Abstract
Mobile health (mHealth) technology can be a valuable tool in the management of chronic illnesses, including HIV. Qualitative research methods were used to identify the desired content and features of a mobile app for meeting and improving the healthcare needs of persons living with HIV (PLWH). We conducted six focus group sessions with 50 English-or Spanish-speaking PLWH in New York City. To inform data analysis and to illustrate how mHealth technology can be used as a persuasive strategy for improving the health of PLWH, we integrated Fogg's functional role triad for computing technology model with the self-determination theory to illustrate how mHealth technology can be used as a persuasive strategy for improving the health of PLWH. Participants suggested several tools for meeting their healthcare needs, including: reminders/alerts, lab results tracking, and notes on health status. mHealth technology can function as a social actor by providing chat boxes/forums, testimonials of lived experiences, and personal outreach. Examples of media that can be used as a persuasive technology include games/virtual rewards, coding of health tasks, and simulations on how to connect with PLWH. Findings from these focus groups can be used to design a mobile app for PLWH that is targeted to meet their healthcare needs.
Keywords: HIV/AIDS, Fogg's functional role triad, Self-determination theory, Mobile health (mHealth) technology
Introduction
Mobile health (mHealth) is the use of mobile devices—such as cellular phones, tablets, smartphones and other wireless devices—for the delivery of health services and information [1]. The ubiquitous nature of mobile technologies in daily life creates opportunities for health behavior management tools that were not previously possible [2]. mHealth can be used to rapidly assess and modify health-related behavior and transform patients’ decision-making about their health [1]. The use of mHealth can reduce geographical and economic disparities and personalize healthcare [3, 4].
mHealth also has the potential to bridge a divide in health-care delivery among underserved racial and ethnic minority groups. The use of mobile technology has made a huge impact on communication, access, and information/resource provision to minority and underserved populations [5]. Ownership of a smartphone is more common among blacks than whites (92 vs. 90 %) [6]; Latinos are more likely than whites or blacks to own a smartphone (61 vs. 59 and 53 %, respectively) [7]; and Latinos and blacks are more likely to send or receive text messages via a cell phone than whites (87 vs. 85 vs. 79 %). Finally, blacks and Latinos are more likely to take advantage of a much greater range of smartphone features, including downloading apps, e-mail and accessing the Internet than whites [7].
mHealth for Persons Living with HIV (PLWH)
The United States (US) HIV epidemic continues to be a significant health challenge [8]. People living with HIV (PLWH) confront a range of psychological and behavioral challenges, including adherence to medication regimens, accessing healthcare services, changes in quality of life, stigma, uncertainty about physical and psychological decline and death [9]. At the same time, the HIV/AIDS epidemic in the US is highly concentrated demographically in racial and ethnic minorities [10–12]. To address this health disparity, health tools tailored to the needs of this population are needed [13, 14]. mHealth tools can promote the management and prevention of chronic illnesses, such as HIV [15], and have the potential to address many of the healthcare needs of PLWH including adherence to HIV medications and retention in HIV care and treatment.
mHealth tools to support HIV care have largely been developed and studied outside the US in low and middle income countries [16]. Two systematic reviews on the use of text messaging for treatment adherence in PLWH have been conducted but the studies were focused on populations outside the US [16, 17]. In another systematic review on the use of health tools for PLWH, all of the US studies in the review focused on the use of mobile technology as a data collection tool for targeting smoking cessation in PLWH [18]. A recent review of 12 technology-based interventions for PLWH in the US and abroad identified several gaps in content including sexual risk reduction, engagement, and retention in care [19]. Currently there are many mHealth apps for PLWH [20] but few have been developed by using information gathered from potential app users or healthcare providers.
Of the limited studies specifically focused on mobile apps for PLWH, one study identified the preferences for a mobile app in HIV positive young mothers [21]. In another study, researchers developed a mobile app consisting of a music program to improve adherence to antiretroviral medications for adult PLWH. Similar to the foundational planning of many of the other interventions that have been developed, this study did not engage the intended end-users in the development of the intervention and was focused on a single outcome of treatment adherence [22]. The study discussed here will inform the development of a multi-component app.
The focus group results reported here are part of a larger research project to inform the development of two mobile apps for (1) HIV treatment and care for PLWH, and (2) HIV prevention for high-risk men who have sex with men. The purpose of this study is to identify the desired content and features of a mobile app for meeting the healthcare needs of PLWH, and ultimately, to improve their health.
Methods
Study Design
We used a qualitative observational study design and focus group methodology as the first step in a series of participatory user-centered design activities to inform the development of a mobile app for PLWH [23].
Recruitment and Eligibility
Eligibility criteria included being HIV positive, 13–65 years of age, having the ability to communicate in English or Spanish, and willingness to provide written informed consent. Parental consent was waived by the Institutional Review Board (IRB) for adolescents. Adolescents had to be willing to provide assent. The IRB of Columbia University reviewed and approved the study protocol.
Participants for the focus group sessions were recruited from June 2013 to October 2013 in New York City. Recruiters placed flyers in an HIV clinic (New York Presbyterian Hospital), three community-based organizations (Gay Men's Health Crisis, Harlem United, and Latino Commission on AIDS), and two HIV case management agencies (Housing Works and AIDS Service Center). During the recruitment period, potential participants were provided with details of the study and screened over the phone to determine if they met the eligibility criteria for study participation.
Procedures
Eligible men and women were invited to attend focus groups based on what was convenient for their schedule and their language preference. Focus group sessions were led by a trained facilitator. Each focus group was attended by at least one additional study team member who recorded notes and tended to logistics, such as administering consent forms, organizing food, and providing the $25 token of appreciation. Focus groups took place in a conference room at the Columbia University School of Nursing campus, lasted approximately 45–70 min. Prior to the start of each focus group, participants were asked to complete quantitative assessments that included basic demographics, HIV health history, HIV stigma [24] and information privacy concerns [25].
Focus group facilitators followed a structured guide that included an introduction and questions grouped in five areas related to the content of a mobile app for PLWH: (1) HIV education and information, (2) identifying HIV treatment resources, (3) HIV care and treatment adherence, (4) health data management, and (5) technology adoption. To support the credibility of the data interpretation, facilitators reflected their interpretations (i.e., member checks) to focus group participants throughout the session. All focus group sessions were audio-recorded and transcribed verbatim. Spanish language transcripts were subsequently translated into English.
Data Analysis
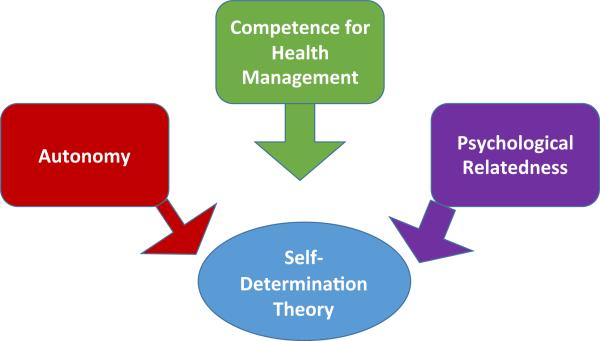
After each focus group, the research team conducted peer debriefing. To analyze the focus group transcripts, a codebook was developed based on two theoretical models: self-determination theory (SDT) and Fogg's functional triad. SDT is a theory of human motivation concerning people's innate psychological needs and was used to describe the behavioral targets that could be achieved through the use of the mHealth app (Fig. 1). SDT is concerned with the motivation behind the choices that people make and focuses on the degree to which an individual's behavior is self-motivated [26]. The basic psychological needs component of SDT identifies three main needs that motivate an individual to initiate a behavior that is essential for his/her well-being: autonomy, competence, and psychological relatedness [27, 28].
Fig. 1.
The self-determination theory (SDT)
Autonomy is an individual's need for regulating behaviors because of the personal importance of the behavior to their health. In the case of HIV, autonomy involves a person's belief that it is important to take HIV medications to improve health and well-being [29]. Competence is an individual's feeling competent about their skills related to a health behavior. Competence can be achieved by improving skills or building on talents to assist a person in improving his/her behavior [30]. This can be understood as a person's ability to take their medications as prescribed and not miss doses. Psychological relatedness is the desire to interact with, be connected to, and experience caring by others [31]. For example, a PLWH may want family support in order to begin HIV treatment.
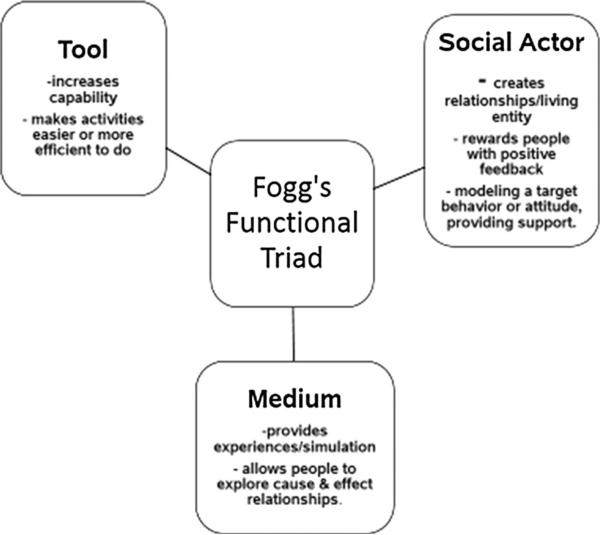
Fogg's functional triad for computing technology model [32] (Fig. 2) was used to describe the modes by which the mHealth app could be designed to affect the behavioral targets. Fogg proposed that technologies designed to influence behavior can operate through a triad of tools, medium, and social actors [32]. Tools are technologies that can increase people's ability to perform a behavior by making it easier. For instance, uploading pedometer data for tracking physical activity progress over time. As medium, technologies can create simulated experiences that support rehearsing a behavior, empathizing, or exploring causal relationships (e.g., helping people create a plan to exercise regularly). As social actors, technologies can cue social responses to influence behaviors; for example, video testimonials describing how to fit regular exercise into daily life.
Fig. 2.
Fogg's functional role triad
Focus group transcripts were recorded, transcribed, and checked for accuracy. Coding began after repeated readings of each transcript, at least twice using NVivo™ Version 10.0 (QSR International, Victoria, Australia) software. Codes were created based on a line-by-line analysis. Data were summarized thematically through an iterative process and organized according to the SDT and Fogg's functional triad models. All transcripts were double coded and discrepancies were discussed among three research team members until consensus was reached. Research team members grouped quotations according to codes. Data analysis continued until saturation was reached, which occurred when similar patterns and themes were identified across focus groups and no new information was being shared [33]. Data from quantitative assessments were entered into SPSS statistical software. Descriptive statistics of the demographic information were calculated and are described below.
Results
Study Sample
There were six focus group sessions. In order to elicit concerns that may be particular to women or adolescents, the study team arranged two targeted focus groups: one for adolescents and young adults (13–24 years of age) and a second for women. Four groups were conducted in English, and two groups were conducted in Spanish with participants whose primary language was Spanish. Among the six focus groups conducted with 50 PLWH, over half of the participants reported their race as black/African American (52 %), and half reported their ethnicity as Latino/Hispanic (50 %) (Table 1). Participants’ ages ranged from 18 to 59 years, with an average age of 42. The majority (83 %) of participants were age 24 and older. The majority of participants were male (74 %). Slightly over half (54 %) of the participants were smartphone users. Participants reported that they first received care for their HIV between 9 months and 30 years ago (Mean = 13.74; Standard Deviation. 8.56).
Table 1.
Persons living with HIV focus group participants
| Frequency (%)* | |
|---|---|
| Gender | |
| Male | 37 (74) |
| Female | 13 (26) |
| Ethnicity | |
| Hispanic/Latino | 25 (50) |
| Non-Hispanic | 22 (44) |
| Race | |
| African American/Black | 26 (52) |
| American Indian/Alaskan Native | 4 (8) |
| Asian | 2 (1.2) |
| Native Hawaiian/Pacific Islander | 2 (1.2) |
| White | 7 (14) |
| Other | 8 (16) |
| Smartphone user | |
| Yes | 27 (54) |
| No | 23 (46) |
Not all numbers total 100 % because some participants declined to state
Results of Qualitative Analysis
The desired mobile app features/functions are categorized by the SDT and Fogg's functional role triad and representative quotes from each category are listed in Table 2.
Table 2.
Desired mobile app features/functions categorized by the SDT and Fogg's functional triad
| SDT behavioral target | Fogg's functional role | Mobile app features/functions | Sample quote |
|---|---|---|---|
| Autonomy | Tool | Calendar | “My phone reminds me to take my medication” |
| Alarm-Medication/appointment reminders | “They have alarms set on their phones and they have calendar applications where they can write appointments” | ||
| Social actor | Testimonials of lived experiences | “The support groups really help and it does motivate you because you're learning or you're giving information” | |
| Media | Games/virtual rewards | “Let's say you did good and you were undetectable for this month you could put that on your calendar, a gold star or something on that day” | |
| Competence for health management | Tool | Interactive health report card | “I think a great thing would be if there was an app that said like here's what you need and when. Like a health report card” |
| Utility for self-monitoring lab results over time | |||
| Social actor | Personal outreach on how to manage medications | “you have email, and there I receive everything regarding HIV, the new stuff, the new medications that have come out, the side effects medications have, what medications are for, and all that is very interesting, so most of the time I am trying to access it, and I have it on my telephone and I check it every day” | |
| “So we just have to get accustomed to using that certain app in our phone to get on, you know to look at our medications, to look at our labs” | |||
| Media | To do list of health monitoring activities | “it had different color codings for different type of appointments that I could use, it had areas where I could write what the appointment was about, who I'm going to see, contact information, there was enough space for that. It had an alarm to tell me when that appointment was and I could set it for an hour before, 2 hours before, a day before” | |
| Color coding of tasks | |||
| Psychological Relatedness | Tool | Virtual lectures | “well lectures for positive and negative people, how you prevent it, and having it, how you survive it,” |
| GPS functionality to locate support groups | |||
| Social actor | Chat boxes | “a link to a forum or a chat room where people could ask questions with other people who have HIV or just express concerns in a way that's confidential, where they feel safe and where other people can respond, both doctors and other positive people” | |
| Social networking forums | |||
| “people can write anonymously (on forums) just to give advice if you're going through this or. just to give people their perspective on what they're going through in their situation” | |||
| Media | Simulation on how to interact and connect with people | “Well, they give you advice and they actually show you...like they'll do two actors and they'll play out a scene. It could go wrong, it could go right. If you want to find out how to disclose, you could go to YouTube” |
Autonomy
To achieve autonomy, defined as an individual's desire to control their own health, study participants identified how a mobile app's features could be used to inform their treatment decisions and behaviors and provide them with greater independence in decision making. Participants described the need to support autonomy related to medication management and organization of appointments. A mobile app could serve as a tool to increase PLWH's ability to increase the efficiency of their activities. Examples of tools to improve autonomy included a calendar and an alarm with reminders for appointments and medications. For example, one participant discussed the usefulness of writing notes on her phone: “It keeps me organized with all my appointments, everything. And I mean I use it every day.” A participant specifically explained how useful it was to have a calendar as a tool: “I use the calendar. I have an iPhone and the calendar allows you to add the appointment time, and it gives you the option to remind you at 30 min or the time you may need, and it's very useful.” A number of participants explained that they set an alarm to remind them to take their medications. As one participant said, “My phone reminds me to take my medications.”
To help a person achieve autonomy in their healthcare decision-making, a mobile app can also serve as a social actor to create relationships to reward people and serve as a model for a target behavior or attitude. Often, a newly diagnosed individual may not want to take the initiative to take care of his/her health. A mobile app can help support autonomy by offering social connection with other PLWH about taking care of one's health (e.g., taking HIV medications). For example, one PLWH participant suggested that a mobile app could be used to “help other kids who I know are not doing well, and tell them look at this, and this and this is what happens, motivate them so they don't do foolish stuff that they don't have to do, that is something good which at least it makes me feel healthy that I am helping someone not to get infected with the virus.”
Finally a mobile app can serve as a medium for promoting motivation for desired behaviors in PLWH by allowing people to explore cause and effect relationships and providing people with vicarious experiences that show the positive effect of healthy behaviors. Specific functionality of a mobile app to achieve this targeted behavior includes gaming and reward systems. For example, one participant suggested that a mobile app “would make people adhere to their medication a little bit more because it would be nice to get a smiley face on your phone, like, good morning, and you've got a smiley face or something or thought for the day or something like that.”
Competence for Health Management
Importantly, PLWH need to feel competent about their ability to manage their own health since they live with a chronic illness that requires self-management. Competence can be achieved by skill-building, tools, and feedback to assist a PLWH in improving his/her behavior. Participants identified the use of a mobile app to support their monitoring of health behaviors, lab results and medication management. A mobile app can serve as a persuasive technology for achieving competence by supporting a person's confidence in his ability to manage his health-related issues. Specific mobile apps tools related to this construct include an interactive health report card and a utility for self-monitoring lab results over time. One participant explained that his lab results fluctuate and “my T-cells went down and I don't know why. So it would be a good tracking device to keep track of each time you do your lab work, instead of walking around with papers.” A few participants also commented that they would want to be able to have an electronic record of their HIV status accessible to them on an app so that they can track their health status and make informed decisions about their health. “I would think getting your labs through [the app] because there are a lot of places that I go to that upon admission or whatever you're going through they want to see proof that you're positive. I know for me it's a problem. I don't carry that information with me. It would be really good if the doctor or CDC put that in an app so that you have access to it and you can show it right then and there.”
A mobile app can also serve as social actor for achieving competence for health management. Other PLWH can provide guidance on how they take their medications or manage their symptoms to support health management in the mobile app user. As one focus group participant said, “It could be an app where you don't show your face or anything, but you want to know your status or you just want to know more about this disease. Some people aren't going to go to a training, some people aren't going to go do certain things, but a person will sit at home and go through their computer...what's the symptoms of this?” Finally a mobile app can be a medium for managing their health by providing a to-do list and color coding of health monitoring tasks. One PLWH explained that he “put asterisks on the sides of the most important ones [tasks]. I color code them to make sure [I complete the task]” Another participant also reflected on how he uses this tool “the red dot means that one must show up (for an appointment).”
Psychological Relatedness
To achieve psychological relatedness, an individual needs to experience a sense of belonging or attachment to others including feeling rapport and connection with others. A mobile app can be used to initiate interactions with others, or can bolster social support received from others (e.g., an app can be shared with family members to increase engagement and support). To achieve psychological relatedness, a mobile app should have functions that serve as a means to make it easier for a person to connect with others. Social networking, GPS functionality, and context-specific links to information resources, are examples of tools that can help participants connect with others. One participant explained how a mobile app could provide information that is important for family and friends to access. “I went into Google to search for information to guide my family because they are from a rural area and they were confused [thinking that] if they ate from the same spoon [used by a person with HIV, they would] get infected.” Another participant said, “But for me, it's like really useful because I can like Google whatever I need to know or like if I need to find a certain location. I GPS-system that.” Another participant shared that, ‘if one wants to find a support group, let's say positive people you want to connect with a young person...will look for other positive people, that have the same struggles as you do... so you go to Google, look up positive people or people with AIDS from 20 to 30 or 40 to 50, according to what you need, and you can look up those connections, contact people who have your same outlook, and then start a relationship.” Participants also suggested that “visuals, videos, you tube” were all important tools that can be included when using a mobile app to connect with others.
Participants suggested the use of chat boxes and social networking forums as social actors for achieving psychological relatedness. One participant spoke highly of his experience with “a website called POZ, and they have forums and people write their own anonymous name...they have a forum, and they write like their CD4 counts, things go up, down, they write their own testimonials.” Integration of social forums into an app was important for focus group participants. Another participant said “That's a good HIV site that does appear and you can ask questions for whenever you need support from people who are infected you know, have a good support because you talk to people from all around and talk about HIV.”
Finally a mobile app has the potential to provide a medium for achieving psychological relatedness for PLWH. The app can provide simulation on ways to interact and connect with others. Participants explained the importance of role-playing disclosure to others and videos demonstrating how others disclose their HIV status. Other focus group participants mentioned the need for a medium to demonstrate how to communicate with providers “Because when I get in there (provider's office), my mind just goes blank. So I need an app that says when I get in there, it'll come up and say ‘Samantha, don't forget to ask this question.”’
Discussion
The findings of this study integrate two theoretical frameworks to address different components of the data analysis–one (SDT) represents the behavioral target component (i.e., the what) and the second (Fogg's triad) the intervention component (i.e., the how). Both aspects are critical to developing a mHealth app that is perceived as useful and easy to use by the intended users, which is critical for supporting use of the technology [34, 35]. This study also identified the content and features necessary to develop a mobile app that can target behavioral change to improve the health and lives of PLWH; a significant need for people living with an infectious and chronic illness that requires self-management of health.
Through our analysis, we identified several key components of a mobile app for meeting the health needs of PLWH including both information and communication needs [36], which are related and represent a continuum [37]. To meet the behavioral targets of the SDT, participants suggested that three primary information tools be integrated into a mobile app: reminders/alerts, lab tracking, and notes. For example, if a PLWH sees a trend of a higher viral load then they will realize that they need to take action which may be as simple as improving medication adherence or may require a follow-up visit with a health-care provider. Participants also discussed the use of a mobile app for symptom management which has been identified as a health management need for PLWH [38]. If PLWH use an app to track moods, stress, and anxiety through real time technology, then the use of an algorithm to tailor self-management advice not just for their HIV but their comorbid conditions (or those they are at high risk for), would change the approach to disease management and mitigation in PLWH [39].
Participants also identified communication tools and that a mobile app can function as a social actor by providing chat boxes/forums, testimonials of lived experiences, and personal outreach. Participants described examples of media that can be used as a persuasive technology, including games/virtual rewards, coding of health tasks, and simulation on how to interact with people. In specific, through the use of social networking, peer rewards can be used with mobile apps to improve HIV self-management [38, 39]. Findings from these focus groups will inform additional follow-up work to identify the functional specifications for a mobile app for PLWH to meet their healthcare needs.
Few studies have been conducted on the use of mHealth tools for PLWH [40]. Two previous reports reviewed the existing mobile apps for PLWH [20, 41]. The findings reported here highlight the novel abilities of mobile applications, such as time stamped data capture, calendars, and tailored messaging, to offer new improve technological capacities for improving information management for those living with HIV.
This study involved focus groups of persons affected by HIV in the United States. Of note, half of our study sample self-identified as being Latino and over half self-identified as being Black. This is significant as racial and ethnic minorities are disproportionately burdened by the HIV epidemic [10, 11]. Moreover, two of our focus groups were conducted in Spanish. The features and content identified in our Spanish focus group sessions are congruent with the findings from English speaking groups highlighting the similarity of needs of PLWH regardless of race and ethnicity. Findings from this study are particularly salient because racial and ethnic minorities are as likely or more likely than whites to use smartphones [42], thus this may be a promising tool for addressing the current disparities in healthcare in this population [43].
Methodologically, our study applied user-centered participatory design methods to inform the content of a mobile app for HIV treatment and care. While numerous mHealth intervention studies have been conducted, none have incorporated user-centered design methods to inform the development of an intervention or a mobile app from the PLWH's perspective [16]. Moreover, our study participants included many of those PLWH who are at highest risk for being underserved and most representative of the current US HIV epidemic, including young adults and racial and ethnic minorities. Given the user-centered design of our study, the findings can be used to refine existing apps or develop new apps to include the identified needs of PLWH.
One of the challenges in the use of mHealth for behavioral health interventions is that users typically engage in the use of apps enthusiastically in the beginning and then the novelty disappears. The work conducted in our study is the first step in building an app for PLWH employing user-centered participatory design methods. Past research has shown that inclusion of the end-users’ in the development of the health behavior intervention makes it more likely to be used [44].
Limitations
Whenever a new area is being explored there are limitations to be expected. Conducting this study in one geographic location limits the generalizability of the findings. Nonetheless, New York City, the setting of our study, is the largest and most diverse city in the United States and has the largest percentage of persons infected with HIV [45–48], our sample represents an important segment of the HIV epidemic in the US. Moreover, study participants were self-selected and so they may be more likely to be interested in the use of mobile technology. Even so, we included study participants who were non-users of mobile technology to expand the diversity of perspectives beyond mobile technology users.
Conclusions
Mobile apps offer novel functionality beyond text messaging, such as time stamped data capture, calendars, GPS, social engagement and tailored messaging, which offer new opportunities for improving the lives of PLWH. This work was focused on the PLWH's views of the functional specifications and features for inclusion in a mobile app for PLWH. Using Fogg's functional triad and the SDT, we were able to identify the salient content and features desired by PLWH for improving management and treatment of the disease.
Acknowledgment
This publication was supported by a cooperative agreement between Columbia University School of Nursing and the Centers for Disease Control and Prevention (CDC; 1U01PS00371501; PI: R Schnall). The authors would like to acknowledge Jocelyn Patterson Mosley, Monique Carry and Deborah Gelaude at the Centers for Disease Control and Prevention, National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention, Division of HIV/AIDS Prevention, Prevention Research Branch, Atlanta, GA for their contributions to this project. The findings and conclusions in this report do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Contributor Information
Rebecca Schnall, Columbia University School of Nursing, 617 West 168th Street, New York, NY 10032, USA.
Suzanne Bakken, Department of Biomedical Informatics and School of Nursing, Columbia University, New York, NY, USA.
Marlene Rojas, Columbia University School of Nursing, 617 West 168th Street, New York, NY 10032, USA.
Jasmine Travers, Columbia University School of Nursing, 617 West 168th Street, New York, NY 10032, USA.
Alex Carballo-Dieguez, HIV Center for Clinical and Behavioral Studies, New York State Psychiatric Institute, Columbia University, New York, NY, USA.
References
- 1.Kumar S, Nilsen W, Pavel M, Srivastava M. Mobile health: revolutionizing healthcare through trans-disciplinary research. Computer. 2013;46(1):28–35. [Google Scholar]
- 2.Estrin D, Sim I. Health care delivery. Open mHealth architecture: an engine for health care innovation. Science. 2010;330(6005):759–60. doi: 10.1126/science.1196187. [DOI] [PubMed] [Google Scholar]
- 3.Akter S, Ray P. mHealth - an Ultimate Platform to Serve the Unserved. IMIA Yearbook 2010: Biomedical Informatics: Building Capacity Worldwide. 2010;5(1):94–100. [PubMed] [Google Scholar]
- 4.Klasnja P, Pratt W. Healthcare in the pocket: mapping the space of mobile-phone health interventions. J Biomed Inform. 2012;45(1):184–98. doi: 10.1016/j.jbi.2011.08.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lenhart A, Hitlin P, Madden M. [1 Sept 2014];Teens and Technology: Pew Internet and American Life Project; 2005 [cited 2010 March 28] Available from: http://www.pewinternet.org/Reports/2005/Teens-and-Technology/06-Communications-Tools-and-Teens/17-Cell-phone-text-messaging-emerges-as-a-formidable-force.aspx?r=1.
- 6.Smith A. African Americans and Internet Use. Pew Research Center; 2013. [Google Scholar]
- 7.Duggan M. [26 Aug 2014];Cell Phone Activities 2013. [updated May 19, 2013]. Available from: http://www.pewinternet.org/2013/09/19/cell-phone-activities-2013/.
- 8.Centers for Disease Control and Prevention [29 Aug 2014];HIV in the Unites States: At A Glance Atlanta, GA 2013 [cited 2014 June 11] Available from: http://www.cdc.gov/hiv/statistics/basics/ataglance.html.
- 9.Remien RH, Mellins CA. Long-term psychosocial challenges for people living with HIV: let’s not forget the individual in our global response to the pandemic. AIDS. 2007;21:S55–63. doi: 10.1097/01.aids.0000298104.02356.b3. doi:10. 1097/01.aids.0000298104.02356.b3. [DOI] [PubMed] [Google Scholar]
- 10.Center for Disease Control and Prevention (CDC) [11 June 2014];HIV Among Latinos. 2014 Available from: http://www.cdc.gov/hiv/risk/racialEthnic/hispanicLatinos/facts/index.html.
- 11.Centers for Disease Control and Prevention (CDC) [1 Sept 2014];HIV Among African Americans Atlanta, GA. 2014 Available from: http://www.cdc.gov/hiv/risk/racialEthnic/aa/facts/.
- 12.Hall HI, Song R, Rhodes P, Prejean J, An Q, Lee LM, et al. Estimation of HIV incidence in the United States. JAMA. 2008;300(5):520–9. doi: 10.1001/jama.300.5.520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Brown W., III . New Media Interventions in Youth Sexual Health Promotion and HIV/STI Prevention. University of California, Berkeley; Berkley: 2010. [Google Scholar]
- 14.Tufts KA, Johnson KF, Shepherd JG, Lee J, Ajzoon MSB, Mahan LB, et al. Novel interventions for HIV self-management in African American women: a systematic review of mHealth interventions. J Assoc Nurses AIDS Care. 2014 doi: 10.1016/j.jana.2014.08.002. doi:10.1016/j.jana.2014.08.002. [DOI] [PubMed] [Google Scholar]
- 15.Kirk GD, Himelhoch SS, Westergaard RP, Beckwith CG. Using mobile health technology to improve HIV care for persons living with HIV and substance abuse. AIDS Res Treat. 2013;2013:194613. doi: 10.1155/2013/194613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Catalani C, Philbrick W, Hamish F, Mechael P, Israelski D. mHealth for HIV treatment & prevention: a systematic review of the literature. Open AIDS J. 2013;7:17–41. doi: 10.2174/1874613620130812003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Horvath T, Azman H, Kennedy GE, Rutherford GW. Mobile phone text messaging for promoting adherence to antiretroviral therapy in patients with HIV infection. Cochrane Database Syst Rev. 2012;3:CD009756. doi: 10.1002/14651858.CD009756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Free C, Phillips G, Galli L, Watson L, Felix L, Edwards P, et al. The effectiveness of mobile-health technology-based health behaviour change or disease management interventions for health care consumers: a systematic review. PLoS Med. 2013;10(1):e1001362. doi: 10.1371/journal.pmed.1001362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pellowski J, Kalichman S. Recent advances (2011-2012) in technology-delivered interventions for people living with HIV. Curr HIV/AIDS Rep. 2012;9(4):326–34. doi: 10.1007/s11904-012-0133-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Muessig KE, Pike EC, Legrand S, Hightow-Weidman LB. Mobile phone applications for the care and prevention of HIV and other sexually transmitted diseases: a review. J Med Internet Res. 2013;15(1):e1. doi: 10.2196/jmir.2301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ramanathan N, Swendeman D, Comulada WS, Estrin D, Rotheram-Borus MJ. Identifying preferences for mobile health applications for self-monitoring and self-management: focus group findings from HIV-positive persons and young mothers. Int J Med Inform. 2013;82(4):e38–46. doi: 10.1016/j.ijmedinf.2012.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Holstad M, Ofotokun I, Farber E, Logwood S, Hira R. There's an App for That! Promoting Antiretroviral Medication Adherence in Rural Georgia: The Music for Health Project. J Mob Technol Med. 2013;2(4):18. [Google Scholar]
- 23.Thursky KA, Mahemoff M. User-centered design techniques for a computerised antibiotic decision support system in an intensive care unit. Int J Med Inform. 2007;76(10):760–8. doi: 10.1016/j.ijmedinf.2006.07.011. [DOI] [PubMed] [Google Scholar]
- 24.Sayles JN, Hays RD, Sarkisian CA, Mahajan AP, Spritzer KL, Cunningham WE. Development and psychometric assessment of a multidimensional measure of internalized HIV stigma in a sample of HIV-positive adults. AIDS Behav. 2008;12(5):748–58. doi: 10.1007/s10461-008-9375-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Whiddett R, Hunter I, Engelbrecht J, Handy J. Patients’ attitudes towards sharing their health information. Int J Med Inform. 2006;75(7):530–41. doi: 10.1016/j.ijmedinf.2005.08.009. [DOI] [PubMed] [Google Scholar]
- 26.Deci EL, Ryan RM. Handbook of self-determination research. University Rochester Press; Rochester: 2002. [Google Scholar]
- 27.Deci el, Ryan RM., editors. A motivational approach to self: integration in personality. Nebraska Symposium on Motivation. 1991 [PubMed] [Google Scholar]
- 28.Deci EL, Ryan RM. Human autonomy. Efficacy, agency, and self-esteem. Springer; New york: 1995. pp. 31–49. [Google Scholar]
- 29.Deci EL, Ryan RM. The “What” and “Why” of Goal Pursuits: Human Needs and the Self-Determination of Behavior. Psychol Inq. 2000;11(4):227–68. [Google Scholar]
- 30.Williams GC, McGregor HA, Sharp D, Levesque C, Kouides RW, Ryan RM, et al. Testing a self-determination theory intervention for motivating tobacco cessation: supporting autonomy and competence in a clinical trial. Health Psychol. 2006;25(1):91–101. doi: 10.1037/0278-6133.25.1.91. [DOI] [PubMed] [Google Scholar]
- 31.Friedland J, Renwick R, McColl M. Coping and social support as determinants of quality of life in HIV/AIDS. AIDS Care. 1996;8(1):15–32. doi: 10.1080/09540129650125966. [DOI] [PubMed] [Google Scholar]
- 32.Fogg BJ. In: Persuasive technology: using computers to change what we think and do. Jonathan G, Jakob N, Stuart C, editors. Science & Technology Books; San Francisco: 2002. [Google Scholar]
- 33.Strauss A, Corbin J. Basics of qualitative research: techniques and procedures for developing grounded theory. Sage; Thousand Oaks: 1998. [Google Scholar]
- 34.Brown W, 3rd, Yen PY, Rojas M, Schnall R. Assessment of the Health IT Usability Evaluation Model (Health-ITUEM) for evaluating mobile health (mHealth) technology. J Biomed Inform. 2013;46(6):1080–7. doi: 10.1016/j.jbi.2013.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Sheehan B, Lee Y, Rodriguez M, Tiase V, Schnall R. A comparison of usability factors of four mobile devices for accessing healthcare information by adolescents. Appl Clin Inform. 2012;3(4):356–66. doi: 10.4338/ACI-2012-06-RA-0021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Winkelman WJ, Leonard KJ, Rossos PG. Patient-perceived usefulness of online electronic medical records: employing grounded theory in the development of information and communication technologies for use by patients living with chronic illness. J Am Med Inform Assoc. 2005;12(3):306–14. doi: 10.1197/jamia.M1712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Coiera E. When conversation is better than computation. J Am Med Inform Assoc. 2000;7(3):277–86. doi: 10.1136/jamia.2000.0070277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Wantland DJ, Holzemer WL, Moezzi S, Willard SS, Arudo J, Kirksey KM, et al. A randomized controlled trial testing the efficacy of an HIV/AIDS symptom management manual. J Pain Symptom Manag. 2008;36(3):235–46. doi: 10.1016/j.jpainsymman.2007.10.011. [DOI] [PubMed] [Google Scholar]
- 39.Schnall R, Wantland D, Velez O, Cato K, Jia H. Feasibility testing of a web-based symptom self-management system for persons living with HIV. J Assoc Nurses AIDS Care. 2014;25(4):364–71. doi: 10.1016/j.jana.2013.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Robbins RN, Brown H, Andries Ehlers B, Joska JA, Thomas KG, Rhonda Burgess M, et al. A smartphone app to screen for HIV-related neurocognitive impairment. J Mob Technol Med. 2014;3(1):23–36. doi: 10.7309/jmtm.3.1.5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Martínez-Pérez B, de la Torre-Díez I, López-Coronado M, Sainz-De-Abajo B. Comparison of mobile apps for the leading causes of death among different income zones: a review of the literature and app stores. J Med Internet Res. 2014;2(1):e1. doi: 10.2196/mhealth.2779. doi:10.2196/mhealth.2779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Lenhart A. [2010 March 28];Teens and Mobile Phones Over the Past Five Years: Pew Internet Looks Back: Pew Internet and American Life Project. 2009 Available from: http://www.pewinternet.org/Reports/2009/14-Teens-and-Mobile-Phones-Data-Memo/1-Data-Memo/5-How-teens-use-text-messaging.aspx?r=1.
- 43.Jackson CS, Gracia JN. Addressing health and health-care disparities: the role of a diverse workforce and the social determinants of health. Public Health Rep. 2014;129(Suppl 2):57–61. doi: 10.1177/00333549141291S211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Maguire M. Methods to support human-centred design. Int J Hum Comput Stud. 2001;55(4):587–634. [Google Scholar]
- 45.CDC's Division of Adolescent and School Health [26 Dec 2011];New York City: Bringing HIV/AIDS Prevention Education into the Spotlight Atlanta, GA. 2008 Available from: http://www.cdc.gov/healthyyouth/stories/pdf/2008/success_08_ny.pdf.
- 46.New York City Department of Health and Mental Hygiene AIDS deaths by year pre-1981-2003, New York City. [26 Dec 2011];HIV Epidemiology Program, HIV/AIDS Surveillance Statistics. 2003 Available from: www.nyc.gov/html/doh/downloads/pdf/ah/surveillance2003_ table2.pdf.
- 47.Centers for Disease Control and Prevention . HIV/AIDS Surveil-lance Report. Vol. 15. US Department of Health and Human Services, Centers for Disease Control and Prevention; Atlanta, GA: 2003. [26 Dec 2011]. 2004. Available from: http://www.cdc.gov/hiv/surveillance/resources/reports/2003report/. [Google Scholar]
- 48.New York City Department of Health and Mental Hygiene [26 Dec 2011];HIV/ AIDS Information New York. 2011 Available from: http://www.nyc.gov/html/doh/html/ah/ah.shtml.