Abstract
Greece has been officially malaria free since 1974. However, from 2009 to 2012, several locally acquired, cases of Plasmodium vivax malaria were detected, in immigrants and in Greek citizens. In this study, the antibody (Ab) response of Greeks and immigrants with documented malaria was initially assessed, followed by an Ab screening of Greeks and immigrant residents of local transmission areas. Of the 38 patients tested, 10.5% of Greeks and 15.7% of immigrants were positive 5–7 months after infection. Of the 1,019 individuals from various areas of Greece, including those of autochthonous transmission, 85 of the 721 (11.8%) immigrants were positive, whereas all 298 Greeks were negative. The rapid Ab titer decline observed is reasonable, given the non-endemic epidemiological setting. The seroepidemiological findings indicate that the local Greek population remains malaria naive and that at this point Greeks are unlikely to serve as reservoir for the infection of local mosquitoes.
Introduction
Of all the Plasmodium species that infect man, Plasmodium vivax has the widest geographic distribution, with an estimated 80–300 million cases occurring annually and almost 2.5 billion people living at risk of infection, most of which reside outside Africa.1 Large population densities and a very low prevalence of the Duffy negative phenotype render central and southeast Asia, the area most affected by P. vivax, by far.2,3 Recently, P. vivax has been recognized as a cause of serious morbidity and occasionally of severe, complicated and ultimately fatal disease, similar to Plasmodium falciparum.4 Additional challenges presented by P. vivax are its tendency to relapse, through the establishment of a dormant liver stage and its ability to complete its sporogony at lower ambient temperatures than P. falciparum, which enables it to extend its area of endemicity well into the temperate zones.5 These biological features often render P. vivax the first Plasmodium species to establish itself in a given focus and the last to be eradicated during control programs.
With increasing international travel, the importation of malaria by returning travelers and immigrants into non-endemic countries has become increasingly common.6–8 Thus, in areas with competent vector populations, the potential for reintroduction of the disease remains. In the United States, 63 outbreaks of locally acquired malaria have been documented from 1957 to 2003, comprising 156 cases.9 Plasmodium vivax was the predominant species involved, a fact that has been attributed to its tendency to relapse, and the high proportion of immigrants originating from P. vivax–endemic regions present in the area.9 Malaria has been eradicated in most of Europe since the middle of the last century. A few cases of suspected autochthonous transmission have been reported in the last decade, in Spain, Corsica, Germany, and The Netherlands.10–13
Greece was officially declared malaria free in 1974.14 Since then malaria cases have been mostly imported, but sporadic cases of locally acquired disease were occasionally reported.15,16 An increase in imported P. vivax malaria cases has been recorded in European countries.17,18 In Greece, from 2009 to 2012, 62 locally acquired, laboratory-confirmed cases of P. vivax malaria were reported to the Hellenic Center for Disease Control and Prevention (HCDCP), Athens, Greece, from various parts of the country.19,20
The longevity of acquired immunity to malaria remains an issue of debate and research.21 It is generally believed that acquired immunity to malaria wanes quickly and that antimalarial antibody (Ab) responses are generally short lived, in the absence of regular reinfection.22 Data from P. falciparum–endemic areas indicate that Ab prevalence can be used as a measure of transmission intensity in endemic countries, as the acquisition and maintenance of seropositivity requires cumulative exposure to the parasite, over several years.23 Other studies carried out in areas of stable transmission revealed a significant inter-household variation in anti–P. falciparum sporozoite response, despite comparable risk of exposure to infective mosquito bites. Age-related prevalence was also observed for anti–P. vivax sporozoite antibodies in an area of unstable transmission.24
To date, only a few studies have investigated the protective potential of these responses, focusing mainly on merozoite surface antigens (PvMSP1, 3, and 9, PvDBPs, PvRBPs) and the circumsporozoite protein (PvCSP).25 In this study, the Ab response of Greeks and immigrants with documented malaria infection during the previous 5–7 months was initially assessed. This pilot study was conducted to confirm the existence of antibodies in a population with known exposure to Plasmodium spp. and to evaluate the performance of the commercial enzyme-linked immunosorbent assay (ELISA) that was selected for screening. Following that, Greeks and immigrants residing in areas of Greece with locally acquired malaria transmission were screened for the detection of antimalarial antibodies, to determine the possible existence of seropositive and potentially asymptomatic Plasmodium carriers.
Materials and Methods
Population groups of the pilot study.
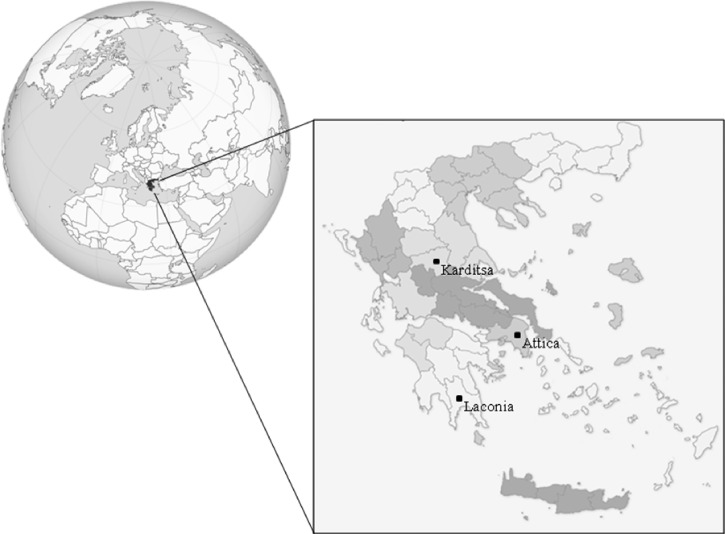
In March 2012, a single serum sample was collected in Laconia prefecture, south Peloponnese (Figure 1), from 38 patients who were microscopically and molecularly diagnosed positive for P. vivax malaria infection, 5–7 months after the acute malaria attack. The patients were divided into two groups: 1) Greek citizens without travel history to a malaria-endemic country (N = 19) and 2) immigrants, originating from Pakistan and Afghanistan (N = 19). A group of healthy Greek children (N = 50) were used as negative controls. Informed consent was obtained from all patients.
Figure 1.
A map of Greece highlighting the study areas (Laconia, Attica, and Karditsa prefectures).
Population groups of the screening study.
Consequently, from April to November 2012, a screening study was carried out in immigrants from malaria-endemic countries and in Greeks considered to be at high risk of the infection as a result of residence in areas of documented local malaria transmission and/or reduced access to health services, such as Romania. For the population screening 1,038 samples were collected from 1,019 individuals. Of those, 253 samples were collected from 248 asymptomatic Greek residents of Laconia; 735 samples from 721 asymptomatic immigrants residing in Laconia, Attica, and Karditsa; and 50 samples from the same number of healthy Greek blood donors residing in Attica without travel history to malaria-endemic areas in the last 3 years. Informed consent was obtained from all individuals. For Greek residents of Laconia, a convenient leftover sampling methodology was followed.26 The samples collected were stratified according to the population of the four villages with autochthonous malaria cases and the age group population. Private and public laboratories of the region were asked to provide the specific number per village and age group of leftover serum samples from individuals examined for chronic diseases or other noncommunicable diseases. The sampling methodology for immigrants was based on a convenient sample during the visits for fever screening at the immigrant's locations. In the Laconia region, the approximate number of immigrants was 900 and 582 (64.6%) who participated in the study. From Attica and Karditsa, the samples were collected during focus investigation of a malaria case.
ELISA.
Serum samples of the pilot and screening studies were analyzed using the Malaria-Ab ELISA (IBL International GMBH, Hamburg, Germany) that detects the presence of antibodies against recombinant circumsporozoite protein (CSP) and merozoite surface protein 1 (MSP1) of P. vivax and P. falciparum immobilized on 96-well plates. Plasmodium ovale and Plasmodium malariae were also detected because of the antigenic similarity between Plasmodium species. The test was carried out according to the manufacturer's instructions. In brief, 100 μL of each serum sample (diluted 1:100) was added to the wells and was incubated for 1 hour at 37°C in a moist chamber. After washing off unbound material, 100 μL of antihuman IgG and IgM antibodies conjugated to horseradish peroxidase was allowed to react with the immune complex for 30 minutes at room temperature. After removal of excess conjugate, 100 μL tetramethylbenzidine (TMB) substrate solution was added and the color was developed. The enzymatic reaction was stopped by addition of 100 μL of 0.2 M sulphuric acid. The optical density (OD) was quantified photometrically at 450 nm using the ChroMate Microplate Reader (Awareness Technology, Palm City, FL). The ODs were converted to units (U), using a formula provided by the manufacturer, based on the measured OD of the cutoff control. Results of > 11 U were considered positive, results of 9–11 U were regarded as borderline and results < 9 U were considered negative. Samples giving borderline results were characterized as equivocal. To normalize OD readings between different ELISA plates, one serum sample from a patient diagnosed with malaria and one from an individual with no history of malaria infection were used as counterbalancing controls in each plate.
The Ab index of each determination is obtained by dividing the OD value of each sample by the cutoff value. A negative reaction corresponds to an Ab index of 0.8 or less, a positive reaction to an Ab index of 1.0 or more, and an equivocal result to an Ab Index between 0.8 and 1.0. The test does not distinguish between IgG and IgM, or between antibodies to P. falciparum, P. vivax, P. ovale, and P. malariae.
Results
Sex and age distribution.
Of the 19 malaria cases in Greeks of the pilot study, 9 (47%) were male and 10 (53%) female. Their age ranged between 17 months and 80 years with a median age of 46 years. Of the 50 healthy Greek children, aged from 1 to 10 years, 23 (46%) were female and 27 (54%) male. All the foreign patients were men and their age ranged from 19 to 55 years (median age: 25 years). In the screening study, 106 of the 248 selected Greek residents of Laconia (43%) were male and the remaining 142 (57%) were female. Their age ranged from 17 months to 94 years with a median age of 53 years. Of the 50 healthy Greek blood donors, aged from 19 to 61 years, residing in Attica, 10 (20%) were female and 40 (80%) male. The group of the 721 asymptomatic immigrants consisted of men aged between 15 and 65 years (median age: 27 years) (Table 1).
Table 1.
Demographic data of individuals included in the pilot and screening studies
| Country of origin | Age median (range) (years) | Sex | Place of residence | ||||||
|---|---|---|---|---|---|---|---|---|---|
| M | F | Laconia | Attica | Karditsa | |||||
| Pilot (N = 88) | Greeks (N = 19) | Greece | 46 (< 1–80) | 9 | 10 | 19 | − | − | |
| Negative controls (N = 50) | Greece | 6 (1–10) | 27 | 23 | − | 50 | − | ||
| Immigrants (N = 19) | Pakistan | 16 (84.2%) | 25 (19–55) | 19 | 0 | 19 | – | – | |
| Afghanistan | 1 (5.2%) | ||||||||
| India | − | ||||||||
| Bangladesh | − | ||||||||
| Morocco | − | ||||||||
| Romania | 2 (10.5%) | ||||||||
| Screening (N = 1,019) | Greeks (N = 298) | Greece | 53 (< 1–94) | 106 | 142 | 248 | − | − | |
| 40 (19–61) | 40 | 10 | − | 50 | − | ||||
| Immigrants (N = 685/721*) | Pakistan | 627 (91.5%) | 27 (15–65) | 721 | 0 | 582 | 124 | 15 | |
| Afghanistan | 24 (3.5%) | ||||||||
| India | 24 (3.5%) | ||||||||
| Bangladesh | 3 (0.44%) | ||||||||
| Morocco | 2 (0.30%) | ||||||||
| Romania | 5 (0.73%) | ||||||||
Data was available for 685 of the 721 immigrants included in the screening study.
Country of origin and place of residence.
Regarding the country of origin, 16 of the pilot study immigrants came from Pakistan, 1 from Afghanistan, and 2 from Romania. As far as the immigrants of the screening study are concerned, information was available for 685 (95%) of the 721 immigrants. Of those, 627 (91.5%) came from Pakistan, 24 (3.5%) from India, 24 (3.5%) from Afghanistan, 3 (0.44%) from Bangladesh, 2 (0.30%) from Morocco, and 5 (0.73%) from Romania. Of the 721 immigrants, 582 resided in Laconia, 124 in East Attica, mainly in Marathon, and 15 in the prefecture of Karditsa (Table 1).
Pilot study.
Of all former malaria patients (N = 38), 13.1% (N = 5) showed a positive serological reaction to Plasmodium spp., specifically, 2 of the 19 Greeks (10.5%) and 3 of the 19 immigrants (15.7%). None of the 50 healthy Greek children, residing in Attica, was found positive for antimalarial antibodies (Table 2).
Table 2.
Detection of antimalarial antibodies for Greeks and immigrants in the pilot and screening studies
| Country of origin | Positive | Total (%) | ||
|---|---|---|---|---|
| Pilot (N = 88) | Negative controls (N = 50) | Greece | 0 | 0 (0) |
| Greeks (N = 19) | 2 | 2 (10.5) | ||
| Immigrants (N = 19) | Pakistan | 2 | 3 (15.7) | |
| Afghanistan | 1 | |||
| Screening (N = 1,019) | Greeks (N = 298) | Greece | 0 | 0 (0) |
| Immigrants (N = 685/721*) | Pakistan | 73 | 85 (11.8) | |
| Afghanistan | 5 | |||
| India | 7 | |||
Data was available for 685 of the 721 immigrants included in the screening study.
Screening study.
None of the 298 Greeks, residing in Laconia (N = 248) and Attica (N = 50) was found positive for antimalarial antibodies. Regarding the immigrant population, of the 735 samples tested, 12 were measured more than once on different dates (10 two times and 2 three times) and yielded a consistently positive or negative result. Of the remaining 721 samples, 85 (11.8%) had a positive serological reaction against Plasmodium spp., whereas 636 (88.2%) gave negative results. Seventy-one of the 582 immigrants residing in Laconia and 14 of the 124 residing in east Attica were positive, whereas all immigrants residing in Karditsa were negative (Table 2).
Discussion
Antibodies are a crucial component of naturally acquired immunity against malaria, particularly the erythrocytic stage of the infection, although not the only one. From a seroepidemiological point of view, the presence of antibodies is used as a marker of exposure, rather than one of protection against infection, and the rate of acquisition and loss of antibodies is of particular interest. The rate of detection depends of course on the sensitivity of the assay used, and on the aptness of the antigenic target. The most frequently used methods for Ab detection are immunofluorescence antibody test (IFAT) and ELISA. The ELISA methods employing recombinant antigens are easier to automate and render more reproducible results, providing a sensitive, more practical, and reproducible alternative to IFAT.27 Regardless of the type of assay used, there seems to be broad agreement on the fact that antibodies are generated relatively quickly, in the course of infection, in most cases within 2 weeks.28,29 How quickly antibodies are lost however, remains a debated issue. They may persist for months or even years in semi-immune individuals who live in malaria-endemic countries, where reinfection is frequent. In naive patients, however, Ab levels fall more rapidly within a year of infection and are usually undetectable by 3–6 months.30
Greece, a country declared malaria free by the World Health Organization (WHO) since 1974, has experienced an increase in locally transmitted vivax malaria in the past 5 years. Reasons for this increase may include the influx into historically recognized malarious foci, such as south Peloponnese, of immigrants mostly from Pakistan, following recent floods that led to increased malaria risk in the Indian subcontinent region, as well as the existence of permissive Anopheles vectors in our country, such as Anopheles maculipennis, Anopheles sacharovi, and Anopheles superpictus.
The last large-scale epidemiological survey for malaria was conducted in Greece in 1974 to assess the success of the elimination program that began with the spraying campaign of 1946. No seropositives were detected in individuals under the age of 20, and the seroprevalence curve showed higher exposure in those aged over 40 years, suggesting little or no transmission at the time of the study.31 Today, the seropositive population sampled in that survey, if still alive, would have to be at least in their 80s or 90s.
The Greeks that were sampled in the follow-up pilot study of 2012 were assessed once, 5–7 months after an acute malaria attack, which most certainly was the first in their entire lifetime. They were all successfully treated with appropriate blood and tissue schizonticidal drugs within a few days of clinical presentation. Of these, 10.5% were found positive for antimalarial antibodies. The immigrant patients were also sampled within the same time frame following acute infection and were likewise promptly, appropriately, and successfully treated for it. Unlike their Greek counterparts, however, as they originated from malaria-endemic countries, it is most likely that they had been infected either with P. falciparum or with P. vivax or even with both in the past, although it cannot be ascertained when and by what genotype. Of the immigrant patients, 15.7% were found positive for antimalarial antibodies. Seronegative individuals may have produced antibodies to polymorphic epitopes that did not cross-react with the antigens used in the assay, or antibodies that did not react as efficiently with the recombinant form of antigen used in the assay as with natural antigen, or they may have developed only very short-lived responses. Finally, they may have failed to mount a humoral response to malaria, altogether.
A limitation of this study is that following acute infection only one sample was collected from each patient with documented malaria at a varying point-in-time postinfection. Unfortunately, in most cases, a single measurement per patient was all that could be achieved. Follow-up of immigrant populations is usually extremely difficult, because they are in constant motion, frequently go into hiding, and give different, often false names when examined, as a result of their illegal status. Fear of consequences, if located by the authorities during hospitalization or presentation in a health-care facility, further discourages them from seeking or accepting medical assistance. Single sample measurement precludes our study from accurately estimating Ab loss rate, which would require repeated measurements at various points postinfection. Nevertheless, the low percentage of Ab positive patients we detected ∼6 months postinfection is an observation also made in studies of Ab titer decline rate in unstable malaria transmission settings.
Specifically, complete loss of Ab has been observed over a few months, suggesting rapid clearance of the infection with prompt effective treatment in individuals with no preexisting immunity.32 Most of the studies reporting short-lived Ab responses have been conducted around the time of acute infection, which was usually consequently promptly terminated by effective antimalarial treatment.33–35
Limitations of the commercial ELISA used in this study include 1) that it simultaneously detects IgM and IgG antibodies, not allowing the discrimination between different classes of Ab reactivity and 2) the inability of the assay to distinguish between antibodies against the different species that cause malaria in humans. However, because the infecting species was known for the confirmed vivax malaria cases and only 13% of patients had any detectable Ab response 5–7 months postinfection, at a time when IgM antibodies have usually disappeared, both these limitations probably had a minor effect on the results of the pilot study. The impact of these limitations, may have been more substantial on the results of the screening study, where the assay's inability to distinguish between the species and Ab classes may have prevented us from detecting additional undiagnosed P. vivax cases that had occurred, and therefore from identifying additional foci of local P. vivax transmission.
Another limitation of the study is the sampling methodology for Greeks and immigrants, which was not randomized and possibly affected the representativeness of the sample. However, the leftover methodology with stratified sample used for the Greek population could be considered satisfactory despite the lack of randomization.26 Moreover, among the immigrants of Laconia, we achieved a relatively high participation rate (64.6%), which indicates sufficient representativeness of the sample. However, selection bias or participation bias may affect our results in both directions.
The serological screening of the local and immigrant population in Laconia, an area where autochthonous malaria transmission has been documented for at least 3 years, showed a small percentage of positive immigrants and no positives at all within the Greek population. These results likely infer rapid Ab titer decline in our non-endemic epidemiological setting, and also indicate that the local Greek population remains malaria naive. Moreover, Greeks are unlikely to serve as reservoir for the infection of local mosquitoes for another reason: their awareness for the risk of disease has been heightened in recent years and they have access to and promptly seek medical attention, when they experience symptoms indicative of malaria.
ACKNOWLEDGMENTS
We would like to thank Dr. Georges Snounou for sharing his expertise and contributing with his suggestions in the development of this project.
Footnotes
Financial support: The study was conducted in the context of the integrated surveillance and control program for West Nile Virus and malaria in Greece (MALWEST Project), which is implemented through the Operational Program entitled “Human Resources Development” of National Strategic Reference Framework” (NSRF) 2007–2013. The program is co-funded by Greece and the European Union—European Regional Development Fund.
Authors' addresses: Evangelia-Theofano Piperaki, Maria Mavrouli, John Routsias, and Athanassios Tsakris, Department of Microbiology, Medical School, University of Athens, Greece, E-mails: epiper@med.uoa.gr, mmavrouli@med.uoa.gr, jroutsias@med.uoa.gr, and atsakris@med.uoa.gr. Maria Tseroni, Athina Kallimani, Lamprini Veneti, and Theano Georgakopoulou, Hellenic Center for Disease Control and Prevention (HCDCP), Athens, Greece, E-mails: tseroni@keelpno.gr, akalliman@yahoo.gr, veneti@keelpno.gr, and georgakopoulou@keelpno.gr. Maria Georgitsou and Maria Chania, General Hospital of Sparti, Sparti, Greece, E-mails: pmas42@otenet.gr and mchania8@gmail.com. Christos Hadjichristodoulou, Laboratory of Hygiene and Epidemiology, Medical School, University of Thessaly, Larissa, Greece, E-mail: xhatzi@med.uth.gr.
References
- 1.Mueller I, Galinski MR, Baird JK, Carlton JM. Key gaps in the knowledge of Plasmodium vivax, a neglected human malaria parasite. Lancet Infect Dis. 2009;9:555–566. doi: 10.1016/S1473-3099(09)70177-X. [DOI] [PubMed] [Google Scholar]
- 2.Miller LH, Mason SJ, Clyde DF, McGinniss MH. The resistance factor to Plasmodium vivax in blacks. The Duffy-blood-group genotype, FyFy. N Engl J Med. 1976;295:302–304. doi: 10.1056/NEJM197608052950602. [DOI] [PubMed] [Google Scholar]
- 3.Culleton RL, Mita T, Ndounga M, Unger H, Cravo PV, Paganotti GM, Takahashi N, Kaneko A, Eto H, Tinto H, Karema C, D'Alessandro U, do Rosário V, Kobayakawa T, Ntoumi F, Carter R, Tanabe K. Failure to detect Plasmodium vivax in west and central Africa by PCR species typing. Malar J. 2008;7:174–181. doi: 10.1186/1475-2875-7-174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mendis K, Sina BJ, Marchesini P, Carter R. The neglected burden of Plasmodium vivax malaria. Am J Trop Med Hyg. 2001;64:97–106. doi: 10.4269/ajtmh.2001.64.97. [DOI] [PubMed] [Google Scholar]
- 5.Gething PW, Elyazar IR, Moyes CL, Smith DL, Battle KE, Guerra CA, Patil AP, Tatem AJ, Howes RE, Myers MF, George DB, Horby P, Wertheim HF, Price RN, Müeller I, Baird JK, Hay SI. A long neglected world malaria map: Plasmodium vivax endemicity in 2010. PLoS Negl Trop Dis. 2012;6:e1814. doi: 10.1371/journal.pntd.0001814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Odolini S, Gautret P, Parola P. Epidemiology of imported malaria in the mediterranean region. Mediterr J Hematol Infect Dis. 2012;4:e2012031. doi: 10.4084/MJHID.2012.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Calderaro A, Piccolo G, Gorrini C, Rossi S. Accurate identification of the six human Plasmodium spp. causing imported malaria, including Plasmodium ovale wallikeri and Plasmodium knowlesi. Malar J. 2013;12:321. doi: 10.1186/1475-2875-12-321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Whitty CJ, Chiodini PL, Lalloo DG. Investigation and treatment of imported malaria in non-endemic countries. BMJ. 2013;346:f2900. doi: 10.1136/bmj.f2900. [DOI] [PubMed] [Google Scholar]
- 9.Centers for Disease Control and Prevention Filler SJ, MacArthur JR, Parise M, Wirtz R, Eliades MJ, Dasilva A, Steketee R. Locally acquired mosquito-transmitted malaria: a guide for investigations in the United States. MMWR Recomm Rep. 2006;55:1–9. [PubMed] [Google Scholar]
- 10.Kruger A, Rech A, Su XZ, Tannich E. Two cases of autochthonous Plasmodium falciparum malaria in Germany with evidence for local transmission by indigenous Anopheles plumbeus. Trop Med Int Health. 2001;6:983–985. doi: 10.1046/j.1365-3156.2001.00816.x. [DOI] [PubMed] [Google Scholar]
- 11.Armengaud A, Legros F, D'Ortenzio E, Quatresous I, Barre H, Houze S, Valayer P, Fanton Y, Schaffner F. A case of autochthonous Plasmodium vivax malaria, Corsica, August 2006. Travel Med Infect Dis. 2008;6:36–40. doi: 10.1016/j.tmaid.2007.09.042. [DOI] [PubMed] [Google Scholar]
- 12.Santa-Olalla Peralta P, Vazquez-Torres MC, Latorre-Fandos E, Mairal-Claver P, Cortina-Solano P, Puy-Azón A, Adiego Sancho B, Leitmeyer K, Lucientes-Curdi J, Sierra-Moros MJ. First autochthonous malaria case due to Plasmodium vivax since eradication, Spain, October. Euro Surveill. 2010;15:19684. doi: 10.2807/ese.15.41.19684-en. [DOI] [PubMed] [Google Scholar]
- 13.Arends JE, Oosterheert JJ, Kraaij-Dirkzwager MM, Kaan JA, Fanoy EB, Haas PJ, Scholte EJ, Kortbeek LM, Sankatsing SU. Two cases of Plasmodium falciparum malaria in The Netherlands without recent travel to a malaria-endemic country. Am J Trop Med Hyg. 2013;89:527–530. doi: 10.4269/ajtmh.13-0213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bruce-Chwatt LJ, de Zulueta J. The Rise and Fall of Malaria in Europe: A Historico-Epidemiological Study. Oxford, NY: Oxford University Press; 1980. pp. 18–25. [Google Scholar]
- 15.Vakalis N. Epidemiological Surveillance of Malaria in Countries of Central and Eastern Europe and Selected Independent States: Greece. Report on a WHO intercountry meeting, June 24–26, 2002, Sofia, Bulgaria. Copenhagen, Denmark: World Health Organization Regional Office for Europe; 2002. p. 10. [Google Scholar]
- 16.Kampen H, Proft J, Etti S, Maltezos E, Pagonaki M, Maier WA, Seitz HM. Individual cases of autochthonous malaria in Evros Province, northern Greece: entomological aspects. Parasitol Res. 2003;89:252–258. doi: 10.1007/s00436-002-0746-9. [DOI] [PubMed] [Google Scholar]
- 17.HPA reports 22 percent increase in malaria cases returning from the Indian sub-continent. http://webarchive.nationalarchives.gov.uk/20140714084352/http://www.hpa.org.uk/NewsCentre/NationalPressReleases/2012PressReleases/120425Malaria/ Available at. Accessed March 6, 2015.
- 18.Stark K, Schöneberg I. Increase in malaria cases imported from Pakistan to Germany in 2012. Euro Surveill. 2012;17:20320. doi: 10.2807/ese.17.47.20320-en. [DOI] [PubMed] [Google Scholar]
- 19.Vakali A, Patsoula E, Spanakos G, Danis K, Vassalou E, Tegos N, Economopoulou A, Baka A, Pavli A, Koutis C, Hadjichristodoulou C, Kremastinou T. Malaria in Greece, 1975 to 2010. Euro Surveill. 2012;17:20322. doi: 10.2807/ese.17.47.20322-en. [DOI] [PubMed] [Google Scholar]
- 20.Danis K, Lenglet A, Tseroni M, Baka A, Tsiodras S, Bonovas S. Malaria in Greece: historical and current reflections on a re-emerging vector borne disease. Travel Med Infect Dis. 2013;11:8–14. doi: 10.1016/j.tmaid.2013.01.001. [DOI] [PubMed] [Google Scholar]
- 21.Struik SS, Riley EM. Does malaria suffer from lack of memory? Immunol Rev. 2004;201:268–290. doi: 10.1111/j.0105-2896.2004.00181.x. [DOI] [PubMed] [Google Scholar]
- 22.Langhorne J, Ndungu FM, Sponaas AM, Marsh K. Immunity to malaria: more questions than answers. Nat Immunol. 2008;9:725–732. doi: 10.1038/ni.f.205. [DOI] [PubMed] [Google Scholar]
- 23.Drakeley CJ, Corran PH, Coleman PG, Tongren JE, McDonald SL, Carneiro I, Malima R, Lusingu J, Manjurano A, Nkya WM, Lemnge MM, Cox J, Reyburn H, Riley EM. Estimating medium- and long-term trends in malaria transmission by using serological markers of malaria exposure. Proc Natl Acad Sci USA. 2005;102:5108–5113. doi: 10.1073/pnas.0408725102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Del Giudice G, Lambert PH, Mendis K, Pessi A, Pessi A, Tanner M. Antibody responses to Plasmodium falciparum and P. vivax sporozoites in areas with stable and unstable malaria. Bull World Health Organ. 1990;68:191–196. [PMC free article] [PubMed] [Google Scholar]
- 25.Mueller I, Galinski MR, Tsuboi T, Arevalo-Herrera M. Natural acquisition of immunity to Plasmodium vivax: epidemiological observations and potential targets. Adv Parasitol. 2013;81:77–131. doi: 10.1016/B978-0-12-407826-0.00003-5. [DOI] [PubMed] [Google Scholar]
- 26.Nardone A, Miller E. Serological surveillance of rubella in Europe: European Sero-Epidemiology Network (ESEN2) Eurosurveillance. 2004;9:4. doi: 10.2807/esm.09.04.00456-en. [DOI] [PubMed] [Google Scholar]
- 27.Doderer C, Heschung A, Guntz P, Cazenave JP, Hansmann Y, Senegas A, Pfaff AW, Abdelrahman T, Candolfi E. A new ELISA kit which uses a combination of Plasmodium falciparum extract and recombinant Plasmodium vivax antigens as an alternative to IFAT for detection of malaria antibodies. Malar J. 2007;97:557–564. doi: 10.1186/1475-2875-6-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Collins WE, Jeffery GM, Skinner JC. Fluorescent antibody studies in human malaria. I. Development of antibodies to Plasmodium malariae. Am J Trop Med Hyg. 1964;13:1–5. doi: 10.4269/ajtmh.1964.13.1. [DOI] [PubMed] [Google Scholar]
- 29.Baird JK, Barcus MJ, Elyazar IR, Bangs MJ, Maguire JD, Fryauff DJ, Richie TL, Sekartuti, Kalalo W. Onset of clinical immunity to Plasmodium falciparum among Japanese migrants to Indonesian Papua. Ann Trop Med Parasitol. 2003;97:557–564. doi: 10.1179/000349803225001472. [DOI] [PubMed] [Google Scholar]
- 30.Park CG, Chwae YJ, Kim JI, Lee JH, Hur GM, Jeon BH, Koh JS, Han JH, Lee SJ, Park JW, Kaslow DC, Strickman D, Roh CS. Serologic responses of Korean soldiers serving in malaria-endemic areas during a recent outbreak of Plasmodium vivax. Am J Trop Med Hyg. 2000;62:720–725. doi: 10.4269/ajtmh.2000.62.720. [DOI] [PubMed] [Google Scholar]
- 31.Bruce-Chwatt LJ, Draper CC, Avramidis D, Kazandzoglou O. Sero-epidemiological surveillance of disappearing malaria in Greece. J Trop Med Hyg. 1975;78:194–200. [PubMed] [Google Scholar]
- 32.Drakeley C, Cook J. Chapter 5. Potential contribution of sero-epidemiological analysis for monitoring malaria control and elimination: historical and current perspectives. Adv Parasitol. 2009;69:299–352. doi: 10.1016/S0065-308X(09)69005-9. [DOI] [PubMed] [Google Scholar]
- 33.Cavanagh DR, Elhassan IM, Roper C, Robinson VJ, Giha H, Holder AA, Hviid L, Theander TG, Arnot DE, McBride JS. A longitudinal study of type-specific antibody responses to Plasmodium falciparum merozoite surface protein-1 in an area of unstable malaria in Sudan. J Immunol. 1998;161:347–359. [PubMed] [Google Scholar]
- 34.Kinyanjui SM, Bull P, Newbold CI, Marsh K. Kinetics of antibody responses to Plasmodium falciparum-infected erythrocyte variant surface antigens. J Infect Dis. 2003;187:667–674. doi: 10.1086/373994. [DOI] [PubMed] [Google Scholar]
- 35.Asito AS, Moormann AM, Kiprotich C, Ng'ang'a ZW, Ploutz-Snyder R, Rochford R. Alterations on peripheral B cell subsets following an acute uncomplicated clinical malaria infection in children. Malar J. 2008;7:238. doi: 10.1186/1475-2875-7-238. [DOI] [PMC free article] [PubMed] [Google Scholar]