Abstract
To assess problematic sexually explicit media (SEM) consumption, and to identify clinically meaningful cut-off points, we examined clinical correlates using the new Compulsive Pornography Consumption (CPC) scale among 1165 participating MSM. Building on scale practices in measuring compulsive sexual behavior, two cut-off points were identified. While most (76-80%) MSM do not report compulsive symptoms, about 16-20% report levels of problematic SEM consumption, including 7% with extreme scores consistent with DSM criteria for compulsive disorders. Demographic, sexual, and HIV risk differences were identified between the three groups. Researchers and clinicians are encouraged to consider using the CPC scale for comprehensive assessment of compulsive sexual behavior.
Keywords: pornography, sexually explicit media, MSM, compulsive pornography consumption, CPC
INTRODUCTION
In the US, there has been considerable scholarly and clinical research in compulsive sexual behavior, also termed sexual addiction(Carnes, 2001; Coleman, 1991; Raymond, Coleman, & Miner, 2003). The National Council on Sexual Addiction and Compulsivity defines sexual addiction/compulsivity as “engaging in persistent and escalating patterns of sexual behavior acted out despite increasing negative consequences to self and others” (The National Council on Sexual Addiction and Compulsivity, 2013). The Society for the Advancement of Sexual Health (SASH), which specializes in sexual addiction treatment, identifies over 110 clinicians and at least 7 treatment centers specializing in sex addiction treatment in the US, while hundreds more treat sexual sequelae as part of chemical dependency treatment and other therapy(The Society for the Advancement of Sexual Health).
Much of the research literature on sexual compulsivity has focused on HIV risk in men who have sex with men (MSM) (Benotsch, Kalichman, & Kelly, 1999; Benotsch, Kalichman, & Pinkerton, 2001; Grov, Parsons, & Bimbi, 2010; Kalichman & Rompa, 1995, 2001; Parsons, Severino, Grov, Bimbi, & Morgenstern, 2007). Two the most widely used scales are the 10-item Kalichman Sexual Compulsivity Scale (Benotsch et al., 1999; Kalichman & Rompa, 1995) and the 13-item subscale of the Coleman Compulsive Sexual Behavior Inventory (Coleman, Miner, Ohlerking, & Raymond, 2001), both validated for use on MSM samples (Coleman et al., 2010; Miner, Coleman, Center, Ross, & Rosser, 2007). A challenge for both scales, however, has been the lack of clearly defined cut-off points or criteria for sexual compulsivity. Coleman, a clinician and pioneer in the conceptualization and treatment of compulsive sexual behavior, has argued that diagnostically significant compulsive sexual behavior is likely rare, and probably less than 5% in the general population (personal communication). His view is supported empirically in a Swedish study which identified 5.6% of 1458 respondents to be sexually compulsive (Daneback, Ross, & Månsson, 2006), and published estimates of 3% to 6% prevalence in the US (Kuzma & Black, 2008). Kalichman, a research psychologist, and studies using the Kalichman scale, have employed a statistical approach, typically using either a one standard deviation above the mean as cut-off (Benotsch et al., 2001; Cooper, Delmonico, & Burg, 2000) or a top quintile cut-off (Benotsch et al., 2001; Grov et al., 2008; Kalichman, Greenberg, & Abel, 1997; Kalichman & Rompa, 1995; Parsons, Bimbi, & Halkitis, 2001). By this method, the top 16-20% of scorers in any sample are pre-defined as sexually compulsive.
Both scales were developed in the late 1990s or early 2000s, before widespread adoption of the Internet, which has made access to pornography accessible, affordable and anonymous (Cooper, 2002; Cooper et al., 2000). As a consequence, neither scale employs items specifically assessing pornography consumption and/or Internet sex addiction. As the first research on Internet addiction was being published (Young, 1998), Cooper (Cooper, Putnam, Planchon, & Boies, 1999) was among the first to investigate compulsive sexual behavior online including excessive Internet pornography consumption. In their study of sexual compulsivity in Sweden, Daneback, Ross and Månsson (Daneback et al., 2006) report a significant association between sexual compulsivity, time spent online, and time consuming pornography. Internet pornography addiction is a popular topic, both in the general media and in clinical treatment, and has resulted in a hearing about its dangers in the US Senate (Singel & Layden, 2004). Dr. Layden, co-director of the Sexual Trauma and Psychopathology Program at University of Pennsylvania testified, “Pornography addicts have a more difficult time recovering from their addiction than cocaine addicts, since … pornography images stay in the brain forever.” According to this view, the Internet is dangerous because it removes barriers in the delivery of pornography, making pornography much more ubiquitous.
As noted in the US Senate committee hearing, there is no consensus among mental health professionals about the dangers of pornography, or even agreement on the term “pornography addiction.” While proponents emphasize that Internet pornography may be additive (speculating it may change neural pathways) and addictive (as clinically defined), others have dismissed such notions as alarmist, noting fifty years of studies into the dangers of pornography which have largely failed to show significant negative effects (Rosser et al., 2012). There is also lack of consensus on terminology, with some viewing the term “pornography” and its derivative “porn” as prejudicial. Researchers are advocated to use more objective terms such as “sexually explicit media” or SEM.
In the absence of a brief screening instrument, clinicians have had to rely on subjective assessment or proxy measures to assess SEM addiction. One such approach is to use estimates from the early literature. For example, Cooper, Scherer, Boies, and Gordon (1999) reported 92% of men and women spend under eleven hours per week “in on-line sexual pursuits.” From this, some clinicians have used eleven hours as a clinical criterion to identify online sex addiction. There are at least four problems with this approach. First, the study which produced this estimate was conducted in 1998, before broadband, when most Americans were not online and before streaming online made SEM technologically accessible. Given the vastly different availability and speed of online access today, time estimates from the nineties are highly likely to be inaccurate. Second, the estimate is for all sexual activities online; it is likely that a much lower estimate is appropriate when examining compulsive SEM use. Third, research by Grov, Bamonte, Fuentes, Parsons, Bimbi and Morgenstern (2008) has demonstrated that proxy measures such as time spent online is a poor predictor of sexual compulsivity in MSM. Fourth, as reflected in the Pew Research Internet Project, we know racial/ethnic minorities, sexual minorities, rural residents, and lower socioeconomic groups access the Internet using different technologies, which will bias time estimates. It is ethically problematic to use tools which will discriminate against minorities and the poor. For all these reasons, a brief screening instrument to assess compulsive SEM use is needed both for research and clinical assessment.
Research into compulsive pornography/SEM consumption (CPC) has been hampered by the lack of validated instruments or accepted criteria for clinical screening. To address this gap, as part of the first NIH-funded study to examine the relationship between pornography consumption and HIV risk behavior in men who have sex with men, we developed a short assessment instrument to screen for CPC. In a companion paper, we report the psychometric qualities of the CPC scale. Here, we report the clinical findings and implications for research.
Six items were developed to assess obsessive thoughts and/or compulsive behaviors based on definitions in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5, American Psychiatric Association, 2013). The DSM-5 characterizes obsessive-compulsive disorders by the presence of recurrent and persistent thoughts, urges, or images experienced as intrusive and unwanted (termed “obsessions”); and/or repetitive behaviors or mental acts that the individual feels driven to perform to reduce anxiety or distress (termed “compulsions”) (American Psychiatric Association, 2013). These were translated into survey items to assess the key criteria. Other supporting criteria – that the obsessions or compulsions are time-consuming, cause clinically significant distress, and/or impair social, occupational or other important areas of functioning – were used to validate the key presenting characteristics.
To the best of our review, this is the first study to assess compulsive SEMuse in men who have sex with men (MSM). The earliest instruments of online sex addiction (e.g., Delmonico and Miller, 2003) did not differentiate between using the Internet for sex seeking, sexual information seeking or pornography. In the Sexual Addiction Screening Test (SAST), developed by Carnes and O’Hara in 2002, two of twenty-eight items ask about online pornography but they do not comprise a separate scale (Carnes, Green and Carnes, 2010). The 34-item Cyber-Pornography Use Inventory (Grubbs, Sessoms, Wheeler and Folk, 2010) was the first published instrument to assess pornography addiction. However, it was designed to assess young male students at Christian Colleges for pornography addiction, “even though most of them do not fall anywhere within the diagnostic range required to diagnose one as a sexual compulsive.” Normed on 94 male and 51 female undergraduate students (mean age=19years), the items are tailored to the college population (e.g., “I have gotten up earlier or gone to bed later than my roommates to view pornography”), making it unsuitable for use in the broader population. Reid, Li, Gilliand, Stein and Fong (2011) published their Pornography Consumption Inventory (PCI) which assessed motivations for pornography use among hypersexual men seeking treatment, 90 percent of whom reported being heterosexual. This 15-item scale yields four factors – emotional avoidance, sexual curiosity, excitement seeking and sexual pleasure – but does not assess the compulsive/addictive nature of the behavior, nor provide any information on pornography consumption behavior. Recently, a 12-item Problematic Pornography Use Scale (Kor, Zilcha-Mano, Fogel, Mikulincer, Reid and Potenza, 2014) scale has been published assessing four factors: distress, excessive use, control difficulties and use for escape and/or avoidance of negative emotions. Normed in Hebrew on an Israeli general population, it uses DSM criteria to assess preoccupation and compulsivity. Its psychometric performance in English has not been studied, and its length may be too long and detailed to be a brief screening instrument. Of relevance to our study, it found only a moderate correlation between the problematic pornography consumption scores and hypersexuality disorder (r=.68; p<.001).
To situate this paper in the broader literature on gay pornography and HIV risk, there have been five recent studies of pornography published investigating whether exposure to sexually explicit media (SEM) increases HIV risk behavior in MSM (two by our team in the US and Norway, and three others, all in the US) (Eaton, Cain, & Cherry, 2012; Nelson et al., 2014; Rosser, Wilkerson, Grey, Iantaffi, & Smolenski, 2011; Stein, Silvera, Hagerty, & Marmor, 2012; Træen et al., 2013). Since they show consistent findings, we will use the estimates from our parent study to contextualize research on CPC in MSM.
The purpose of the Sexually Explicit Media (SEM-I) Study was to investigate a hypothesized relationship between SEM consumption and HIV risk behavior in MSM, while advancing research on the effects of SEM/pornography. In the quantitative online survey phase of study, almost all (98.5%) of the 1391 MSM participants reported watching gay sexually explicit media (SEM); reported very high consumption (at 24.9 minutes average viewing per day), and mainly consumption online (Rosser, Smolenski, Erickson, Iantaffi, Brady, Galos, et al., 2013). While overall SEM consumption was not related to HIV risk, a preference for and greater consumption of bareback SEM was associated with increased unprotected anal intercourse with multiple male partners (Rosser, Smolenski, Erickson, Iantaffi, Brady, Galos, et al., 2013). In addition to these main findings, we have published a new model on how SEM consumption influences behavior (Wilkerson et al., 2012), and a series of papers advancing research on various aspects of SEM consumption in MSM (Galos, Smolenski, Grey, Iantaffi, & Rosser, 2013; Hald, Smolenski, & Rosser, 2013; Hald, Træen, Noor, Iantaffi, Galos, et al., 2014; Hald, Træen, Noor, Iantaffi, & Rosser, 2014; Rosser et al., 2012; Rosser, Smolenski, Erickson, Iantaffi, Brady, Galos, et al., 2013; Rosser, Smolenski, Erickson, Iantaffi, Brady, Grey, et al., 2013; Sullivan, Grey, & Rosser, 2013; Træen et al., 2013; Wilkerson et al., 2012; Wilkerson, Iantaffi, Smolenski, Horvath, & Rosser, 2013)
In this paper, we examine the clinical evidence for CPC. In our analysis, we were guided by the following three aims: (1) to identify appropriate clinical cut-off points for the scale in order to estimate the prevalence of CPC in MSM; (2) to identify clinically relevant co-factors of CPC; and (3) through multivariable analysis, to identify how MSM with CPC differ from MSM without.
METHODS
Study Samples
The SEM (Rosser, Smolenski, Erickson, Iantaffi, Brady, Galos, et al., 2013) Study was conducted in three phases: (1) a formative research phase involving online synchronous focus groups to understand participants’ SEM use; (2) a 7-day, test–retest reliability study to develop and assess new measures; and (3) a large quantitative online survey to study effects. For all phases of the study, banner advertisements were placed on 148 gay-oriented websites through the Gay Ad Network to identify potential participants. Eligibility criteria included self-identification as male, at least 18 years of age, a report of at least one male sexual partner in the last 5 years, and residing in the United States or one of its territories. For the main survey, conducted between May and August 2011, participants were quota-sampled by race/ethnicity to increase diversity. In the main survey, a total of 5,201 MSM met the behavioral eligibility criteria; 3,338 MSM were excluded because their racial/ethnic category had filled, leaving a total of 1,863 MSM who met all eligibility criteria. Of these, 1,479 (79.4%) consented to participate in the study and provided information on exposure to SEM. All surveys underwent a standard de-duplication, cross-validation and data cleaning protocol developed by our team to exclude duplicate surveys, and invalid participants with impossible or nonsensical data patterns.(Konstan, Rosser, Ross, Stanton, & Edwards, 2005) This identified 88 surveys for exclusion. We further constrained this analysis to participants who completed all items on the CPC scale, leaving a final study sample of 1,165 participants. All study protocols and consent procedures were approved by the Institutional Review Board at the investigators’ home institution.
Participant Characteristics
Socio-demographic characteristics of the main study sample are presented in Table 1. Similar to previous work with Internet based samples, most (68.1%) participants were younger than 35 years old. Unlike other Internet based samples, most (57.0%) were MSM of Color. The largest single racial group (43.0%) identified their race as non-Hispanic white, almost half were well-educated (49.4% had a college degree or greater), 83.9% lived in urban/suburban areas; 91.4% were HIV-negative (by self-report), 90.9% had not been diagnosed with a sexually transmitted infection (STI) in the past 12 months, and about half (51.2%) were single. In terms of experience with SEM, 41.7% reported first seeing SEM before age 13, and 58.3% after that; about half watched less than 2.9 hours of SEM per week; most (65.4%) watched SEM alone, but one-in-three participants reported watching it with others, and only one in four reported paying for SEM in the last month (see Table 2).
Table 1.
Demographic characteristics of the SEM study participants by Compulsive Pornography Consumption (CPC) scale score (N=1165 MSM) 1
| Variable | Total n (%) |
No n (%) |
Problemat ic n (%) |
Compulsiv e n (%) |
χ2(df) |
p- value |
|---|---|---|---|---|---|---|
|
|
||||||
| 917 (78.7) | 165 (14.2) | 83 (7.1) | ||||
|
|
||||||
| Age: | 23.23(6) | 0.001 | ||||
| 18 – 24 | 422 (36.2) | 309 (33.7) | 74 (44.8) | 39 (46.9) | ||
| 25 – 34 | 371 (31.9) | 286 (31.2) | 58 (35.2) | 27 (32.5) | ||
| 35 – 44 | 184 (15.8) | 156 (17.1) | 20 (12.1) | 8 (9.6) | ||
| ≥45 | 188 (16.1) | 166 (18.1) | 13 (7.9) | 9 (10.8) | ||
| Race/ethnicity: | 13.86(8) | 0.08 | ||||
| NH white | 501 (43.0) | 406 (44.3) | 61 (36.9) | 34 (40.9) | ||
| NH black | 125 (10.7) | 98 (10.6) | 15 (9.1) | 13 (15.7) | ||
| Latino | 333 (28.6) | 255 (27.8) | 57 (34.6) | 21 (25.3) | ||
| Asian/PI | 94 (8.1) | 65 (7.1) | 19 (11.5) | 10 (12.1) | ||
| Other2 | 112 (9.6) | 94 (10.3) | 13 (7.9) | 5 (6.0) | ||
| Education: | 3.20(2) | 0.20 | ||||
| Less than college degree |
590 (50.6) | 452 (49.3) | 91 (55.2) | 47 (56.6) | ||
| College degree or greater |
575 (49.4) | 465 (50.7) | 74 (44.8) | 36 (43.4) | ||
| Residence: | 22.29(4) | <0.001 | ||||
| Rural/small town | 188 (16.1) | 152 (16.6) | 23 (13.9) | 13 (15.7) | ||
| Medium size/suburb |
599 (51.5) | 440 (48.0) | 107 (64.9) | 52 (62.6) | ||
| Large city | 377 (32.4) | 324 (35.4) | 35 (21.2) | 18 (21.7) | ||
| Self-reported HIV status: |
1.18(2) | 0.55 | ||||
| Positive | 100 (8.6) | 83 (9.1) | 11 (6.7) | 6 (7.2) | ||
| Negative3 | 1064 (91.4) | 834 (90.9) | 153 (93.3) | 77 (92.8) | ||
| Non-HIV STI4 | 1.04(2) | 0.59 | ||||
| No | 1057 (90.9) | 830 (90.6) | 149 (90.8) | 78 (94.0) | ||
| Yes | 106 (9.1) | 86 (9.4) | 15 (9.2) | 5 (6.0) | ||
| In a long-term relationship |
8.66(2) | 0.013 | ||||
| No | 596 (51.2) | 458 (58.7) | 91 (71.1) | 47 (68.1) | ||
| Yes | 381 (32.7) | 322 (41.3) | 37 (28.9) | 22 (31.9) | ||
| Missing | 188 (16.1) | |||||
| Member of a Gay Organization |
1.85(2) | 0.39 | ||||
| No | 909 (78.9) | 711 (78.4) | 135 (82.8) | 63 (76.8) | ||
| Yes | 243 (21.1) | 196 (21.6) | 28 (17.2) | 19 (23.7) | ||
Note: NH= Non-Hispanic; PI= Pacific Islander; SEM= Sexually Explicit Media; STI= Sexually Transmitted Infection;
Due to missing values N=977~1165
Other: Native American (1.9%); Multi Race (7.7%)
Negative: Self-reported negative (77.1%)/Unsure (12.9%)/Don’t know (1.3%)
In the past 12 months
Table 2.
SEM consumption, psychosocial and sexual behavior of the SEM study participants by Compulsive Pornography Consumption (CPC) scale score (N=1165 MSM)
| Variable | Total n (%) |
No n (%) |
Problemat ic n (%) |
Compulsive n (%) |
χ2/F- test(df) |
p- value |
|---|---|---|---|---|---|---|
|
|
||||||
| 917 (78.7) | 165 (14.2) | 83 (7.1) | ||||
|
|
||||||
| SEM use: | ||||||
| Age at first SEM use |
1.79(2) | 0.41 | ||||
| 13 years or younger | 482 (41.7) | 372 (40.7) | 72 (45.0) | 38 (46.3) | ||
| Older than 13 years | 673 (58.3) | 541 (59.3) | 88 (55.0) | 44 (53.7) | ||
| Amount of SEM viewed, hr/wk |
31.02(2) | <0.001 | ||||
| 1 – 2.9 | 596 (51.5) | 508 (55.8) | 58 (35.4) | 30 (36.6) | ||
| 3.0+ | 561 (48.5) | 403 (44.2) | 106 (64.6) | 52 (63.4) | ||
| Watching SEM alone |
3.91(2) | 0.14 | ||||
| No, with company | 400 (34.6) | 326 (35.8) | 53 (32.3) | 21 (25.6) | ||
| Yes, alone | 756 (65.4) | 584 (64.2) | 111 (67.7) | 61 (74.4) | ||
| Masturbated at public place while watching SEM |
0.31(2) | 0.86 | ||||
| No, | 167 (37.6) | 130 (38.2) | 25 (34.7) | 12 (37.5) | ||
| Yes, at public place | 444 (62.4) | 210 (61.8) | 47 (65.3) | 20 (62.5) | ||
| Dollar spent on SEM |
1.47(2) | 0.48 | ||||
| None | 870 (74.7) | 685 (74.7) | 127 (76.9) | 58 (69.9) | ||
| $1 or more | 295 (25.3) | 232 (25.3) | 38 (23.1) | 25 (30.1) | ||
| Number of windows open while watching SEM |
16.74(2) | <0.001 | ||||
| 1-2 | 642 (57.4) | 537 (60.4) | 66 (44.0) | 39 (48.7) | ||
| More than 2 | 477 (42.6) | 352 (39.6) | 84 (56.0) | 41(51.3) | ||
| Behavioral: | ||||||
| Drug use in the last 90 days |
0.421 | |||||
| No | 1069 (91.9) | 842 (91.9) | 148 (90.2) | 79 (95.2) | ||
| Yes, once a week | 94 (8.1) | 74 (8.1) | 16 (9.8) | 4 (4.8) | ||
| Heavy alcohol use in the last 30 days |
0.031 | |||||
| No | 840 (92.0) | 676 (92.6) | 106 (86.2) | 58 (96.7) | ||
| Yes | 73 (8.0) | 54 (7.4) | 17 (13.8) | 2 (3.3) | ||
| Age at first sex with a male |
8.79(2) | 0.01 | ||||
| 13 years or younger | 235 (20.4) | 201 (22.1) | 19 (11.9) | 15 (18.1) | ||
| Older than 13 years | 919 (79.6) | 711 (77.9) | 140 (88.1) | 68 (81.9) | ||
| History of child sexual abuse |
4.22(2) | 0.12 | ||||
| No | 928 (81.5) | 733 (81.6) | 122 (77.2) | 73 (87.9) | ||
| Yes | 211 (18.5) | 165 (18.4) | 36 (22.8) | 10 (12.1) | ||
| Hours spent online partner seeking |
15.66(2) | <0.001 | ||||
| 3 hours or less | 847 (74.1) | 695 (76.6) | 98 (62.8) | 54 (66.7) | ||
| More than 3 hours | 297 (25.9) | 212 (23.4) | 58 (37.2) | 27 (33.3) | ||
| Number of sex partners in lifetime |
6.03(2) | 0.04 | ||||
| 20 or less | 591 (52.7) | 450 (50.8) | 92 (58.9) | 49 (61.3) | ||
| More than 20 | 530 (47.3) | 435 (49.2) | 64 (41.1) | 31 (38.7) | ||
| Number of partners in the last 90 days |
0.45(2) | 0.80 | ||||
| 3 or less | 701 (60.9) | 558 (61.3) | 92 (58.6) | 51 (62.2) | ||
| More than 3 | 449 (39.1) | 353 (38.7) | 65 (41.4) | 31 (37.8) | ||
| Engage in UAI with casual partners in the last 90 days |
3.56(2) | 0.17 | ||||
| No | 828 (72.2) | 662 (72.8) | 103 (66.5) | 63 (76.8) | ||
| Yes | 319 (27.8) | 248 (27.2) | 52 (33.5) | 19 (23.2) | ||
| Psycho-social: | ||||||
| Sexual identification |
5.36(2) | 0.06 | ||||
| Gay/Homosexual | 957 (82.6) | 765 (83.7) | 132 (80.5) | 60 (74.1) | ||
| Other2 | 202 (17.4) | 149 (16.3) | 32 (19.5) | 21 (25.9) | ||
| Outness | 36.08(8) | <0.001 | ||||
| Not out at all | 39 (3.4) | 24 (2.6) | 6 (3.7) | 9 (10.9) | ||
| Out to few | 182 (15.7) | 129 (14.1) | 33 (20.1) | 20 (24.4) | ||
| Out to half | 115 (9.9) | 87 (9.5) | 20 (12.2) | 8 (9.8) | ||
| Out to most | 265 (22.8) | 206 (22.5) | 36 (21.9) | 23 (28.1) | ||
| Out to all | 560 (48.2) | 469 (51.3) | 69 (42.1) | 22 (26.8) | ||
| Internalized Homonegativity |
46.31 (2,1161) |
<0.001 | ||||
| Mean ± SD | 2.51±1.28 | 2.33±1.20 | 3.10±1.25 | 3.33±1.53 | A≠B3 A≠C |
|
| CSBI | 150.05 (2,1161) |
<0.001 | ||||
| Mean ± SD | 2.05±0.76 | 1.87±0.65 | 2.60±0.75 | 2.91±0.86 | A≠B A≠C B≠C |
|
| PANAS, positive | 3.20 | 0.05 (2,1160) |
||||
| Mean ± SD | 3.40±0.82 | 3.42±0.82 | 3.35±0.75 | 3.20±0.92 | ||
| PANAS, negative | 20.75 (2,1160) |
<0.001 | ||||
| Mean ± SD | 2.19±0.88 | 2.11±0.83 | 2.54±0.99 | 2.45±0.95 | A≠B A≠C |
|
| PCES | 1.92 (2,1162) |
0.14 | ||||
| Mean ± SD | 0.97±0.63 | 0.99±0.61 | 0.96±0.63 | 0.84±0.86 | ||
| Condom use self- efficacy |
9.20 (2,1146) |
<0.001 | ||||
| Mean ± SD | 4.01±1.00 | 4.07±1.00 | 3.76±0.92 | 3.77±1.07 | A≠B A≠C |
|
| Sexual Confidence | 14.65 (2,1158) |
<0.001 | ||||
| Mean ± SD | 3.43±1.00 | 3.51±1.00 | 3.16±0.93 | 3.08±0.97 | A≠B A≠C |
|
| Sexual Satisfaction | 22.14 (2,1154) |
<0.001 | ||||
| Mean ± SD | 2.85±1.15 | 2.97±1.16 | 2.43±0.99 | 2.42±1.08 | A≠B A≠C |
|
Note: SEM=Sexually Explicit Material; IH = Internalized Homonegativity; CSBI = Compulsive Sexual Behavior Inventory; PCES= Effects of Pornography Consumption Scale; PANAS = Positive and Negative Affect Schedule; SD= Standard deviation;
One-way analysis of variance with Scheffe correction used to compare the means;
p-value for Fisher’s Exact test
Other: Bisexual (11.7%)/Straight (0.5%)/Same-gender loving (1.2%)/ Queer (2.1%)/Other (1.8%)
A: No; B: Problematic and C: Compulsive
Measures
Participants completed a web-based survey designed to explore the impact of sexually explicit material on HIV-related risk behaviors. The test battery collected self-reported data on basic demographics, SEM consumption and preferences in SEM, sexual behavior, use of condoms; current alcohol and drug use; sexuality and role in sex; long-term relationships (LTRs); openness as gay and bisexual men; mental health; internalized homonegativity; HIV and STI status, and sexual risk taking including number of partners and unprotected anal intercourse. The average completion time for the survey was 42 minutes, and participants were compensated $25.
Compulsive Pornography Consumption (CPC) Scale
The CPC scale is comprised of five items (Noor, Rosser, & Erickson, 2014). Two items assess obsessive thinking about pornography: (1) I thought of pornography when I was trying to focus on other things; and (2) I was upset because I could not stop thinking about pornography; and three items assess compulsive pornography behavior: (3) I watched pornography even though I did not want to; (4) It was necessary for me to watch pornography to feel at ease; and (5) I could only have an orgasm when watching pornography. Participants answer each item using a seven-point Likert-type scale, with a response range of 1 = “Very frequently”, 4 = “Sometimes”, and 7 = “Never”. Each item is reverse-scored so that higher scores indicate more potentially problematic behavior (30 point range: 5= no CPC to 35= severe CPC). Cronbach’s α in this sample was 0.85. Two-sided 95% confidence intervals (CI) for the Cronbach’s alpha was 0.84-0.86.
To identify a clinically meaningful cut-off, we considered three different approaches to defining cut-off points: (a) Subjectively meaningful cut-off points: Anyone reporting a mean score of symptoms of CPC on 50% or more of the time (i.e. a score of 20 or above) is by definition reporting CPC symptoms most of the time, and those reporting an average score of 30 or more would appear to be rarely, if ever, symptom free; (b) Graphically-defined cutoff points: If a subgroup of participants have CPC, we reasoned it should be observable as an excess of participants reporting extreme scores. Thus, we hypothesized we should see an observable “bump” in scores at the extreme end of the graph; and (c) Statistically derived cutoff points: Our third approach was to mirror the methods of Kalichman, who uses an a priori 20% upper bound to identify MSM at risk of compulsive sexual behavior, and the expert advice of Coleman, who considers a maximum of 5% of the population as likely experiencing clinically-diagnosable compulsive behavior. Having identified candidate cut-off points, we triangulated the data to identify the actual clinical cut-off points.
Exposure to SEM
By exposure to SEM, the study consistently referred to gay SEM except for age at first SEM exposure where the study referred to general SEM use. Accordingly, exposure measures to SEM included the age at which participants began consuming SEM, collected as a continuous item and categorized here using the median for comparison groups. A second item was used to ask participants about their preference for condom use during anal intercourse in SEM, with three nominal response options: (i) no condoms; (ii) condoms; and (iii) no preference. Four items were used to assess the frequency of accessing SEM through the following four sources: (i) magazines; (ii) video/DVD; (iii) Internet on a computer; and (iv) Internet through a phone or mobile device. Response options to each of these items ranged from 1 = “Not at all” to 6 = “More than once a day.” One item asked participants to report the typical duration of use of SEM when it was used in the last 90 days, with response categories including: (i) 1– 15 minutes; (ii) 16–30 minutes; (iii) 31–45 minutes; (iv) 46–60 minutes; (v) between 1 and 1 1/2 hours; (vi) between 1 1/2 and 2 hours; and (vii) more than 2 hours. Finally, frequency and duration measures of SEM consumption in the last 3 months were combined to create an index of the hours per week dedicated to SEM consumption.
Compulsive Sexual Behavior Inventory (CSBI)
The “control” subscale of the CSBI was used to assess compulsive, or out-of-control sexual behavior (Coleman et al., 2001). The subscale comprised 13 items measured using five-point Likert-type response scales with 1 = “Very frequently”, 3=”Occasionally” and 5 = “Never”. The valence of the arithmetic mean was reversed so that higher scores indicate a stronger manifestation of the construct. Cronbach’s α in this sample was 0.90 (95% CI: 0.89-0.91).
Positive and Negative Affect Schedule (PANAS)
The 10-item short-form PANAS (Thompson, 2007) was used to assess positive and negative affect in the last 90 days. All items were responded to using a five-point Likert-type index, with 1 = “Very little or not at all,” and 5 = “Extremely.” Cronbach’s alpha was 0.82 (95% CI: 0.80-0.83) for positive affect and 0.87 (95% CI: 0.86-0.88) for negative affect in this sample.
Internalized Homonegativity (IH)
The revised Reactions to Homosexuality Scale (Smolenski, Diamond, Ross, & Rosser, 2010) was used to measure internalized homonegativity. The measure consisted of seven items answered using a seven-point Likert-type scale ranging from 1 = “Strongly disagree” to 7 = “Strongly agree.” A sample item is, “Social situations with gay men make me feel uncomfortable.” A higher aggregated score indicated greater internalized homonegativity. Alpha reliability for this scale in this sample was 0.82 (95% CI=0.80-0.83).
The Pornography Consumption Effect Scale (PCES)
First person effect of SEM consumption was measured using the seven item PCES (Hald et al., 2013). Participants were asked to answer two response sets for each item: (i) a five-point Likert-type item on the magnitude of the effect, if any, with a response range of 1 = “Decreased”, 3 = “No effect”, and 5 = “Increased”; and (ii) a five-point Likert-type item on the valence of the effect, if any, with a response range of 1 = “Very bad”, 3 = “Neither bad nor good”, and 5 = “Very good.” Following Hald et al (2013), composites of the two responses for each item were developed by first recoding the magnitude to range from −2 to 2, with −2 indicating a strong reduction and 2 indicating a strong increase. Second, the information on valence (bad or very bad and good or very good) was used to determine if the reduction or increase on any item was considered positive or negative. As an example, a magnitude of −1 remained −1 if the valence was reported as “bad,” and a magnitude of −1 became 1 if the valence was reported as “good”. This resulted in a single index ranging from −2 = “Strong, negative effect” to 2 = “Strong, positive effect” with 0 indicating neither a positive nor a negative effect. Participants were assigned a zero if they reported either no effect in terms of magnitude or no effect in terms of valence. Cronbach’s α of this measure in this sample was 0.80 (95% CI=0.78-0.82).
Condom Use Self-Efficacy
We used a 13 item condom use self-efficacy scale (Marin, Gomez, Tschann, & Gregorich, 1997) to assess the perceived condom use confidence of study participants. Items were measured on five-point Likert-type scale ranging from 1 = “Definitely not” to 5 = “Definitely yes”. We used the arithmetic mean of the items to create a composite measure. Higher scores on the measure indicate greater condom use confidence. Cronbach’s alpha was 0.96 (95% CI: 0.95-0.96) in this sample.
Sexual Confidence and Sexual Satisfaction
The sexual confidence and sexual satisfaction subscales of the Multidimensional Sexuality Questionnaire (Snell, Fisher, & Walters, 1993) were used to assess the perceived sexual confidence and satisfaction of study participants. Each measure included 5 items. Items were measured on five-point Likert-type scale ranging from 1 = “Not at all like me” to 5 = “Extremely like me.” We used arithmetic mean of the items to create a composite measure. Higher scores on the measures indicate greater sexual confidence and satisfaction. Cronbach’s alpha was 0.91 (95% CI: 0.91-0.92) for sexual confidence measure and 0.93 (95% CI: 0.92-0.94) for sexual satisfaction measure in this sample.
Sexual Risk Behavior
A sexual behavior battery investigated sexual risk behavior of the participants. Participants were asked to report age at first sexual encounter as well as number of male sexual partners in lifetime and in the last 90 days. The age at which participants first had sex with a male partner was collected as a continuous item and categorized here using the median for comparison groups. The two male partner counts were dichotomized by 75/25 split to compare participants clearly engaging in high-risk behavior with men at no-to-low risk. Participants were also asked two items relating to the number of casual male sex partners in the last 90 days with whom they had engaged in unprotected receptive and unprotected insertive anal intercourse. To compare participants who engaged in unprotected anal intercourse (UAI) with those who did not on the CPC scale, participants who reported one or more unprotected anal intercourse casual male partner either as receptive or insertive in the last 90 days were classified as engaging in UAI with a casual male partner. Participants who reported 0 counts to both items were classified as not engaging in UAI with a causal partner. We identified a participant as a victim of sexual abuse if the participant had sex before reaching the age of eighteen with a male partner who was four or more years older than the participant.
Other Variables
Demographic variables included age, education, race/ethnicity, long-term relationship status (90+ days), sexual identification, alcohol and drug use, history of any sexually transmitted infections (STI) and HIV serostatus. Participants’ sexual identity was measured by asking, “Do you identify as…” with response options being gay/homosexual, bisexual, heterosexual, or other (with a space to write in their response). How out a man is about his homosexuality was assessed by asking, “How ‘out’ are you about your sexual attraction to other men?” with response options ranging from 1= “Not ‘out’ at all” to 5= “‘Out’ to all or almost all people I know”. A higher score indicated greater outness. Participants were asked to provide information about their alcohol consumption and drug use. We assessed the drinking pattern by using the item, “In the past thirty (30) days, how many times did you have five (5) or more drinks in one sitting?” At analysis, “heavy alcohol use” was defined as drinking 5 or more drinks in one sitting twice or more in a week (Jones-Webb, Smolenski, Brady, Wilkerson, & Rosser, 2013). Participants also provided information on the frequency of (1= “Not at all”, 2= “Less than monthly”, 3= “Once a month”, 4= “Once a week” 5= “Daily”) using marijuana/hashish, cocaine, uppers (methamphetamines, crystal, crank), downers (valium, sedatives), club drugs (GHB, ecstasy), opioids (heroin, Vicodin), erectile enhancement drugs (e.g., Viagra, Cialis) and poppers (i.e., amyl nitrite) in the last 90 days. At analysis, we defined “drug use” as using one of the drugs once or more in a week.
Data Analysis
Summary statistics were used to describe the study sample and to calculate the prevalence of compulsive pornography use among the participants. We used Pearson’s chi-square test (for categorical) and one-way analysis of variance (for continuous variables) to examine if compulsive pornography users differ by selected personal characteristics. We also examined if the groups differed by behavioral and psycho-social factors.
Our goal was to assess the association between compulsive pornography use and personal, behavioral, and psycho-social factors. We wanted to assess the relative contribution of each factor as well as the block of factors on pornography use. Therefore, we used a block regression strategy. Three separate multiple multinomial regression models were run to identify factors associated with compulsive use (0= No, 1= Problematic, 2= Compulsive use). Personal characteristics that were significant (p ≤ 0.10) at the bivariate level were entered into the first multiple multinomial regression model. In the second multiple multinomial regression model, we included behavioral variables that were significant (p ≤ 0.10) at the bivariate level. In the third model we included the significant (p ≤ 0.10) psycho-social variables. Finally, in the fourth model we included all the variables that were significant (p ≤ 0.05) in the first three regression models. All statistical tests were two-tailed, and all analyses were conducted using Stata 11 software.(Jones-Webb et al., 2013)
RESULTS
Aim 1: Clinical cut-off points for the CPC scale
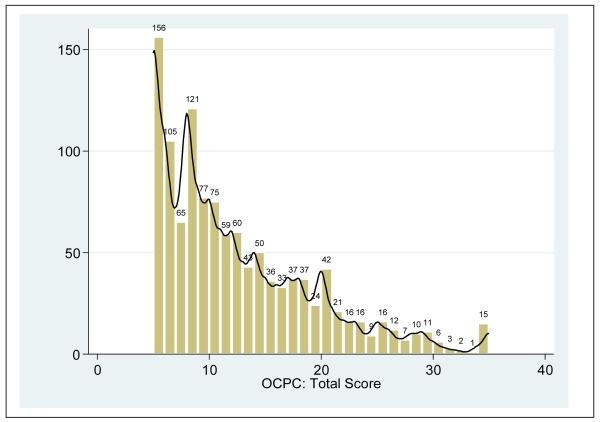
For the subjectively meaningful cut-off point, 16% of participants scored 20 or above, while the cut-off point for the top 20% was 17. Using the graphical approach, as shown in Figure 1, there is a clear “excess” in scores above 24 (representing 7% of participants). This corresponds approximately to Coleman’s expert opinion of around 5% of the population having clinically defined compulsive sexual behaviors. Triangulating these approaches, we identified three groups: (a) those scoring 5-17 who report little to no symptoms of CPC, which we term the “no” (evidence of CPC) group; (b) those scoring 18-24 who report, on average, symptoms of CPC on 50% or more occasions, which we term the “problematic” or “potentially CPC” group; and the top segment (scores of 25 or more), which we term the “extreme” or “CPC” group.
Figure 1.
Frequency of Compulsive Pornography Consumption (CPC) scale scores with kernel density plot among the SEM study participants (N=1165 MSM)
Aim 2: Co-factors of CPC
Bivariate comparisons of CPC by selected personal, behavioral and psycho-social measures are detailed in Table 1 and Table 2. In terms of demographics, the three CPC groups differed by age, residence and relationship status. Behaviorally, both the problematic and CPC groups reported consuming more SEM (measured in hours per week), spent more hours seeking sexual partners, and were more likely to report heavy alcohol use, earlier age of sexual debut and more than twenty lifetime sexual partners. They also scored higher on internalized homonegativity and compulsive sexual behavior. The CPC group scored lower on the following scales: positive affect schedule, condom use self-efficacy, sexual confidence and sexual satisfaction.
Aim 3: Characteristics of MSM with CPC compared to other MSM
Results of the three preliminary simple (multiple) multinomial regression models are presented in Table 3. Demographically, the problematic group had lower odds of being older (OR=0.45, 95% CI: 0.22-0.93) and lower odds of being in a long-term relationship (OR=0.59, 95% CI: 0.39-0.92) than the no-CPC group. Behaviorally, the CPC-group was more likely to spend over three hours watching SEM per week than the no-CPC group (OR=2.22, 95% CI: 1.23-4.00). However, the CPC-group had lower odds of reporting more than twenty lifetime sexual partners than the no-CPC group (OR=0.50, 95% CI: 0.28-0.89).
Table 3.
Adjusted Models of Compulsive Pornography Consumption by Personal, Behavioral and Psychosocial Measures
| No vs. Problematic | No vs. Compulsive | Problematic vs. Compulsive |
|||||||
|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||
| OR | 95% CI | p | OR | 95% CI | p | OR | 95% CI | p | |
|
|
|||||||||
| Model 1: Personal | |||||||||
| Age | |||||||||
| 18 – 24 | Ref | ||||||||
| 25 – 34 | 1.11 | 0.71-1.72 | 0.65 | 0.98 | 0.55-1.75 | 0.94 | 0.88 | 0.45-1.74 | 0.72 |
| 35 – 44 | 0.67 | 0.36-1.26 | 0.21 | 0.53 | 0.22-1.27 | 0.15 | 0.79 | 0.29-2.19 | 0.66 |
| ≥45 | 0.45 | 0.22-0.93 | 0.03 | 0.59 | 0.25-1.38 | 0.22 | 1.32 | 0.46-3.82 | 0.61 |
| Race/ethnicity | |||||||||
| NH white | Ref | ||||||||
| NH black | 0.91 | 0.45-1.81 | 0.78 | 1.58 | 0.76-3.30 | 0.21 | 1.75 | 0.68-4.47 | 0.23 |
| Latino | 1.24 | 0.79-1.95 | 0.34 | 0.88 | 0.47-1.63 | 0.69 | 0.71 | 0.34-1.45 | 0.35 |
| Asian/PI | 1.38 | 0.67-2.80 | 0.38 | 1.20 | 0.47-3.09 | 0.70 | 0.87 | 0.29-2.61 | 0.81 |
| Other | 0.71 | 0.33-1.53 | 0.38 | 0.57 | 0.19-1.70 | 0.32 | 0.81 | 0.22-2.89 | 0.74 |
| Residence: | |||||||||
| Rural/small town | Ref | ||||||||
| Medium size/suburb | 1.52 | 0.87-2.66 | 0.14 | 1.86 | 0.84-4.09 | 0.12 | 1.22 | 0.48-3.05 | 0.67 |
| Large city | 0.76 | 0.40-1.44 | 0.40 | 1.02 | 0.42-2.47 | 0.95 | 1.35 | 0.48-3.83 | 0.57 |
| In a long-term relationship | |||||||||
| No | Ref | ||||||||
| Yes | 0.59 | 0.39-0.90 | 0.02 | 0.70 | 0.41-1.21 | 0.20 | 1.18 | 0.62-2.26 | 0.61 |
|
| |||||||||
| Model 2: Behavioral | |||||||||
| Amount of SEM viewed, hr/wk | |||||||||
| 1 – 2.9 | Ref | ||||||||
| > 2.9 | 2.07 | 1.34-3.20 | 0.001 | 2.22 | 1.23-4.00 | 0.008 | 1.07 | 0.53-2.15 | 0.84 |
| Number of windows open while watching SEM |
|||||||||
| 1-2 | Ref | ||||||||
| More than 2 | 1.82 | 1.19-2.77 | 0.005 | 1.61 | 0.92-2.80 | 0.09 | 0.88 | 0.46-1.69 | 0.71 |
| Heavy alcohol use in the last 30 days |
|||||||||
| No | Ref | ||||||||
| Yes | 2.18 | 1.18-4.02 | 0.013 | 0.41 | 0.10-1.76 | 0.23 | 0.19 | 0.04-0.65 | 0.03 |
| Age at first sex with a male | |||||||||
| 13 years or younger | Ref | ||||||||
| Older than 13 years | 2.52 | 1.34-4.71 | 0.004 | 0.99 | 0.51-1.94 | 0.99 | 0.40 | 0.17-0.94 | 0.04 |
| Hours spent on partner seeking | |||||||||
| 3 hours or less | Ref | ||||||||
| More than 3 hours | 1.53 | 0.98-2.41 | 0.06 | 1.55 | 0.85-2.81 | 0.15 | 1.01 | 0.50-2.02 | 0.98 |
| Number of sex partners in lifetime | |||||||||
| 20 or less | Ref | ||||||||
| More than 20 | 0.67 | 0.44-1.02 | 0.06 | 0.50 | 0.28-0.89 | 0.02 | 0.75 | 0.38-1.47 | 0.41 |
|
| |||||||||
| Model 3: Psycho-social | |||||||||
| Sexual identification | |||||||||
| Gay/Homosexual | Ref | ||||||||
| Other | 1.13 | 0.69-1.88 | 0.62 | 1.00 | 0.51-1.95 | 0.99 | 0.88 | 0.42-1.83 | 0.73 |
| Outness1 | 1.09 | 0.91-1.30 | 0.34 | 0.90 | 0.71-1.14 | 0.38 | 0.83 | 0.64-1.07 | 0.14 |
| Internalized Homonegativity | 1.34 | 1.14-1.57 | <0.001 | 1.27 | 1.02-1.59 | 0.03 | 0.95 | 0.75-1.20 | 0.66 |
| CSBI | 2.99 | 2.30-3.91 | <0.001 | 4.86 | 3.40-6.95 | <0.001 | 1.62 | 1.12-2.34 | 0.01 |
| PANAS, positive | 1.09 | 0.86-1.39 | 0.45 | 0.91 | 0.65-1.26 | 0.56 | 0.82 | 0.57-1.18 | 0.29 |
| PANAS, negative | 1.11 | 0.89-1.38 | 0.36 | 0.88 | 0.65-1.20 | 0.43 | 0.80 | 0.57-1.11 | 0.17 |
| Condom use self-efficacy | 0.77 | 0.65-0.92 | 0.005 | 0.82 | 0.63-1.06 | 0.13 | 1.06 | 0.81-1.39 | 0.67 |
| Sexual Confidence | 0.97 | 0.76-1.21 | 0.76 | 0.89 | 0.64-1.25 | 0.51 | 0.92 | 0.65-1.33 | 0.67 |
| Sexual Satisfaction | 0.77 | 0.62-0.96 | 0.02 | 0.83 | 0.60-1.14 | 0.25 | 1.07 | 0.76-1.51 | 0.69 |
Note: OR=Odds Ratio; CI= Confidence Interval; NH= Non-Hispanic; PI= Pacific Islander; SEM=Sexually Explicit Material; CSBI = Compulsive Sexual Behavior Inventory; PANAS = Positive and Negative Affect Schedule; Bold faces indicate p≤0.05
As continuous scale
Table 4 presents the results of the final multinomial regression model. After adjusting for the other variables, the CPC-group had significantly lower odds of heavy alcohol use (OR=0.20, 95% CI: 0.04-0.98), later sexual debut (OR=0.29, 95% CI: 0.11-0.79) compared to the problematic group, and lower odds of having more than twenty lifetime sexual partners (OR=0.40, 95% CI: 0.18-0.91) compared to the no-CPC group. Both the problematic group (OR=1.26, 95% CI: 1.05-1.52) and CPC group (OR=1.31, 95% CI: 1.02-1.67) had significantly higher odds of elevated internalized homonegativity scores than the no-CPC group. Compulsive sexual behavior significantly distinguished all three groups, with the CPC group having higher odds of compulsive sexual behavior than either the problematic group (OR=1.90, 95% CI: 1.15-3.15) or the no-CPC group (OR=5.72, 95% CI: 3.52-9.31), while the problematic group also had significantly higher odds than the no-CPC group (OR=3.01, 95% CI: 2.13-4.25). The problematic group was also more likely to report lower condom use self-efficacy (OR=0.79, 95% CI: 0.62-1.00) and sexual satisfaction (OR=0.75, 95% CI: 0.58-0.96) compared to the no-CPC group.
Table 4.
Final Multivariable Model of Compulsive Pornography Consumption among the SEM Study Participants (N=1165 MSM)
| No vs. Problematic | No vs. Compulsive | Problematic vs. Compulsive |
|||||||
|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||
| OR | 95% CI | p | OR | 95% CI | p | OR | 95% CI | p | |
|
|
|||||||||
| Personal | |||||||||
| Age | |||||||||
| 18 – 24 | Ref | ||||||||
| 25 – 34 | 1.28 | 0.71-2.31 | 0.41 | 1.28 | 0.56-2.91 | 0.55 | 1.00 | 0.41-2.43 | 0.99 |
| 35 – 44 | 1.17 | 0.52-2.63 | 0.71 | 0.87 | 0.24-3.10 | 0.83 | 0.75 | 0.19-2.94 | 0.66 |
| ≥45 | 0.79 | 0.28-2.22 | 0.66 | 1.91 | 0.54-6.71 | 0.31 | 2.40 | 0.54-10.79 | 0.25 |
| In a long-term relationship | |||||||||
| No | Ref | ||||||||
| Yes | 0.84 | 0.47-1.50 | 0.56 | 0.83 | 0.37-1.87 | 0.66 | 0.99 | 0.40-2.42 | 0.98 |
| Behavioral | |||||||||
| Amount of SEM viewed, hr/wk | |||||||||
| 1 – 2.9 | Ref | ||||||||
| > 2.9 | 2.07 | 1.25-3.44 | 0.005 | 1.96 | 0.97-3.96 | 0.06 | 0.95 | 0.43-2.06 | 0.89 |
| Number of windows open while watching SEM |
|||||||||
| 1-2 | Ref | ||||||||
| More than 2 | 1.53 | 0.94-2.49 | 0.09 | 1.31 | 0.66-2.58 | 0.44 | 0.85 | 0.40-1.80 | 0.68 |
| Heavy alcohol use in the last 30 days |
|||||||||
| No | Ref | ||||||||
| Yes | 1.59 | 0.75-3.39 | 0.22 | 0.32 | 0.07-1.54 | 0.15 | 0.20 | 0.04-0.98 | 0.05 |
| Age at first sex with a male | |||||||||
| 13 years or younger | Ref | ||||||||
| Older than 13 years | 3.70 | 1.69-8.10 | 0.001 | 1.07 | 0.47-2.41 | 0.87 | 0.29 | 0.11-0.79 | 0.02 |
| Number of sex partners in lifetime | |||||||||
| 20 or less | Ref | ||||||||
| More than 20 | 0.76 | 0.44-1.32 | 0.34 | 0.40 | 0.18-0.91 | 0.03 | 0.52 | 0.22-1.28 | 0.16 |
| Psycho-social | |||||||||
| Internalized homonegativity | 1.26 | 1.05-1.52 | 0.01 | 1.31 | 1.02-1.67 | 0.04 | 1.04 | 0.79-1.36 | 0.81 |
| CSBI | 3.01 | 2.13-4.25 | <0.001 | 5.72 | 3.52-9.31 | <0.001 | 1.90 | 1.15-3.15 | 0.01 |
| Condom use self-efficacy | 0.79 | 0.62-1.00 | 0.05 | 0.81 | 0.58-1.34 | 0.22 | 1.03 | 0.71-1.49 | 0.87 |
| Sexual Satisfaction | 0.75 | 0.58-0.96 | 0.03 | 0.85 | 0.60-1.21 | 0.36 | 1.13 | 0.76-1.68 | 0.54 |
Note: OR=Odds Ratio; CI= Confidence Interval; NH= Non-Hispanic; PI= Pacific Islander; SEM=Sexually Explicit Material; CSBI = Compulsive sexual behavior inventory; Bold faces indicate p≤0.05
DISCUSSION
To advance clinical assessment and research on CPC, our first aim was to identify appropriate scale cut-off points. Two are proposed: a lower cut-off point of 17 on our scale to distinguish MSM with no evidence of CPC from those with problematic pornography consumption, and a higher cut-off point of 25 to distinguish MSM who meet multiple criteria for CPC. These cut-off points divide MSM into three distinct groups based on criteria for CPC: participants with no evidence of CPC; participants whose scores reveal some problems with CPC; and participants whose scores indicate they clearly meet all or nearly all criteria for CPC.
To the best of our knowledge and review, this study is the first to undertake an empirical approach to studying CPC. We highlight the following key findings. First, although high SEM consumption was extremely common in the sample of MSM, clinical CPC is rare. Most MSM did not report any symptoms of CPC. Nevertheless, 7% of our sample reported significant obsessions and/or lack of control regarding their SEM consumption. The bivariate investigations reveal some interesting patterns that researchers and clinicians may wish to keep in mind. Younger MSM, MSM in the suburbs and rural areas, less sexually experienced MSM, and those not in long-term relationships may be more likely to present with CPC.
Second, consistent with DSM criteria for compulsive behaviors (criteria which includes being time-consuming), in unadjusted and adjusted analyses, CPC was significantly associated with more time spent in SEM consumption. In the final model, however, time spent consuming SEM only distinguished between the no-CPC and problematic groups. This suggests that just asking about or screening time spent on SEM consumption is insufficient to assess CPC. Similarly, the lack of differences in dollars spent on SEM likely reflects the ready availability of free SEM on the Internet, and suggests that unless clinicians assess specifically for CPC (for example by using the scale), CPC is likely to be under-reported and go untreated.
Third, consistent with the Sexual Health Model (Robinson et al., 2002), the unadjusted and adjusted analyses show multiple sexual health concerns associated with problematic and compulsive pornography consumption. These include the number of windows open when watching SEM, earlier age of first sex, greater internalized homonegativity, not being gay identified and being less out, and more compulsive sexual behaviors with fewer sexual partners and less sexual satisfaction. In terms of HIV risk, the results suggest a complex picture. Using the lower cut-off point, men with problematic SEM consumption had high odds of heavy alcohol use and were more likely to report later sexual debut than the no-CPC group. However, at the higher cut-off point, this relationship is reversed, and high CPC is associated with lower odds of heavy alcohol use and later sexual debut. This pattern is consistent with “problematic” CPC being correlated or possibly even symptomatic of broader compulsive sexual behavior, while “severe” CPC may limit or prevent MSM from engaging in other compulsive sexual behavior.
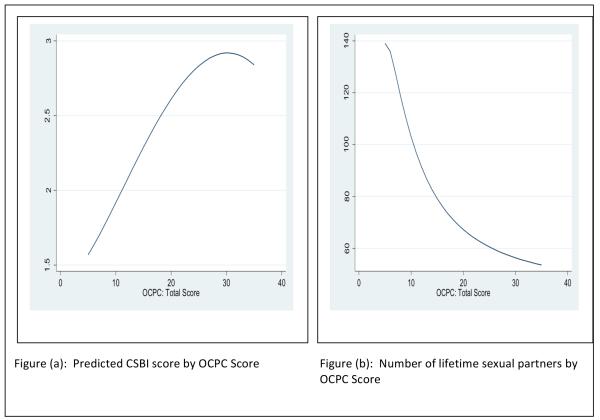
Fourth, the final model reveals an interesting clinical picture of CPC. A later age of sexual debut, higher internalized homonegativity, more compulsive sexual behavior and less sexual satisfaction were all significantly elevated in the problematic group compared to those with no-CPC. At the higher cut-off, younger sexual debut, less heavy alcohol use, and higher compulsive sexual behavior scores distinguished the highest scorers from the problematic group. More MSM research into age of first sexual encounter, including qualitative studies and life histories may illuminate how early sexual experiences may influence later behavior. Finally, while a strong relationship at both cut-off points was observed between compulsive sexual behavior and CPC, the correlation between the two scales is only moderate (r=.53, p<.001). This suggests that while compulsive sexual behaviors and CPC may share common variance, each also has distinct elements. Furthermore, as shown in Figure 2, the relationship between CPC and CSB is more quadratic curvilinear than linear and that at extreme scores, the direction of the relationship changes. This is consistent with CSB and CPC being correlated for most people; however for persons with extreme CPC, they appear more likely to be focused solely on CPC to the exclusion of other sexual behavior. The relationship between number of sexual partners and CPC is negative and curvilinear, suggesting both that the higher the CPC score, the less number of partners, and that this relationship is strongest for those with low and high to extreme scores. For clinicians interested in assessing for compulsive sexual behaviors, we conclude screening for both compulsive sexual behavior and compulsive pornography consumption is necessary; and that inference solely from number of partners or time spent is not sufficient.
Figure 2.
Predicted Compulsive Sexual Behavior Inventory (CSBI) score (a) and number of lifetime sexual partners (b) by Compulsive Pornography Consumption (CPC) scale scores among the SEM study participants (N=1165 MSM)
In interpreting these findings, there are several limitations to keep in mind. As a new area of study, the reliability of our findings is unknown. Similarly, although the sample is relatively large, it is a convenience sample of MSM in the US who volunteered to participate in an online study advertised as being on “porn”. Generalizability of findings to other MSM is unknown. We specifically caution against using the identified cut-off points with non-MSM samples without further validation, as SEM use in MSM is culturally specific, and hence, generalizability to other groups might be unlikely. Third, since the data are cross-sectional, temporality and causality should not be assumed.
The publication of a new short screening scale for CPC in MSM opens up new opportunities. Both researchers and clinicians may wish to add this screening scale as part of any comprehensive assessment for compulsive sexual behaviors. While existing scales of compulsive sexual behaviors assess for obsessions and compulsions in sex (with others), the short scale focuses on pornography consumption, which is typically viewed alone. We encourage clinicians and researchers to consider adding it to either the Coleman or Kalichman instruments as an additional scale, given that evidence from this study suggests that for a small but significant percentage of MSM consumers, SEM consumption is deeply distressing, preoccupying and experienced as beyond the person’s control. Future research directions include identifying norms and cut-off points for other populations (e.g., heterosexual populations) and key demographics (e.g., by gender); validation studies (comparing clients with clinically defined CPC with those without); and replication studies in MSM samples to assess the reliability of findings in this study.
Acknowledgment
The SEM study was funded by the National Institute of Mental Health Center for Mental Health Research on AIDS, grant number R01MH087231.
REFERENCES
- American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders. Fifth Edition American Psychiatric Association; Arlington, VA: 2013. [Google Scholar]
- Benotsch EG, Kalichman SC, Kelly JA. Sexual compulsivity and substance use in HIV-seropositive men who have sex with men: Prevalence and predictors of high-risk behaviors. Addictive Behaviors. 1999;24:857–868. doi: 10.1016/s0306-4603(99)00056-8. [DOI] [PubMed] [Google Scholar]
- Benotsch G, Kalichman SC, Pinkerton SD. Sexual compulsivity in HIV-positive men and women: Prevalence, predictors, and consequences of high-risk behaviors. Sexual Addiction &Compulsivity: The Journal of Treatment and Prevention. 2001;8(2):83–99. [Google Scholar]
- Carnes P. Out of the shadows: Understanding sexual addiction. Hazeldon Publishing; Minneapolis, MN: 2001. [Google Scholar]
- Carnes P, Green B, Carnes S. The same yet different: Refocusing the Sexual Addiction Screening Test (SAST) to reflect orientation and gender. Sexual Addiction & Compulsivity. 2010;17(1):7–30. [Google Scholar]
- Coleman E. Compulsive sexual behavior: New concepts and treatments. Journal of Psychology & Human Sexuality. 1991;4(2):37–52. [Google Scholar]
- Coleman E, Horvath KJ, Miner MH, Ross MW, Oakes JM, Rosser BRS, the Men’s INTernet Sex (MINTS-II) Team Compulsive sexual behavior and risk for unsafe sex among men who use the Internet to seek sex with men. Archives of Sexual Behavior. 2010;39:1045–1053. doi: 10.1007/s10508-009-9507-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coleman E, Miner M, Ohlerking F, Raymond NC. Compulsive sexual behavior inventory: A preliminary study of reliability and validity. Journal of Sex and Marital Therapy. 2001;27:325–332. doi: 10.1080/009262301317081070. [DOI] [PubMed] [Google Scholar]
- Cooper A. Sex and the Internet: A guidebook for clinicians. Brunner-Routledge; New York, NY: 2002. [Google Scholar]
- Cooper A, Delmonico DL, Burg R. Cybersex users, abusers, and compulsives: New findings and implications. Sexual Addiction and Compulsivity. 2000;7:5–29. [Google Scholar]
- Cooper A, Putnam DE, Planchon LA, Boies SC. Online sexual compulsivity: Getting tangled in the net. Sexual Addiction and Compulsivity. 1999;6(2):79–104. [Google Scholar]
- Cooper A, Scherer CR, Boies SC, Gordon BL. Sexuality on the Internet: From sexual exploration to pathological expression. Professional Psychology: Research and Practice. 1999;30(2):154. [Google Scholar]
- Daneback K, Ross MW, Månsson SA. Characteristics and behaviors of sexual compulsives who use the Internet for sexual purposes. Sexual Addiction & Compulsivity. 2006;13(1):53–67. [Google Scholar]
- Delmonico DL, Miller JA. The Internet Sex Screening Test: A comparison of sexual compulsives versus non-sexual compulsives. Sexual and Relationship Therapy. 2003;18(3):261–276. [Google Scholar]
- Eaton LA, Cain DN, Cherry C. The relationship between pornography use and sexual behaviors among at-risk HIV negative men who have sex with men. Sexual Health. 2012;9:166–170. doi: 10.1071/SH10092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galos DL, Smolenski DJ, Grey JA, Iantaffi A, Rosser BS. Preferred aspects of sexually explicit media among men who have sex with men: where do condoms fit in? Psychology & Sexuality. 2013:1–19. doi: 10.1080/19419899.2013.851108. (ahead-of-print) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grov C, Bamonte A, Fuentes A, Parsons JT, Bimbi DS, Morgenstern J. Exploring the internet’s role in sexual compulsivity and out of control sexual thoughts/behaviour: a qualitative study of gay and bisexual men in New York City. Cultural, Health & Sexuality. 2008;10(2):107–125. doi: 10.1080/13691050701564678. [DOI] [PubMed] [Google Scholar]
- Grov C, Parsons JT, Bimbi DS. Sexual compulsivity and sexual risk in gay and bisexual men. Archives of Sexual Behavior. 2010;39(4):940–949. doi: 10.1007/s10508-009-9483-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grubbs JB, Sessoms J, Wheeler DM, Volk F. The Cyber-Pornography Use Inventory: The development of a new assessment instrument. Sexual Addiction & Compulsivity. 2010;17(2):106–126. [Google Scholar]
- Hald GM, Smolenski D, Rosser BRS. Perceived effects of sexually explicit materials among men who have sex with men and psychometric properties of the pornography consumption effect scale. Journal of Sexual Medicine. 2013;10(3):757–767. doi: 10.1111/j.1743-6109.2012.02988.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hald GM, Træen B, Noor SW, Iantaffi A, Galos DL, Rosser BRS. Does sexually explicit media (SEM) affect me? Assessing first person effects of SEM consumption among Norwegian men who have sex with men. Psychology & Sexuality. 2014 in press. [Google Scholar]
- Hald GM, Træen B, Noor SW, Iantaffi A, Rosser BRS. Phenomenological experiences of sexually explicit media consumption among men who have sex with men. Psychology & Sexuality. 2014 doi: 10.1080/19317611.2013.823900. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones-Webb R, Smolenski DJ, Brady SS, Wilkerson JM, Rosser BRS. Drinking settings, alcohol consumption, and sexual risk behavior among gay men. Addictive Behaviors. 2013;38(3):1824–1830. doi: 10.1016/j.addbeh.2012.11.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalichman SC, Greenberg J, Abel GG. HIV-seropositive men who engage in high-risk sexual behaviour: psychological characteristics and implications for prevention. AIDS Care. 1997;9(4):441–450. doi: 10.1080/09540129750124984. [DOI] [PubMed] [Google Scholar]
- Kalichman SC, Rompa D. Sexual sensation seeking and sexual compulsivity scales: Reliabliity, validity and predicting HIV risk behavior. Journal of Personality Assessment. 1995;65(3):581–601. doi: 10.1207/s15327752jpa6503_16. [DOI] [PubMed] [Google Scholar]
- Kalichman SC, Rompa D. The sexual compulsivity scale: Further development and use with HIV-positive persons. Journal of Personality Assessment. 2001;76(3):379–395. doi: 10.1207/S15327752JPA7603_02. [DOI] [PubMed] [Google Scholar]
- Konstan JA, Rosser BRS, Ross MW, Stanton J, Edwards WM. The story of Subject Naught: A cautionary but optimistic tale of Internet survey research. Journal of Computer-Mediated Communication. 2005;10(2) Retrieved from At: http://jcmc.indiana/edu/vol10/issue2/konstan.html. [Google Scholar]
- Kor A, Zilcha-Mano S, Fogel YA, Mikulincer M, Reid RC, Potenza MN. Psychometric development of the Problematic Pornography Use scale. Addictive Behaivors. 2014;39:861–868. doi: 10.1016/j.addbeh.2014.01.027. [DOI] [PubMed] [Google Scholar]
- Kuzma JM, Black DW. Epidemiology, prevalence, and natural history of compulsive sexual behavior. Psychiatric Clinics of North America. 2008;31(4):603–611. doi: 10.1016/j.psc.2008.06.005. [DOI] [PubMed] [Google Scholar]
- Marin BV, Gomez CA, Tschann JM, Gregorich SE. Condom use in unmarried Latino men: A test of cultural constructs. Health Psychology. 1997;16(5):458–467. doi: 10.1037//0278-6133.16.5.458. [DOI] [PubMed] [Google Scholar]
- Miner MH, Coleman E, Center BA, Ross MW, Rosser BRS. The compulsive sexual behavior inventory: Psychometric properties. Archives of Sexual Behavior. 2007;36:579–587. doi: 10.1007/s10508-006-9127-2. [DOI] [PubMed] [Google Scholar]
- Nelson KM, Simoni JM, Morrison DM, George WH, Leickly E, Lengua LJ, Hawes SE. Sexually explicit online media and sexual risk among men who have sex with men in the United States. Archives of Sexual Behavior. 2014 doi: 10.1007/s10508-013-0238-2. provisionally accepted. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Noor SW, Rosser BRS, Erickson D. A brief scale to measure problematic sexually explicit media consumption: psychometric properties of the Compulsive Pornography Consumption (CPC) scale among men who have sex with men. Sexual Addiction & Compulsivity. 2014 doi: 10.1080/10720162.2014.938849. submitted for publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parsons JT, Bimbi DS, Halkitis PN. Sexual compulisivty among gay/bisexual male escorts who advertise one the Internet. Sexual Addiction & Compulsivity. 2001;8:101–112. [Google Scholar]
- Parsons JT, Severino JP, Grov C, Bimbi DS, Morgenstern J. Internet use among gay and bisexual men with compulsive sexual behavior. Sexual Addiction & Compulsivity. 2007;14(3):239–256. [Google Scholar]
- Raymond NC, Coleman E, Miner MH. Psychiatric comorbidity and impulsive/compulsive traits in individuals with compulsive sexual behavior. Comprehensive Psychiatry. 2003;24(8):370–380. doi: 10.1016/S0010-440X(03)00110-X. [DOI] [PubMed] [Google Scholar]
- Reid RC, Li DS, Gilliland R, Stein JA, Fong T. Reliability, validity, and psychometric development of the Pornography Consumption Inventory in a sample of hypersexual men. Journal of Sex & Marital Therapy. 2011;37(5):359–385. doi: 10.1080/0092623X.2011.607047. [DOI] [PubMed] [Google Scholar]
- Robinson BE, Bockting WO, Rosser BRS, Rugg DL, Miner M, Coleman E. A sexological approach to HIV prevention: The sexual health model. Health Education Research. 2002;17:43–57. doi: 10.1093/her/17.1.43. [DOI] [PubMed] [Google Scholar]
- Rosser BRS, Grey JA, Wilkerson JM, Iantaffi A, Brady SS, Smolenski DJ, Horvath KJ. A commentary on the role of sexually explicit media (SEM) in the transmission and prevention of HIV among men who have sex with men (MSM) AIDS and Behavior. 2012;16(6):1375–1381. doi: 10.1007/s10461-012-0135-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosser BRS, Smolenski D, Erickson D, Iantaffi A, Brady SS, Galos D, Wilkerson JM. The effects of gay sexually explicit media on the HIV risk behavior of men who have sex with men. AIDS and Behavior. 2013;17(4):1488–1498. doi: 10.1007/s10461-013-0454-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosser BRS, Smolenski DJ, Erickson D, Iantaffi A, Brady SS, Grey JA, Wilkerson JM. The effects of gay sexually explicit media on the HIV risk behavior of men who have sex with men [Abstracts of the 21st World Congress for Sexual Health, Porto Alegre, Brazil, September 21-24. Awarded best abstract] Journal of Sexual Medicine. 2013 in press. [Google Scholar]
- Rosser BRS, Wilkerson JM, Grey JA, Iantaffi A, Smolenski DJ. The relationship between gay pornography use and sexual risk behavior in men who have sex with men. Journal of Sexual Medicine. 2011;8(s3):258. (Abstract 696) [Google Scholar]
- Singel R, Layden MA. Internet porn: Worse than crack? 2004 https://www.shelleylubben.com/articles/internetporn.pdf.
- Smolenski DJ, Erickson DJ, Wilkerson JM, Rosser BRS. Measuring the effect of sexually-explicit media (SEM) among men who have sex with men. Paper presented at the Society for the Scientific Study of Sex; Houston, TX. 2011. [Google Scholar]
- Smolenski DJ, Diamond PM, Ross MW, Rosser BRS. Revision, criterion validity, and multigroup assessment of the reactions to homosexuality scale. Journal of Personality Assessment. 2010;92(6):568–576. doi: 10.1080/00223891.2010.513300. doi:10.1080/00223891.2010.513300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Snell WE, Fisher TD, Walters AS. The Multidimensional Sexuality Questionnaire: An objective self-report measure of psychological tendencies associated with human sexuality. Annals of Sex Research. 1993;6(1):27–55. [Google Scholar]
- Stein D, Silvera R, Hagerty R, Marmor M. Viewing pornography depicting unprotected anal intercourse: Are there implications for HIV prevention among men who have sex with men. Archives of Sexual Behavior. 2012;41(2):411–419. doi: 10.1007/s10508-011-9789-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sullivan PS, Grey JA, Rosser BRS. Emerging technologies for HIV prevention for MSM: What we have learned, and ways forward. Journal of Acquired Immune Deficiency Syndromes. 2013;63:S102–S107. doi: 10.1097/QAI.0b013e3182949e85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The National Council on Sexual Addiction and Compulsivity 2013 from www.ncsac.org.
- The Society for the Advancement of Sexual Health 2014 from www.sash.net.
- Thompson ER. Development and validation of an internationally reliable short-form of the Positive and Negative Affect Schedule (PANAS) Journal of Cross-Cultural Psychology. 2007;38(2):227–242. [Google Scholar]
- Træen B, Hald GM, Noor SW, Iantaffi A, Grey J, Rosser BRS. The relationship between use of sexually explicit media and sexual risk behavior in men who have sex with men: exploring the mediating effects of sexual self-esteem and condom use self-efficacy. International Journal of Sexual Health. International Journal of Sexual Health. 2013:1–32. doi: 10.1080/19317611.2013.823900. (ahead-of-print) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilkerson JM, Iantaffi A, Smolenski DJ, Brady SS, Horvath KJ, Grey JA, Rosser BRS. The SEM risk behavior (SRB) model: A new conceptual model of how pornography influences the sexual intentions and HIV risk behavior of MSM. Sexual and Relationship Therapy. 2012;27(3):217–230. doi: 10.1080/14681994.2012.734605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilkerson JM, Iantaffi A, Smolenski DJ, Horvath KJ, Rosser BRS. Acceptability of HIV-prevention messages in sexually explicit media viewed by men who have sex with men. AIDS Education and Prevention. 2013;25(4):315–326. doi: 10.1521/aeap.2013.25.4.315. doi: 10.1521/aeap.2013.25.4.315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Young KS. Internet addiction: The emergence of a new clinical disorder. CyberPsychology & Behavior. 1998;1(3):237–244. [Google Scholar]