescents. Adults are somewhat removed from this immediate peer emphasized environment, and the effects of stigmatization on their functioning may be more reflective of how well the experiences match with their own beliefs. For adults, perhaps it is a history of repeated teasing that forms their ideologies. Subsequent work should investigate the transition from the immediate negative effects of teasing to the development of ideologies.
Finally, as hypothesized, both frequency of, and distress about, WRT was significantly associated with adolescents’ involvement with the treatment program and peers and this relationship differed by BMI. Adolescents who weighed less and reported more frequent or distressing WRT were more involved with their peers and the activities. However, adolescents who weighed more and reported more frequent or distressing WRT were less involved. Because of the cross-sectional nature of this data, it is unclear whether the most severely overweight adolescents are less involved because they have the most negative self-perceptions, feel the least efficacious, and are the most fearful of being further stigmatized, or whether those adolescents who are most sensitive to teasing and most inclined to withdraw have a long-standing pattern of retreating from social and athletic activities and this has led to greater weight gain. Surprisingly, despite its focus on one’s lack of ability or skill, CRT did not evidence similar relationships to social involvement or activity participation, suggesting that for these treatment-seeking adolescents, it is weight-specific stigmatization that may be most motivating for the lightest of them and most discouraging for the heaviest.
There were several limitations to this research study. This was a self-selected, mainly middle to upper socioeconomic status sample of mostly White females, and it is unclear whether these findings would generalize to other groups. Additionally, youth actively seeking weight-loss treatment may be more sensitive to weight-related peer and psychosocial issues than youth not seeking weight loss. Moreover, this research is cross-sectional in nature and both teasing experiences and psychosocial functioning were assessed by self-report measures, making it impossible to infer causality. Future research on these issues should be longitudinal and should attempt to more directly assess, either through the use of multiple informants or through the use of direct observation, levels of teasing experiences without relying solely on self report.
Despite these limitations, this study shows that adolescent overweight is not only associated with health risks, but also with psychological risks related to problematic peer interactions. Although we were unable to formally establish causality, this research does illuminate the relationships between WRT experiences and multiple psychosocial and behavioral factors. It also extends the body of knowledge related to teasing by showing that non-WRT is also negatively associated with functioning in overweight youth and may be key to the internalization of anti-fat stereotypes and the stigmatized overweight identity. The patterns of effects discerned in this study further highlight the need for effective prevention and intervention for experiences of peer teasing. Overweight youth may need help recognizing and adjusting to weight-related social issues while simultaneously learning to defend against the prevalent, and damaging, stereotypes of overweight that surface in negative peer interactions.
References
- Allon N. Tensions in interactions of overweight adolescent girls. Women and Health. 1976;1:14–20. [Google Scholar]
- Banis HT, Varni JW, Wallander JL, Korsch BM, Jay SM, Adler R, et al. Psychological and social adjustment of obese children and their families. Child Care, Health and Development. 1988;14:157–173. doi: 10.1111/j.1365-2214.1988.tb00572.x. [DOI] [PubMed] [Google Scholar]
- Baum CG, Forehand R. Social factors associated with adolescent obesity. Journal of Pediatric Psychology. 1984;9:293. doi: 10.1093/jpepsy/9.3.293. [DOI] [PubMed] [Google Scholar]
- Cash TF. Developmental teasing about physical appearance: Retrospective descrip-tions and relationships with body image. Social Behavior and Personality. 1995;23:123–130. [Google Scholar]
- Cramer P, Steinwert T. Thin is good, fat is bad: How early does it begin? Journal of Applied Developmental Psychology. 1998;19:429–451. [Google Scholar]
- Crandall CS. Prejudice against fat people: Ideology and self-interest. Journal of Personality and Social Psychology. 1994;66:882–894. doi: 10.1037//0022-3514.66.5.882. [DOI] [PubMed] [Google Scholar]
- Crandall CS, Biernat M. The ideology of anti-fat attitudes. Journal of Applied Social Psychology. 1990;20:227–243. [Google Scholar]
- Davison KK, Birch LL. Predictors of fat stereotypes among 9-year-old girls and their parents. Obesity Research. 2004;12:86–94. doi: 10.1038/oby.2004.12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eaton DK, Kann L, Kinchen S, Ross J, Hawkins J, Harris WA, et al. Youth risk behavior surveillance—United States, 2005. Morbidity and Mortality Weekly Report. 2006;55(SS-5):1–108. [PubMed] [Google Scholar]
- Eisenberg ME, Neumark-Sztainer D, Story M. Associations of weight-based teasing and emotional well-being among adolescents. Archives of Pediatrics and Adolescent Medicine. 2003;157:733–738. doi: 10.1001/archpedi.157.8.733. [DOI] [PubMed] [Google Scholar]
- Epstein LH, Myers MD, Anderson K. The association of maternal psychopa-thology and family socioeconomic status with psychological problems in obese children. Obesity Research. 1996;4:65–74. doi: 10.1002/j.1550-8528.1996.tb00513.x. [DOI] [PubMed] [Google Scholar]
- Fabian LJ, Thompson JK. Body image and eating disturbance in young females. International Journal of Eating Disorders. 1989;8:63–74. [Google Scholar]
- Faith MS, Leone MA, Ayers TS, Heo M, Pietrobelli A. Weight criticism during physical activity, coping skills, and reported physical activity in children. Pediatrics. 2002;110:1–8. doi: 10.1542/peds.110.2.e23. [DOI] [PubMed] [Google Scholar]
- Friedman KE, Reichmann SK, Costanzo PR, Zelli A, Ashmore JA, Musante GJ. Weight stigmatization and ideological beliefs: Relation to psychological functioning in obese adults. Obesity Research. 2005;13:907–916. doi: 10.1038/oby.2005.105. [DOI] [PubMed] [Google Scholar]
- Hayden-Wade HA, Stein RI, Ghaderi A, Saelens BE, Zabinski MF, Wilfley DE. Prevalence, characteristics, and correlates of teasing experiences among overweight children vs. non-overweight peers. Obesity Research. 2005;13:1381–1392. doi: 10.1038/oby.2005.167. [DOI] [PubMed] [Google Scholar]
- Hedley AA, Ogden CL, Johnson CL, Carroll MD, Curtin LR, Flegal KM. Prevalence of overweight and obesity among US children, adolescents, and adults. Journal of the American Medical Association. 2004;291:2847–2850. doi: 10.1001/jama.291.23.2847. [DOI] [PubMed] [Google Scholar]
- Heinberg LH, Thompson JK, Mateson JL. Body image dissatisfaction as a motivator for healthy lifestyle change: Is some stress beneficial? In: Striegel-Moore R, Smolak L, editors. Eating disorders: Innovative directions for research and practice. American Psychological Association; Washington, DC: 2001. pp. 215–232. [Google Scholar]
- Janssen I, Craig WM, Boyce WF, Pickett W. Associations between overweight and obesity with bullying behaviors in school-aged children. Pediatrics. 2004;113:1187–1194. doi: 10.1542/peds.113.5.1187. [DOI] [PubMed] [Google Scholar]
- Keltner D, Capps L, Kring AM, Young RC, Heerey EA. Just teasing: A conceptual analysis and empirical review. Psychological Bulletin. 2001;127:229–248. doi: 10.1037/0033-2909.127.2.229. [DOI] [PubMed] [Google Scholar]
- Kraig KA, Keel PK. Weight-based stigmatization in children. International Journal of Obesity. 2001;25:1661–1666. doi: 10.1038/sj.ijo.0801813. [DOI] [PubMed] [Google Scholar]
- Lagerspetz KMJ, Bjorkqvist K, Berts M, King E. Group aggression among school children in three schools. Scandinavian Journal of Psychology. 1982;23:45–52. [Google Scholar]
- Latner JD, Stunkard AJ. Getting worse: The stigmatization of obese children. Obesity Research. 2003;11:452–456. doi: 10.1038/oby.2003.61. [DOI] [PubMed] [Google Scholar]
- Lunner K, Werthem EH, Thompson JK, Paxton SJ, McDonald F, Halvaarson KS. A cross-cultural examination of weight-related teasing, body image, and eating disturbance in Swedish and Australian samples. International Journal of Eating Disorders. 2000;28:430–435. doi: 10.1002/1098-108x(200012)28:4<430::aid-eat11>3.0.co;2-y. [DOI] [PubMed] [Google Scholar]
- Melnyk BM, Small L, Morrison-Beedy D, Strasser A, Spath L, Kreipe R, et al. Mental health correlates of health lifestyle attitudes, beliefs, choices, and behaviors in overweight adolescents. Journal of Pediatric Health Care. 2006;20:401–406. doi: 10.1016/j.pedhc.2006.03.004. [DOI] [PubMed] [Google Scholar]
- Mendelson BK, White DR. Relation between body-esteem and self-esteem of obese and normal children. Perceptual and Motor Skills. 1982;54:899–905. doi: 10.2466/pms.1982.54.3.899. [DOI] [PubMed] [Google Scholar]
- Mooney A, Creeser R, Blatchford P. Children’s views on teasing and fighting in junior high school. Education Research. 1991;33:103–112. [Google Scholar]
- Neumark-Sztainer D, Falkner N, Story M, Perry C, Hannan PJ, Mulert S. Weight-teasing among adolescents: Correlations with weight status and disordered eating behaviors. International Journal of Obesity. 2002;26:123–131. doi: 10.1038/sj.ijo.0801853. [DOI] [PubMed] [Google Scholar]
- Puhl RM, Latner LD. Stigma, obesity, and the health of the nation’s children. Psychological Bulletin. 2007;133:557–580. doi: 10.1037/0033-2909.133.4.557. [DOI] [PubMed] [Google Scholar]
- Quinlan NJP, Costanzo PR, Hoy MB. The effects of a residential summer treatment program on weight loss and psychosocial outcomes in youth; Poster presented at the annual meeting of the North American Association for the Study of Obesity; Vancouver, BC, Canada. 2005. [Google Scholar]
- Quinn DM, Crocker J. When ideology hurts: Effects of belief in the Protestant ethic and feeling overweight on the psychological well-being of women. Journal of Personality and Social Psychology. 1999;77:402–414. doi: 10.1037//0022-3514.77.2.402. [DOI] [PubMed] [Google Scholar]
- Radloff L. The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:385–401. [Google Scholar]
- Radloff LS. The use of the Center of Epidemiologic Studies depression scale in adolescents and young adults. Journal of Youth and Adolescence. 1991;20:149–166. doi: 10.1007/BF01537606. [DOI] [PubMed] [Google Scholar]
- Rand CSW, Wright BA. Continuity and change in the evaluation of ideal and acceptable body sizes across a wide age span. International Journal of Eating Disorders. 2000;28:90–100. doi: 10.1002/(sici)1098-108x(200007)28:1<90::aid-eat11>3.0.co;2-p. [DOI] [PubMed] [Google Scholar]
- Richardson SA. Age and sex differences in values toward physical handicaps. Journal of Health and Social Behavior. 1970;11:207–214. [PubMed] [Google Scholar]
- Richardson SA. Handicap, appearance, and stigma. Social Science and Medicine. 1971;5:621–628. doi: 10.1016/0037-7856(71)90011-4. [DOI] [PubMed] [Google Scholar]
- Rosenberg M. Society and the adolescent self-image. Princeton University Press; Princeton, NJ: 1965. [Google Scholar]
- Sallis JF, Alcaraz JE, McKenzie TL, Hovell MF. Predictors of change in children’s physical activity over 20 months. Variation by gender and level of adiposity. American Journal of Prevention Medicine. 1999;16:222–229. doi: 10.1016/s0749-3797(98)00154-8. [DOI] [PubMed] [Google Scholar]
- Sigelman CK, Miller TE, Whitworth LA. The early development of stigmatizing reactions of physical differences. Journal of Applied Developmental Psychology. 1986;7:17–32. [Google Scholar]
- Storch EA, Milsom VA, DeBraganza N, Lewis AB, Geffken GR, Silverstein JH. Peer victimization, psychosocial adjustment, and physical activity in overweight and at-risk-for-overweight youth. Journal of Pediatric Psychology. 2007;32:80–89. doi: 10.1093/jpepsy/jsj113. [DOI] [PubMed] [Google Scholar]
- Strauss RS, Pollack HA. Epidemic increase in childhood overweight, 1986–1998. The Journal of the American Medical Association. 2001;286:2845–2848. doi: 10.1001/jama.286.22.2845. [DOI] [PubMed] [Google Scholar]
- Strauss RS, Pollack HA. Social marginalization of overweight children. Archives of Pediatrics and Adolescent Medicine. 2003;157:746–752. doi: 10.1001/archpedi.157.8.746. [DOI] [PubMed] [Google Scholar]
- Thompson JK. Exacting beauty: Theory, assessment, and treatment of body-image disturbance. American Psychological Association; Washington, DC: 1999. [Google Scholar]
- Thompson JK, Cattarin J, Fowler B, Fisher E. The perception of teasing scale (POTS): A revision and extension of the physical appearance-related teasing scale (PARTS) Journal of Personality Assessment. 1995;65:146–157. doi: 10.1207/s15327752jpa6501_11. [DOI] [PubMed] [Google Scholar]
- Tiggemann M, Rothblum ED. Gender difference in social consequences of perceived overweight in the United States and Australia. Sex Roles. 1988;18:75–86. [Google Scholar]
- Young-Hyman D, Schlundt DG, Herman-Wenderoth L, Bozylinski K. Obesity, appearance, and psychosocial adaptation in young African American children. Journal of Pediatric Psychology. 2003;28:463–472. doi: 10.1093/jpepsy/jsg037. [DOI] [PubMed] [Google Scholar]