Abstract
Based on the data from the Behavioral Risk Factor Surveillance System 2012, this study examines the association of neighborhood built environments with individual physical inactivity and obesity in the U.S. Multilevel modeling is used to control for the effects of individual socio-demographic characteristics. Neighborhood variables include built environment, poverty level and urbanicity at the county level. Among the built environment variables, a poorer street connectivity and a more prominent presence of fast-food restaurants are associated with a higher obesity risk (especially for areas of certain urbanicity levels). Analysis of data subsets divided by areas of different urbanicity levels and by gender reveals the variability of effects of independent variables, more so for the neighborhood variables than individual variables. This implies that some obesity risk factors are geographically specific and vary between men and women. The results lend support to the role of built environment in influencing people’s health behavior and outcome, and promote public policies that need to be geographically adaptable and sensitive to the diversity of demographic groups.
Keywords: built environment, walk score, food environment, urbanicity, obesity
1. Introduction
Obesity is a major risk factor for heart disease, diabetes, stroke, depression, sleep apnea, osteoarthritis, and some cancers (Ahima and Lazar 2013). Regular leisure time physical activity can help control weight and improve health. However, less than half (48.4%) of adults of 18 years of age and over met the Physical Activity Guidelines for aerobic physical activity in 2011 (National Center for Health Statistics 2013), and more than one-third (34.9%) adults were obese in 2011–2012 (Ogden et al. 2013). Medical costs for obese people are substantially higher than those of normal weight (Finkelstein et al. 2009). In the U.S., obesity prevalence rates vary a great deal across states, ranging from 21.3% in Colorado to 35.1% in Mississippi and West Virginia in 2013 (CDC 2015), and even more among smaller geographic areas such as counties.
The cause of obesity arises from a positive energy balance over time. Energy intake is basically from food and drink, and energy consumption is related to individual’s physical activity. An individual with a high level of consumption of fast foods and sugar-sweetened beverages (Pereira et al. 2005, Schulze et al. 2004) and a low level of physical activity (Koh-Banerjee et al. 2003) has a high risk of obesity. The obesogenic environment thesis suggests that disparities of obesity prevalence are partially attributable to differentiated exposure to a healthy food environment that promotes healthier dietary choices and built environments that encourage physical activities (Swinburn, Egger and Raza 1999; Powell, Spears and Rebori 2010). Built environment refers to human-made resources and infrastructure designed to support human activity, such as buildings, roads, parks, restaurants, grocery stores and other amenities, as compared with natural environment (Pierce, Ernest and Ashworth 2012).
There is a large body of literature examining the relationship between built environment (including factors such as access to healthy food, distance to nearby amenities, walkable urban form and neighborhood safety) and obesity (Feng et al. 2010, Papas et al. 2007, O Ferdinand et al. 2012, Durand et al. 2011). However, due to challenges of data requirements and computational complexity for measuring obesogenic built environments, few studies have examined obesity in the U.S. at a national scale until recently. Among the recent national studies, Wen and Kowaleski-Jones (2012) and Wen et al. (2013) considered two major built environment factors such as distance to the nearest parks and street connectivity, and Wang et al. (2013) focused on the role of population-adjusted street connectivity. This nationwide analysis considers two built environment factors that have not been included in previous studies of such a scale, namely walk score and the ratio of fast-food to full-service restaurants.
Furthermore, recent literature suggests that the linkage between built environment and physical activity (and thus obesity) varies in different geographic settings such as urban versus rural areas (Monnat and Pickett 2011, Ding and Gebel 2012, Ewing et al. 2014). Urban neighborhoods have more sidewalks, mixed land uses, better street connectivity and more playgrounds than rural areas (Lopez and Hyness 2006). Within urban area, children in inner city neighborhoods are engaged in less physical activity than those in suburban areas (Weir, Etelson and Brand 2006). More anxiety about neighborhood safety may deter physical activity and help explain a higher obesity rate in inner city areas (Felton et al. 2002, Wilson et al. 2004). A recent study shows that better street connectivity reduces obesity risk only in suburbia of large metropolitan areas, not urban areas or smaller metropolitan or rural areas (Wang et al. 2013). Some recent studies emphasize the spatial heterogeneity in the association of community environment and obesity risk (Chalkias et al. 2013; Chi et al. 2013; Slack et al. 2014). This research examines the association between built environment and obesity with an emphasis on the likely variability across different levels of urbanicity.
On the methodological front, multilevel models are common in public health research. Individual behaviors such as eating habit and physical activity are influenced by socio-environmental factors including built environment (Huang et al. 2009). This study uses the multilevel modeling approach to analyze the influence of built environment on adult physical inactivity and obesity in the U.S. while controlling for individual attributes (e.g., race, age, gender, marital status, education attainment, employment status, income, and whether an individual smokes). The focus of our work is on possible different impacts of built environment factors in areas at various urbanicity levels and between males and females.
2. Data Sources and Variable Definitions
Individual Variables from BRFSS
The Behavioral Risk Factor Surveillance System (BRFSS) is an annual health-related telephone survey system for tracking risk behaviors, health conditions, and use of preventive services in the U.S. since 1984. Since 2011, the survey data added cell-phone-only respondents to landline respondents that were covered by the survey data for 1984–2010. We used the 2012 BRFSS data set (http://www.cdc.gov/brfss/annual_data/annual_2012.html), the most recent one available at the time this research was conducted. The data set contains a large volume of individual data geocoded to county. After eliminating the records with missing values for variables used in this study, the study area includes 328, 156 observations from the BRFSS in the 48 conterminous states and Washington D.C.1
The BRFSS data contains two dependent variables used in this research: physical inactivity and obesity. Physical inactivity refers to no leisure-time physical activity or exercise in the last month as reported. Individuals with BMI ≥ 30 were considered obese. They are coded as binary, i.e., 1 for no physical activity and 0 otherwise, 1 for being obese and 0 otherwise.
Individual independent variables are also from the BRFSS data set (Table 1). In addition to age (18+), “age squared” is added to check the curvilinear impact of age in the multilevel models. Race-ethnicity is categorical including non-Hispanic Black, Hispanic, and others with non-Hispanic White as the reference category. Binary variables include sex (female as the reference category), employment status (not employed as the reference category), marital status (currently not married as the reference category), and smoker (non-smoker as the reference category). Education and income are ordinal such as: education level = 1–4, income level = 1–5 (Table 1). For simplicity, both education and income are coded numerical in the multilevel models; and the results are consistent with those from models coding them as categorical dummy variables.
Table 1.
BRFSS Individual Variables and Distributions
| Demographic Variables | Sample Size | Physical inactivity rate (PIR, %) | Obesity rate (OBR, %) | |
|---|---|---|---|---|
| All |
328,156
|
23.49
|
29.25
|
|
| Race- ethnicity | Non-Hispanic Whites* | 262,745 | 22.29 | 27.69 |
| Non-Hispanic Blacks | 29,697 | 30.82 | 42.67 | |
| Hispanics | 20,154 | 27.80 | 31.79 | |
| Others | 15,560 | 24.22 | 26.68 | |
|
|
|
|
|
|
| Age | 18–29 | 27,817 | 13.78 | 20.41 |
| 30–41 | 47,614 | 16.87 | 29.82 | |
| 42–53 | 69,925 | 21.08 | 31.96 | |
| 54–65 | 90,479 | 24.47 | 33.25 | |
| 65+ | 92,321 | 30.70 | 25.65 | |
|
|
|
|
|
|
| Gender | Men | 139,697 | 21.07 | 29.26 |
| Women* | 188,459 | 25.29 | 29.24 | |
|
|
|
|
|
|
| Married | Yes | 175,530 | 19.73 | 28.58 |
| No* | 152,626 | 27.82 | 30.02 | |
|
|
|
|
|
|
| Education | Did not graduate high school (1) | 25,139 | 44.17 | 36.28 |
| Graduated high school (2) | 92,497 | 32.23 | 32.81 | |
| Attend college or technical school (3) | 89,963 | 22.82 | 31.60 | |
| Graduate from college or technical school (4) | 120,557 | 12.98 | 23.29 | |
|
|
|
|
|
|
| Employed | Yes | 144,165 | 17.65 | 29.42 |
| No* | 183,991 | 28.07 | 29.11 | |
|
|
|
|
|
|
| Income | Less than $15,000 (1) | 38,300 | 40.22 | 35.89 |
| $15,000 to less than$25,000 (2) | 58,007 | 34.72 | 33.01 | |
| $25,000 to less than $35,000 (3) | 37,480 | 28.30 | 30.33 | |
| $35,000 to less than$50,000 (4) | 48,081 | 22.63 | 29.95 | |
| $50,000 or more (5) | 146,288 | 13.71 | 25.52 | |
|
|
|
|
|
|
| Smoker | Yes | 55,530 | 33.46 | 26.29 |
| No* | 272,626 | 21.46 | 29.85 | |
Note:
indicates the reference category in the group.
Rates of Physical Inactivity and Obesity for Various Socio-Demographic Groups
Table 1 summarizes the sample distributions across the individual socio-demographic variables reported in the 2012 BRFSS. The overall physical inactivity rate is 23.49%, and the overall obesity rate is 29.25%. Among the four major racial-ethnic groups, non-Hispanic Whites account for the vast majority (80%), both physical inactivity rate (PIR) and obesity rate (OBR) for non-Hispanic Blacks or Hispanics are higher than the averages and more so for non-Hispanic Blacks, and the PIR for others is slightly higher than the average but the OBR for others is slightly lower than the average. The PIR increases with age, so does the OBR till the 54–65 age group but drops in the 65+ age group. The latter suggests a curvilinear association of age with obesity. The PIR for women is higher than men, but their OBRs are about the same. Married people have a lower PIR and a lower OBR than their unmarried counterparts. Both the PIR and OBR drop with increasing educational attainment. Employed people have a lower PIR than their unemployed counterparts, but their OBRs are very close. Both the PIR and OBR drop with increasing income, similar to the influence of educational attainment. Smokers have a higher PIR but a lower OBR.
For the most part, the trend for the PIR is consistent with that of OBR. However, they also differ in several cases such as the minor discrepancy in their associations with age, gaps in their associations with marital status and employment status, and the major contrast in the associations with smokers/non-smokers. The above observations do not consider the joint effects of multiple variables let alone the neighborhood effects, and thus are preliminary.
Neighborhood Variables at the County Level from Census and Other Sources
All neighborhood variables are defined at the county level as county is the smallest geographic unit identified in the BRFSS dataset. Guided by the literature, two social-demographic variables are included: poverty rate and race heterogeneity, both derived from the Census 2010 data. Poverty rate is the estimated percent of people of all ages in poverty. Racial-ethnic heterogeneity reflects the racial-ethnic composition defined as 1- Σpi2, where pi is the fraction of the population in a given group (Sampson and Groves 1989). This study includes six racial-ethnic groups (Non-Hispanic Whites, Blacks, Asians/Pacific Islanders, Hispanics, American Indians/Alaska Natives, and others) for calculating the index in a county. The heterogeneity index ranges between 0 and 1. If the value equals to 0, it means that there is only one racial/ethnic group in the unit; while a value approaching 1 reflects a maximum heterogeneity. A lower heterogeneity index (e.g., dominated by a disadvantaged minority group) may be tied to a lower level of social capital suggested by the social disorganization theory (Sampson and Groves 1989) and discourages physical activity (and thus a higher obesity risk) in a community. It may also work in a reverse direction as some minorities (e.g., Blacks and Hispanics) are reported to experience higher obesity rates and thus a neighborhood with above-average representations of these minorities could have a relatively high heterogeneity index. The index is used in several studies of community environment and obesity risk (Wen and Kowaleski-Jones 2012, Wang, Wen and Xu 2013, Xu, Wen and Wang 2015).
The built environment is also measured at the county level, and includes street connectivity, walkability and food environment. Intersection density (i.e., number of intersections per km2) is the most commonly used index to measure street connectivity. Ball et al. (2012) concluded that street connectivity is not significantly associated with either adult BMI or BMI categories. Wang et al. (2013) argued that intersection density varies a great deal within a large geographic area such as county, and the conventional measure of street connectivity can be biased for a county with the majority of population concentrated in limited urban area. Therefore, “population-adjusted street connectivity” is a preferred choice. In implementation, intersection density is calculated at the census tract level and then aggregated to the county level by computing a weighted average value (using population as weight). Walkability is measured by the Walk Score (http://www.walkscore.com/) based on the algorithm developed by the Front Seat Management (http://www.frontseat.org/). It calculates the Euclidean distances from a point of interest to nearby amenities such as food, retail, education, recreation, and entertainment, and then integrates them by a linear combination of these distances with weights that account for facility type priority and a distance decay function (Front Seat 2013). Similarly, walk score is first obtained at the census tract level and then aggregated to the county level by computing the population-weighted averages. Food consumption relying on fast food restaurants is likely to promote more meals or increase consumption of high fat meals, leading to higher caloric intake (Michimi and Wimberly 2010). Some studies used the number of fast-food restaurants per capita to measure food environment (Wang et al. 2007, Jay 2004, Lamichhane et al. 2013). Such an approach does not account for the availability of choices between healthy and unhealthy food by consumers. This research uses the ratio of fast-food to full-service restaurant numbers at the county level to measure food environment. The restaurant data is extracted from the 2012 County Business Patterns (CBP), an annual series providing subnational economic data by industry (http://www.census.gov/econ/cbp/). In the dataset, restaurants are classified into fast food and full service. There are other measures for food environment (Mehta and Chang 2008; Chi et al. 2013; Xu and Wang 2015). As suggested by Xu, Wen and Wang (2015), the fast food restaurant ratio is an adequate measure at the county level. While walk score and food environment are used in many studies for obesity risk, our attempt is the first at a national scale.
For urbanicity, we first use the 2013 NCHS Urban-Rural Classification Scheme for Counties prepared by the National Center for Health Statistics (NCHS), in accordance with the 2010 OMB (Office of Management and Budget) standards for defining metropolitan and micropolitan areas (Ingram and Franco 2014). There are six urban-rural categories such as large central metro, large fringe metro, medium metro, small metro, micropolitan and noncore, where noncore is used as the reference category for coding. In order to capture urbanicity more accurately, this research also uses another definition based on the 2010 Census Urban and Rural Classification (Census, 2014). The Census defines an urban area with minimal criteria of population and population density using much smaller geographic units such as census tracts and census block. For each county, its urbanicity is defined as a continuous urbanization ratio, i.e., urban population in urban areas over the total population in the county (Wang et al. 2013). While the two measures of urbanicity are generally consistent with each other (as verified in the next section), the latter is more accurate than the former for the aforementioned reason.
3. Methods
Analysis of Variability of County-Level Variables by Urbanicity
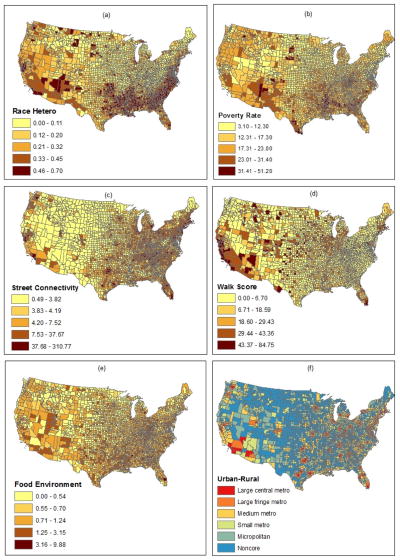
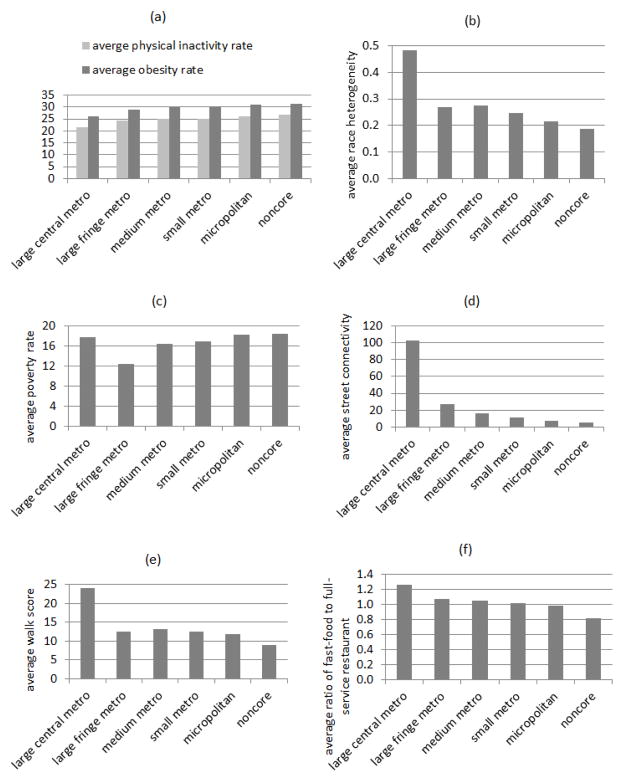
Figure 1a-f show the spatial patterns of the aforementioned county-level variables. Given the emphasis of examining the association of built environment and obesity by urbanicity, it is valuable to examine the variability of each county-level variable across the urbanicity categories (here based on the NCHS classifications as an example). In addition to the two socio-demographic variables and three built environment variables, we also calculate the average physical inactivity and obesity rates in the counties.
Figure 1.
County-level variables: (a) racial-ethnic heterogeneity; (b) poverty rate; (c) street connectivity; (d) walk score; (e) food environment; (f) urbanicity
As the urbanicity decreases from large central metro to noncore counties, (1) both the average physical inactivity rate (PIR) and obesity rate (OBR) increase from the lowest to the highest, as shown in Figure 2a; (2) both the average racial-ethnic heterogeneity index and walk score decrease in general (only slightly higher in medium metro than in large fringe metro), as shown in Figures 2b and 2e; and (3) both the average street connectivity and fast-food to full-service restaurants ratio decrease, as shown in Figures 2d and 2f. For the average poverty rate, the order is noncore > micropolitan > large central metro > small metro > medium metro > large fringe metro, as shown in Figure 2c. In other words, the poverty rate is the highest at the two ends of urbanicity (rural counties such as in noncore or micropolitan and urban core such as in large central metro) and declines toward the middle with the lowest poverty rate in suburbia (fringe) of large metro.
Figure 2.
Averages of county-level variables by urbanicity: (a) physical inactivity rate and obesity rate, b) racial-ethnic heterogeneity, (c) poverty rate, (d) street connectivity, (e) walk score; (f) food environment
Are differences in the average values statistically significant across the urban-rural classifications? This may be answered by conducting the ANOVA (analysis of variance) test. Here a simple regression model is employed for the same purpose for its simplicity and easy interpretation (Wang et al. 2014). The dependent variable is the variable of interest (e.g., “obesity rate (OBR)”), and the independent variables are five dummy variables that code the six urbanicity categories with the noncore counties as the reference type. The results are reported in Table 2. For example, for obesity rate, the average for noncore counties is 31.259, for large central metro counties is 31.259-5.359=25.900, for large fringe metro counties is 31.259-2.261=28.998 and so on. The results reported in Table 2 are consistent with Figures 2a–2f. Moreover, the t-values indicate that the differences between the reference category (noncore counties) and any other types of counties are statistically significant in most cases.
Table 2.
Variability of county-level variables across urban-rural classifications
| Physical inactivity rate | Obesity rate | Racial-ethnic heterogeneity | Poverty rate | Street connectivity | Walk score | Food environment | Urban ratio | |
|---|---|---|---|---|---|---|---|---|
| Large central metro | −5.254*** (−8.55) | −5.359*** (−9.96) | 0.296*** (15.19) | −0.753 (−0.96) | 97.903*** (44.37) | 15.137*** (8.24) | 0.440*** (5.11) | 0.877*** (29.15) |
| Large fringe metro | −2.765*** (−9.49) | −2.261*** (−8.86) | 0.080*** (8.66) | −6.085*** (−16.41) | 22.407*** (21.41) | 3.628*** (4.16) | 0.257*** (6.29) | 0.396*** (28.40) |
| Medium metro | −1.882*** (−6.47) | −1.175** (−4.61) | 0.087*** (9.45) | −2.062*** (−5.57) | 11.312*** (10.83) | 4.262*** (4.90) | 0.235*** (5.76) | 0.366*** (25.61) |
| Small metro | −1.741*** (−5.89) | −0.907*** (−3.51) | 0.057*** (6.14) | −1.487*** (−3.96) | 6.274*** (5.91) | 3.613*** (4.09) | 0.197*** (4.76) | 0.316*** (22.31) |
| Micropolitan | −0.766*** (−3.21) | −0.260 (−1.24) | 0.028*** (3.77) | −0.242 (−0.80) | 2.277** (2.66) | 3.047*** (4.27) | 0.166*** (4.97) | 0.167*** (15.29) |
| Non-core | 26.908*** (197.26) | 31.259 (261.63) | 0.188*** (43.40) | 18.437*** (106.22) | 4.976*** (10.16) | 8.869*** (21.74) | 0.817*** (42.70) | 0.080*** (12.66) |
| R2 | 0.051 | 0.051 | 0.095 | 0.085 | 0.428 | 0.029 | 0.025 | 0.389 |
p≤ 0.001,
p≤ 0.01,
p≤ 0.05
This approach is also used to examine how the two urbanicity measures (six NCHS categories vs. continuous urbanization ratio) are related, and the result is shown in the last column in Table 2. Clearly, the average urbanization ratio increases steadily from 0.080 for non-core counties, to 0.247 (i.e., 0.080+0.157) for micropolitan, and so on, and reaches as high as 0.957 for large central metro. The differences in urbanization ratio across the NCHS classes are all statistically significant, and thus the two measures are generally consistent with each other.
Once again, the above discussion is based on analysis of aggregated data for a single variable at a time and has limited value. The actual effect of county-level variables needs to be examined in a multilevel modeling schema.
Multilevel Modeling
Multilevel modeling (MLM) examines the risk of individual health behavior (i.e., physical inactivity) or outcome (i.e., obesity) by considering both individual and neighborhood-level (county) variables. Specifically, in a multilevel logistic model, the dependent variable is binary (0, 1) such as an individual being physically inactive (= 1, and 0 otherwise) or being obese (=1, and 0 otherwise). Tables 3 and 4 present the results. There are four models for each, labeled “PI” and “OB” for physical inactivity and obesity, respectively. In Table 3, model 1 is the unconditional model with only individual-level predictors, model 2 adds the county-level variables. In Table 4, in order to capture the effect of urbanicity, model 3 adds five dummy variables to code the six NCHS classifications (noncore county as the reference category), and model 4 uses the continuous variable “urban ratio” and its square term. See the previous section on the definitions of reference categories for several categorical individual variables such as race-ethnicity, sex, marital status, employment status, and smoker or nonsmoker.
Table 3.
Odds ratios of multilevel logistic models for physical inactivity (PI) and Obesity (OB)
| Model PI1 | Model PI2 | Model OB1 | Model OB2 | |
|---|---|---|---|---|
| Individual variables | ||||
| Non-Hispanic Black | 1.205*** | 1.196*** | 1.666*** | 1.671*** |
| Hispanic | 1.217*** | 1.219*** | 1.055** | 1.059*** |
| Other race/ethnicity | 1.173*** | 1.171*** | 0.922*** | 0.925*** |
| Age (18+) | 1.037*** | 1.036*** | 1.125*** | 1.124*** |
| Age2 | 0.999*** | 0.999*** | 0.999*** | 0.999*** |
| Male | 0.867*** | 0.868*** | 1.060*** | 1.062*** |
| Married | 1.002 | 0.998 | 0.952*** | 0.947*** |
| Education (1–4) | 0.712*** | 0.714*** | 0.833*** | 0.834*** |
| Employed | 0.843*** | 0.844*** | 0.781*** | 0.782*** |
| Income (1–5) | 0.818*** | 0.820*** | 0.919*** | 0.922*** |
| Smoker | 1.571*** | 1.570*** | 0.612*** | 0.611*** |
| County variables | ||||
| Racial-ethnic Heterog. | 0.985 | 0.885* | ||
| Poverty | 1.008*** | 1.010*** | ||
| Street connectivity | 0.999* | 0.998*** | ||
| Walk Score | 0.998*** | 0.999 | ||
| Fast food ratio | 1.052*** | 1.049*** | ||
| AIC | 334287.3 | 334158.8 | 390893.6 | 390705.0 |
p≤ 0.001,
p≤ 0.01,
p≤ 0.05
Table 4.
Odds ratios of multilevel logistic models with urbanicity for physical inactivity (PI) and Obesity (OB)
| Model PI3 | Model PI4 | Model OB3 | Model OB4 | |
|---|---|---|---|---|
| Individual variables | ||||
| Non-Hispanic Black | 1.194*** | 1.183*** | 1.675*** | 1.681*** |
| Hispanic | 1.222*** | 1.211** | 1.059*** | 1.064*** |
| Other race/ethnicity | 1.170*** | 0.150*** | 0.926*** | 0.930*** |
| Age (18+) | 1.036*** | 1.035*** | 1.124*** | 1.122*** |
| Age2 | 0.999*** | 0.999*** | 0.999*** | 0.999*** |
| Male | 0.868*** | 0.868*** | 1.062*** | 1.061*** |
| Married | 0.997 | 0.997 | 0.947*** | 0.945*** |
| Education (1–4) | 0.714*** | 0.715*** | 0.834*** | 0.836*** |
| Employed | 0.844*** | 0.845*** | 0.783*** | 0.782*** |
| Income (1–5) | 0.820*** | 0.819*** | 0.922*** | 0.920*** |
| Smoker | 1.570*** | 1.568*** | 0.611*** | 0.607*** |
| County variables | ||||
| Racial-ethnic Heterog. | 1.008 | 1.105 | 0.847*** | 0.897* |
| Poverty | 1.008*** | 1.007*** | 1.011*** | 1.007*** |
| Street connectivity | 0.999 | 1.000 | 0.998*** | 0.999*** |
| Walk Score | 0.998*** | 0.998*** | 0.999 | 0.999 |
| Fast food ratio | 1.053** | 1.062*** | 1.042*** | 1.040*** |
| Large central metro | 0.864*** | 1.003 | ||
| Large fringe metro | 0.973 | 1.088*** | ||
| Medium metro | 0.928*** | 1.063** | ||
| Small metro | 0.921*** | 1.057* | ||
| Micropolitan | 0.959* | 1.051* | ||
| Urban ratio | 1.048 | 1.301*** | ||
| Urban ratio squared | 0.795* | 0.702*** | ||
| AIC | 334145.2 | 325877.5 | 390696.7 | 380893.1 |
p≤ 0.001,
p≤ 0.01,
p≤ 0.05
In order to test the complexity of impact by urbanicity, we extract the subsets of data by urban-rural classifications. In other words, we are interested in examining whether the effects of individual and county-level variables are consistent in various geographic settings, here at different urbanicity levels. Tables 5 and 6 present the MLM results by the six NCHS urban-rural county categories and by the urban ratio ranges, respectively. Given the focus of this study, only the results on obesity are presented.
Table 5.
Odds ratios of multilevel logistic models for obesity by NCHS urban-rural classification
| Large central metro (N=37,354) | Large fringe metro (N=50,806) | Medium metro (N=53,722) | Small metro (N=35,562) | Micropolitan (N=40,551) | Noncore (N=15,617) | |
|---|---|---|---|---|---|---|
| Individual variables | ||||||
| Non-Hispanic Black | 1.866*** | 1.513*** | 1.689*** | 1.552*** | 1.606*** | 1.684*** |
| Hispanic | 1.121** | 1.048 | 1.073* | 1.080 | 1.010 | 0.973 |
| Other race/ethnicity | 0.824*** | 0.786*** | 0.941 | 1.027 | 1.138** | 1.164* |
| Age (18+) | 1.128*** | 1.122*** | 1.123** | 1.126*** | 1.118*** | 1.108*** |
| Age squared | 0.999*** | 0.999*** | 0.999*** | 0.999*** | 0.999*** | 0.999*** |
| Male | 1.004 | 1.148*** | 1.056*** | 1.073*** | 1.047* | 1.028 |
| Married | 0.893*** | 0.919*** | 0.964 | 0.950* | 0.982 | 0.997 |
| Education (1–4) | 0.800*** | 0.825*** | 0.832*** | 0.845*** | 0.860*** | 0.894*** |
| Employed | 0.779*** | 0.790*** | 0.778*** | 0.750*** | 0.782*** | 0.828*** |
| Income (1–5) | 0.959*** | 0.928*** | 0.916*** | 0.900*** | 0.899*** | 0.914*** |
| Smoker | 0.660*** | 0.623*** | 0.604*** | 0.607*** | 0.546*** | 0.587*** |
| County variables | ||||||
| Race Heterogeneity | 0.911 | 0.931 | 0.864 | 0.974 | 0.981 | 0.839 |
| Poverty | 1.019*** | 1.018*** | 1.007* | 0.994 | 1.000 | 1.009* |
| Street connectivity | 0.999*** | 0.998*** | 0.998 | 0.998 | 1.002 | 1.003 |
| Walk Score | 0.998*** | 0.999 | 0.999 | 1.000 | 1.001 | 1.001 |
| Fast food ratio | 1.006 | 0.999 | 1.152*** | 1.145** | 1.198*** | 1.032 |
| AIC | 61864.7 | 78092.6 | 88965.2 | 51172.4 | 63099.2 | 37431.2 |
p≤ 0.001,
p≤ 0.01,
p≤ 0.05
Table 6.
Odds ratios of multilevel logistic models for obesity by urban ratio ranges
| Completely urban (0.99, 1.00] (N=19,791) | Highly urban (0.90, 0.99] (N=63,773) | Mostly urban (0.50, 0.90] (N=119,568) | Marginally urban (0.01, 0.50] (N=92,764) | Completely rural [0, 0.01] (N=32,260) | |
|---|---|---|---|---|---|
| Individual variables | |||||
| Non-Hispanic Black | 1.907*** | 1.662*** | 1.605*** | 1.622*** | 1.681*** |
| Hispanic | 1.043 | 1.129*** | 1.084** | 0.997 | 0.949 |
| Other race/ethnicity | 0.829* | 0.809*** | 0.874*** | 1.099** | 1.224** |
| Age (18+) | 1.127 *** | 1.125*** | 1.126*** | 1.117*** | 1.112*** |
| Age squared | 0.999*** | 0.999*** | 0.999*** | 0.999*** | 0.999*** |
| Male | 0.900** | 1.082*** | 1.090*** | 1.061*** | 1.044 |
| Married | 0.853*** | 0.924*** | 0.946*** | 0.967* | 0.990 |
| Education (1–4) | 0.797*** | 0.804*** | 0.836*** | 0.857*** | 0.872*** |
| Employed | 0.753*** | 0.797*** | 0.774*** | 0.779*** | 0.813*** |
| Income (1–5) | 0.966* | 0.941*** | 0.914*** | 0.906*** | 0.914*** |
| Smoker | 0.657*** | 0.665*** | 0.616*** | 0.565*** | 0.563*** |
| County variables | |||||
| Race Heterogeneity | 1.029 | 0.731 | 0.881 | 0.865 | 0.981 |
| Poverty | 1.020*** | 1.014*** | 1.004 | 1.002 | 1.011*** |
| Street connectivity | 0.998*** | 1.000 | 0.998 | 0.998 | 1.004 |
| Walk Score | 0.999 | 0.998* | 0.999 | 1.000 | 1.000 |
| Fast food ratio | 0.963 | 1.003 | 1.203*** | 1.135*** | 1.025 |
| AIC | 21854.4 | 70995.4 | 138288.8 | 110971 | 38490.1 |
p≤ 0.001,
p≤ 0.01,
p≤ 0.05
Furthermore, some literature suggests that the association between built environment and physical activity (and obesity) may vary by gender (e.g., Berke et al. 2007; Wen and Kowaleski-Jones 2012). We further divide the data by gender, and explore the likely difference of associations between men and women. The results are presented in Table 7 and 8 for men and women, respectively.
Table 7.
Odds ratios of multilevel logistic models for obesity by NCHS urban-rural classification among men
| Large central metro (N=23,657) | Large fringe metro (N=29,413) | Medium metro (N=32,784) | Small metro (N=18,570) | Micropolitan (N=22,501) | Noncore (N=12,772) | |
|---|---|---|---|---|---|---|
| Individual variables | ||||||
| Non-Hispanic Black | 1.402*** | 1.118* | 1.240*** | 1.123 | 1.140 | 1.118 |
| Hispanic | 1.157** | 1.002 | 1.038 | 1.071 | 0.991 | 1.049 |
| Other race/ethnicity | 0.746*** | 0.741*** | 0.843** | 1.019 | 1.163* | 1.183 |
| Age (18+) | 1.122*** | 1.123*** | 1.127*** | 1.119*** | 1.125*** | 1.125*** |
| Age squared | 0.999*** | 0.999*** | 0.999*** | 0.999*** | 0.999*** | 0.999*** |
| Married | 1.137*** | 1.054 | 1.090** | 1.087* | 1.118*** | 1.150** |
| Education (1–4) | 0.828*** | 0.829*** | 0.834*** | 0.852*** | 0.838*** | 0.904*** |
| Employed | 0.763*** | 0.776*** | 0.761*** | 0.762*** | 0.777*** | 0.725*** |
| Income (1–5) | 1.004 | 0.993 | 0.999 | 0.963* | 0.983 | 0.994 |
| Smoker | 0.691*** | 0.623*** | 0.646*** | 0.553*** | 0.552*** | 0.602*** |
| County variables | ||||||
| Race Heterogeneity | 0.650 | 1.083 | 0.788 | 0.952 | 0.819 | 0.809 |
| Poverty | 1.024*** | 1.014*** | 1.009* | 0.995 | 1.001 | 1.009 |
| Street connectivity | 0.998*** | 0.998*** | 0.999** | 0.998* | 1.001 | 0.998 |
| Walk Score | 0.999 | 1.000 | 1.000 | 1.000 | 1.000 | 1.001 |
| Fast food ratio | 1.017 | 0.991 | 1.117** | 1.218** | 1.210*** | 1.022 |
| AIC | 26334.9 | 78092.6 | 88965.2 | 51172.4 | 63099.2 | 37431.2 |
p≤ 0.001,
p≤ 0.01,
p≤ 0.05
Table 8.
Odds ratios of multilevel logistic models for obesity by NCHS urban-rural classification among women
| Large central metro (N=31,794) | Large fringe metro (N=39,051) | Medium metro (N=43,617) | Small metro (N=25,238) | Micropolitan (N=30,582) | Noncore (N=18,177) | |
|---|---|---|---|---|---|---|
| Individual variables | ||||||
| Non-Hispanic Black | 2.138*** | 1.785*** | 1.960*** | 1.821*** | 1.865*** | 2.029*** |
| Hispanic | 1.090 | 1.088 | 1.114* | 1.101 | 0.989 | 0.921 |
| Other race/ethnicity | 0.891 | 0.829** | 1.026 | 1.031 | 1.116 | 1.134 |
| Age (18+) | 1.134*** | 1.123** | 1.121*** | 1.133*** | 1.115*** | 1.098*** |
| Age squared | 0.999*** | 0.999*** | 0.999*** | 0.999*** | 0.999*** | 0.999*** |
| Married | 0.739*** | 0.844*** | 0.887*** | 0.873*** | 0.923** | 0.923* |
| Education (1–4) | 0.764*** | 0.813*** | 0.821*** | 0.832*** | 0.867*** | 0.875*** |
| Employed | 0.773*** | 0.772*** | 0.769*** | 0.719*** | 0.758*** | 0.868*** |
| Income (1–5) | 0.936*** | 0.894*** | 0.871*** | 0.864*** | 0.846*** | 0.870*** |
| Smoker | 0.654*** | 0.631*** | 0.586*** | 0.667*** | 0.554*** | 0.587*** |
| County variables | ||||||
| Race Heterogeneity | 0.695 | 0.851 | 0.876 | 0.866 | 1.133 | 0.791 |
| Poverty | 1.016*** | 1.021*** | 1.007* | 0.995 | 1.000 | 1.009* |
| Street connectivity | 0.999*** | 0.998*** | 0.999** | 0.998* | 1.003*** | 1.001 |
| Walk Score | 0.998** | 0.999 | 0.999 | 1.001 | 0.999 | 1.000 |
| Fast food ratio | 1.003 | 1.012 | 1.176*** | 1.147* | 1.196*** | 1.045 |
| AIC | 35348.5 | 43600.1 | 50178.1 | 29058.3 | 35940.4 | 21828.8 |
p≤ 0.001,
p≤ 0.01,
p≤ 0.05
4. Results and Discussion
Results from General Models
Based on Tables 3 and 4, the effects of individual variables largely confirm the preliminary observations from Table 1 on the distributions of PI and OB rates by various socio-demographic groups, but some details are new. Even when the findings may appear consistent from the two tables, the MLM results have more clarity for the statistical significance associated with each variable and are also more reliable because the effects of neighborhood variables are controlled. The differences are highlighted here. Note that the findings are also consistent across the four PI models and across the four OB models. Non-Hispanic Blacks and Hispanics have higher risks of physical inactivity and obesity than their non-Hispanic White counterparts; and between the two major minority groups, the odd ratio of obesity is even higher for non-Hispanic Blacks than for Hispanics, but the odd ratio of physical inactivity is reversed. The latter finding (the reversed gaps in PI and OB between the two groups) is new from MLM. Both risks of physical inactivity and obesity increase initially with age and then drops after passing a certain age. The curvilinear effect of age is present in both PI and OB here, but absent for PI from Table 1. Males tend to be more physically active, but bear a higher risk of obesity. The latter finding is also new from MLM (certainly much stronger and more evident). In the MLMs, marital status is not significant for physical inactivity, but being married is negatively associated with the risk of obesity. This suggests that the large gap in PI between married (19.73%) and unmarried people (27.82%) from Table 1 may be caused by other confounding factors (age and others), and does not necessarily imply that the marital status is a factor in influencing physical activity. The lower obesity ratio for married people (also from Table 1) remains after other variables are controlled for. Higher education, being employed and higher income are all associated with lower risks of physical inactivity and obesity. Smokers have a higher risk of being inactive but a lower risk of obesity.
There are several discrepancies in an individual variable’s associations with PI and OB risks. It is understandable that smokers may tend to be more physical inactive while maintaining lower body weight since nicotine consumption increases energy expenditure and could suppress appetite (Chiolero et al. 2008). The results are rather puzzling for other variables (e.g., lower PI risk but higher OB risk for males, indifferent for PI but lower OB risk for married people) as higher PI is expected to be associated with a higher risk of OB. Why is the effect on PI not transferred to the effect on OB for the above population groups? Unless there is evidence of different behavior in food and beverage intakes or different metabolism, one may question the reliability of PI (a subjective assessment loosely defined) in comparison to OB (a rather more objective measure based on BMI) (Wang et al. 2013: 10–11). Also see Fan, Wen and Kowaleski-Jones (2014) for the difference in subjective and objective PI measures. We will keep this in mind, and hereafter focus more on the MLM results on obesity.
Net of individual controls, models PI2 and OB2 in Table 3 add two socio-demographic variables and three built environment measures at the county level, and models PI3, PI4, OB3 and OB4 in Table 4 add the effect of urbanicity. Declining AIC values from model PI1 to PI2 to PI3 to PI4 and also from OB1 to OB2 to OB3 to OB4 confirm the value and validity of MLMs, particularly models PI4 and OB4 with urbanicity defined by urban ratio. The lower AIC values in models PI4 and OB4 than their counterparts PI3 and OB3 demonstrate the higher explaining power by urban ratio (i.e., a continuous value built from data of finer spatial resolution) than the NCHS rural-urban category. The following discussion focuses on the results from models PI3, PI4, OB3 and OB4.
Racial-ethnic heterogeneity is not significantly associated with physical inactivity but negatively associated with obesity. Poverty rate is positively associated with both physical inactivity and obesity risks. Among the built environment variables, the ratio of fast-food-to-full-service restaurants is positively associated with physical inactivity and obesity risks in all models. Street connectivity is negatively associated with obesity (but not significant with physical inactivity), and walk score is negatively associated with physical inactivity (but not significant with obesity). Physical inactivity largely decreases with the level of urbanicity (measured in either NCHS classifications or urban ratio), which is consistent with the preliminary observation from Figure 2a. However, based on model OB3, obesity risk is the lowest in noncore and large central metro counties (with no statistically significant difference between them), and increases gradually in the order of micropolitan, small metro, medium metro, and large fringe metro. That is to say, with the exception of large central metro with the highest urbanicity, obesity risk climbs up with increasing urbanicity. It is captured by the curvilinear effect of urban ratio in model OB4, i.e., obesity risk increases with urban ratio and comes down after a certain urban ratio. This finding on obesity risk from Table 4 is different from the preliminary reading from Figure 2a. Again, one possible reason for the deviation between PI and OB models is the gap in measurement reliability between the two.
Results by Urbanicity Level and By Gender
Tables 5 and 6 show the MLM results on data subsets grouped by the NCHS categories and urban ratios, respectively. Here we highlight the differences from those based on all samples in the study area. Among the individual variables, the effects of most of the variables (e.g., non-Hispanic Black, age, education, employment, income and smoker) remain consistent across all six NCHS categories (Table 5) or across the five urban ratio ranges (Table 6), but others vary. For instance, with comparison to the findings from the global models, the higher obesity risk for Hispanics is no longer significant in the less urbanized areas, neither is the higher obesity risk for male in areas of the highest/lowest urbanicity, nor is the lower risk for married people in rural areas. These findings on the individual attributes call for more in-depth studies that may uncover possibly distinctive behavior of these demographic groups in different geographic environments.
Among the county-level variables, here we focus the discussion on the effects of built-environment variables. The relationship between street connectivity and obesity becomes insignificant in less urbanized areas, better walk score is only linked to reduced risk of obesity in large central metro areas (Table 5) or highly urban areas (Table 6), a higher ratio of fast-food to full-service restaurants is associated with a higher risk of obesity in moderately urbanized areas (i.e., medium metro, small metro and micropolitan from Table 5, marginally or mostly urban areas from Table 6). In other words, the positive effects of better street connectivity and walk score on lowering obesity risk are present in highly urbanized areas, and the food environment is in play more so in areas of middle-range urbanicity.
The consistency in results from Tables 5 and 6 validates the two systems of urban-rural classifications. Some of the effects of independent variables derived from the “global” model are altered in the “urbanicity-specific” models, more so for the neighborhood variables than individual variables. This implies that some obesity risk factors are sensitive to variation of geographic settings.
Comparing the results in Tables 7 and 8 indicates that some of the associations of individual or county variables with obesity risk differ between men and women, and such differences also vary by urbanicity. Here only noticeable gender differences are highlighted. For example, Black men are associated with a higher obesity risk across all urbanicity levels, but for Black women, the higher obesity risk is only present in more-urbanized counties (large central, large fringe and medium metro). Among Hispanics, a higher obesity risk is only significant for men in large central metro and for women in medium metro. These findings indicate that racial gaps in obesity risks (i.e., the higher risks for Blacks and Hispanics) as suggested by the general models on the whole data sample (reported in Table 3) are attributable to only specific gender(s) in selected geographic areas. Marital status is found to be positively associated with male obesity but negatively associated with female obesity, which is consistent with findings from the NHANES data (Wen and Kowaleski-Jones 2012). For income, it has little impact on men’s obesity risk in different urbanicity contexts, but is negatively associated with women’s obesity risk across areas of all urbanicity levels.
Among the county variables, the effects of most variables are consistent between men and women, and gender differences are only noticed in two cases. One is that better street connectivity remains relevant in lowering obesity risk in more urbanized areas (as observed from Tables 5–6 without dividing the samples by gender), but now with a counterintuitive exception (i.e., raising obesity risk for women in micropolitan counties). The other is that the positive effect of walk score on lowering obesity risk in the highest urbanized areas (as observed from Tables 5–6 without dividing the samples by gender) is only valid for women. The former calls for more in-depth analysis. On the latter, one may suspect that traditional domestic division of labor might be in play in a certain geographic setting such as central cities of large metro. In these areas, shopping for grocery and other items is more likely to be done by women than men, and therefore better walk environment influences women’s behavior more so than men.
5. Conclusion
The objective of this study is to explore the role of contextual attributes such as built environment in contributing to physical inactivity and obesity risks. While the measurements of neighborhood built environment are similar to those commonly investigated in the literature, the implementations at the national level, particularly walk score and food environment, are new. There is a significant association between built environment variables and physical inactivity/obesity, net of individual attributes and neighborhood socio-demographic characteristics. Another important highlight is the examination of possible variability of association between built environment and obesity across different urbanization levels and by gender. The lesson is simple and echoed by others (e.g., Slack et al. 2014): some obesity risk factors are geographically specific and vary between men and women, and one-size-fits-all public policies cannot be effective and need to be geographically adaptable and sensitive to the diversity of demographic groups.
The analysis on data subsets reveals the variability of effects of both individual and county-level variables in areas of different urbanicity levels. For county-level built environment variables, better street connectivity and walk score lowers obesity risk only in the highly urbanized areas, and food environment seems to be more of a factor in areas of middle urbanicity levels. Both street connectivity and walk score reflect walkability, whose variability is most likely to play a role in people’s health behavior across large cities but to a less extent in small-medium cities or rural areas. The prominent influence of food environment in areas of moderate urbanicity is interesting. One plausible theory may be that due to the ubiquity of fast-food restaurants in U.S., accessibility of fast food is fairly uniform in large cities or countryside and only exhibits a certain variability in areas between the two. Testing this theory or others on built environment begs for data with finer geographic resolutions than the county level available to this study.
Finally, gender is found to be an important moderator in obesity risks associated with both individual and neighborhood variables. The racial gaps in obesity risks as suggested by the general models are attributable to only a specific gender in selected geographic areas. The association of marital status and obesity is opposite between men and women, and benefit of high income for lowering obesity risk is only evident for women. There are also some gender differences in the effects of built environment factors.
Several limitations of the study need to be acknowledged. The first issue concerns the data. Both measures of physical inactivity and obesity rely on the survey data from the BRFSS. As pointed out previously, physical activity is loosely defined as “leisure-time physical activity in the last 30 days” reported by oneself, and raises the concern of reliability. In addition, county is the smallest geographic unit geocoded by the BRFSS data. A finer geographic resolution would help us define built environment at a spatial scale that is more relevant to people’s activity space such as zip code area or census tracts (Krieger et al. 2003, Sturm and Datar 2005, Xu and Wang 2015). The average size of the counties in the study area is 2,502.11 km2. Urban planners assume that one quarter mile (0.4 km) is a comfortable range for pedestrians (Rundle, Roux and Freeman 2007). Secondly, the measurements of built environment can be more comprehensive in future work. Limited by data availability and time, this study does not include variables such as accessibility of recreational facilities (e.g., parks, gyms), presence of mixed land use, climate and others that have been suggested to affect health behavior and outcome. Lastly, this study is cross-sectional without considering any temporal changes. The built environment defined is the present state of environment for an individual. A person’s BMI reflects the accumulated effect of one’s living environment and behavior, both of which may have changed. The research may establish the link between an environment factor and obesity, but cannot tell whether the neighborhood factor causes residents to live healthy or whether healthy individuals choose to live in neighborhood with such an environment. A longitudinal study similar to Jones and Huh (2014) may shred light on this issue.
Highlights.
This study examines association of built environments with obesity in the U.S.
Multilevel modeling considers both individual and neighborhood variables.
A poorer street connectivity is associated with a higher obesity risk.
A higher fast-food restaurants ratio is associated with a higher obesity risk.
A higher walk score is linked to a lower risk of obesity in urban areas for women.
Some obesity risk factors vary by urbanicity levels and between men and women.
Public policies need to be geographically adaptable.
Acknowledgments
Support by the National Institute of General Medical Sciences of the National Institutes of Health under award number R01CA140319-01A1 is gratefully acknowledged. Wang also acknowledges the support of a visiting professorship at Yunnan University of Finance and Economics in the summer of 2014.
Footnotes
The research is part of a larger project which has a component on examining spatial non-stationarity. Hawaii and Alaska are excluded for that component because of their non-contiguity with the conterminous U.S. For consistency, they are also excluded from this research.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Ahima RS, Lazar MA. The Health Risk of Obesity—Better Metrics Imperative. Science. 2013;341:856–858. doi: 10.1126/science.1241244. [DOI] [PubMed] [Google Scholar]
- Ball K, Lamb K, Travaglini N, Ellaway A. Street connectivity and obesity in Glasgow, Scotland: Impact of age, sex and socioeconomic position. Health & Place. 2012;18:1307–1313. doi: 10.1016/j.healthplace.2012.09.007. [DOI] [PubMed] [Google Scholar]
- Berke EM, Koepsell TD, Moudon AV, Hoskins RE, Larson EB. Association of the Built Environment With Physical Activity and Obesity in Older Persons. American Journal of Public Health. 2007;97(3):486–492. doi: 10.2105/AJPH.2006.085837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (CDC) [last accessed 3-13-2015];Obesity Prevalence Maps 2013. 2015 available http://www.cdc.gov/obesity/data/table-adults.html.
- Chalkias C, Papadopoulos AG, Kalogeropoulos K, Tambalis K, Psarra G, Sidossis L. Geographical heterogeneity of the relationship between childhood obesity and socio-environmental status: Empirical evidence from Athens, Greece. Applied Geography. 2013;37:34–43. [Google Scholar]
- Chi S-H, Grigsby-Toussaint DS, Bradford N, Choi J. Can Geographically Weighted Regression improve our contextual understanding of obesity in the US? Findings from the USDA Food Atlas. Applied Geography. 2013;44:134–142. [Google Scholar]
- Chiolero A, Faeh D, Paccaud F, Cornuz J. Consequences of smoking for body weight, body fat distribution, and insulin resistance. The American Journal of CLINICAL NUTRITION. 2008;87:801–809. doi: 10.1093/ajcn/87.4.801. [DOI] [PubMed] [Google Scholar]
- Ding D, Gebel K. Built environment, physicalactivity, and obesity: What have we learned from reviewing the literature? Health & Place. 2012;18:100–105. doi: 10.1016/j.healthplace.2011.08.021. [DOI] [PubMed] [Google Scholar]
- Durand C, Andalib M, Dunton G, Wolch J, Pentz M. A systematic review of built environment factors related to physical activity and obesity risk: implications for smart growth urban planning. Obes Rev. 2011:5. doi: 10.1111/j.1467-789X.2010.00826.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ewing R, Meakins G, Hamidi S, Nelson AC. Relationship between urban sprawl and physical activity, obesity, and morbidity-Update and refinement. Health & Place. 2014;26:118–126. doi: 10.1016/j.healthplace.2013.12.008. [DOI] [PubMed] [Google Scholar]
- Fan JX, Wen M, Kowaleski-Jones L. Rural-Urban Differences in Objective and Subjective Measures of Physical Activity: Findings From the National Health and Nutrition Examination Survey (NHANES) 2003–2006. Prev Chronic Dis. 2014:11. doi: 10.5888/pcd11.140189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Felton G, Dowda M, Ward D, Dishman R, Trost S, Saunders R, Pate R. Differences in physical activity between black and white girls living in rural and urban areas. J Sch Health. 2002;72:250–5. doi: 10.1111/j.1746-1561.2002.tb07338.x. [DOI] [PubMed] [Google Scholar]
- Feng J, Glass TA, Curriero FC, Stewart WF, Schwartz BS. The built environment and obesity: A systematic review of the epidemiologic evidence. Health & Place. 2010;16:175–190. doi: 10.1016/j.healthplace.2009.09.008. [DOI] [PubMed] [Google Scholar]
- Finkelstein EA, Trogdon JG, Cohen JW, Dietz W. Annual Medical Spending Attributable To Obesity: Payer-And Service-Specific Estimates. Health Affairs. 2009;28:w822–w831. doi: 10.1377/hlthaff.28.5.w822. [DOI] [PubMed] [Google Scholar]
- Front Seat. Walk Score API. 2013. [Google Scholar]
- Huang TT, Drewnowski A, Kumanyika SK, Glass TA. A Systems-Oriented Multilevel Framework for Addressing Obesity in the 21st Century. Prev Chronic Dis. 2009:6. [PMC free article] [PubMed] [Google Scholar]
- Ingram DD, Franco SJ. 2013 NCHS urban-rural classification scheme for counties. [last accessed on 3-13-2015];Vital Health Stat. 2014 2(166) available http://www.cdc.gov/nchs/data/series/sr_02/sr02_166.pdf. [PubMed] [Google Scholar]
- Jay M. The Relationship Between Obesity and the Prevalence of Fast Food Restaurants: State-Level Analysis. American Journal of Health Promotion. 2004;19:137–143. doi: 10.4278/0890-1171-19.2.137. [DOI] [PubMed] [Google Scholar]
- Jones M, Huh J. Toward a multidimensional understanding of residential neighborhood: A latent profile analysis of Los Angeles neighborhoods and longitudinal adult excess weight. Health & Place. 2014;27:134–141. doi: 10.1016/j.healthplace.2014.01.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krieger N, Chen J, Waterman P, Soobader M, Subramanian SV, Carson R. Choosing area based socioeconomic measures to monitor social inequalities in low birth weight and childhood lead poisoning: The Public Health Disparities Geocoding Project (US) J Epidemiol Community Health. 2003;57:186–99. doi: 10.1136/jech.57.3.186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lamichhane AP, Warren J, Putee R, Porter DE, Bottai M, Mayer-Davis EJ, Liese AD. Spatial patterning of supermarkets and fast food outlets with respect to neighborhood characteristics. Health & Place. 2013;23:157–164. doi: 10.1016/j.healthplace.2013.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lopez RP, Hyness HP. Obesity, physical activity, and the urban environment: public health research needs. ENVIRONMENTAL HEALTH. 2006:5. doi: 10.1186/1476-069X-5-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mehta NK, Chang VW. Weight Status and Restaurant Availability: A Multilevel Analysis. American Journal of Preventive Medicine. 2008;34:127–133. doi: 10.1016/j.amepre.2007.09.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Michimi A, Wimberly MC. Associations of supermarket accessibility with obesity and fruit and vegetable consumption in the conterminous United States. International Journal of Health Geographics. 2010;9:94–112. doi: 10.1186/1476-072X-9-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monnat SM, Pickett CB. Rural/urban differences in self-rated health: Examining the roles of county size and metropolitan adjacency. Health & Place. 2011;17:311–319. doi: 10.1016/j.healthplace.2010.11.008. [DOI] [PubMed] [Google Scholar]
- National Center for Health Statistics. Health, United States, 2012: With Special Feature on Emergency Care. Hyattsville, MD: 2013. [PubMed] [Google Scholar]
- National Center for Health Statistics (NCHS) [last accessed on 1-30-2015];NCHS Urban-Rural Classification Scheme for Counties. 2006 http://www.cdc.gov/nchs/data_access/urban_rural.htm.
- Ferdinand OA, Sen B, Rahurkar S, Engler S, Menachemi N. The relationship between built environments and physical activity: a systematic review. American Journal of Public Health. 2012;102:e7–e13. doi: 10.2105/AJPH.2012.300740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ogden CL, Carroll MD, Kit BK, Flegal KM. NCHS Data Brief. Hyattsville, MD: National Center for Health Statistics; 2013. Prevalence of Obesity Among Adults: United States 2011–2012. [PubMed] [Google Scholar]
- Papas MA, Alberg AJ, Ewing R, Helzlsouer KJ, Gary TL, Klassen AC. The Built Environment and Obesity. Epidemiologic Reviews. 2007;29:129–143. doi: 10.1093/epirev/mxm009. [DOI] [PubMed] [Google Scholar]
- Pereira M, Kartashov A, Ebbeling C, Van Horn L, Slattery M, Jocobs DJ, Ludwig DS. Fast-food habits, weight gain, and insulin resistance (the CARDIA study): 15-year prospective analysis. Lancet. 2005;365:36–42. doi: 10.1016/S0140-6736(04)17663-0. [DOI] [PubMed] [Google Scholar]
- Pierce I, Ernest V, Ashworth J. Tool for Health and Resilience in Vulnerable Environments. Health Department and Community Health Center; 2012. [Google Scholar]
- Powell P, Spears K, Rebori M. What is Obesogenic Environment? Reno: University of Nevada Cooperative Extension; 2010. [Google Scholar]
- Rundle A, Roux A, Freeman LM. The Urban Built Environment and Obesity in New York City: A Multilevel Analysis. American Journal of Health Promotion. 2007;21:326–34. doi: 10.4278/0890-1171-21.4s.326. [DOI] [PubMed] [Google Scholar]
- Sampson RJ, Groves WB. Community Structure and Crime: Testing Social-Disorganization Theory. American Journal of Sociology. 1989;94:774–802. [Google Scholar]
- Schulze MB, Manson JE, Ludwig DS, Colditz G, Stampfer MJ, Willett WC. Sugar-sweetened beverages, weight gain, and incidence of type 2 diabetes in young and middle-aged women. Journal of the American Medical Association. 2004;292:927–934. doi: 10.1001/jama.292.8.927. [DOI] [PubMed] [Google Scholar]
- Slack T, Myers CA, Martin CK, Heymsfield SB. The Geographic Concentration of US Adult Obesity Prevalence and Associated Social, Economic, and Environmental Factors. Obesity. 22:868–874. doi: 10.1002/oby.20502. [DOI] [PubMed] [Google Scholar]
- Sturm R, Datar A. Body mass index in elementary school children, metropolitan area food prices and food outlet density. Public Health. 2005;119:1059–68. doi: 10.1016/j.puhe.2005.05.007. [DOI] [PubMed] [Google Scholar]
- Wang F, Wen M, Xu Y. Population-Adjusted Street Connectivity, Urbanicity and Risk of Obesity in the U.S. Applied Geography. 2013;41:1–14. doi: 10.1016/j.apgeog.2013.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang MC, Kim S, Gonzalez AA, MacLeod KE, Winkleby MA. Socioeconomic and food-related physical characteristics of the neighbourhood environment are associated with body mass index. J Epidemiol Community Health. 2007;61:491–498. doi: 10.1136/jech.2006.051680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weir LA, Etelson D, Brand DA. Parents’ perceptions of neighborhood safety and children’s physical activity. Preventive Medicine. 2006;43:212–217. doi: 10.1016/j.ypmed.2006.03.024. [DOI] [PubMed] [Google Scholar]
- Wen M, Kowaleski-Jones L. The built environment and risk of obesity in the United States: Racial–ethnic disparities. Health & Place. 2012;18:1314–1322. doi: 10.1016/j.healthplace.2012.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson D, Kirtland K, Ainsworth B, Addy C. Socioeconomic status and perceptions of access and safety for physical activity. Ann Behav Med. 2004;28:20–8. doi: 10.1207/s15324796abm2801_4. [DOI] [PubMed] [Google Scholar]
- Xu Y, Wang L. GIS-based analysis of obesity and the built environment in the U.S. Cartography and Geography Information Science. 2015;42:9–21. [Google Scholar]
- Xu Y, Wen M, Wang F. Multilevel Built Environment Features and Individual Odds of Overweight and Obesity in Utah. Applied Geography. 2015 doi: 10.1016/j.apgeog.2014.10.006. forthcoming. [DOI] [PMC free article] [PubMed] [Google Scholar]