Abstract
Symptom management research is a priority for both children and adults with cancer. The UCSF Symptom Management Theory (SMT) is a middle range theory depicting symptom management as a multidimensional process. A theory analysis using the process described by Walker and Avant evaluated the SMT with attention to application in research involving children with cancer. Application of the SMT in studies involving children has been limited to descriptive studies testing only portions of the theory. Findings of these studies have provided empiric support for the relationships proposed within the SMT. Considerations for future research involving children include attention to measurement of symptoms and clarity regarding the location of the parents and family within the model. With additional testing and refinement, the SMT has the potential to guide nursing research and practice to improve symptoms for children with cancer.
Keywords: theory analysis, UCSF symptom management theory, pediatric oncology nursing, research
Introduction
Research addressing symptom management is recognized as a priority for both children and adults with cancer (Berger, Cochrane, & Mitchell, 2009; Hockenberry, 2004). As research in this area grows, the need for relevant theories and conceptual models to guide this research, as well as related nursing practice, becomes increasingly important.
Theory development in nursing creates conceptual meaning by linking related concepts together in such a way as to illustrate meaning (Chinn & Kramer, 2004). As theoretical models are developed, they also should be subject to analysis. Theory analysis provides a systematic process through which strengths and inconsistencies of theories are identified. Identification of the strengths of a theory provides support for its utility in guiding clinical practice. Theory analysis also reveals opportunities for additional theory testing and refinement. Such opportunities could include extension of a theory’s applicability across health and illness states or across developmental groups, including children with cancer (Walker & Avant, 2005).
UCSF Symptom Management Theory and Project Aims
The UCSF Symptom Management Theory (SMT) is a deductive, middle range theory depicting symptom management as a multidimensional process occurring in the domains of nursing science (Humphreys et al., 2008). Although the model is based on programs of research working with adult patients, the model also is proposed to be applicable for children (Dodd, Janson, et al., 2001). The aims of this theory analysis are twofold: (a) to analyze the SMT using the process described by Walker and Avant (2005) and (b) to evaluate the utility of the SMT for potential use in research with children with cancer and other chronic illnesses.
Process of Theory Analysis
Walker and Avant (2005) describe 7 key steps in theory analysis: (a) identification of the theory’s origins, (b) examination of the theory’s meaning, (c) analysis of the theory’s logical adequacy, (d) determination of the theory’s usefulness, (e) definition of the theory’s generalizability, (f) determination of the theory’s parsimony, and (g) determination of the theory’s testability. Use of this systematic process facilitates a greater understanding of a theory and stimulates further development and refinement of the theory (Walker & Avant, 2005).
Analysis of the Symptom Management Theory
Origins
Model development
The SMT is a middle range model illustrating a multidimensional process of symptom management. It was initially published as the UCSF Symptom Management Model in 1994 as a collaborative effort by members of the Symptom Management Faculty Group at the University of California at San Francisco School of Nursing (UCSF School of Nursing Symptom Management Faculty Group, 1994). This group of nurse scientists represented a broad scope of programs of research in multiple adult illness states, including diabetes, cardiac disease, chronic pulmonary disease, chronic pain, and cancer. The result of their efforts was the development of a deductive, process-focused model addressing 3 interactive components of symptom management: symptom experience, symptom management strategies, and outcomes. The underlying premise of the model was that effective symptom management required consideration of all 3 components.
An updated version of the UCSF Symptom Management Model was published in 2001 (Dodd, Janson, et al., 2001; see Figure 1). This revised model places the process of symptom management within the context of the domains of nursing science: the person, environment, and health and illness. The symptom management dimension was revised to reflect components of symptom management strategies. This change was intended to guide the development of interventions, which then could be replicated. Changes to the outcome dimension included conceptualization of all of the outcomes of symptom management as being interrelated. Another addition to the model was the concept of adherence, which is depicted as extrinsic to the dimensions of symptom management and having the potential to disrupt the relationship between symptom management strategies and the outcomes dimension. The model was further updated in 2008 and was renamed the Symptom Management Theory (SMT; Humphreys et al., 2008).
Figure 1.
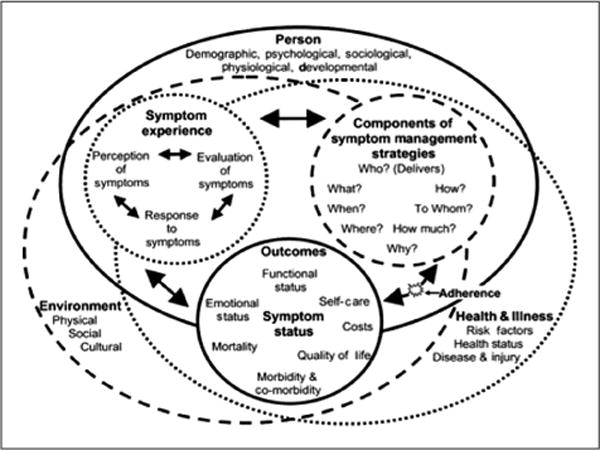
Revised UCSF symptom management model Source: Dodd, Janson, et al. (2001). Reprinted with permission from Wiley-Blackwell.
Assumptions
The SMT includes 6 stated assumptions addressing the nature of symptoms, the focus of symptom management strategies, and relationships within the model. These assumptions, as posed in the 2001 update, are as follows:
That the gold standard for the study of symptoms is based on the perception of the individual experiencing the symptom and his/her self-report.
That the symptom does not have to be experienced by an individual to apply this model of symptom management. The individual may be at risk for the development of the symptom because of the influence (impact) of a context variable such as a work hazard. Intervention strategies may be initiated before an individual experiences the symptom.
That nonverbal patients (infants, poststroke aphasic persons) may experience symptoms and the interpretation by the parent or caregiver is assumed to be accurate for purposes of intervening.
That all troublesome symptoms need to be managed.
That a management strategy may be targeted at the individual, a group, a family, or the work environment.
That symptom management is a dynamic process; that is, it is modified by individual outcomes and the influences of the nursing domains of person, health/illness, or environment (Dodd, Janson, et al., 2001, pp. 669–670).
Meaning
The second component of theory analysis involves identification of definitions of key concepts within the model or theory, as well as relational statements and specified relationships within the model (Walker & Avant, 2005). The authors define a symptom as “a subjective experience reflecting changes in the biophysical functioning, sensations, or cognition of an individual” (Dodd, Janson, et al., 2001, p. 669). Symptom management is recognized as a multidimensional process that requires consideration of each of the 3 components of the model to be considered effective (Dodd, Janson, et al., 2001). The authors also maintain that each of the model’s components requires attention for effective symptom management to occur.
Components of symptom management
The SMT includes 3 components of symptom management: the symptom experience, symptom management strategies, and outcomes. Each component is conceptualized with examples from the authors’ research. Each dimension is depicted as being related to the other 2 dimensions through the use of bidirectional arrows.
The symptom experience component, with its 3 aspects, is the most thoroughly described component of the model and is depicted as the beginning of the symptom management process. This dimension consists of the individual’s perception, evaluation, and response to a symptom. Bidirectional arrows are used to depict the relationships among these components. These relationships are recognized as occurring in a repetitious manner, or even simultaneously (Humphreys et al., 2008).
Application of this dimension of the model in children with cancer may pose unique challenges. The authors note that parents and children may ascribe different meaning to perceived symptoms. Previous studies involving children with cancer indicate that parents may be less perceptive of more subjective symptoms such as nausea and pain (Lo & Hayman, 1999; Miser, Dothage, Wesley, & Miser, 1987). Such incongruency can lead to difficulty in planning interventions. The authors also acknowledge the benefits of technology as contributing to the measurement of symptoms in children (Dodd, Janson, et al., 2001). Such measures add a component of objectivity and can complement more subjective measures offered by children and parents.
The second component of the model comprises the individual aspects of symptom management strategies. These are described as the “what, where, why, how much, to whom, and how,” which guide the clinician or investigator in selecting appropriate intervention strategies (Dodd, Janson, et al., 2001, p. 673) and are intended to “avert, delay, or minimize the symptom experience” (Humphreys et al., 2008, p. 147). The model acknowledges that multiple symptom management strategies may be used and that they may be targeted toward the individual, family, or community group (Dodd, Janson, et al., 2001; Humphreys et al., 2008). Such an application of symptom management strategies supports the theory’s use in research involving children with cancer by acknowledging the role of family members in the child’s care through the illness experience. This potential application of the model, however, has not been tested in study populations that include children with cancer or with other illness states.
Adherence is defined as “whether the intended recipient of the strategy actually receives or uses the strategy prescribed” and is depicted as influencing the relationship between symptom management strategies and outcomes (Dodd, Janson, et al., 2001, p. 674). Nonadherence is conceptualized as occurring in the context of interventions that are too demanding, nonapplication of interventions, or inconsistent application of interventions (Humphreys et al., 2008). The authors also pose that factors within the 3 dimensions of nursing science also may influence adherence (Humphreys et al., 2008).
Of the 3 components of the SMT, the outcomes component is the least clearly developed. In addition to the status of the symptom, this component includes 7 other outcomes that the individual may experience as the result of the symptom experience and/or symptom management strategies. These include functional status, emotional status, self-care, costs, quality of life, morbidity and comorbidity, and mortality (Dodd, Janson, et al., 2001). No relationships are specified within this dimension; however, the authors posit that each of the identified outcomes may be related to the symptom status and to each other (Dodd, Janson, et al., 2001).
Dimensions of nursing science
The dimensions of nursing science were added in the 2001 update to depict the context in which the symptom management process occurs. These include the person, health and illness, and environment dimensions, all of which are described as influencing each of the dimensions of symptom management (Dodd, Janson, et al., 2001). The person dimension encompasses variables “intrinsic to the way an individual views and responds to the symptom experience” (Dodd, Janson, et al., p. 670). These include demographic, psychological, sociological, physiological, and developmental variables. Recognition of the significance of development on the symptom experience and the overall symptom management process is essential for research involving children whose physiologic responses to symptoms and perception of symptoms along with their related distress varies based on normal developmental differences.
The health and illness dimension includes those variables “unique to the health or illness state of an individual” (Dodd, Janson, et al., 2001, p. 670). These are identified as risk factors, health status, and disease and injury. Previous studies by the authors of the SMT have demonstrated both direct and indirect relationships between variables in the health and illness domain and the model’s 3 dimensions.
The third dimension, the environment, encompasses physical, cultural, and social variables representing the “aggregate of conditions” in which a symptom is occurring (Dodd, Janson, et al., 2001). Physical variables may include the individual’s home, work, or the hospital setting. Social variables could include an individual’s interpersonal relationships or sources of social support. Cultural variables represent values, practices, and beliefs that arise from the individual’s racial, ethnic, or religious group (Dodd, Janson, et al., 2001).
Relationships within the model
The bidirectional arrows illustrated in the model’s diagram depict associational relationships among the 3 components of symptom management. Associational relationships also are depicted among the 3 aspects of the symptom experience. Each of the overlapping dimensions of nursing science is depicted as influencing the components of symptom management. Predicted relationships are described only for the health and illness dimension, which is identified as having both direct and indirect effects on symptom management. The authors also describe alternate relationships among variables, such as the influence of gender on cardiovascular outcomes in which morbidity and mortality are worse for women than for men, and the impact of developmental stage on interventions in which premature infants are at increased risk for inadequate analgesia based on health care providers’ misinterpretation of behavioral cues (Dodd, Janson, et al., 2001).
The diagram of the SMT also depicts relationships among model components, which are not clearly explained. The dimensions of nursing science are illustrated as overlapping ellipses in the model diagram; however, relationships among variables in these dimensions are not specified. The diagram also illustrates each dimension as connected to one of the components of symptom management, for example, the health and illness dimension is drawn as being connected to the symptom experience component. The rationale for illustrating the theory in this manner is not specified, nor is any proposed relationships between the interconnected model components.
Boundaries of the theory
The SMT is a middle range theory. As such, it is limited to the phenomenon of symptom management, yet it is sufficiently broad in its application to encompass a wide scope of illness states and developmental groups, including children with cancer. Smith and Liehr (2008) describe a middle range theory as a “basic, usable structure of ideas” (p. 19) and one that is less concretely defined than empirical generalizations and less abstract than grand theories. The SMT is based on the empirical work of its authors and represents their collaborative efforts to develop a framework to guide research and clinical practice.
Logical Adequacy
Evaluation of the logical adequacy of a theory attends to the ability to make predictions independent of the theory’s content, the extent to which scientists agree on predictions that can be made from the theory, whether or not the theory makes sense, and any logical fallacies that may be present.
Predictions independent of content
Because the SMT is an interactive, iterative model, directional relationships among its components are more difficult to predict. Bidirectional arrows illustrate proposed relationships and guide the ability to predict relationships among the theory’s components. Because the direction of these relationships is not specified within the diagram, they could be either positive or negative. Likewise, associations are predicted between each dimension of nursing science and the components of symptom management. The theory’s diagram suggests that interactive relationships are predicted among variables in the 3 dimensions of nursing science; however, the nature of these relationships is not described by the authors (Humphreys et al., 2008). Adherence is depicted as predicting the relationship between symptom management strategies and outcomes.
Agreement of scientists
Review of publications describing application of the SMT, as well as the location of study variables within aspects of the model, suggests agreement among researchers regarding predictions that can be made from the model in both pediatric and adult studies. Intervention strategies were predicted to influence symptom outcomes in children with cancer (Van Cleve et al., 2004) as well as adults with schizophrenia (Kanungpairn, Sitthimongkol, Wattanapailin, & Klainin, 2007). Relationships between the variables in the symptom experience and symptom outcome dimensions have been proposed among adults with several health conditions, including cancer (Dodd, Miaskowski, & Paul, 2001), HIV (Voss, 2005), and traumatic brain injury (Bay & Bergman, 2006).
Although investigators have posed similar hypotheses among the components of the SMT, the selection of variables for inclusion within the components of the model and choices of measures has varied depending on the study sample and the symptom(s) of interest. Selection of measures for studies involving children with cancer also has reflected the developmental characteristics of this population. Gedaly-Duff, Lee, Nail, Nicholson, and Johnson (2006) used wrist actigraphy, which provides an objective measure of sleep, along with daily symptom diaries to capture the symptom experience of children with leukemia and their families. Van Cleve et al. (2004) used age-appropriate pain measures for children and adolescents ranging in age from 4 to 17 years to measure the pain experience across the continuum of treatment for childhood leukemia. These tools, including the Poker Chip Tool, Preschool Body Outline, Adolescent Pediatric Pain Tool, Dot Matrix, and Pediatric Pain Coping Inventory, allowed participants to self-report their pain experiences. Self-report scales also have been used in adult studies guided by the SMT (Bay & Bergman, 2006; Dodd, Miaskowski, et al., 2001; Kanungpairn et al., 2007; Kris & Dodd, 2004; Voss, 2005).
Selection of variables for inclusion in the dimensions of nursing science has varied somewhat based on the population of interest. The SMT authors’ description of the environment dimension emphasizes physical, cultural, and social variables. Gedaly-Duff et al. (2006) located the parents within the environment dimension of children undergoing treatment for leukemia, which could be argued as consistent with the social aspect of this domain. Voss (2005) included income and health insurance as environment variables. The rationale for the placement of these 2 variables in the environment domain was not stated.
Making sense
Use of the SMT as a guiding framework for research across illness states and developmental stages, including childhood cancer, provides support for its logical sense. That the model itself is a collaborative effort derived from research and practice further contributes to its ability to make sense across practice settings.
Logical fallacies
Despite its strengths in agreement and making sense, several logical fallacies are present within the SMT. One of these issues relates to the aspect of time across the illness trajectory (Henly, Kallas, Klatt, & Swenson, 2003; Van Cleve, Bossert, & Savedra, 2002). For an illness such as childhood cancer with a varying symptom trajectory across the treatment continuum, this is particularly significant.
In the SMT, time is reflected in the symptom management strategies as a component of “when” an intervention is delivered; however, changes in the symptom experience and process of symptom management across the duration of an illness are not specified (Dodd et al., 2001; Henly et al., 2003). To address this limitation, Van Cleve et al. (2002) adapted the model to express the 3 dimensions of the model as occurring along a spiral across the first year of treatment for leukemia.
Another potential logical fallacy within the theory is the assumption that the interpretation of symptoms by the parent or caregiver of nonverbal patients (including children) is adequate for initiating intervention. Previous studies involving symptoms in children with cancer suggest that more subjective symptoms are less recognized by parents and that children with greater levels of pain are at increased risk for having their pain underrecognized by health care providers (Lo & Hayman, 1999; Miser, Dothage, Wesley, & Miser, 1987). Although parental report of a symptom may be regarded as adequate for initiating intervention, report of the absence of a symptom may not indicate the absence of a need for intervention.
The authors acknowledge that the SMT is limited in its ability to capture the experience of multiple symptoms occurring simultaneously, an issue that is particularly concerning for children with cancer (Collins et al., 2000; Collins et al., 2002; Dodd, Janson, et al., 2001). The authors presently propose that a symptom cluster may be addressed as an entity within the theory (Dodd, Miaskowski, et al., 2001; Humphreys et al., 2008). A limitation of such an approach is that the model does not guide the researcher or clinician to identify which symptom should be addressed initially. Such an approach also does not address symptoms, which are not a component of the identified cluster. The SMT also does not explain interactions among multiple symptoms.
The SMT does not distinguish between acute and chronic symptoms, both of which may be occurring in the child with cancer (Dodd, Janson, et al., 2001). The model also does not clarify where to locate other related symptoms within the model when a given symptom is the focus of attention and intervention. One plausible approach may be to locate chronic symptoms within the health and illness domain that exerts an influence on the process of managing an acute symptom. As the SMT undergoes further testing and development, attention to multiple symptoms and the nature of these symptoms is warranted.
Usefulness
As a middle range theory addressing the phenomenon of symptom management, the SMT is proposed to be relevant across populations experiencing illness-related symptoms and even those identified as being at risk for symptoms (Dodd, Janson, et al., 2001). The SMT is emerging as a useful framework for research involving children with cancer and their families (Gedaly-Duff et al., 2006; Van Cleve et al., 2004). Continued use of the SMT in research involving children with cancer and their families will provide additional information to support its usefulness in this population.
To date, the model has been established as a useful framework for research among adults with a variety of health and illness states (Bay & Bergman, 2006; Humphreys et al., 2008; Kanungpairn et al., 2007; Kris & Dodd, 2004; Voss, 2005). Studies that were guided by the SMT involving adults have included descriptive studies that sought to identify relationships among variables within the model’s components as well as those exploring symptom management strategies. The model has been used to explore differences in symptoms based on race and ethnicity (Humphreys et al., 2008). It also has been used as a framework for synthesizing current research related to family caregiver symptoms (Fletcher, Dodd, Schumacher, & Miaskowski, 2008). Knowledge gained from these studies adds to further understanding of different aspects of the symptom management process, which then can lead to the development of testable interventions.
Generalizability
A theory’s generalizability relates to the focus of its content and the extent of its boundaries. By its definition, the content of the SMT is limited to the process of symptom management and the context in which it is occurring. As presented in its assumptions, however, the SMT is applicable across multiple settings. It is regarded to be applicable in both symptomatic and presymptomatic states as well as across developmental stages. The model also supports the development of individual- or group-based intervention strategies.
Parsimony
In its simplest sense, the SMT can be reduced to 3 components of symptom management and 3 dimensions of nursing science, giving it a semblance of parsimony. The number of variables for consideration within each of the dimensions of nursing science and the intricate interrelationships within each component of symptom management, however, significantly increases the complexity of the model. As a process-oriented theory, multiple relationships are encompassed within its scope, with some of these occurring simultaneously. This level of complexity can be regarded as both a strength and a limitation. Each of the SMT’s components and proposed relationships are well described, which supports the researcher or clinician in locating variables of interest in the model for potential research or clinical application. These definitions also serve to protect the integrity of the model as the authors intended. Conversely, the number of relationships and variables within the model require careful review of the model’s definitions to ensure correct application of the model. The scope of processes contained within the model also make full application challenging.
Testability
Support for the testability of the SMT is its foundation in the empirical work of its authors (Humphreys et al., 2008). Each of the components of the model is conceptualized to support selection of variables and relationships to be tested empirically. Since its publication, the model has demonstrated the ability to generate research questions and hypotheses across a range of illness states. These attributes add to the overall validity and strength of the model.
The scope and complexity of the SMT limit the number of proposed relationships that can be investigated within a single study. Although studies have addressed different proposed relationships within the SMT, no studies have tested the theory in its entirety. For example, Gedaly-Duff et al. (2006) used the SMT as a framework for investigating pain, sleep disturbance, and fatigue in school-age children with cancer and their parents but did not address relationships between the dimensions of nursing science and these symptoms. Dodd, Miaskowski, et al. (2001) investigated the impact of the experience of a symptom cluster (pain, fatigue, and disturbed sleep) on the outcome of functional status in adults but did not include symptom management strategies. Age was included in the regression analyses, yet analyses did not address relationships between the dimensions of nursing science and the symptom experience or outcome.
Empirical Support for the SMT
As a deductive model, the SMT is derived from the empirical work of its authors (Humphreys et al., 2008). Because individual studies have investigated only selected components of the theory, comparison of empirical support across studies is more challenging. Investigators’ selection of variables for inclusion in each of the theory’s components, in particular, variables included in the dimensions of nursing science, also has not been consistent across studies. This also limits comparisons of findings across studies even though investigators may have proposed similar relationships among model components.
Relationships Between Components of Symptom Management
Empiric support for relationships between theory components has been evident in studies involving adults (Humphreys et al., 2008). Because application of the SMT has been less widely used in research involving children, evidence to support relationships among theory components in this population is limited. Continued use of the SMT in studies involving children with cancer will provide additional empiric support for its use in this population.
Research involving children with cancer has provided varying evidence in support of the proposed relationships among the model’s components. Among children with acute lymphoblastic leukemia, perceived effective pain management was associated with decreased pain intensity across the treatment continuum for older children (8–17 years; Van Cleve et al., 2004). This pattern was not observed in younger children (4–7 years), suggesting that further investigation of developmental differences in reporting pain perception and identification of effective pain management may be warranted.
Studies involving adults have provided support for the SMT’s proposed relationships between the symptom experience and outcomes. For example, Dodd, Miaskowski, et al. (2001) found that initial functional status, pain, and fatigue were predictive of change in functional status in adults undergoing outpatient chemotherapy.
Relationships Between Nursing Science and Symptom Management
Although the dimensions of nursing science were added in 2001, limited application of the full scope of their potential influence has been described in subsequent studies, in particular, those involving children with cancer. Studies involving adults do provide initial empiric support for these proposed relationships. As an example, relationships between symptoms in adults with HIV infection and variables in each of the 3 dimensions of nursing science are present (Voss, 2005). Further exploration of the influence of the dimensions of nursing science, including identification of potential variables for inclusion in these dimensions is warranted in research involving children with cancer.
Considerations for Research Involving Children With Cancer
Although the SMT is based largely in research and practice involving adults, it has been developed with the intent of being applied in pediatric populations. The influence of development is acknowledged in the person dimension of nursing science, and the symptom management strategies component acknowledges that the child’s parent may intervene on behalf of the child. As the SMT is applied in research involving children with cancer, continued attention to measurement of symptoms in children, consideration of the parents and family, and testing across pediatric populations is warranted.
Report and Measurement of Symptoms
The SMT assumes that self-report is the standard for identifying the existence of symptoms and that parental report of symptoms is accurate for the purpose of intervening (Dodd, Janson, et al., 2001). Although a parent or caregiver’s report of the existence of a child’s symptom may be regarded as sufficient to initiate an intervention, reliance on proxy reporting may result in underrecognition and inadequate management of more subjective symptoms (Linder, 2008). Younger children tend to be more present oriented and may emphasize physical rather than mental aspects of symptoms (Hockenberry-Eaton et al., 1998). These children also tend to have more difficulty responding to multiple individual items and may benefit from being asked to describe overall feeling states (Woodgate, Degner, & Yanofsky, 2003). This understanding of children’s perception of symptoms calls for the development of reliable and valid instruments for the assessment of symptoms in children, including the use of less traditional methodological approaches to capture the child’s perspective. Use of technologic devices, such as wrist actigraphy in the assessment of disturbed sleep, also may support objective measurement of symptoms in young children (Gedaly-Duff et al., 2006; Hinds et al., 2007).
Inclusion of Parents and Family Members
Central to research and practice involving children is consideration of the parents and the influence of the child’s illness on the family. Although the model recognizes that parents may be involved in symptom management strategies for the child, the location of the parents and family members within the theory is unclear. The environment dimension includes the social variables, represented as the individual’s support network and interpersonal relationships, suggesting that parents and family members could be located in this component (Humphreys et al., 2008). Gedaly-Duff et al. (2006) placed parents of children with cancer in the environment dimension; however, their published analyses did not address this relationship.
The current focus of the outcomes dimension is the individual. The SMT does not specifically address the impact of the symptom and its management on other family members, which can be particularly significant in children with cancer, as an aspect of the outcomes component (Woodgate, 2006). Such considerations raise questions as to how best to include child and family outcomes as part of the symptom management process.
Application Across Pediatric Populations
Application of the SMT is needed in research involving children experiencing both acute and chronic symptoms. To date, its use has been limited to children with cancer; however, these studies have been largely descriptive and have provided only limited testing of the model’s proposed relationships (Gedaly-Duff et al., 2006; Van Cleve et al., 2004). Studies across other pediatric populations will increase understanding of the SMT’s generalizability, usefulness, and testability in children. They will contribute to comparison of similarities and differences in the symptom trajectories for children with cancer and children with other chronic illness states. Such studies also will contribute to further refinement of the SMT for application in pediatric research and clarification of its logical adequacy in the pediatric population.
Implications for Practice
Because of its foundation in research and clinical practice, the SMT has the potential to influence pediatric oncology nursing practice as well as research. The model provides a conceptual framework for understanding relationships between factors influencing the symptom experience as well as the larger contextual factors influencing symptom management. It can guide nursing interventions aimed at influencing the context in which symptoms are occurring and the development of symptom management strategies. The SMT also has the potential to influence institution-based practices relating to symptom management and to create care environments conducive to minimizing symptoms.
Summary
The SMT is a process-focused, noncategorical middle range theory that has been applied across a variety of illness states in adults and has demonstrated initial applicability in research involving children with cancer (Gedaly-Duff et al., 2006; Van Cleve et al., 2004). Strengths of the theory include its attention to the context in which symptoms are occurring and its ability to inform research hypotheses and clinical practice. Limitations of the SMT are its lack of parsimony, limiting the extent to which the model can be tested, and its inability to capture the changing nature of symptoms across the illness trajectory.
Although the SMT is conceptualized as being applicable in research with children, additional testing is necessary to validate its proposed relationships in pediatric populations. Additional refinement is necessary to investigate and clarify the role of proxy reporting of children’s symptoms by parents or other caregivers, including health care professionals. Clarification of the location of parents and family within the model’s components is warranted as well. As these areas are explored and addressed across pediatric populations, the SMT has the potential to guide nursing research and practice to improve symptoms and overall quality of life for children with cancer.
Acknowledgments
The author wishes to acknowledge Becky J. Christian, PhD, RN, for her support in the development and review of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research and/or authorship of this article:
Individual National Research Service Award, National Institute for Nursing Research (F31NR010175-01); Doctoral Scholarship in Cancer Nursing, American Cancer Society (DSCN-06-204-1); and Dissertation Grant Scholarship, Western Institute of Nursing and the Council for the Advancement of Nursing Science.
Biography
Lauri Linder holds a joint appointment as an Assistant Professor with the University of Utah College of Nursing where she teaches in the undergraduate and graduate nursing programs and as a clinical nurse specialist with the Hematology/Oncology/Transplant Service Line at Primary Children’s Medical Center.
Footnotes
Declaration of Conflicting Interests
The author(s) declared no conflicts of interest with respect to the authorship and/or publication of this article.
References
- Bay E, Bergman K. Symptom experience and emotional distress after traumatic brain injury. Care Management Journals. 2006;7:3–9. doi: 10.1891/cmaj.7.1.3. [DOI] [PubMed] [Google Scholar]
- Berger AM, Cochrane B, Mitchell SA. The 2009–2013 research agenda for oncology nursing. Oncology Nursing Forum. 2009;36:E274–E282. doi: 10.1188/09.ONF.E274-E282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chinn PL, Kramer MK. Integrated knowledge development in nursing. 6th. St. Louis, MO: Mosby; 2004. [Google Scholar]
- Collins JJ, Byrnes ME, Dunkel IJ, Lapin J, Nadel T, Thaler HT, Portenoy RK. The measurement of symptoms in children with cancer. Journal of Pain and Symptom Management. 2000;19:363–377. doi: 10.1016/s0885-3924(00)00127-5. [DOI] [PubMed] [Google Scholar]
- Collins JJ, Devine TD, Dick GS, Johnson EA, Kilham HA, Pinkerton CR, Portenoy RK. The measurement of symptoms in young children with cancer: The validation of the Memorial Symptom Assessment Scale in children aged 7–12. Journal of Pain and Symptom Management. 2002;23:10–16. doi: 10.1016/s0885-3924(01)00375-x. [DOI] [PubMed] [Google Scholar]
- Dodd M, Janson S, Facione N, Faucett N, Froelicher ES, Humphreys J, Taylor D. Advancing the science of symptom management. Journal of Advanced Nursing. 2001;33:668–676. doi: 10.1046/j.1365-2648.2001.01697.x. [DOI] [PubMed] [Google Scholar]
- Dodd MJ, Miaskowski C, Paul SM. Symptom clusters and their effect on the functional status of patients with cancer. Oncology Nursing Forum. 2001;28:465–470. [PubMed] [Google Scholar]
- Fletcher BAS, Dodd MJ, Schumacher KL, Miaskowski C. Symptom experiences of family caregivers with cancer. Oncology Nursing Forum. 2008;35:E23–E44. doi: 10.1188/08.ONF.E23-E44. [DOI] [PubMed] [Google Scholar]
- Gedaly-Duff V, Lee KA, Nail LM, Nicholson S, Johnson KP. Pain, sleep disturbance, and fatigue in children with leukemia and their parents: A pilot study. Oncology Nursing Forum. 2006;33:641–646. doi: 10.1188/06.ONF.641-646. [DOI] [PubMed] [Google Scholar]
- Henly SJ, Kallas KD, Klatt CM, Swenson KK. The notion of time in symptom experiences. Nursing Research. 2003;52:410–417. doi: 10.1097/00006199-200311000-00009. [DOI] [PubMed] [Google Scholar]
- Hinds PS, Hockenberry MJ, Rai SN, Zhang L, Bassem I, Razzouk BI, Rodriguez-Galindo C. Nocturnal awakenings, sleep environment interruptions, and fatigue in hospitalized children with cancer. Oncology Nursing Forum. 2007;34:393–402. doi: 10.1188/07.ONF.393-402. [DOI] [PubMed] [Google Scholar]
- Hockenberry M. Symptom management research in children with cancer. Journal of Pediatric Oncology Nursing. 2004;21:132–136. doi: 10.1177/1043454204264387. [DOI] [PubMed] [Google Scholar]
- Hockenberry-Eaton M, Hinds PS, Alcoser P, O’Neill JB, Euell K, Howard V, Taylor S. Fatigue in children and adolescents with cancer. Journal of Pediatric Oncology Nursing. 1998;15:172–182. doi: 10.1177/104345429801500306. [DOI] [PubMed] [Google Scholar]
- Humphreys J, Lee KA, Carrieri-Kohlman V, Puntillo K, Faucett J, Janson S, Donesky-Cuenco D. Theory of symptom management. In: Smith MJ, Liehr PR, editors. Middle range theory for nursing. 2nd. New York, NY: Springer; 2008. pp. 145–158. [Google Scholar]
- Kanungpairn T, Sitthimongkol Y, Wattanapailin A, Klainin P. Effects of a symptom management program on auditory hallucinations in Thai outpatients with a diagnosis of schizophrenia: A pilot study. Nursing and Health Sciences. 2007;9:34–39. doi: 10.1111/j.1442-2018.2007.00302.x. [DOI] [PubMed] [Google Scholar]
- Kris AE, Dodd MJ. Symptom experience of adult hospitalized medical-surgical patients. Journal of Pain and Symptom Management. 2004;28:451–459. doi: 10.1016/j.jpainsymman.2004.01.015. [DOI] [PubMed] [Google Scholar]
- Linder LA. Developmental diversity in symptom management for children with cancer. Journal of Pediatric Nursing. 2008;23:296–309. doi: 10.1016/j.pedn.2007.10.003. [DOI] [PubMed] [Google Scholar]
- Lo LH, Hayman LL. Parents associated with children in measuring acute and delayed nausea and vomiting. Nursing and Health Sciences. 1999;1:155–161. doi: 10.1046/j.1442-2018.1999.00020.x. [DOI] [PubMed] [Google Scholar]
- Miser AW, Dothage JA, Wesley M, Miser JS. The prevalence of pain in a pediatric and young adult cancer population. Pain. 1987;29:73–83. doi: 10.1016/0304-3959(87)90180-1. [DOI] [PubMed] [Google Scholar]
- Smith MJ, Liehr PR. Understanding middle range theory by moving up and down the ladder of abstraction. In: Smith MJ, Liehr PR, editors. Middle range theory for nursing. New York, NY: Springer; 2008. pp. 13–31. [Google Scholar]
- UCSF School of Nursing Symptom Management Faculty Group. A model for symptom management. Image: Journal of Nursing Scholarship. 1994;26:272–276. [PubMed] [Google Scholar]
- Van Cleve L, Bossert E, Beecroft P, Adlard K, Alvarez O, Savedra MC. The pain experience of children with leukemia during the first year after diagnosis. Nursing Research. 2004;53:1–10. doi: 10.1097/00006199-200401000-00001. [DOI] [PubMed] [Google Scholar]
- Van Cleve L, Bossert E, Savedra MC. Cancer pain in children: The selection of a model to guide research. Journal of the Society of Pediatric Nurses. 2002;7:163–165. doi: 10.1111/j.1744-6155.2002.tb00172.x. [DOI] [PubMed] [Google Scholar]
- Voss JG. Predictors and correlates of fatigue in HIV/AIDS. Journal of Pain and Symptom Management. 2005;29:173–184. doi: 10.1016/j.jpainsymman.2004.05.006. [DOI] [PubMed] [Google Scholar]
- Walker LO, Avant KC. Strategies for theory construction in nursing. 4th. Upper Saddle River, NJ: Pearson Education; 2005. [Google Scholar]
- Woodgate RL. Siblings’ experiences with childhood cancer: A different way of being in the family. Cancer Nursing. 2006;29:406–414. doi: 10.1097/00002820-200609000-00010. [DOI] [PubMed] [Google Scholar]
- Woodgate RL, Degner LF, Yanofsky R. A different perspective to approaching cancer symptoms in children. Journal of Pain and Symptom Management. 2003;26:800–817. doi: 10.1016/s0885-3924(03)00285-9. [DOI] [PubMed] [Google Scholar]


