Abstract
Introduction
In children, elevated amino terminal pro B-type naturetic peptide (NT-proBNP) levels are associated with impaired heart function. The predictive value of serial monitoring of NT-proBNP levels in acute decompensated heart failure (ADHF) is unclear.
Methods
This prospective observational study enrolled patients ≤ 21 years with primary myocardial dysfunction and ADHF. NT-proBNP levels were obtained on enrollment (D0), day 2 (D2) and day 7 (D7). Clinical, laboratory and imaging data were collected on enrollment. CV outcome was defined as Heart Transplant (HTx), Ventricular Assist Device (VAD) placement, Extracorporeal Membrane Oxygenation or death at 1 year after admission. NT-proBNP levels and the percent change from D0 to D2 and D0 to D7 were calculated and compared between those with and without adverse cardiovascular (ACV) outcome.
Results
Sixteen consecutive patients were enrolled. ACV outcome occurred in 6 (37.5%, 4 HTx and 2 VAD). In patients with an ACV outcome, median NT-ProBNP levels at D7 were significantly higher (7,365 Vs. 1,196 pg/ml; p= 0.02) and the percent decline in NT-proBNP was significantly smaller (28% vs. 73%, p=0.02) compared to those without an ACV outcome. ROC curve analysis revealed that a less than 55% decline in NT-proBNP levels at D7 had a sensitivity and specificity of 83% and 90% respectively in predicting an ACV [AUC 0.86, CI (0.68,1.0), p=0.02].
Conclusions
In conclusion, children with primary myocardial dysfunction and ADHF, a persistently elevated NT-proBNP and/or a lesser degree of decline in NT-proBNP during the first week of presentation were strongly associated with ACV outcome. Serial NT-proBNP monitoring may allow the early identification of children at risk for worse outcome.
Keywords: acute decompensated heart failure, NT-proBNP, pediatric heart failure, cardiomyopathy, heart failure outcomes, heart transplant
INTRODUCTION
Heart failure in children less than 16 years of age is a rare but important medical problem with an annual incidence of about 0.87 per 100,000 population.1 The natriuretic peptides include B-type natriuretic peptide (BNP), prohormone BNP (pro-BNP) and amino-terminal pro-BNP (NT-proBNP). ProBNP (108 amino acids) has been shown to be released from ventricular myocardium in heart failure.2 It is cleaved by a circulating endoprotease, termed corin, into two polypeptides: the inactive NT-pro-BNP (76 amino acids), and a bioactive BNP (32 amino acids). NT-proBNP is more stable and has a longer half-life of about 2 hours as compared BNP, which has half-life of about 20 minutes. Elevations in plasma BNP have been described in children and young adults with ventricular dysfunction and cardiomyopathy or congenital heart.3,4 In adults with heart failure, BNP and NT-proBNP levels have been used as a predictor of adverse cardiovascular outcomes and hospital readmission.5–9 In some adult heart failure studies, serial monitoring of natriuretic peptides has been used to direct medical management and predict prognosis.10,11 Small studies in children with primary and acquired myocardial dysfunction have found serial monitoring useful in predicting the need for mechanical circulatory support12 or predicting outcome in patients with dilated cardiomyopathy.13 This study evaluates the ability of serial NT-proBNP monitoring in children with primary myocardial dysfunction and acute decompensated heart failure (ADHF) to identify high-risk patients and predict outcomes.
METHODS
This prospective observational study was conducted at the Children’s Hospital at Montefiore, Bronx, New York. All children younger than 21 years of age with primary myocardial dysfunction who were admitted with ADHF to the pediatric intensive care unit were enrolled within 24 hours of admission between June, 2011 and June, 2012. ADHF was defined as new onset decompensated heart failure or decompensation of chronic, established heart failure with symptoms sufficient to warrant hospitalization.14 Children with ADHF associated with congenital heart disease, arrhythmia, previous history of heart transplant, sepsis, endocrine abnormalities and ischemia were excluded from the study. Each patient’s clinical course in the hospital including need for inotropic support, diuretics and vasoactive medications was recorded and vasoactive inotrope calculated as described by Gaies et al15. Heart failure was classified according to the modified Ross Heart Failure or NYHA classification depending on the age of the patient.16 Basic demographic and laboratory data including electrolytes, blood urea nitrogen, serum creatinine and echocardiogram were obtained on hospital day 0 and 7. NT-proBNP levels were obtained within 24 hours of enrollment (D0), 48 hours later (D2) and at 7 days after admission (D7). Samples were immediately sent to and analyzed by our clinical laboratory. Assays were performed on an Elecsys electro chemiluminescent immunoassay system using Elecsys 1010/2010 immunoassay analyzers (Roche Diagnostics). Death, the need for heart transplantation, extracorporeal membrane oxygenator (ECMO) support or ventricular assist device within the first year after enrollment were recorded. The echocardiogram at last follow-up was also reviewed. A composite endpoint of adverse cardiovascular (ACV) outcome was defined as the need for ECMO, heart transplantation, VAD or death. Demographic and laboratory values and ejection fraction at enrollment were compared between those with and without an ACV outcome at the end of 1 year.
In this prospective observational study, the clinicians were aware of the NT-proBNP levels and management of the patients was directed by the attending intensivist and cardiologist. Prior to and during the study, there were no clinical management protocols or pathways based on NT-proBNP levels. This study was approved by the Institutional Review Board of Montefiore Medical Center and the Albert Einstein College of Medicine.
STATISTICAL ANALYSIS
Continuous variables were not normally distributed so data from these are expressed as median [interquartile range (IQR)]. NT-proBNP values were assessed in pg/ml units and also log transformed. Percent change in NT-proBNP at D2 and D7 was calculated by using the following formula:
%change NT-proBNP = [(NT-proBNP Day 0– NT-proBNP Day 2 or NT-proBNP Day 7) / NT-proBNP Day 0]*100.
Demographic and laboratory variables including the NT-proBNP levels were compared between D0 and D7. The NT-proBNP levels at D0, D2 and D7 were compared between patients with and without an ACV outcome as were the percent change in NT-proBNP levels. The predictive value of a rise in NT proBNP level was determined by comparing patients who had an increase in the NT-proBNP level at from D0 to D2, D2 to D7 or D0 to D7 to those who did not.
Tests of bivariate associations were performed with Mann-Whitney U tests, Wilcoxon rank-sum tests, Fisher's exact tests and Spearman rho as appropriate. A two-tailed alpha of .05 was used to denote statistical significance. A multivariate analysis for factors associated with ACV outcome was not performed due to the small number of patients in the study. All statistical analyses were performed with SPSS software (Version 19).
RESULTS
Patient Demographics
Sixteen consecutive patients who met study inclusion criteria were enrolled in the study. All patients were enrolled within 24 hours of admission to the intensive care unit. Ten patients were receiving inotropic support at the time of enrollment. No patients who met study criteria during the study time period were excluded. Median (IQR) age was 16 (5, 18) years and 50% were male (Table 2). The most common underlying diagnosis associated with ADHF was dilated cardiomyopathy (10/16, 62%). More than half of the patients (9/16, 56%) had NYHA/Modified Ross heart failure class ≥ 3. NT-proBNP levels were obtained at the prespecified time points for all patients.
Table 2.
Patient demographics, clinical and laboratory profile on admission and day 7 of pediatric critical care unit stay. Data expressed as median with interquartile ranges. NYHA=New York Heart Association, HF=heart failure.
| Day 0 | Day 7 | p-value* | |
|---|---|---|---|
| Total patients | 16 | ||
| Age (yrs) | 16 (5, 18) | ||
| Males (%) | 8 (50%) | ||
| Ross/NYHA HF class | 3(2–4) | 3(1–4) | 0.52 |
| Vasopressor Score | 5(0–5) | 5(0–5) | 0.62 |
| Ejection fraction (%) | 33 (19–46) | 29 (21–53) | 0.31 |
| Sodium (mEq/L) | 136 (135–140) | 137 (136–141) | 0.69 |
| Blood Urea Nitrogen (mg/dL) | 14 (11–17) | 16 (12–24) | 0.07 |
| Serum Creatinine (mg/dL) | 0.7 (0.3–1.0) | 0.7 (0.4–0.8) | 0.61 |
| NT-pro BNP (pg/ml) | 5,578 (2,952–14,591) | 3,226 (642–7,610) | 0.006 |
Values expressed as median (25 and 75th percentiles). Comparisons by Wilcoxon signed-rank test.
For the entire cohort, there was no significant difference in ejection fraction, serum sodium, BUN or creatinine from D0 to D7 (Table 2). NT-proBNP levels at D7 were significantly lower compared to D0 (p=0.006). NT-proBNP levels correlated significantly with ejection fraction on D0 and D7 (rho =−0.06, p=0.01 and −0.75, rho=0.003 respectively).
ACV Outcome and laboratory measures
Six patients (37.5%) reached an ACV outcome at a median of 1 month (range 1 –7 months) following enrollment. Four patients underwent heart transplant and two patients received VAD and underwent subsequent transplantation (Figure 1). None of the patients died. Ten patients did not reach an ACV outcome, 8 of whom had normalization of their ejection fraction. One out 6 patient in the ACV outcome group had EF>30% and 2 out of 10 patients in the No ACV group had EF<30%. Patients with ACV outcomes had significantly worse Ross/NYHA HF class at enrollment, lower ejection fraction on D0 and D7 and longer PICU and hospital length of stay (Table 1). ACV outcome showed modestly stronger statistically significant correlation to D0–D7 percent change in NT-proBNP compared to change in D0–D7 EF (rho=0.616, p=0.01 and rho=−0.423, p=0.15 respectively). Renal function and serum sodium levels were not significantly different between the groups. Table 3 depicts the trends in NT-proBNP levels at D0, D2 and D7 in the whole cohort and in patients with and without ACV outcome. NT-proBNP levels on D7 were significantly higher in patients with an ACV outcome.
Figure 1.
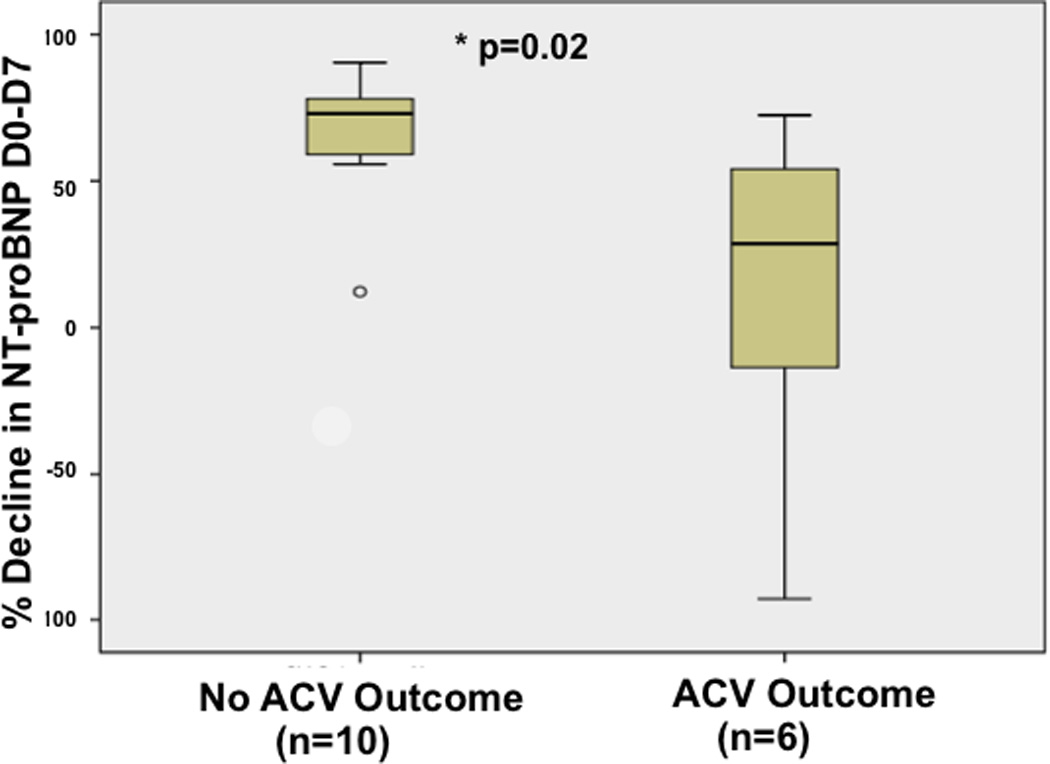
Percent decline in NT Pro-BNP from Day 0 to Day 7 in patients with and without ACV outcome
Table 1.
Patient characteristics: No adverse cardiovascular outcome (ACV) versus ACV group
| No ACV (n=10) | ACV (n=6) | *p-value | |
|---|---|---|---|
| Age (years) | 16.4 (10.4, 18.7) | 11.0 (4.1, 18.2) | 0.49 |
| Etiology of HF DCM Myocarditis RCM |
4 5 1 |
6 0 0 |
|
| Acute HF Acute on chronic HF |
8 2 |
2 4 |
|
| NYHA/Ross HF class | 2 (2,3) | 4 (3–4) | 0.04 |
| Vasopressor score | 1.5 (0.0, 5.0) | 5 (4, 6) | 0.12 |
| Blood Urea Nitrogen (BUN) | 13 (11, 16) | 17.5 (11.5–20.5) | 0.12 |
| Creatinine (mg/dl) | 0.7 (0.30, 0.85) | 0.65 (0.35–1.05) | 0.88 |
| Sodium (mEq/L) | 138 (136, 140) | 136 (128, 140) | 0.31 |
| Ejection Fraction (EF) D0 (%) | 44 (29, 50) | 21 (17, 27) | 0.02 |
| EF D7 (%) | 42 (29, 57) | 20 (11, 23) | 0.002 |
| PICU length of stay (days) | 7 (4–10) | 24 (21–40) | 0.004 |
| Hospital length of stay (days) | 9 (8–11) | 30 (25–47) | 0.02 |
| Outcomes | EF normal = 8 EF abnormal = 2 |
HTx = 4 VAD = 2 |
Values expressed as median (25 and 75th percentiles). Comparisons by Mann-Whitney U test
EF= Ejection fraction, Htx=Heart transplant, VAD ventricular assist device
Table 3.
NT-proBNP levels (pg/ml)* at D0, D2 and D7
| All patients (n=16) |
CV outcome (n=6) |
No CV outcome (n=10) |
p value | |
|---|---|---|---|---|
| NT-proBNP Day 0 | 5,578 (2,952–14,591) | 13,150 (7,865–15,274) | 4,425 (1,637–6,392) | 0.10 |
| NT-pro BNP Day 2 | 3,581 (1,707–6,205) | 5,329 (4,382–13,981) | 2,147 (866–3,574) | 0.07 |
| NT-pro BNP Day 7 | 3,226 (642–7,610) | 7,365 (4613–14,333) | 1,196 (313–3,084) | 0.02 |
| NT-pro BNP percent decline Day 2 | 48 (36–57) | 34 (33–60) | 49 (40–56) | 0.45 |
| NT-pro BNP percent decline Day 7 | 62 (35–75) | 28.5 (−7–51) | 73 (61–79) | 0.02 |
Values expressed as median (25 and 75th percentiles). Comparisons by Mann-Whitney U test
NT pro-BNP levels significantly decreased from D0 to D7 in the patients without an ACV outcome (p=0.005). NT-proBNP levels did not significantly change from D0 to D7 in the patients with an ACV outcome. NT-proBNP levels were significantly higher at D7 in patients who had an ACV outcome compared to patients without an ACV outcome. The percent decline in the NT-proBNP levels was significantly smaller in patients with CV outcome (Figure 1). Receiver operating curve analysis (ROC) to study the association between percent change in NT-proBNP levels and ACV outcome revealed significant association between percent change in NT-proBNP D0–D7 and D2–D7(AUC 0.87, 95% CI (0.68,1.0), p=0.02 and AUC 0.86, 95% CI (0.67,1.0), p=0.02 respectively, Table 4). A decline of < 55% in the D0–D7 NT-proBNP level had a sensitivity of 83% and specificity of 90% for predicting ACV outcome and a decline of < 35% in the D2–D7 NT-proBNP level had a sensitivity of 100% and specificity of 70% for predicting CV outcome (Table 4).
Table 4.
Receiver operating curve (ROC) analysis for percent change in NT-proBNP levels and ACV outcome.
| % change in NT-proBNP D0–D7 AUC 0.87, 95% CI (0.68,1.0) p=0.02 |
Percent Decline in NT- proBNP D0–D7 |
Sensitivity | Specificity |
| ≤ 72% | 100% | 50% | |
| ≤ 0% | 33% | 100% | |
| Inflection point | <55% | 83% | 90% |
| % change in NT-proBNP D0–D2 AUC 0.62, 95% CI (0.25,0.98) p=0.45 |
Percent Decline in NT- proBNP D0–D2 |
Sensitivity | Specificity |
| ≤ 5% | 100% | 50% | |
| ≤ 0% | 33% | 100% | |
| Inflection point | <65% | 83% | 90% |
| % change in NT-proBNP D2–D7 AUC 0.86, 95% CI (0.67,1.0) p=0.02 |
Percent Decline in NT- proBNP D2–D7 |
Sensitivity | Specificity |
| ≤ 35% | 100% | 70% | |
| ≤ 0% | 33% | 100% | |
| Inflection point | <35% | 100% | 70% |
DISCUSSION
In this prospective study of children with primary myocardial dysfunction and ADHF, the serial change in NT-proBNP levels during the first week after presentation was strongly associated with outcome at one year. Baseline NT-proBNP levels were markedly elevated with a median of 5,578pg/ml. A greater degree of elevation in NT-proBNP in pediatric heart failure as compared to adults is not uncommon and has been reported in other pediatric studies.12, 17 A higher NT-proBNP levels correlated with lower ejection fraction and worse heart failure class.
Diagnostic tests (Echo or laboratory values) add an element of objectivity to the clinician’s assessment. While it is expected that patients with lower EF would have worse outcomes, in our study, 1 out 6 patient in the Adverse cardiovascular (ACV) outcome group had EF>30% and 2 out of 10 patients in the No ACV group had EF<30%. On analysis using spearman’s correlation coefficient, we found that change in NT-proBNP level had a modestly stronger and statistically significant rho value in predicting adverse cardiovascular outcome compared to change in EF (rho= 0.616, p=0.01 vs rho= −0.42, p=0.15 respectively) and getting repeated values from a simple blood draw may be easier in many clinical settings than getting frequent repeated EF values. Hence we believe serial testing of NT-proBNP would be useful in addition to clinical and echocardiographic assessment of children with ADHF.
The serial change in NT-proBNP levels during the first week after presentation was strongly associated with outcome at one year. Those in whom the NT-proBNP remained high or escalated during the first week were more likely to have an ACV outcome. The converse was also demonstrated, a greater decline in NT-proBNP levels at D7 was associated with a better cardiovascular outcome. Higher NT-proBNP levels have been found to predict adverse cardiovascular events in children with chronic heart failure.8 Price et al studied BNP levels in children with chronic left ventricular dysfunction associated with primary and secondary myocardial diseases and reported that BNP level were higher in patients with adverse cardiovascular outcome and a BNP cutoff level >300 pg/ml had a sensitivity and specificity of 93% and 95% respectively. Although, we did not check for an absolute value, but we found a similar sensitivity and specificity of 83% and 90% respectively with a less than 55% decline in NT-proBNP levels at D7.
In a study of children with ventricular dysfunction and ADHF of heterogeneous etiology including cardiomyopathy, arrhythmia, ischemia, congenital heart disease and post-transplant rejection, Wong et al12 reported that patients who required escalation of therapy to mechanical circulatory support (MCS) had higher median NT-proBNP levels at all-time points but did not report the magnitude of the change from baseline. While we found percent change in the NT-proBNP to be significantly different in patients with and without ACV, they reported significant difference in the rate of change of NT-proBNP levels between patients with and without need for MCS, and that absolute levels were not predictive of need for MCS support. This is similar to our findings that the trend rather than the absolute value of NT-proBNP matters most in predicting the adverse cardiovascular outcome.
The current study demonstrates that a < 55% decline in NT-proBNP at D7 had a specificity of 90% for ACV outcome. Di Somma et al18 studied adults with ADHF and found that a decline in the BNP level > 46% at discharge and an absolute value of < 300 pg/ml had a strong negative predictive value for future adverse cardiovascular events in ADHF. Bayes-Genis et al19 reported that in adults with heart failure, a decline in NT-proBNP level < 30% identified a subgroup of high risk patients and was also the best predictor of cardiovascular death.
In children, Kim et al13 retrospectively evaluated the utility of serial NT-proBNP levels drawn at presentation and 3 and 6 months after diagnosis in children with primary and acquired dilated cardiomyopathy. They found that the NT-proBNP levels 3 months after diagnosis and not the change in NT-proBNP level (percent or absolute) were predictive of adverse outcome. In contrast to our study, serial levels within the first week of presentation were not measured and patients were included for study only if they had levels available at 3 months after presentation. In our study, 5/6 patients had reached the CV endpoint within one month of presentation. Also, it is not clear how many of their patients were inpatients since all of our patients were inpatients in the pediatric critical care unit. Further, Metra et al20 and Michtalik et al21 reported percent change in NT-proBNP levels by 48 hours and 1st month to be predictive of adverse cardiovascular outcome in patients with acute heart failure.
Tan et al22 reported an association between final, rather than admission, BNP levels and adverse outcomes (hospital readmission and death) in children, but did not comment upon the importance of a change in levels over time. The number of blood samples/BNP measurements and the interval between initial and final measurement was variable among patients. Also, in contrast to our study, they did not consider need for surgery/transplant and MCS as an adverse outcome, as a result 29/34 (85%) of the children who needed surgery/MCS were in “low risk / readmission and death free” group. In our study we found an association between percent changes in the NT-proBNP levels and ACV. It seems from our results and the results of other studies13, 20 that adverse cardiovascular outcomes are related to BNP/NT-proBNP levels at some time point later than the admission/initial levels. The NT-proBNP levels after admission in some way indicates the adequacy or inadequacy of the medical therapy, thereby differentiating the high-risk patients likely to have adverse cardiovascular events.
Limitations
The limitations of our study include the small sample size which precluded multivariable analysis for other factors that would influence CV outcome. Our institution is a referral center for advanced therapy for HF; thus the patient population may be selective for more seriously ill children with HF and may not represent the entire spectrum of ADHF in children. The treating clinicians were not blinded to the NT-proBNP levels. This probably would have caused minimal bias if at all since no clinical management protocols or pathways based on NT-proBNP levels were present prior to/or during the study.
Conclusion
This prospective, observational hypothesis-driven study provides evidence that a persistently elevated NT-proBNP level or a decline of < 50% in NT-proBNP levels shortly after presentation is prognostic for adverse cardiovascular outcomes in pediatric patients with primary myocardial dysfunction and ADHF. Further larger studies will be needed to establish the value of serial monitoring of NT-proBNP levels in the management of pediatric ADHF patients.
Acknowledgments
This work was supported in part by the CTSA Grant 1 UL1 TR001073-01, 1 TL1 TR001072-01, 1 KL2 TR001071-01 from the National Center for Advancing Translational Sciences (NCATS), a component of the National Institutes of Health (NIH).
Dr. Hsu consulted for Novartis and Bayer. Her institution received grant support from the National Institutes of Heath (NIH). Dr. Cohen received support for article research from the NIH and consulted for the American Journal of Hypertension (Co-executive Editor of a nonprofit medical journal). His institution received grant support from the NIH (CTSA grant for core support) and various federal grants (support for salary from the Medical School).
Footnotes
Copyright form disclosures:
The remaining authors have disclosed that they do not have any potential conflicts of interest.
REFERENCES
- 1.Andrews RE, Fenton MJ, Ridout DA, Burch M British Congenital Cardiac A. New-onset heart failure due to heart muscle disease in childhood: a prospective study in the United kingdom and Ireland. Circulation. 2008;117:79–84. doi: 10.1161/CIRCULATIONAHA.106.671735. [DOI] [PubMed] [Google Scholar]
- 2.Braunwald E. Biomarkers in heart failure. N Engl J Med. 2008;358:2148–2159. doi: 10.1056/NEJMra0800239. [DOI] [PubMed] [Google Scholar]
- 3.Law YM, Keller BB, Feingold BM, Boyle GJ. Usefulness of plasma B-type natriuretic peptide to identify ventricular dysfunction in pediatric and adult patients with congenital heart disease. Am J Cardiol. 2005;95:474–478. doi: 10.1016/j.amjcard.2004.10.014. [DOI] [PubMed] [Google Scholar]
- 4.Mangat J, Carter C, Riley G, Foo Y, Burch M. The clinical utility of brain natriuretic peptide in paediatric left ventricular failure. Eur J Heart Fail. 2009;11:48–52. doi: 10.1093/eurjhf/hfn001. [DOI] [PubMed] [Google Scholar]
- 5.Doust JA, Pietrzak E, Dobson A, Glasziou P. How well does B-type natriuretic peptide predict death and cardiac events in patients with heart failure: systematic review. BMJ. 2005;330:625. doi: 10.1136/bmj.330.7492.625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Valle R, Aspromonte N, Carbonieri E, D’Eri A, Feola M, Giovinazzo P, Noventa F, Prevaldi C, Barro S, Milani L. Fall in readmission rate for heart failure after implementation of B-type natriuretic peptide testing for discharge decision: a retrospective study. Int J Cardiol. 2008;126:400–406. doi: 10.1016/j.ijcard.2006.03.097. [DOI] [PubMed] [Google Scholar]
- 7.Auerbach SR, Richmond ME, Lamour JM, Blume ED, Addonizio LJ, Shaddy RE, Mahony L, Pahl E, Hsu DT. BNP levels predict outcome in pediatric heart failure patients: post hoc analysis of the Pediatric Carvedilol Trial. Circ Heart Fail. 2010;3:606–611. doi: 10.1161/CIRCHEARTFAILURE.109.906875. [DOI] [PubMed] [Google Scholar]
- 8.Price JF, Thomas AK, Grenier M, Eidem BW, O’Brian Smith E, Denfield SW, Towbin JA, Dreyer WJ. B-type natriuretic peptide predicts adverse cardiovascular events in pediatric outpatients with chronic left ventricular systolic dysfunction. Circulation. 2006;114:1063–1069. doi: 10.1161/CIRCULATIONAHA.105.608869. [DOI] [PubMed] [Google Scholar]
- 9.Valle R, Aspromonte N, Feola M, Milli M, Canali C, Giovinazzo P, Carbonieri E, Ceci V, Cerisano S, Barro S, Milani L. B-type natriuretic peptide can predict the medium-term risk in patients with acute heart failure and preserved systolic function. J Card Fail. 2005;11:498–503. doi: 10.1016/j.cardfail.2005.05.002. [DOI] [PubMed] [Google Scholar]
- 10.Januzzi JL, Troughton R. Are serial BNP measurements useful in heart failure management? Serial natriuretic peptide measurements are useful in heart failure management. Circulation. 2013;127:500–507. doi: 10.1161/CIRCULATIONAHA.112.120485. [DOI] [PubMed] [Google Scholar]
- 11.Desai AS. Are serial BNP measurements useful in heart failure management? Serial natriuretic peptide measurements are not useful in heart failure management: the art of medicine remains long. Circulation. 2013;127:509–516. doi: 10.1161/CIRCULATIONAHA.112.120493. [DOI] [PubMed] [Google Scholar]
- 12.Wong DT, George K, Wilson J, Manlhiot C, McCrindle BW, Adeli K, Kantor PF. Effectiveness of serial increases in amino-terminal pro-B-type natriuretic peptide levels to indicate the need for mechanical circulatory support in children with acute decompensated heart failure. Am J Cardiol. 2011;107:573–578. doi: 10.1016/j.amjcard.2010.10.015. [DOI] [PubMed] [Google Scholar]
- 13.Kim G, Lee OJ, Kang IS, Song J, Huh J. Clinical implications of serial serum N-terminal prohormone brain natriuretic Peptide levels in the prediction of outcome in children with dilated cardiomyopathy. Am J Cardiol. 2013;112:1455–1460. doi: 10.1016/j.amjcard.2013.07.007. [DOI] [PubMed] [Google Scholar]
- 14.Fonarow GC, Adams KF, Jr, Abraham WT, Yancy CW, Boscardin WJ ADHERE Scientific Advisory Committee, Study Group, and Investigators. Risk stratification for in-hospital mortality in acutely decompensated heart failure: classification and regression tree analysis. JAMA. 2005;293:572–580. doi: 10.1001/jama.293.5.572. [DOI] [PubMed] [Google Scholar]
- 15.Gaies Michael G, MD, MPH, Gurney James G, PhD, Yen Alberta H, Napoli Michelle L, Gajarski Robert J, MD, Ohye Richard G, MD, Charpie John R, MD, PhD, Hirsch Jennifer C., MD Vasoactive–inotropic score as a predictor of morbidity and mortality in infants after cardiopulmonary bypass. Pediatr Crit Care Med. 2010;11:234–238. doi: 10.1097/PCC.0b013e3181b806fc. [DOI] [PubMed] [Google Scholar]
- 16.Ross RD, Bollinger RO, Pinsky WW. Grading the severity of congestive heart failure in infants. Pediatr Cardiol. 1992;13:72–75. doi: 10.1007/BF00798207. [DOI] [PubMed] [Google Scholar]
- 17.Fried I, Bar-Oz B, Perles Z, Rein AJ, Zonis Z, Nir A. N-terminal pro-B-type natriuretic peptide levels in acute versus chronic left ventricular dysfunction. J Pediatr. 2006;149:28–31. doi: 10.1016/j.jpeds.2006.02.038. [DOI] [PubMed] [Google Scholar]
- 18.Di Somma S, Magrini L, Pittoni V, Marino R, Mastrantuono A, Ferri E, Ballarino P, Semplicini A, Bertazzoni Z, Carpinteri G, Mule’ P, Pazzaqlia M, Shah K, Mailsel A, Clopton P. In-hospital percentage BNP reduction is highly predictive for adverse events in patients admitted for acute heart failure: the Italian RED Study. Critical care. 2010;14:R116. doi: 10.1186/cc9067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bayes-Genis A, Lopez L, Zapico E, Cotes C, Santalo’ M, Ordonez-Llanos J, Cinca J. NT-ProBNP reduction percentage during admission for acutely decompensated heart failure predicts long-term cardiovascular mortality. J Card Fail. 2005;11:S3–S8. doi: 10.1016/j.cardfail.2005.04.006. [DOI] [PubMed] [Google Scholar]
- 20.Metra Marco, Nodari Savina, Parrinello Giovanni, Specchia Claudia, Brentana Loretta, Rocca Patrizia, Fracassi Francesco, Bordonali Tania, Milani Patrizia, Danesi Rossella, Verzura Giulia, Chiari Ermanna, Dei Cas Livio. The role of plasma biomarkers in acute heart failure. Serial changes and independent prognostic value of NT-proBNP and cardiac troponin-T. European Journal of Heart Failure. 2007;9:776–786. doi: 10.1016/j.ejheart.2007.05.007. [DOI] [PubMed] [Google Scholar]
- 21.Michtalik Henry J, MD, MPH, Yeh Hsin-Chieh, PhD, Campbell Catherine Y, MD, Haq Nowreen, MD, MPH, Park Haeseong, MD, MPH, Clarke William, PhD, MBA, Brotman Daniel J., MD Acute Changes in N-Terminal Pro-B-Type Natriuretic Peptide During Hospitalization and Risk of Readmission and Mortality in Patients With Heart Failure. Am J Cardiol. 2011;107:1191–1195. doi: 10.1016/j.amjcard.2010.12.018. [DOI] [PubMed] [Google Scholar]
- 22.Tan LH, Jefferies JL, Liang JF, Denfield SW, Dreyer WJ, Mott AR, Grenier MA, Dickerson HA, Price JF, Towbin JA, Ou CN, Chang AC. Concentrations of brain natriuretic peptide in the plasma predicts outcomes of treatment of children with decompensated heart failure admitted to the Intensive Care unit. Cardiology in the young. 2007;17:397–406. doi: 10.1017/S1047951107000601. [DOI] [PubMed] [Google Scholar]


