Abstract
Background
Dizziness and unsteady gait are common in the elderly but are too often dismissed as supposedly nonspecific, inevitable accompaniments of normal aging. For many affected persons, the factors leading to dizziness and gait impairment in old age are never identified, yet some of these factors can be specifically detected and treated.
Methods
This review is based on publications (2005–2014) retrieved by a selective search in PubMed on the terms “aging,” “dizziness,” “elderly,” “gait,” “gait disorder,” “geriatric,” “locomotion,” and “vertigo.”
Results
Dizziness interferes with the everyday activities of 30% of persons over age 70 and is so severe that it constitutes a reason for consulting a physician. The more common causes of dizziness and unsteady gait in old age are sensory deficits, such as bilateral vestibular failure, polyneuropathy, and impaired visual acuity; benign paroxysmal positioning vertigo; and central disorders such as cerebellar ataxia and normal-pressure hydrocephalus. Further relevant factors include sedative or antihypertensive medication, loss of muscle mass (sarcopenia), and fear of falling. Many elderly persons have multiple factors at the same time. Benign paroxysmal positioning vertigo can be effectively treated with specific physical maneuvers. Sedating drugs are indicated only for the treatment of acute rotatory vertigo and are not suitable for long-term use. Sarcopenia can be treated with physical training.
Conclusion
If a specific cause can be identified, dizziness and gait unsteadiness in old age can often be successfully treated. The common causes can be revealed by systematic clinical examination. Controlled clinical trials on the efficacy of treatments for elderly persons are urgently needed.
Impaired mobility and falls are among the main factors contributing to a reduced quality of life in old age (1). In this context, patients often report unstable gait and dizziness. This review article aims to provide a structured diagnostic approach for this situation, which makes it possible to identify relevant deficits and factors. Dizziness and unsteady gait are not effects of normal aging but indicate potential:
Deficits in peripheral and central sensory functions (visual, vestibular, somatosensory)
Musculoskeletal deficits (sarcopenia, arthritis)
Cognitive and mental disorders (dementia, anxiety).
Elderly people often have deficits in several areas. Multifactorial disorders should, however, not prevent deficits from being identified and from receiving targeted treatment. In many cases, interdisciplinary collaboration is required for the purpose of detailed classification and therapy.
Prevalence of dizziness and unstable gait in old age
In patients >75 years, dizziness is the most common leading symptom (2). The 1-year prevalence for significant dizziness that prompts a visit to the doctor and restricts activities of everyday life in persons older than 60 is 20%; in those older than 70, it is 30%, and in those older than 80, 50% (3). In the context of the population-based KORA-Age study in the Augsburg area, dizziness was identified as a crucial factor for an impaired quality of life and therefore reduced participation in age-appropriate activities in older persons (4, 5).
The terms “vertigo” and “dizziness” are used to describe a whole spectrum of perceptions and symptoms that range from a rotatory sensation to staggering dizziness to gait unsteadiness, lightheadedness, or anxiety. A structured history and clinical examination are therefore the most important elements in clarifying the etiology. The mostly older patients with long-term dizziness problems also experience gait abnormalities. When measured by using a simple clinical test (modified Romberg test), the prevalence of balance disorders in persons older than 80 in the US was 85% (6). An important and quantifiable parameter in this context is the frequency of falls. Within a year, more than 30% of persons living in their own homes and more than 50% of persons living in care homes experience at least one fall, even without experiencing dizziness (7, e1). Often, mobility will then decrease because of fear of further falls (e2). The direct consequences of falls are responsible for >1% of healthcare costs in Europe (8). The most important risk factors for falls in old age include symptoms of dizziness and gait abnormalities (8, 9).
Important causes of vertigo and dizziness in old age
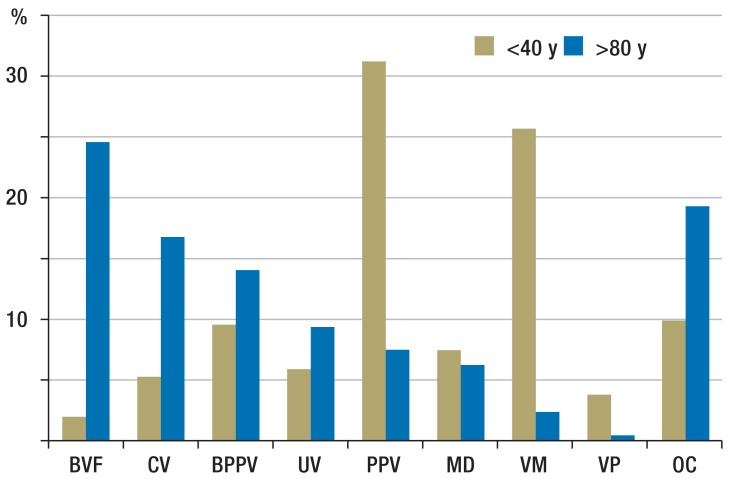
The Figure shows a diagnostic spectrum of patients >80 years compared with patients <40 in a specialist outpatient clinic in Munich. The Figure highlights some important aspects regarding dizziness in old age:
Figure.
Rates of symptoms of vertigo in a specialist outpatient clinic of the German Center for Vertigo and Balance Disorders in Munich. The figure shows the relative frequencies in 500 consecutive patients aged <40 (5–39) years and >80 (81–99) years. In older patients, bilateral vestibular failure (BVF), central vertigo (CV), and benign paroxysmal positioning vertigo (BPPV) are particularly common.
Further abbreviations: y, years; OC, other causes, MD, Menière’s disease; PPV, somatoform and phobic postural vertigo; UV, unilateral vestibulopathy; VM, vestibular migraine; VP, vestibular paroxysmia
The entire diagnostic spectrum is covered.
Sensory deficits—for example, bilateral vestibular failure (BVF)—and central vertigo (CV)—for example, cerebellar ataxia—are very common.
Psychosomatic forms of vertigo and vestibular migraine are less common than in younger patients.
Benign paroxysmal positioning vertigo (BPPV) is more common in older persons, and other factors have a greater role—for example, polyneuropathy and orthostatic dysregulation.
Benign paroxysmal positioning vertigo
In older patients, BPPV is common, because the probability of release of otolith particles in the inner ear increases with age (e3). Symptomatic cases, of the kind that occur after cranial trauma or as a consequence of peripheral vestibular disorders, are also more common because of the higher incidence of the latter.
Diagnostic clues are provided by the typical medical history, whereby short attacks of rotatory vertigo are triggered by changing the position of the head; these attacks may be accompanied by nausea and vomiting. Typical triggers are:
Turning around in bed—for example, in order to look at the alarm clock
Tilting the head backwards—for example, in order to look up
Bending the head forwards—for example, in order to spit while brushing one’s teeth.
The diagnostic maneuvers—for example, the Dix-Hallpike maneuver for the posterior semicircular canal and head rotation to the side in a supine position for the horizontal semicircular canal—should always be conducted in vertigo and balance impairments, especially in older patients, because the disorder may present in an atypical manner in case of multifactorial etiology (2, 10). In a positive case, a crescendo-decrescendo nystagmus appears after a latency period; this will typically last less than one minute. Depending on which semicircular canal is affected, the direction of the beat will be vertical to the forehead, with torsion to the lower-positioned ear (posterior semicircular canal) or purely horizontal (horizontal semicircular canal). The posterior semicircular canal is affected in most cases (90%). Treatment consists of specific release maneuvers, whose efficacy has been confirmed in controlled studies. An overview of the evidence was published in Deutsches Ärzteblatt International fairly recently (11). Current guidelines are available at www.eaono.org, for example.
Bilateral vestibular failure
In case of bilateral impairment of the peripheral vestibular function, movement-dependent staggering dizziness is present (while walking); symptoms typically increase in the dark and on uneven ground (10, 12). A proportion of patients also experiences oscillopsia, which arises from a dysfunction of the vestibulo-ocular reflex (VOR) (10). In about 50% of cases, no specific cause is identified when a diagnosis is made (12). If an etiology is confirmed, ototoxic medications (aminoglycosides) or pre-existing inner-ear disorders (bilateral Menière’s disease) are often implicated (12). The association with polyneuropathies and cerebellar disorders (cerebellar ataxia with neuropathy and bilateral vestibular areflexia [CANVAS syndrome]) is also important (e4, e5).
Bilateral vestibular failure as a cause of dizziness and unstable gait in older persons is often overlooked. In addition to the typical medical history, the clinical findings with confirmed VOR deficit (pathological result after head impulse test with eye adjustment after fast head rotation) will provide a clue (13). The balance disorder becomes obvious, similar to other sensory deficits, especially when the eyes are closed (lack of visual control) or while walking slowly (impaired sensory integration) (14, 15). The most important element of treatment is targeted balance training with active gait training and postural stabilization training (16). The aim of vestibular training is an improvement in vestibulo-ocular and vestibulo-spinal reflexes in posture regulation.
Central vertigo
Central vestibular disorders develop because of lesions along the vestibular structures and pathways including the vestibular nuclei in the medulla oblongata, the oculomotor nuclei and centers in the mesencephalon and the cerebellum, the thalamus, and the vestibular cortex (10). If there are lesions—for example, after a stroke or if a primary brain tumor is present—the result will be clearly defined brain stem syndromes with typical deficits in oculomotor function and postural regulation.
The clinical finding in this setting usually prompts further investigation using imaging (magnetic resonance imaging [MRI]), which will confirm the lesion. It is more difficult, especially for non-neurologists, to detect and correctly categorize vertigo and dizziness symptoms in the context of new-onset neurodegenerative disorders. Patients with atypical Parkinson’s syndromes—for example, progressive supranuclear palsy (PSP)—or cerebellar disorders—for example, downbeat nystagmus syndrome—often present with dizziness and gait instability as their main symptom. In this setting it is important to interpret even discrete clinical signs correctly and refer the patient to the specialist; in case of doubt, a follow-up consultation should be arranged in order not to overlook progression of the deficits.
The treatment of forms of central vertigo depends on their cause. Acquired forms of nystagmus after stroke or inflammatory brainstem lesions—for example, acquired pendular nystagmus with oscillopsia—can be reduced by using medication—for example, memantine or gabapentin (17). Patients with cerebellar disorders benefit from targeted physiotherapy with balance training (18, e6) and symptomatic drug treatment—for example, with aminopyridines or acetyl-DL-leucine (19) Table 1 summarizes the causes of vertigo and dizziness in old age.
Table 1. Common causes of vertigo and dizziness in old age.
| Disorder | Typical presentation and treatment |
|---|---|
| Benign paroxysmal positioning vertigo (BPPV) | Vertigo attacks (5–60 sec) after changing the position of the head; morning onset common; therapy using release maneuvers |
| Orthostatic vertigo | Transient vertigo after getting up from lying down/sitting position; possibly after medication use; therapy with blood pressure regulation |
| Menière’s disease | Episodes of vertigo (min–h) with ear pressure, tinnitus, impaired hearing; progressive hearing loss; therapy with betahistine, for example |
| Bilateral vestibular failure (complete or incomplete) | Dizziness and unstable gait, especially in the dark and on uneven ground; in some cases oscillopsias; chronic course; therapy with balance training |
| Central vertigo and dizziness | Mostly continuous dizziness with clinical-neurological abnormality (e.g. oculomotor functioning, coordination, extrapyramidal symptoms); in the context of focal lesions (e.g. stroke), cerebral microangiopathy or neurodegenerative disorders (e.g. cerebellar ataxia); therapy of underlying disorder and balance training; symptomatic drug treatment if needed |
Causes of gait disorders in old age
In the normal aging process, the speed of walking continually decreases; after the age of 60 it reduces by about 1% every year (13). Although slowing down in old age has many causes—for example, deficits in muscle and joint biomechanics, in the function of the sensory organs, signal processing in the brain, and the capacity of lung and heart—and although these causes are interrelated in multifarious and complicated ways, walking speed has been found to be a very meaningful parameter in assessing older persons’ health (20). If a person spontaneously walks slower than 0.6 m/s, s/he will mostly require help. By contrast, practically all persons who walk faster than 1 m/s will be independent (20).
Among elderly patients who present to neurologists, the following causes for gait disorders are particularly common (13):
Sensory (for example, as a result of polyneuropathies)
Hypokinetic (for example, owing to Parkinson’s disease)
Ataxic (for example, because of degenerative cerebellar atrophy)
Phobic (for example, owing to fear of falls).
In addition, antalgic (for example, owing to osteoarthritis of the knee) and paretic (for example, owing to radicular pain because of disc herniation) gait disorders account for a large proportion of those affected by gait disorders in general practice, orthopedic surgery, and neurology (21). Important aspects in association with unsteady gait in old age include the function of the sensory systems, cognitive reserve, and locomotor reserve (22).
Gait and sensory function
The sensory control of walking is important especially in the context of slow walking and is less relevant in fast, automatic walking (14, 23, 24). Recent studies have shown that gait variability subsequent to sensory deficits is increased particularly for slow walking (14, 15). It may be assumed that the risk of falls is increased in this setting because gait variability correlates with the risk of falls (8).
Gait, cognition, and anxiety
Normally, walking is automatic and requires little attention. With age, cerebral control of walking increases and, simultaneously, the central sensory interaction is often impaired (25). In difficult situations that require more posture control, other activities—such as a conversation, for example—will then need to be interrupted in order to safeguard posture control. The interaction between gait and cognition is most obvious in a setting of developing dementia. Older persons with dementia fall more often than people of the same age who are cognitively healthy (e7). In some forms of dementia—for example, in the early phases of vascular and frontotemporal dementia and Alzheimer’s disease—gait disorders and falls occur as simultaneous symptoms of cognitive decline. Recent studies have shown that an impaired gait can be a predictor of a dementia disorder at a later stage (22, e8). Recently the concept of motoric cognitive risk syndrome (MCR syndrome) has been proposed for older patients with subjective cognitive impairment and slowed-down gait (>1 standard deviation under the age-specific mean). Persons with MCR syndrome are at treble the risk of developing a degenerative form of dementia (for example, Alzheimer’s disease) and 12 times the risk of developing vascular dementia—triggered by multiple occurrences of small vessel disease in the brain (22).
The performance while dual tasking—for example, walking while simultaneously solving cognitive tasks—provides an insight into the functional locomotor-cognitive reserves of an elderly person. This ability is often impaired before obvious cognitive or locomotor deficits manifest (26, 27). Setting dual tasks enables detection of deficits at an early stage, as well as recommending preventive measures, such as increased physical activity by increasing the daily walking distance (e9). Among others, the Honolulu Asia Aging Study showed that the risk of developing dementia in men who walked less than 0.25 miles per day was double that of men who walked more than 2 miles every day (e10).
Fear of falling is a prime concern of many elderly patients with unstable gait. The prevalence of this fear has been reported in different studies between 21% and 85% (28). Compared with controls of the same age, fearful patients walk more slowly (28). The fear of falling is associated with anxiety disorders and depression and substantially impairs a person’s quality of life (e11). Increasing avoidance behaviors reduce the confidence in one’s own balance even further, so that symptoms increase in the sense of a downward spiral. Recent studies have shown that a partial cause of the fear of falling in old age may be the interaction between the sensory systems—for example, between the visual and vestibular systems. Affected persons receive too much feedback about their multisensory environment (25, 29). Physical training therapy can reduce the fear of falling in the short term, but, thus far, proof of long-term positive effects of such treatments are lacking (30).
Muscle strength and mobility
The loss in muscle mass in old age can affect up to one-third of a person’s former muscle mass and is a known main risk factor for gait disorders and falls (e2). Muscle atrophy combined with impairment of muscle function is known as sarcopenia. The functional impairment may manifest as reduced walking speed (below 0.8 m/s), for example. Sarcopenia is mostly associated with dynapenia—that is, concomitant impairment of muscle innervation and neuronal muscle control (31, e13).
Muscle (speed) training, preferably in combination with a sufficiently high protein intake (1.2–1.5 g/kg body weight/day) is eminently suitable for regaining muscle strength in older persons (32). In order to regain everyday functioning and gait stability, they additionally require muscle coordination training and muscle control. Gait training, dancing, tai chi, and Dalcroze eurhythmics are all appropriate in this setting (33).
Table 2 summarizes common causes of gait abnormalities in old age.
Table 2. Common causes of unstable gait in old age.
| Deficit (disorder) | Typical presentation and treatment |
|---|---|
| Sensory deficits (polyneuropathy, bilateral vestibulopathy, visus reduction) | Problems especially when walking, especially in poor light and on uneven ground; therapy of underlying disorder and treatment with physical training for standing still and walking |
| Neurodegeneration (Parkinson’s syndrome, cerebellar ataxia, degenerative dementias) | Gait abnormality with additional motor, coordination and cognitive abnormalities; therapy of underlying disorder; training for standing still and walking |
| Normal pressure hydrocephalus and vascular encephalopathy | Small-step gait disorder with subcortical dementia (alertness) and possibly urinary incontinence; depending on MRI: diagnostic drainage of CSF; therapy with blood pressure regulation (vascular encephalopathy) or ventriculo-peritoneal shunt (normal pressure hydrocephalus) |
| Fear of falling; intoxication (alcohol, medical drugs) | Slowed-down gait with support-seeking arm movements, avoidance behavior; therapy by adjusting medication (Table 3), counseling, training for standing still and walking |
Clinical assessment of the deficits
History
The medical history of patients with gait abnormalities, dizziness and vertigo captures crucial factors that may escape attention in the clinical exam. Rotatory vertigo and staggering dizziness need to be distinguished from feeling dazed. When gathering information about falls, information should also be gathered about the situations where such falls occurred and distinction needs to be made between whether a patient almost fell or did actually fall (34, e14). It is important to elicit which medications a patient might be taking (Table 3). Sedating drugs for vertigo (cinnarizine, dimenhydrinate) are suitable only for acute rotatory vertigo with nausea and vomiting, not for long-term therapy.
Table 3. Examples of medications that commonly trigger dizziness.
| Group of substances | Example substances |
|---|---|
| Blood pressure lowering drugs (antihypertensive drugs) in overdose (hypotension) |
|
| Sedating antidepressants/antipsychotics |
|
| Anticonvulsive drugs used to treat epileptic seizures and pain |
|
| Other sedatives used to treat insomnia, anxiety, vertigo or dizziness |
|
Clinical examination
Box 1 summarizes crucial aspects of the clinical examination. The function of the horizontal semicircular canal in the inner ear—and, therefore, peripheral-vestibular functioning—can be assessed by using the head impulse test (e14), but without video-aided oculography this cannot always be assessed with a high enough degree of certainty, especially in elderly patients (34). In this scenario, caloric testing of the function of the semicircular canal or apparatus-based video head impulse testing is indicated, in cooperation with otorhinolaryngologist colleagues or an interdisciplinary center (35). As three semicircular canals and two otolith organs in each ear contribute to the perception of movement, targeted specialist investigations may be indicated. In order to assess central vestibular function, oculomotor examination is crucial. Subjective visual vertical (SVV) testing is helpful in patients with unstable gait and tendency to fall and is simple to conduct (“bucket test” [e15]).
Box 1. History and baseline examination in vertigo, dizziness and unstable gait in old age.
-
History
Rotational vertigo/staggering gait/daze (“as if walking on cotton wool”, “feeling as if in an elevator”, “muffled head”)
Falls/near falls/situations in which falls occur
Attacks/long-term symptoms
Triggers/amplifying factors
Accompanying symptoms
Medication use / alcohol consumption
Comorbidities
-
Examination, standing posture and gait
Standing still:
Standing still with open/shut eyes (Romberg test)
Tandem standing (heel-toe position) with open/shut eyes and reclining head / standing on foam rubber surface
Pull test
Cognitive dual tasking (multiple challenge, for example, standing and performing calculations simultaneously)
Gait:
Three speeds: slow, self-selected, maximum speed
Walking with eyes shut
Walking while performing cognitive dual task
“Timed up and go” test (time measured for getting up from chair, walk 3 meters, turn round, walk back, sit down again)
-
Examination, sensory systems
Visual:
Static and dynamic visual acuity
Eye position (cover test)
Motility and central oculomotor function
Vestibular:
Spontaneous nystagmus (with or without fixation)
Positioning (posterior and horizontal semicircular canal)
Head impulse test horizontal (if needed, video head impulse test, caloric testing)
Clinical hearing test (audiogram if needed)
Somatosensory:
Independent muscle reflexes
Surface sensitivity
Distal vibration sensation (tuning fork)
-
Cognitive examination
For example, Montreal Cognitive Assessment (MOCA; available in many languages, at www.mocatest.org)
-
Musculoskeletal examination
Muscle strength/trophic condition
Joint mobility passive/active
Posture while standing and walking should also be tested under more difficult conditions—for example:
On a reduced standing area (tandem standing [heel-toe position])
With reduced sensory intake (eyes shut)
Increased cognitive demands (dual task).
The clinical examination of vertigo, dizziness and unstable gait in old age should always include the evaluation of sensory deficits (visual, vestibular, somatosensory). Furthermore, patients should undergo complete internal medical and neurological examinations (especially of the extremities and oculomotor function), and active and passive mobility in the large joints should be assessed.
Dual tasking
In order to test the ability to dual task, either cognitive tasks—such as doing calculations backwards or listing words within a category—or motor tasks—for example, carrying items while standing and walking—should be carried out. A typical clinical sign for the disruptive interaction of gait and cognition is if the patient stops walking while talking (36); this may also be used as a predictor of falls (37). Gait deterioration under dual tasking demands is typical for gait disorders with cortical and subcortical involvement of the brain (for example, in degenerative forms of dementia, but also in Parkinson’s disease). In patients with functional (psychogenic) gait disorders, the situation often improves if the patient is distracted while dual tasking (Box 2).
Box 2. Differential diagnostic relevance of gait abnormalities.
The box summarizes the influence of walking speed, cognitive dual tasking, and shutting eyes in some disorders that affect elderly people disproportionately.
-
Speed
Particularly unsteady when walking slowly (fast = more stable)
Sensory disorder (polyneuropathy [PNP], bilateral vestibular failure [BVF])
Particularly unsteady when walking fast
Cerebellar disorder (moderate speed is best)
Pyramidal tract lesion (for example, after stroke)
Difficulty changing speed while walking
For example, Parkinson’s syndrome
-
Dual tasking (multiple challenges)
Gait abnormality only obvious while dual tasking (for example: standing still during walk once a cognitive task is set simultaneously)
Mild cognitive impairment
Degenerative dementia
Deterioration of gait abnormality owing to dual tasking
Parkinson’s syndrome
Vascular encephalopathy
Normal pressure hydrocephalus
Gait abnormality reduced while dual tasking
Functional gait disorder
-
Eyes shut
Noticeable deterioration of gait abnormality when eyes are shut
Sensory disorder (PNP, BVF)
Moderate deterioration of gait abnormality when eyes are shut
Cerebellar disorders
Vascular encephalopathy
Gait only slightly deteriorated when eyes are shut
Parkinson’s syndrome
Pyramidal tract lesion (for example, after stroke)
Treating gait abnormalities in old age
Motor-cognitive training
In many cases, gait abnormalities in elderly persons are indicative of a combination of disorders affecting muscles, joints, and nerves (sensory and motor) and impaired cerebral functioning. The treatment requires combinations of various procedures. It makes sense to use combined motor-cognitive training in order to improve gait stability and brain functioning. Successful prevention of falls with methods traditionally known to challenge and support motor and cognitive skills—such as tai chi (38) or Dalcroze eurhythmics (33)—achieved an average success rate of 50%.
The Dalcroze eurhythmics study showed, in addition to a reduction in falls, improvements in executive functions (responsible brain functions for planning, dual tasking, abstract thought), thus providing the first indications that specific motor training can be used to improve cognitive brain functioning. It has been shown meanwhile that walking does not only improve physical performance but also cognitive functioning (39). Animal experiments have shown that exercise promotes the neoformation of neurons in the hippocampal formation (40). It is likely that in humans, the stem cell pool in the adult brain is kept active by walking and exercise; consequently, physical activity is one of the most effective measures for counteracting the threat of neurodegeneration.
Key Messages.
Vertigo, dizziness, and unstable gait have specific causes, even in elderly people.
The combination of several causes is typical for these problems.
Sensory, motor, and cognitive deficits have to be meticulously identified and require treatment.
Combined motor-cognitive training can prevent falls and their sequelae.
Acknowledgments
Translated from the original German by Birte Twisselmann, PhD.
Footnotes
Conflict of interest statement
The authors declare that no conflict of interest exists.
References
- 1.Rubenstein LZ. Falls in older people: epidemiology, risk factors and strategies for prevention. Age Ageing. 2006;35(Suppl 2):ii37–ii41. doi: 10.1093/ageing/afl084. [DOI] [PubMed] [Google Scholar]
- 2.Furman JM, Raz Y, Whitney SL. Geriatric vestibulopathy assessment and management. Curr Opin Otolaryngol Head Neck Surg. 2010;18:386–391. doi: 10.1097/MOO.0b013e32833ce5a6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jonsson R, Sixt E, Landahl S, Rosenhall U. Prevalence of dizziness and vertigo in an urban elderly population. J Vest Res. 2004;14:47–52. [PubMed] [Google Scholar]
- 4.Mueller M, Strobl R, Jahn K, et al. Impact of vertigo and dizziness on self-perceived participation and autonomy in older adults: results from the KORA-Age study. Qual Life Res. 2014;23:2301–2308. doi: 10.1007/s11136-014-0684-x. [DOI] [PubMed] [Google Scholar]
- 5.Mueller M, Strobl R, Jahn K, Linkohr B, Peters A, Grill E. Burden of disability attributable to vertigo and dizziness in the aged: results from the KORA-Age study. Eur J Pub Health. 2014;24:802–807. doi: 10.1093/eurpub/ckt171. [DOI] [PubMed] [Google Scholar]
- 6.Agrawal Y, Carey JP, Della Santina CC, Schubert MC, Minor LB. Disorders of balance and vestibular function in US adults: data from the National Health and Nutrition Examination Survey, 2001-2004. Arch Int Med. 2009;169:938–944. doi: 10.1001/archinternmed.2009.66. [DOI] [PubMed] [Google Scholar]
- 7.Masud T, Morris RO. Epidemiology of falls. Age Ageing. 2001;30(Suppl 4):3–7. doi: 10.1093/ageing/30.suppl_4.3. [DOI] [PubMed] [Google Scholar]
- 8.Ambrose AF, Paul G, Hausdorff JM. Risk factors for falls among older adults: a review of the literature. Maturitas. 2013;75:51–61. doi: 10.1016/j.maturitas.2013.02.009. [DOI] [PubMed] [Google Scholar]
- 9.Verghese J, Ambrose AF, Lipton RB, Wang C. Neurological gait abnormalities and risk of falls in older adults. J Neurol. 2010;257:392–398. doi: 10.1007/s00415-009-5332-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Brandt T. 2nd edition. London: Springer; 1999. Vertigo - its multisensory syndromes. [Google Scholar]
- 11.Strupp M, Dieterich M, Brandt T. The treatment and natural course of peripheral and central vertigo. Dtsch Arztebl Int. 2013;110:505–515. doi: 10.3238/arztebl.2013.0505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zingler VC, Cnyrim C, Jahn K, et al. Causative factors and epidemiology of bilateral vestibulopathy in 255 patients. Ann Neurol. 2007;61:524–532. doi: 10.1002/ana.21105. [DOI] [PubMed] [Google Scholar]
- 13.Jahn K, Zwergal A, Schniepp R. Gait disturbances in old age: classification, diagnosis, and treatment from a neurological perspective. Dtsch Arztebl Int. 2010;107:306–315. doi: 10.3238/arztebl.2010.0306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Schniepp R, Wuehr M, Neuhaeusser M, et al. Locomotion speed determines gait variability in cerebellar ataxia and vestibular failure. Mov Disorders. 2012;27:125–131. doi: 10.1002/mds.23978. [DOI] [PubMed] [Google Scholar]
- 15.Wuehr M, Schniepp R, Schlick C, et al. Sensory loss and walking speed related factors for gait alterations in patients with peripheral neuropathy. Gait Posture. 2014;39:852–858. doi: 10.1016/j.gaitpost.2013.11.013. [DOI] [PubMed] [Google Scholar]
- 16.Herdman SJ. Vestibular rehabilitation. Curr Opin Neurol. 2013;26:96–101. doi: 10.1097/WCO.0b013e32835c5ec4. [DOI] [PubMed] [Google Scholar]
- 17.Strupp M, Hufner K, Sandmann R, et al. Central oculomotor disturbances and nystagmus: a window into the brainstem and cerebellum. Dtsch Arztebl Int. 2011;108:197–204. doi: 10.3238/arztebl.2011.0197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.van de Warrenburg BP, van Gaalen J, Boesch S, et al. EFNS/ENS Consensus on the diagnosis and management of chronic ataxias in adulthood. Eur J Neurol. 2014;21:552–562. doi: 10.1111/ene.12341. [DOI] [PubMed] [Google Scholar]
- 19.Ilg W, Bastian AJ, Boesch S, et al. Consensus paper: management of degenerative cerebellar disorders. Cerebellum. 2014;13:248–268. doi: 10.1007/s12311-013-0531-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Studenski S, Perera S, Patel K, et al. Gait speed and survival in older adults. JAMA. 2011;305:50–58. doi: 10.1001/jama.2010.1923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Snijders AH, van de Warrenburg BP, Giladi N, Bloem BR. Neurological gait disorders in elderly people: clinical approach and classification. Lancet Neurol. 2007;6:63–74. doi: 10.1016/S1474-4422(06)70678-0. [DOI] [PubMed] [Google Scholar]
- 22.Verghese J, Annweiler C, Ayers E, et al. Motoric cognitive risk syndrome: multicountry prevalence and dementia risk. Neurology. 2014;83:718–726. doi: 10.1212/WNL.0000000000000717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Brandt T, Strupp M, Benson J. You are better off running than walking with acute vestibulopathy. Lancet. 1999;354 doi: 10.1016/S0140-6736(99)03179-7. [DOI] [PubMed] [Google Scholar]
- 24.Jahn K, Strupp M, Schneider E, Dieterich M, Brandt T. Differential effects of vestibular stimulation on walking and running. Neuroreport. 2000;11:1745–1748. doi: 10.1097/00001756-200006050-00029. [DOI] [PubMed] [Google Scholar]
- 25.Zwergal A, Linn J, Xiong G, Brandt T, Strupp M, Jahn K. Aging of human supraspinal locomotor and postural control in fMRI. Neurobiol Aging. 2012;33:1073–1084. doi: 10.1016/j.neurobiolaging.2010.09.022. [DOI] [PubMed] [Google Scholar]
- 26.Beauchet O, Freiberger E, Annweiler C, Kressig RW, Herrmann FR, Allali G. Test-retest reliability of stride time variability while dual tasking in healthy and demented adults with frontotemporal degeneration. J Neuroeng Rehab. 2011;8 doi: 10.1186/1743-0003-8-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Theill N, Martin M, Schumacher V, Bridenbaugh SA, Kressig RW. Simultaneously measuring gait and cognitive performance in cognitively healthy and cognitively impaired older adults: the Basel motor-cognition dual-task paradigm. J Am Geriatr Soc. 2011;59:1012–1018. doi: 10.1111/j.1532-5415.2011.03429.x. [DOI] [PubMed] [Google Scholar]
- 28.Reelick MF, van Iersel MB, Kessels RP, Rikkert MG. The influence of fear of falling on gait and balance in older people. Age Ageing. 2009;38:435–440. doi: 10.1093/ageing/afp066. [DOI] [PubMed] [Google Scholar]
- 29.Sturnieks DL, St George R, Lord SR. Balance disorders in the elderly. Clin Neurophysiol. 2008;38:467–478. doi: 10.1016/j.neucli.2008.09.001. [DOI] [PubMed] [Google Scholar]
- 30.Kendrick D, Kumar A, Carpenter H, et al. Exercise for reducing fear of falling in older people living in the community. Cochr Rev. 2014;11 doi: 10.1002/14651858.CD009848.pub2. CD009848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Cruz-Jentoft AJ, Baeyens JP, Bauer JM, et al. Sarcopenia: European consensus on definition and diagnosis: Report of the European Working Group on Sarcopenia in Older People. Age Ageing. 2010;39:412–423. doi: 10.1093/ageing/afq034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Deutz NE, Bauer JM, Barazzoni R, et al. Protein intake and exercise for optimal muscle function with aging: recommendations from the ESPEN expert group. Clin Nutr. 2014;33:929–936. doi: 10.1016/j.clnu.2014.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Trombetti A, Hars M, Herrmann FR, Kressig RW, Ferrari S, Rizzoli R. Effect of music-based multitask training on gait, balance, and fall risk in elderly people: a randomized controlled trial. Arch Int Med. 2011;171:525–533. doi: 10.1001/archinternmed.2010.446. [DOI] [PubMed] [Google Scholar]
- 34.Lehnen N, Schneider E, Jahn K. Do neurologists need the head impulse test? Nervenarzt. 2013;84:973–974. doi: 10.1007/s00115-013-3822-8. [DOI] [PubMed] [Google Scholar]
- 35.Jahn K, Schneider E. Apparative Untersuchung der vestibulären Funktion bei Schwindelpatienten. Nervenheilkunde. 2012;5:370–377. [Google Scholar]
- 36.Lundin-Olsson L, Nyberg L, Gustafson Y. „Stops walking when talking“ as a predictor of falls in elderly people. Lancet. 1997;349 doi: 10.1016/S0140-6736(97)24009-2. [DOI] [PubMed] [Google Scholar]
- 37.Montero-Odasso M, Verghese J, Beauchet O, Hausdorff JM. Gait and cognition: a complementary approach to understanding brain function and the risk of falling. J Am Geriatr Soc. 2012;60:2127–2136. doi: 10.1111/j.1532-5415.2012.04209.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Wolf SL, Barnhart HX, Kutner NG, McNeely E, Coogler C, Xu T. Reducing frailty and falls in older persons: an investigation of Tai Chi and computerized balance training. Atlanta FICSIT Group. Frailty and Injuries: Cooperative Studies of Intervention Techniques. J Am Geriatr Soc. 1996;44:489–497. doi: 10.1111/j.1532-5415.1996.tb01432.x. [DOI] [PubMed] [Google Scholar]
- 39.Coelho FG, Andrade LP, Pedroso RV, et al. Multimodal exercise intervention improves frontal cognitive functions and gait in Alzheimer’s disease: A controlled trial. Geriatr Gerontol Int. 2013;13:198–202. doi: 10.1111/j.1447-0594.2012.00887.x. [DOI] [PubMed] [Google Scholar]
- 40.Kempermann G. New neurons for ’survival of the fittest’. Nat Rev Neurosci. 2012;13:727–736. doi: 10.1038/nrn3319. [DOI] [PubMed] [Google Scholar]
- e1.Alexander NB. Definition and epidemiology of falls and gait disorders. In: Sirven JI, Malamut BL, editors. Clinical neurology of the older adult. Philadelphia: Lippincott Williams & Wilkins; 2002. pp. 108–116. [Google Scholar]
- e2.Jorstad EC, Hauer K, Becker C, Lamb SE. Measuring the psychological outcomes of falling: a systematic review. J Am Geriatr Soc. 2005;53:501–510. doi: 10.1111/j.1532-5415.2005.53172.x. [DOI] [PubMed] [Google Scholar]
- e3.Bachor E, Wright CG, Karmody CS. The incidence and distribution of cupular deposits in the pediatric vestibular labyrinth. Laryngoscope. 2002;112:147–151. doi: 10.1097/00005537-200201000-00026. [DOI] [PubMed] [Google Scholar]
- e4.Migliaccio AA, Halmagyi GM, McGarvie LA, Cremer PD. Cerebellar ataxia with bilateral vestibulopathy: description of a syndrome and its characteristic clinical sign. Brain. 2004;127:280–293. doi: 10.1093/brain/awh030. [DOI] [PubMed] [Google Scholar]
- e5.Szmulewicz DJ, Waterston JA, MacDougall HG, et al. Cerebellar ataxia, neuropathy, vestibular areflexia syndrome (CANVAS): a review of the clinical features and video-oculographic diagnosis. Ann N Y Acad Sci. 2011;1233:139–147. doi: 10.1111/j.1749-6632.2011.06158.x. [DOI] [PubMed] [Google Scholar]
- e6.Fonteyn EM, Schmitz-Hubsch T, Verstappen CC, et al. Prospective analysis of falls in dominant ataxias. Eur Neurol. 2013;69:53–57. doi: 10.1159/000342907. [DOI] [PubMed] [Google Scholar]
- e7.Holtzer R, Friedman R, Lipton RB, Katz M, Xue X, Verghese J. The relationship between specific cognitive functions and falls in aging. Neuropsychol. 2007;21:540–548. doi: 10.1037/0894-4105.21.5.540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- e8.Verghese J, Wang C, Lipton RB, Holtzer R, Xue X. Quantitative gait dysfunction and risk of cognitive decline and dementia. J Neurol Neurosurg Psychiatry. 2007;78:929–935. doi: 10.1136/jnnp.2006.106914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- e9.Ravaglia G, Forti P, Lucicesare A, et al. Physical activity and dementia risk in the elderly: findings from a prospective Italian study. Neurology. 2008;70:1786–1794. doi: 10.1212/01.wnl.0000296276.50595.86. [DOI] [PubMed] [Google Scholar]
- e10.Abbott RD, White LR, Ross GW, Masaki KH, Curb JD, Petrovitch H. Walking and dementia in physically capable elderly men. JAMA. 2004;292:1447–1453. doi: 10.1001/jama.292.12.1447. [DOI] [PubMed] [Google Scholar]
- e11.van Haastregt JC, Zijlstra GA, van Rossum E, van Eijk JT, Kempen GI. Feelings of anxiety and symptoms of depression in community-living older persons who avoid activity for fear of falling. Am J Geriatr Psychiatry. 2008;16:186–193. doi: 10.1097/JGP.0b013e3181591c1e. [DOI] [PubMed] [Google Scholar]
- e12.Verghese J, Wang C, Lipton RB, Holtzer R. Motoric cognitive risk syndrome and the risk of dementia. J Gerontol A. 2013;68:412–418. doi: 10.1093/gerona/gls191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- e13.Cruz-Jentoft AJ, Landi F. Sarcopenia. Clin Med. 2014;14:183–186. doi: 10.7861/clinmedicine.14-2-183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- e14.Halmagyi GM, Curthoys IS. A clinical sign of canal paresis. Arch Neurol. 1988;45:737–739. doi: 10.1001/archneur.1988.00520310043015. [DOI] [PubMed] [Google Scholar]
- e15.Zwergal A, Rettinger N, Frenzel C, Dieterich M, Brandt T, Strupp M. A bucket of static vestibular function. Neurology. 2009;72:1689–1692. doi: 10.1212/WNL.0b013e3181a55ecf. [DOI] [PubMed] [Google Scholar]