Abstract
Robust and responsive surveillance systems are critical for malaria elimination. The ideal information system that supports malaria elimination includes: rapid and complete case reporting, incorporation of related data, such as census or health survey information, central data storage and management, automated and expert data analysis, and customized outputs and feedback that lead to timely and targeted responses. Spatial information enhances such a system, ensuring cases are tracked and mapped over time. Data sharing and coordination across borders are vital and new technologies can improve data speed, accuracy, and quality. Parts of this ideal information system exist and are in use, but have yet to be linked together coherently. Malaria elimination programs should support the implementation and refinement of information systems to support surveillance and response and ensure political and financial commitment to maintain the systems and the human resources needed to run them. National malaria programs should strive to improve the access and utility of these information systems and establish cross-border data sharing mechanisms through the use of standard indicators for malaria surveillance. Ultimately, investment in the information technologies that support a timely and targeted surveillance and response system is essential for malaria elimination.
Introduction
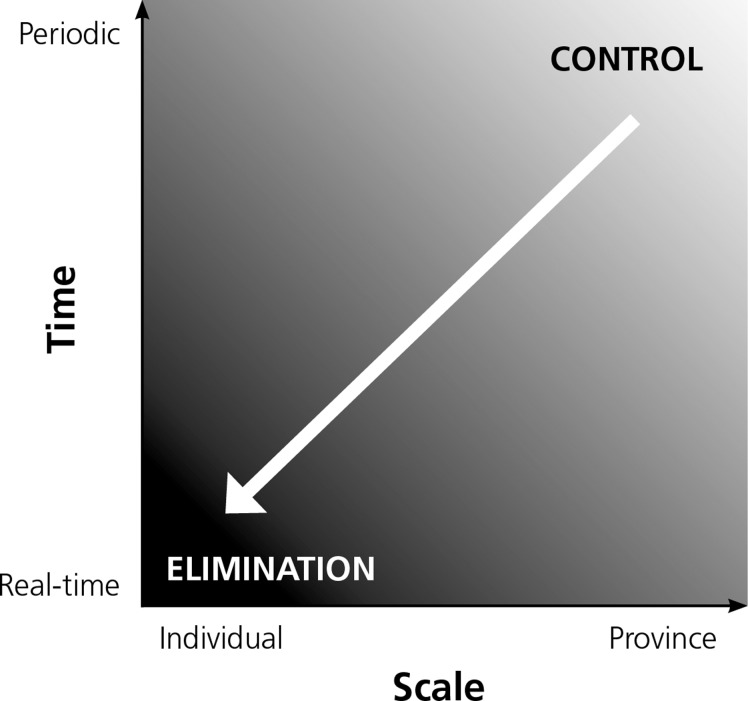
Robust and responsive information systems are critical for successful malaria control and elimination.1–5 In elimination settings, surveillance must be an intervention where data collection, analysis, output, and response occur quickly to identify symptomatic and asymptomatic cases, prevent onward transmission, and reduce vectorial capacity. The best way to ensure that this occurs rapidly and efficiently is to work with information systems designed to support malaria surveillance and response. Specifically, in an elimination setting, case reporting needs to shift from being periodic and aggregated at the district or provincial level to real-time reporting of individual geo-located cases (Figure 1).
Figure 1.
Changes in the spatial and temporal scale of malaria surveillance and response in the shift to elimination (Modified from Cao and others6).
Technologies that support elimination surveillance can facilitate many essential elements such as real-time or rapid reporting and case and intervention mapping. Here we describe the characteristics of an ideal malaria elimination information system that has the capacity to identify individual cases, analyze and share information, and stimulate real-time action to prevent onward transmission.
This article is one in a series of four that is intended to guide malaria elimination program decision making. These articles draw on both published and unpublished literature and qualitative data gathered from key informant interviews. This article offers specific recommendations to guide the choice of information systems in elimination settings.
Methods
These findings were informed by published and grey literature. In addition to a review of publications specific to malaria elimination and other disease eradication, the literature search included combinations of the following topics and search terms: chagas, cross-border data sharing, data management, dengue, geospatial, guidelines, influenza, information systems for health, polio, imported malaria, integrated disease surveillance, inter-country collaboration, malaria elimination, monitoring and evaluation, outbreak alert, rapid reporting, sentinel surveillance, surveillance, World health Organization (WHO), yellow fever, zero reporting, and specific country programs mentioned by key informants. A total of 157 documents were identified and reviewed. The authors conducted 21 key informant interviews with malaria field experts, surveillance specialists, geographic information systems (GIS) experts, information technology experts, and members of malaria control and elimination programs, as well as experts in the control and eradication of diseases other than malaria.
Characteristics of an ideal elimination information system
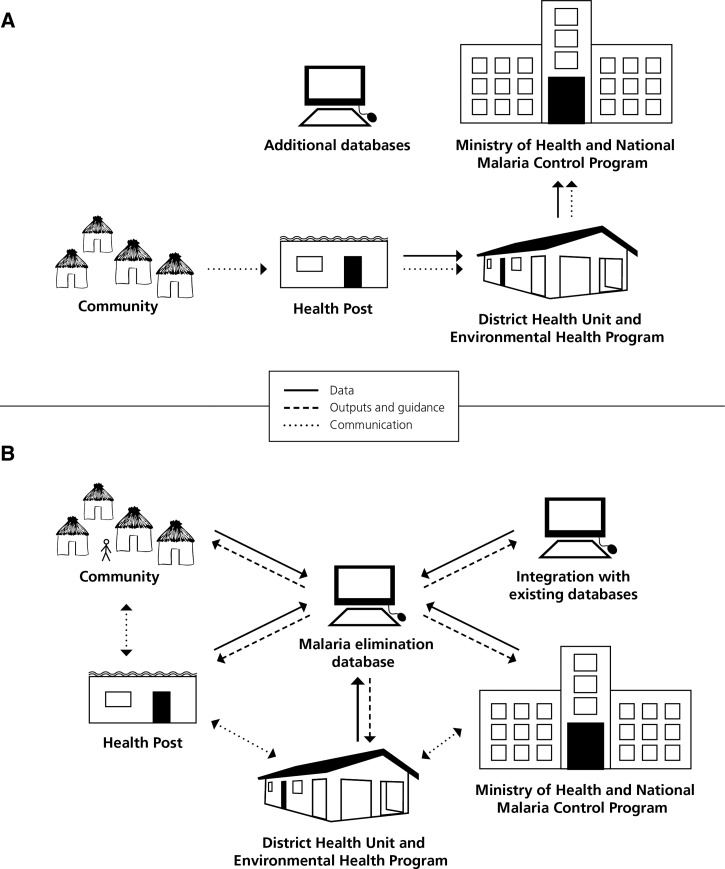
Surveillance for malaria control aims to estimate the burden of malaria and inform population-level programs, whereas surveillance for malaria elimination strives to capture and respond to every malaria case.7 An ideal malaria elimination information system to support surveillance and response activities collects and transmits data about cases and program activities swiftly, incorporates data from other existing surveillance systems in real time and analyzes data to inform rapid response strategies (Figure 2).8
Figure 2.
Malaria surveillance systems. (A) Traditional malaria surveillance. In a traditional malaria surveillance system, data movement is unidirectional, and outputs do not inform community-level response. Additional data are not incorporated into a central database. (B) Ideal malaria surveillance. In an ideal malaria surveillance system, all levels contribute data to a central database, the central database provides data analysis and guidelines to all levels, and communication is bi-directional.
To achieve these aims, the system requires several key features as follows:
Rapid and complete reporting.
Data should be collected from the lowest level and in the most direct manner possible.9 This includes data collected passively at health facilities and in communities from community health workers as well as through active case detection during case investigations or screening activities and intervention data from district-level malaria programs. Consensus on key indicators, or minimum essential data, that a malaria elimination information system needs to capture is fundamental. Complete, timely reporting is an essential element of a malaria elimination surveillance system. Methods for capturing data must be rapid, locally appropriate, feasible, and sustainable by the malaria program. Malaria should be made a notifiable disease once incidence is low enough that malaria surveillance teams can investigate and report every individual case. Instituting a “zero reporting” policy that requires all reporting sites to communicate the number of cases tested and detected regularly, regardless of whether a new case has been detected. This policy, as outlined in the WHO's surveillance guidelines for poliomyelitis and Japanese encephalitis, will further improve data quality.10 Zero reporting reduces missing data and helps identify locations where reporting is irregular or incomplete.11
Incorporation of additional data.
Incorporating data sources external to the malaria program, and even the health system, into the malaria elimination information system will improve decision making. For example, the use of census data can provide population denominators, climate and land use data warn of potential areas at risk of outbreaks, and population movement information may indicate the need for a rapid shift in resource targeting. The malaria elimination information system must be flexible enough to receive information from and export to external databases to ensure data can be used by and shared among multiple stakeholders.
Accessible data storage and management.
Data should be accessible to key members of the health system from the central level down to the implementation units in the communities.9,12,13 The database should be appropriate for local conditions, taking into account existing community-level assets and skills, as well as access to power and equipment repair.14,15 In some locations, a cloud-based database will make the most sense because anyone with Internet access and administrative clearance can submit and obtain data in real time. However, in locations where reliable Internet access is unavailable, local databases that feed into a central server may help ensure that work can continue during Internet outages. Regardless of the type of data storage used, guidelines for timeliness of reporting must be established.6,16 Data storage and management systems must be computer based and should include a plan for ongoing maintenance.9
Automated and expert analysis.
A malaria elimination information system should include automated data analysis to ensure timely outputs and expert analysis for policy and programming decisions.9,17 Automation is vital because a malaria elimination information system must receive and analyze data and output results quickly to identify threats such as outbreaks, inform responses, and monitor the functioning of the whole elimination program. It is essential to incorporate technical assistance and capacity building for malaria program staff at all levels to ensure the database is used effectively. Malaria experts working where the surveillance system is implemented, including in the field, should participate in analysis and interpretation of outputs to ensure that recommended interventions are feasible and reflect local conditions.
Expert analysis can be used to model the expected impact of different combinations of interventions and has been used in other contexts to improve complex processes and systems and decision making.18 The models can use data from the surveillance system to help determine which interventions should be used and in what manner to ensure the most impactful, efficient, and cost-effective response.19,20 The impact of the response can be captured by the surveillance system and can inform further iterative changes to the interventions. Geospatial modeling was conducted in Haiti to produce malaria risk maps as part of an assessment of the feasibility of malaria elimination.21 Because of the unreliability of passive surveillance data, parasite prevalence data were used to better understand the temporal and spatial distribution of malaria. From this work, optimal interventions and treatment strategies for various populations and locations were suggested.
Customized output and feedback.
An ideal malaria information system should automatically generate outputs tailored to the level of the health system that receives them, including visualizations of analyzed data, work task lists, and reports for internal use, external organizations, and donors. Once data are analyzed, visualizing results is essential to effectively share the information. Outputs to the lowest levels should be understandable and directly useful for operational responses, for example, including information that directs the surveillance officer to the household or health facility of the case. Monitoring and evaluation of the outputs are necessary to measure the value added of the malaria elimination information system itself and understand how the system can be improved.
Targeted response.
Response to malaria elimination information system outputs needs to be timely, effective, and targeted.9,13,22 At the local level, once health staff receive outputs, including a work task list, they must take immediate action.23,24 This list may include households to be screened for infection, receive preventive interventions such as indoor residual spraying with insecticide, and receive health education. As the workers are implementing their task list, they can also collect data that should be uploaded into the information system that will further inform the intervention strategy, such as coverage and use of interventions, and the occupational risk factors of the people within the target area. The uploading of data from the response activity acts to inform the information system that the activity has taken place operating as a tool for monitoring and evaluation. Findings from the review and key informant interviews highlighted that connecting outputs from the information system to action is the weakest element of existing systems.
Description of existing Information systems
Currently, few malaria information systems exist that can collect, store, analyze, and provide feedback to implementers based on real-time information. Many existing systems are limited in geographic coverage, do not collect sufficient data to inform rapid response, or are not connected to decision making. While no existing malaria information system contains all the elements listed above, below are examples of existing systems that contain elements of what an ideal system might look like and offer valuable lessons on how to conduct surveillance that can lead to effective responses. Comparisons of these and other systems are highlighted in Table 1.
Table 1.
Existing surveillance systems for malaria elimination
| Country | System description | Data capture | Outputs | Strengths | Challenges |
|---|---|---|---|---|---|
| Cambodia | MIS is a stand-alone system developed to assess malaria transmission and intervention coverage.25 Two additional pilot systems | Passive Case Detection case notification | MIS: Automatically generated report including tabular summaries, graphics and mapping to village level26 | MIS: | Uncaptured private, migrant, military sectors |
| D0AS Pf cases | MIS: District level data reported monthly, including species, severe malaria, cases, deaths | D0AS: Real-time SMS alert to Provincial Health Department and National Malaria Center. Day-28 follow-up reminder is sent to the same plus health center management | Covers all endemic areas | Most data aggregated monthly, challenge to get real-time data | |
| D3AS Day 3 positive malaria smears to identify resistance | D0AS: Health staff send SMS for Pf cases from pilot areas | D3AS: Real-time SMS when parasites remain by Day 3 | Tracks severe malaria, deaths | Inconsistent decision making and response based on available data | |
| Population covered: > 3M | D3AS: Only includes Pf cases parasitemic after three days of treatment in areas of artemisinin-resistance | Malaria incidence and intervention coverage to village level | Does not capture time-to-case reporting, or intervention quality | ||
| Automatically generated monthly bulletin | Case follow-up challenges | ||||
| Pilot D0AS and D3AS | No mapping to household or where case acquired | ||||
| SMS and Internet-based notification systems | |||||
| Integrated with MIS | |||||
| China | Two integrated web-based systems: febrile illness reporting and focus investigation and intervention tracking. Data stored at the National Centers for Disease Control and Prevention.6,27 | PCD case notification: Data entered within 24 hours. Data include date, facility, reporting person, patient info and diagnostic result with method and treatment | SMS alerts | Web-based system integrated with reportable diseases system | Mobile technology not integrated |
| Population covered: > 1.3B | Monthly MoH report, tabular summary results, graphics and mapping | Data fed into HMIS | Limited baseline data | ||
| “1-3-7 strategy” time tracking to case notification (one day), case investigation (three days), completed interventions (seven days) | Very little missing data | Does not capture new interventions or intervention quality | |||
| Rapid case reporting | No mapping to household or where case acquired | ||||
| Diagnosis is confirmed by microscopy and PCR | |||||
| “1-3-7 strategy” is easy to use and understand | |||||
| Solomon Islands/Vanuatu | SDSS.17,35 Data are stored in a relational database, using local, provincial and nationally based servers (three levels for backup). | PCD case notification: Health facility calls provincial center within 48 hours. | Real-time case reporting | SDSS includes extensive baseline data28 | Mobile technology not integrated |
| Population covered: > 90 k, implemented in four island provinces | Frontline and active case detection planning by household, follow-up list of households that did not receive intervention | Rapid case reporting | Inconsistent decision making and response | ||
| Tabular output, spatial analysis, graphics, and mapping, including foci classification | Automated GIS-based queries with high-resolution mapping | Does not capture time-to-case reporting, or intervention quality | |||
| Generates lists to support targeted action at the household level | Human resource constraints | ||||
| Readily adaptable to other locations or systems | No mapping to where case was acquired | ||||
| Swaziland | HMIS, IDNS for 15 reportable diseases, and MSDS for case investigation and interventions.16,29,36 | PCD case notification: RDT or microscopy-confirmed malaria cases dictated through a toll-free hotline. Data entered on a central server, surveillance agent receives an SMS with date, facility, reporting person, patient info and case number to conduct case investigation and intervention. | IDNS: Toll-free hotline resulting in SMS to surveillance agent | Integrated with notifiable disease reporting system | Relatively low reporting completeness to IDNS |
| Population covered: 1.2M | MSDS: Monthly tabular and graphic summary, mapping to household. Maps of cases investigated, locations of positive cases, IRS, ITNs, breeding sites, risk maps, households screened, or remaining. | Web-based system using mobile technology | Low case reporting from private sector facilities | ||
| Free mobile reporting | Does not capture time-to-case reporting or intervention quality | ||||
| Entire country covered | No mapping to where case was acquired | ||||
| Simple, rapid case notification | |||||
| Temporal–spatial analysis of case distribution | |||||
| Thailand | Stand-alone, web-based system. Data storage is in a database at Mahidol University. GPS-enabled tablets for patient follow-up, data captured in same server. | PCD case notification: Case data entered at malaria clinic level within 24 hours. Data include date, facility, reporting person, patient info, diagnostic result with method and foci classification.30 | Pf case alerts to malaria clinic staffs' tablets within 24 hours | Web-based system with mobile technology being integrated | Hospital-based cases in a separate system |
| Population covered: > 21M | Tablet-based follow-up form for directly observed therapy and resistance monitoring | Implemented in large regions, covering all areas of multi-drug resistance | Challenges with migrant and cross-border follow-up | ||
| Monthly MoH report, tabular summary, graphics, maps, with mapping to Pf case household and likely case location.31 | Rapid case reporting | More baseline data needed, such as intervention coverage and forest sleeping locations | |||
| Captures DOT | No time to case reporting or intervention quality | ||||
| Captures Pf resistance | |||||
| Zambia | DHIS2 is a web-based health information system. Data storage and mobile phones linked to the same database.32,33 | PCD case notification: urban and rural health staff report weekly by mobile phone. Data include clinic visits, clinical cases, RDT-tested and positive cases, microscopy-tested and positive cases, ACT and RDT stock tracking. CHWs report cases monthly by mobile phone.33 | Regular reports, with online access to data in real-time | Open source free web-based system fully integrated with HMIS | Case data not reported to DHIS2 in real-time |
| Population covered: > 6M | Graphs created and provided in real time to mobile phones or computers, summarizing case reporting and stock data, with summary data from all areas, reporting to the facility | Tables, charts and maps shared with all users with online dashboard | Does not capture time to case reporting or intervention quality | ||
| Maps, graphs display village, clinic-level malaria incidence | Mobile technology fully integrated | Remains to be determined if DHIS2 can support full malaria elimination surveillance system to household level | |||
| Timeliness and completeness of data reporting tracked | |||||
| Zanzibar, Tanzania | Integrated system combining Coconut Surveillance and MCN. MCN includes rapid reporting and analysis, outputs with geo-location of cases, through Coconut Surveillance. Cases reported to health staff via SMS. Coconut uses data to guide household oriented index case follow up. | PCD case notification: | MCN: Real-time case reporting via Coconut Surveillance, monthly MoH reports. Tabular summary results, graphics and mapping to the village level. | MCN and Coconut are an integrated SMS-based system and tablet web-based system | Cases from extensive private sector not captured |
| Population covered: ∼1.3M | Public health unit staff send an SMS for each positive case. Data include all-cause visits, malaria tested/positive cases and age. | Coconut: Real-time tabular summary results, graphics, and detailed mapping to the household level. Real-time tracking of case follow-up and new interventions. | Mobile technology fully integrated | Limited capture of baseline data | |
| Coconut Surveillance notifies malaria officers of cases immediately via SMS. Patient and household follow-up with GPS enabled tablet. | Rapid case reporting | Does not currently capture intervention quality | |||
| Real-time tabular output of key variables makes it easy for management to track progress real time | No mapping to where case was acquired | ||||
| MEEDS data are used to calculate supply orders | Denominator (population) data not captured with Coconut |
D0AS = Day 0 Alert System; D3AS = Day 3 Alert System; DOT = directly observed therapy; HMIS = Health Management Information System; GIS = geographic information systems: MCN = malaria case notification; IDNS = Immediate Disease Notification System; MIS = Malaria Information System; MoH = Ministry of Health; MSDS = Malaria Surveillance Database System; Pf = Plasmodium falciparum; PCR = polymerase chain reaction; SDSS = Integrated Spatial Decision Support System; SMS = short message service.
China.
The strength of the Chinese Information System for Disease Control and Prevention is its timeliness, ease of reporting, and intuitive 1-3-7 monitoring framework. The 1-3-7 framework dictates that malaria cases be reported within one day, case investigation must occur within three days, and foci investigation and increased prevention measures implemented within 7 days.6 The recommended responses vary by the levels of endemicity and risk, with “active and passive surveillance, with particular attention to mobile populations,” in areas with higher incidence, “passive surveillance in the transmission season and active surveillance targeting transmission foci” in zones with seasonal malaria, and “intensified surveillance and response” in border areas.34
Solomon Islands and Vanuatu.
Automated analyses and customized outputs, as well as the potential to guide targeted, rapid response, are the strengths of the Spatial Decision Support System (SDSS), implemented in Vanuatu and the Solomon Islands.35 This GIS uses the time and place of malaria cases and intervention coverage to automatically classify areas according to risk and then generate specific response recommendations. The information system creates automated maps of households, including coverage, incidence, and additional geographic and entomologic data. Work task lists are generated for intervention and case management teams for each geo-located house they should visit.
Swaziland.
The strengths of Swaziland's malaria information system include rapid case reporting through the Immediate Disease Notification System (IDNS), a surveillance system integrated with the reportable disease system, and surveillance outputs that are rapidly relayed to a team that can initiate a response.36 The health facility staff members call a toll-free number to report cases to the IDNS, which then sends multiple short message service (SMS) messages with case details to the local malaria program manager and the surveillance team, who investigate within 48 hours. Weekly goals and feedback are provided to surveillance officers to improve coverage and speed of follow-up and screening.
Zanzibar.
The strengths of Zanzibar's Malaria Case Notification (MCN) system are its rapid reporting and outputs detailing geo-location of cases.37 Through MCN, cases are reported in real time and then a tablet-based platform alerts district malaria officers to follow-up, guiding which households are visited to conduct reactive case detection. In this system, surveillance is an intervention, where mobile reporting allows the collection of data in real time that are used to guide a local response.15,38
Linkage between regional and global information systems
Ideally, national malaria control and elimination information systems would link seamlessly with related regional and global structures, prioritizing cross-border intelligence sharing information regarding transmission hotspots, outbreaks, and human movement. This would lead to appropriate allocation of national and regional resources and timelier targeted action. However, database linkage between countries and within regions is difficult due to the sensitivity of sharing and nonstandardized collection of data. As more countries move toward malaria elimination and cross-border and regional malaria elimination initiatives are implemented, sharing of data should become a priority. In an effort to facilitate data sharing for malaria control, WHO now coordinates a “situation room” that is focused on the 10 African countries with the highest malaria burden, bringing country representatives together virtually every 2 weeks to discuss stock control, funding issues, and to track current and potential outbreaks. Similar regional situation rooms such as the data sharing hub being developed by the Emergency Response to Artemisinin Resistance in the Greater Mekong Subregion could facilitate data sharing and coordination among malaria-eliminating countries.
Recommendations
To build a robust and action-oriented malaria elimination information system, a number of key issues require consideration.
Reporting.
In countries pursuing malaria elimination, when incidence is low enough, rapid reporting of cases should be implemented. Once in the malaria elimination phase reporting must be required by law, preferably within a defined period, and appropriately incentivized in all sectors caring for malaria patients, including private sector health providers and militaries. Reporting should include negative diagnostic test results and zero case reporting.
Database management.
The malaria elimination database must be manageable by the National Malaria Control Program (NMCP). A malaria elimination surveillance system must provide a framework to guide strategic decision making and support the effective management, coordination, and implementation of interventions. All levels of the malaria control program, from the community to the national level, should receive information from the system. Expert epidemiological and information technology oversight of the system is crucial requiring human resources to support data analysis, including surveillance database managers and epidemiologists who can program database queries, analyze, and interpret data.
Information and results feedback.
An effective information system must feed analyzed data back to those executing the malaria program, particularly at the community level. In this review, we found few examples of systems that rapidly shared analyzed surveillance information, which could contribute to more rapid and complete responses. For surveillance to function as an intervention, real-time feedback and effective responses are essential. Global stakeholders must take note of this weakness and target investments to improve appropriate rapid feedback from malaria information systems that lead to effective responses.
Technology.
Locally appropriate technologies, such as mobile phones and web-based systems, can help support data quality improvements and reporting timeliness. Most importantly, comprehensive spatial decision support systems that incorporate GIS are invaluable, as they enable mapping of cases and interventions, automated foci identification, and targeted responses.35,39
Data sharing and commitment.
Real-time sharing of standardized malaria data across borders has the potential to contribute to malaria elimination. A key element of malaria elimination programs is rapid and appropriate response to malaria cases. Standardized and streamlined methods and indicators will improve reporting and decision making. Interventions will need to be adapted to the location and population; however, there is an urgent need for generic and adaptable standard operating procedures on which NMCPs can base their surveillance and response strategies. The effective implementation of regional collaborations within malarious regions looking to eliminate may be crucial for the success of national and regional malaria elimination. Currently there are few functioning cross-border malaria elimination collaborations. Ideally, surveillance systems would be unified across countries and would incorporate information from militaries who liaise with government and civilian authorities. Harmonizing existing surveillance systems will require both political and financial commitments in short term and long term. In short-term, commitment is needed to bring stakeholders together to develop political and financial capital for malaria elimination surveillance and information systems. Malaria elimination is a long-term strategy, therefore, commitment is needed to maintain a cadre of workers who can work with the software and adapt it to fit changing circumstances.
Many new technology developments to improve surveillance for malaria elimination appear attractive for investment. However, an investment in technologies is not a panacea; a surveillance system is only as good as its implementation. An excellent information system should be at the core of malaria elimination programs to ensure that all cases are detected and responded to in an effective and timely manner. Investment in robust, response-focused systems is essential to achieve malaria elimination.
ACKNOWLEDGMENTS
We acknowledge with thanks the contributions of the people who have participated in the collection and exploration of information contained in this report: Ahmed Mohammad Abdalla (National Malaria Control Program, Abu Dhabi, United Arab Emirates), Patrick Blair (Naval Medical Research Center-Asia, Singapore), Bradley Ringeisen (Defense Threat Reduction Agency, Portsmouth, VA), Daniel Bridges and Anna Winters (Akros Global Health, Lusaka, Zambia), Keith Carter (Pan American Health Organization, Washington, DC), Richard Cibulskis and Raman Velayudhan (World Health Organization [WHO], Geneva, Switzerland), Rajeev Colaco, Richard Reithinger and Gordon Cressman (RTI International, Washington, DC), Michael Coleman (Liverpool School of Tropical Medicine, Liverpool, UK), Peggy D'Adamo (USAID, Washington, DC), Arantxa Roca (Malaria Consortium, Phnom Penh, Cambodia), Mitiku Aychiluhim Damtew, Kaddu Ssentamu Simon and Ella Watson-Stryker (WHO, Freetown, Sierra Leone), Eric Hale (Solomon Islands Ministry of Health [MoH], Honiara, Solomon Islands), Herdie Hizon (Philippines MoH, Manila, Philippines), Eduardo Jezierski, Dennis Israelski and Channe Suy (Innovative Support To Emergencies Diseases and Disasters [InSTEDD], Sunnyvale, CA), Jun Cao (Jiangsu Institute of Parasitic Diseases, Wuxi, China), Jaranit Kaewkungwal and Amnat Khamsiriwatchara (Mahidol University, Bangkok, Thailand), Gerard Kelly (University of Queensland, Brisbane, Australia), Jirapat Ketkaew, Apinya Niramitramtipong, Duangdeun Puangmanee and Wittaya Saipromsut (Thailand MoH, Bangkok, Thailand), Dysoley Lek and Siv Sovannaroth (Cambodia MoH Phnom Penh, Cambodia), Adam Liederman (Fio Corporation, Toronto, Canada), John Miller and Rick Steketee (Program for Appropriate Technology in Health [PATH]: The Malaria Control and Elimination Partnership in Africa [MACEPA], Seattle, WA), Mwiyini I. Msellem (Zanzibar Malaria Elimination Program, Zanzibar City, Unguja, Zanzibar), Rose Nani Mudin (Malaysia MoH, Kuala Lumpur, Malaysia), Thang Duc Ngo (National Institute of Malariology Parasitology and Entomology, Hanoi, Vietnam), Nyasatu Ntshalintshali (Clinton Health Access Initiative [CHAI], Mbabane, Swaziland), Elvieda Saraiwati, Budi Pramono and Mienerva Theodora (Indonesia MoH, Jakarta, Indonesia), Chris Schwabe (Medical Care Development International, Silver Spring, MD), David Sintasath (Family Health International [FHI] 360, Washington, DC), Mark Smolinski and Jennifer Olsen (Skoll Global Threats Fund, Palo Alto, CA), Jeff Tackle and Kathleen Poer (Abt Associates, Bethesda, MD), Marcel Tanner (Swiss Tropical and Public Health Institute, Basel, Switzerland), and Allison Tatarsky (CHAI, Gaborone, Botswana). We acknowledge the participants of the Asia Pacific Malaria Elimination Network Surveillance and Response Thematic Group for their insightful discussions on the program requirements for malaria elimination surveillance systems.
Disclaimer: The following individuals reviewed the report and provided important assistance and feedback: Chris Cotter (Global Health Group, University of California San Francisco, San Francisco, CA), Gerard Kelly (University of Queensland, Brisbane, Australia), Richard Reithinger (RTI International, Washington, DC), Arantxa Roca (Malaria Consortium, Phnom Penh, Cambodia), Chris Schwabe (Medical Care Development International, Silver Spring, MD), David Sintasath (FHI 360, Washington, DC) and Rick Steketee (PATH: MACEPA, Seattle, WA).
Footnotes
Financial support: This background article is a rapid synthesis of current evidence commissioned and funded by the Bill and Melinda Gates Foundation.
Authors' addresses: Colin Ohrt, Malaria Elimination Initiative, Global Health Group, University of California, Hanoi, Vietnam, E-mails: colin.ohrt@ucsf.edu or colin8994@gmail.com. Kathryn W. Roberts, Hugh J. W. Sturrock, Jennifer Wegbreit, and Roly D. Gosling, Global Health Group, University of California, San Francisco, CA, E-mails: kathryn.roberts@ucsf.edu, hugh.sturrock@ucsf.edu, jennifer.wegbreit@ucsf.edu, and roly.gosling@ucsf.edu. Bruce Y. Lee, Johns Hopkins Bloomberg School of Public Health, Baltimore, MD, E-mail: brucelee@jhu.edu.
References
- 1.Feachem RG, Phillips AA, Targett GA, Snow RW. Call to action: priorities for malaria elimination. Lancet. 2010;376:1517–1521. doi: 10.1016/S0140-6736(10)61500-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tanner M, de Savigny D. Malaria eradication back on the table. Bull World Health Organ. 2008;86:82. doi: 10.2471/BLT.07.050633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Alonso PL, Brown G, Arevalo-Herrera M, Binka F, Chitnis C, Collins F, Doumbo OK, Greenwood B, Hall BF, Levine MM, Mendis K, Newman RD, Plowe CV, Rodríguez MH, Sinden R, Slutsker L, Tanner M. A research agenda to underpin malaria eradication. PLoS Med. 2011;8:e1000406. doi: 10.1371/journal.pmed.1000406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hay SI, Smith DL, Snow RW. Measuring malaria endemicity from intense to interrupted transmission. Lancet Infect Dis. 2008;8:369–378. doi: 10.1016/S1473-3099(08)70069-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nájera JA, González-Silva M, Alonso PL. Some lessons for the future from the Global Malaria Eradication Programme (1955–1969) PLoS Med. 2011;8:e1000412. doi: 10.1371/journal.pmed.1000412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cao J, Sturrock HJW, Cotter C, Zhou S, Zhou H, Liu Y, Tang L, Gosling RD, Feachem RGA, Ga Q. Communicating and monitoring surveillance and response activities for malaria elimination: China's “1-3-7” Strategy. PLoS Med. 2014;11:e1001642. doi: 10.1371/journal.pmed.1001642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.The malERIA Consultative Group on Monitoring, Evaluation, and Surveillance The malERA Consultative Group on Monitoring, E. A research agenda for malaria eradication: monitoring, evaluation, and surveillance. PLoS Med. 2011;8:e1000400. doi: 10.1371/journal.pmed.1000400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.M'ikanatha NM, Lynfield R, Julian KG, Van Beneden CA, de Valk H. Infectious disease surveillance: a cornerstone for prevention and control. In: M'ikanatha NM, Lynfield R, Beneden CAV, de Valk H, editors. John Wiley and Sons Ltd; 2013. pp. 1–20.http://onlinelibrary.wiley.com/doi/10.1002/9781118543504.ch1/summary Available at. [Google Scholar]
- 9.World Health Organization and Global Malaria Programme . Disease Surveillance for Malaria Elimination an Operational Manual. Geneva, Switzerland: World Health Organization; 2012. [Google Scholar]
- 10.World Health Organization . WHO Recommended Standards for Surveillance of Selected Vaccine-Preventable Diseases. Geneva, Switzerland: World Health Organization; 2008. http://apps.who.int/iris/handle/10665/42510 Available at. [Google Scholar]
- 11.Harris BN, Dürrheim DN, Ogunbanjo GA. Polio eradication—the validity of surveillance indicators. Trop Med Int Health. 2003;8:386–391. doi: 10.1046/j.1365-3156.2003.01048.x. [DOI] [PubMed] [Google Scholar]
- 12.Van Beneden CA, Arvay M, Thamthitiwat S, Lynfield R. Active, population-based surveillance for infectious diseases. In: M'ikanatha NM, Lynfield R, Beneden CAV, de Valk H, editors. Infectious Disease Surveillance. John Wiley and Sons Ltd; 2013. pp. 93–108.http://onlinelibrary.wiley.com/doi/10.1002/9781118543504.ch8/summary Available at. [Google Scholar]
- 13.Sahal N, Reintjes R, Aro AR. Review article: communicable diseases surveillance lessons learned from developed and developing countries: literature review. Scand J Public Health. 2009;37:187–200. doi: 10.1177/1403494808101179. [DOI] [PubMed] [Google Scholar]
- 14.Breman JG, Alilio MS, Mills A, Breman JG, Alilio MS. Conquering the Intolerable Burden of Malaria: What's New, What's Needed: A Summary. 2004. http://www.ncbi.nlm.nih.gov/books/NBK3750/ Available at. [PubMed] [Google Scholar]
- 15.Zhou X-N, Bergquist R, Tanner M. Elimination of tropical disease through surveillance and response. Infect Dis Poverty. 2013;2:1. doi: 10.1186/2049-9957-2-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Novotny, J. Swaziland Malaria Elimination Update 2012–2013 2013 [Google Scholar]
- 17.Kelly GC, Tanner M, Vallely A, Clements A. Malaria elimination: moving forward with spatial decision support systems. Trends Parasitol. 2012;28:297–304. doi: 10.1016/j.pt.2012.04.002. [DOI] [PubMed] [Google Scholar]
- 18.Operations Research Merriam-Webster. http://www.merriam-webster.com/dictionary/operations research Available at.
- 19.Hamrock E, Paige K, Parks J, Scheulen J, Levin S. Discrete event simulation for healthcare organizations: a tool for decision making. J Healthc Manag Am Coll Healthc Exec. 2013;58:110–124. discussion 124–125. [PubMed] [Google Scholar]
- 20.Gray M. Value: operations research and the new health care paradigm. Oper Res Health Care. 2012;1:20–21. [Google Scholar]
- 21.Clinton Health Access Initiative Malaria Elimination in Haiti 2013 [Google Scholar]
- 22.The Roll Back Malaria Partnership . Eliminating Malaria: Learning from the Past, Looking Ahead. Geneva, Switzerland: World Health Organization; 2011. [Google Scholar]
- 23.World Health Organization WHO|Malaria Programme Reviews: A Manual for Reviewing the Performance of Malaria Control and Elimination Programmes. 2010. http://www.who.int/malaria/publications/atoz/whomprmalariaprogramperformancemanual/en/ Available at.
- 24.World Health Organization WHO|Malaria Case Management: Operations Manual. 2009. http://www.who.int/malaria/publications/atoz/9789241598088/en/ Available at.
- 25.Malaria Consortium, National Center for Parasitology, Entomology and Malaria Control, World Health Organization Moving Towards Malaria Elimination: Tools for Strengthening Malaria Surveillance in Cambodia. 2011. http://www.malariaconsortium.org/userfiles/file/Resistance-Resources/Surveillance%20Tools%20-%20Moving%20Towards%20Malaria%20Elimination.pdf Available at.
- 26.National Center for Parasitology Entomology and Malaria Control. Cambodia Malaria Bulletin Jan–Jun 2013. 2013. http://www.cnm.gov.kh/userfiles/file/Buletin/Malaria%20Bulletin%20Jan-Jun%202013_23Jul2013.pdf Available at.
- 27.Qi G. 1, 3, 7 New Malaria Elimination Strategy Implementation in China [Google Scholar]
- 28.Kelly GC, Hii J, Batarii W, Donald W, Hale E, Nausien J, Pontifex S, Vallely A, Tanner M, Clements A. Modern geographical reconnaissance of target populations in malaria elimination zones. Malar J. 2010;9:289. doi: 10.1186/1475-2875-9-289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hsiang MS, Hwang J, Kunene S, Drakeley C, Kandula D, Novotny J, Parizo J, Jensen T, Tong M, Kemere J, Dlamini S, Moonen B, Angov E, Dutta S, Ockenhouse C, Dorsey G, Greenhouse B. Surveillance for malaria elimination in Swaziland: a national cross-sectional study using pooled PCR and serology. PLoS One. 2012;7:e29550. doi: 10.1371/journal.pone.0029550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Thailand Bureau of Vector-borne Disease National Monitoring and Evaluation Plan for Malaria Control and Elimination in Thailand, 2011–2016. 2010. http://whothailand.healthrepository.org/bitstream/123456789/1443/1/Thailand%20Malaria%20Plan.pdf Available at.
- 31.Biophics and Thailand Malaria Control and Elimination Program . Thailand—The Single Stream Funding—Malaria. http://www.biophics.org/malariaR10/ Available at. [Google Scholar]
- 32.Zambia Ministry of Health Zambia DHIS2 Rapid Reporting Web Dashboard. http://dhis.co.zm/R/dash?&organisationunitid=3829 Available at.
- 33.Littrell M, Miller JM, Ndhlovu M, Hamainza B, Hawela M, Kamuliwo M, Hamer DH, Steketee RW. Documenting malaria case management coverage in Zambia: a systems effectiveness approach. Malar J. 2013;12:371. doi: 10.1186/1475-2875-12-371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Yang G-J, Tanner M, Utzinger J, Malone JB, Bergquist R, Chan EYY, Gao Q, Zhou X-N. Malaria surveillance-response strategies in different transmission zones of the People's Republic of China: preparing for climate change. Malar J. 2012;11:426. doi: 10.1186/1475-2875-11-426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kelly GC, Hale E, Donald W, Batarii W, Bugoro H, Nausien J, Smale J, Palmer K, Bobogare A, Taleo G, Vallely A, Tanner M, Vestergaard LS, Clements ACA. A high-resolution geospatial surveillance-response system for malaria elimination in Solomon Islands and Vanuatu. Malar J. 2013;12:108. doi: 10.1186/1475-2875-12-108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Cohen JM, Dlamini S, Novotny JM, Kandula D, Kunene S, Tatem AJ. Rapid case-based mapping of seasonal malaria transmission risk for strategic elimination planning in Swaziland. Malar J. 2013;12:61. doi: 10.1186/1475-2875-12-61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Moonen B, Cohen JM, Snow RW, Slutsker L, Drakeley C, Smith DL, Abeyasinghe RR, Rodrigues MH, Maharaj R, Tanner M, Targett G. Operational strategies to achieve and maintain malaria elimination. Lancet. 2010;376:1592–1603. doi: 10.1016/S0140-6736(10)61269-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Zanzibar National Malaria Control Program Malaria Elimination in Zanzibar. 2009. http://www.soperstrategies.com/countries/pemba/tanzania-library/files/EliminationZanzibar.pdf Available at.
- 39.Clements AC, Reid HL, Kelly GC, Hay SI. Further shrinking the malaria map: how can geospatial science help to achieve malaria elimination? Lancet Infect Dis. 2013;13:709–718. doi: 10.1016/S1473-3099(13)70140-3. [DOI] [PubMed] [Google Scholar]