Abstract
Objective To examine whether maternal depressive symptoms: (a) predicted the level of maternal involvement in diabetes management tasks across adolescence; and (b) moderated associations of involvement with adolescent adherence, metabolic control, and depression. Methods Eighty-two youth aged 10–15 years with type 1 diabetes and their mothers completed measures at baseline and 16 months later. Participants rated maternal involvement in diabetes tasks, adherence, and depressive symptoms; metabolic control was indexed from medical records. Results Maternal depressive symptoms were associated with higher involvement at baseline, and slower declines in involvement across time. At baseline, involvement was associated with lower adolescent depression and better metabolic control, but this association was stronger when mothers reported fewer depressive symptoms. Interactions of maternal depression with involvement across time suggested maternal involvement was associated with better subsequent adherence primarily when mothers reported fewer depressive symptoms. Conclusions Mothers’ depressive symptoms may undermine her care-giving effectiveness during adolescence.
Keywords: adolescence, diabetes management, maternal depression, maternal involvement, type 1 diabetes
Introduction
Parenting an adolescent with type 1 diabetes poses unique challenges that may be difficult to meet when parents experience symptoms of depression. Type 1 diabetes is a serious illness that has a complex and demanding treatment regimen, where patients coordinate multiple daily behaviors (i.e., insulin injections, blood glucose monitoring, diet, exercise) in order to normalize blood glucose levels. Adolescence is a difficult time for diabetes management, partially because this is when responsibility for diabetes care is transferred from parent to child (Anderson, Ho, Brackett, & Laffel, 1997; Wysocki, et al., 1996). If parents’ instrumental involvement declines prematurely, diabetes management may be impaired (Palmer et al., 2004; Wysocki et al., 1996). If it does not decline, however, adolescents may not develop independent diabetes skills, or may experience parents’ involvement as excessive or intrusive. Navigating the sometimes conflicting developmental and health needs of a teen with diabetes requires flexible and sensitive parenting skills, which may be compromised when parents experience depressive symptoms. The present study examined how symptoms of maternal depression were associated with age-related changes in mothers’ instrumental involvement in diabetes management across adolescence.
Mothers’ depressive symptoms may relate to involvement in her adolescent’s diabetes care in complex ways. Depressed mothers may be less involved given the low energy, social withdrawal, and hostile parenting that accompany depression (Gelfand & Teti, 1990). Mothers with depressive symptoms may thus initiate less active involvement in diabetes, and her adolescent may be less likely to seek her out as a resource. There are also reasons to expect depressed mothers to be more involved and slower to transfer diabetes responsibilities to her adolescent. Depressed mothers tend to choose parenting strategies that require less cognitive effort than do controls (Kochanska, Kuczynski, Radke-Yarrow, & Welsh, 1987). Depressed mothers may thus continue to assume responsibility for diabetes tasks, rather than to engage in the more complex task of renegotiating responsibilities and scaffolding her adolescent toward better management. Mothers with more depressive symptoms also have lower confidence in the adolescent’s ability to manage diabetes (Butler et al., 2009). This association, coupled with the anxiety and rumination that often accompany depression (Nolen-Hoeksema, 2000), may heighten maternal involvement by prompting excessive worries about diabetes symptom management.
Few studies have examined associations between maternal depression and levels of instrumental involvement in diabetes during adolescence. Jaser et al. (Jaser, Whittemore, Ambrosino, Lindemann, & Grey, 2008) found maternal depression was unrelated to measures of parental responsibility for diabetes tasks among 8- to 12-year-olds, but no study has examined this association among adolescents more broadly. Maternal anxiety, which has similar characteristics to depression (e.g., pervasive distress symptoms; Watson, 2009), was associated with heightened parental responsibility for adolescents’ diabetes care tasks (Cameron, Young, & Wiebe, 2007), and maternal depressive symptoms were associated with more care-giving intentions in response to vignettes of sick children (Scalzo, Williams, & Holmbeck, 2005). One aim of the current study was to explore whether maternal depressive symptoms were associated with levels of maternal responsibility for diabetes care tasks across adolescence.
Although parents’ instrumental involvement in diabetes care has generally been associated with better diabetes outcomes during adolescence (Anderson et al., 1997; Palmer et al., 2004), the benefit of such involvement is likely to be compromised when mothers are more depressed. Symptoms of maternal depression place children at risk for a host of psychosocial difficulties (Downey & Coyne, 1990; Gelfand & Teti, 1990; Goodman & Gotlib, 1999) and are associated with poorer psychosocial adjustment among youth with diabetes (Eckshtain, Ellis, Kolmadin, & Naar-King, 2010; Jaser et al., 2008; Kovacs, Goldson, Obrosky, & Bonar, 1997). Associations with physical functioning are less commonly studied, but maternal depression has also been associated with poorer illness management among adolescents with diabetes (Eckshtain et al., 2010). Such associations may occur because depressed mothers engage in more negative and intrusive parenting (Gelfand & Teti, 1990; Goodman & Gotlib, 1999; Jaser & Grey, 2010), which are related to poorer diabetes management and higher depression among youth with diabetes (Berg et al., 2007; Jaser & Grey, 2010; Wiebe et al., 2005). Exposure to the risks of negative parenting may be higher when mothers are more involved caregivers. Depressive symptoms may also undermine mothers’ ability to be involved in a way that is most beneficial for adolescents with diabetes. Adolescents with diabetes benefit from warm/sensitive parenting (Berg et al., 2008; Jaser & Grey, 2010), and from caregivers who are collaborative (Wiebe et al., 2005; Wysocki et al., 2009) and have good diabetes problem-solving skills (Wysocki et al., 2008). Such positive parenting and care-giving practices are likely to be disrupted by maternal depressive symptoms (e.g., Jaser & Grey, 2010).
In summary, we examined cross-sectional and longitudinal associations among maternal depressive symptoms, maternal involvement in diabetes, and adolescent psychosocial adjustment and diabetes management. First, we examined whether mothers’ depressive symptoms were associated with different age-related patterns of instrumental involvement. We anticipated age-related decreases in maternal involvement in both cross-sectional (i.e., indicated by a negative association between age and involvement at the initial time point) and longitudinal analyses (i.e., indicated by declines in involvement across time, particularly among older adolescents). We also determined whether maternal depressive symptoms moderated these age-related declines in involvement. Second, we examined whether maternal involvement was differentially associated with adolescent adjustment as a function of maternal depressive symptoms. We anticipated that maternal involvement would be associated with positive adolescent adjustment (i.e., better adherence and metabolic control, less depression), but that this association would be weaker when mothers had more depressive symptoms.
Methods
Participants
Early adolescents with type 1 diabetes (43 boys and 39 girls) and their mothers were recruited from a larger pool of 127 families who had participated in a cross-sectional study of maternal involvement in adolescent diabetes. In the original study, youth were ages 10–15 years, had been diagnosed with diabetes longer than 1 year, and lived with their mothers (see Berg et al., 2007; Palmer et al., 2004; Wiebe et al., 2005). We refer to these participants as adolescents, consistent with the view that adolescence is the age period from age 10 to 18 years (Arnett, 2000). Mothers were recruited because they are the primary caregivers for children with chronic illness. These original families were recontacted by mail and invited to complete a follow-up survey ∼16 months after the original study. The final sample for the present study included the 82 mother–adolescent dyads (65% of the original sample) who returned signed informed consent/assent forms and follow-up questionnaires using postage paid return envelopes. Those who participated in the follow-up had longer illness duration than those who did not, M = 5.4 vs. 4.1 years, t (125) = 2.49, p < .05, Cohen d = .458, but did not differ on any other variable (i.e., age, gender, adherence, HbA1c, adolescent or mother depressive symptoms, maternal involvement). Procedures were approved by the institutional review board, and signed consent and assent were obtained.
Adolescents had an average age of 12.79 (SD = 1.70) years at Time 1 (range = 10.00–15.99), and 14.16 (SD = 1.69) years at follow-up (range = 11.58–17.41). Most youth were on a regimen of multiple daily injections, reporting an average of 4.67 blood glucose tests per day (range = 3–8, SD = 1.17). Mothers were largely European-American (99%), married (90%), and well-educated with 40% having a bachelor’s or advanced degree. Hollingshead Index indicated a minor professional, medium business class sample.
Measures
Maternal Depressive Symptoms
Mothers completed the Center of Epidemiological Studies of Depression Scale (CESD; Radloff, 1977) to assess maternal depression. This widely used scale discriminates between psychiatric and nonpatient samples, and had strong reliability in the present sample (α > .91 at Times 1 and 2). Raw scores were computed by summing across items. A score of 16 identifies elevated risk of depression; 23 mothers (28%) were above this cutoff at each time point, while 9 were above this cutoff at both time points.
Maternal Involvement
Mothers and teens individually completed the responsibility items from the Diabetes Responsibility and Conflict Scale (Rubin, Young-Hyman, & Peyrot, 1989) to measure mother’s instrumental involvement in diabetes care. Participants reported who was responsible for 25 aspects of diabetes care (e.g., who determines the insulin dose), using a 1 (child does it alone) to 3 (child and mother share equally) to 5 (mother does it alone) scale. Scores were averaged across items separately for mothers and adolescents, such that higher scores indicated higher levels of maternal involvement. The scale had strong reliability in the present sample (α > .88 for mother and adolescent reports at Times 1 and 2).
Adolescent Depression
Youth completed the Children’s Depression Inventory (CDI; Kovacs, 1985), choosing one of three response choices for each of 27 items to indicate depressive symptoms experienced in the past 2 weeks (possible scores range from 0 to 54). This widely used scale has been normed on 7- to 17-year-olds (Kovacs et al., 1997), and has high reliability (α > .87 at Times 1 and 2 in this study). Raw scores were computed by summing across items. A score of 13 or greater reflects elevated depression symptoms; 14 adolescents met this criterion at each time point, while 9 did so across both time points. Endorsement of critical items indicating suicidal thought (e.g., “I want to kill myself”) resulted in an assessment by a licensed clinical psychologist who coordinated access to resources as needed.
Adherence
Mothers and teens individually completed the Self Care Inventory (SCI; Lewin et al., 2009) to measure adolescent adherence over the preceding month. Participants rated the frequency with which each of 14 diabetes management tasks (e.g., glucose testing, administering insulin) was completed using a 1 (Never did it) to 5 (Always did it, without fail) scale. Each item had a not applicable option, and scores were computed by averaging ratings across applicable items (i.e., scores ranged from 1 to 5 for mothers and for adolescents). This scale has good reliability, and correlates well with more intensive interview measures of adherence, as well as with blood glucose control (Lewin et al., 2009). Internal consistency in the present sample was good (α > .71 for mother and adolescent reports at Times 1 and 2).
Metabolic Control
Metabolic control was obtained via glycosylated hemoglobin (HbA1c) from medical records. HbA1c is the medical standard for evaluating the quality of diabetes control, and reflects average blood glucose levels over the past 3–4 months. Higher values reflect poorer control. The first HbA1c measure recorded beyond 3 months after questionnaire completion for both Time 1 and Time 2 was analyzed to ensure that we captured diabetes control levels that had occurred after questionnaire completion. The average time between questionnaire completion and HbA1c was 5.40 (2.08) and 5.22 (2.12) months at Times 1 and 2, respectively. Time to HbA1c was uncorrelated with all study variables, p > .09.
Analysis Plan
A mean (item) replacement strategy was used when a participant was missing <25% of the data for a given measure. Regression analyses were conducted to examine whether: (a) mothers’ depressive symptoms were associated with different age-related patterns of involvement; and (b) mothers’ depressive symptoms moderated associations between maternal involvement and adolescent adjustment. For each aim, we initially analyzed cross-sectional associations between predictor and outcome variables measured at Time 1, and then analyzed longitudinal associations between predictor variables at Time 1 and changes in the outcome variable from Times 1 to 2. Main effects were mean centered (Aiken & West, 1991) and entered on Step 1, and interactions were entered on subsequent steps. Interactions were interpreted by computing predicted means, substituting scores ±1 SD for the predictor variables into the regression equation (Aiken & West, 1991). Demographic (i.e., gender, ethnicity, marital status, socioeconomic status) and illness variables (i.e., duration, intensity of regimen, age at diagnosis) were examined as potential covariates, but were unrelated to the outcome variables with one exception; illness duration was associated with some indices of poorer adolescent adjustment, and was therefore covaried in all Aim 2 analyses. Prior to conducting the regression analyses, distributions were examined for normality and outliers. The distributions were normal with the exception of mother [Skew (SE) = 1.43 (0.27); 0.95 (0.27)], and child reports of depressive symptoms [Skew (SE) = 1.54 (0.27); 1.32 (0.27)], at Times 1 and 2, respectively. However, the assumptions underlying regression were met in all cases (i.e., the residuals were normally distributed and unrelated to predicted values, and there was no significant multicollinearity). Thus, analyses based on untransformed scores are reported below. Effect sizes for each statistically significant regression term are reported using Cohen’s f2 (Cohen, 1988).
Results
Descriptive information on study variables is reported in Table I. Correlations revealed strong associations between adolescent age and reduced maternal involvement, and indicated mothers’ initial depressive symptoms were related to higher involvement in her adolescent’s diabetes at both time points. In contrast, initial levels of maternal involvement were unrelated to mothers’ subsequent depressive symptoms, suggesting depressive symptoms were not primarily a response to higher involvement. Correlations also revealed that mothers’ depressive symptoms and her involvement in diabetes were generally unrelated to adolescent well-being when considered in the absence of other variables; a notable exception is that maternal depressive symptoms were associated with lower (i.e., better) metabolic control at Time 1.
Table I.
Correlations among Study Variables at Time 1 (T1) and 2 (T2)
| Maternal depression |
Maternal involvement T1 |
Maternal involvement T2 |
||||||
|---|---|---|---|---|---|---|---|---|
| Variable | Time 1 (T1) | Time 2 (T2) | Mother report | Teen report | Mother report | Teen report | Teen age | M (SD) |
| Time1 | ||||||||
| Involvement T1 | ||||||||
| Mother | .32** | .12 | – | .73*** | .76*** | .60*** | −.65*** | 2.73 (0.51) |
| Teen | .14 | .07 | – | – | .70*** | .76*** | −.68*** | 2.55 (0.56) |
| CDI | −.00 | .02 | −.09 | −.10 | −.21+ | −.13 | .20+ | 6.84 (6.22) |
| SCI-teen | −.04 | .01 | .01 | .05 | .12 | .19+ | −.17 | 3.64 (0.64) |
| SCI-mother | −.06 | −.04 | .03 | .09 | .14 | .27* | −.28** | 3.47 (0.58) |
| HbA1ca | −.26* | −.21 | −.19 | −.10 | −.16 | −.27* | .08 | 8.86 (1.31) |
| Time 2 | ||||||||
| Involvement T2 | ||||||||
| Mother | .27* | .20+ | – | – | – | .65*** | −.72*** | 2.61 (0.43) |
| Teen | .32** | .21+ | – | – | – | – | −.67*** | 2.26 (0.52) |
| CDI | .02 | .09 | −.09 | −.10 | −.21+ | −.13 | .32** | 7.69 (6.88) |
| SCI-teen | −.15 | −.12 | −.06 | .04 | .07 | .11 | −.05 | 3.71 (0.58) |
| SCI-mother | −.09 | −.29** | .17 | .18 | .14 | .27* | −.23* | 3.51 (0.45) |
| HbA1ca | −.15 | .02 | −.21 | −.23+ | −.14 | −.20 | .05 | 8.63 (1.40) |
aHbA1c was available on 65 youth at Time 1, and 55 youth at Time 2. CDI = children's depression inventory; SCI = self care inventory.
***p < .005, **p < .01, *p < .05, +p < .10.
Associations of Maternal Depressive Symptoms with Her Involvement in Diabetes Care
Cross-sectional regression analyses of measures obtained at Time 1 are displayed in the top section of Table II. Age was associated with lower levels of maternal involvement reported by both mother and teen, independently of mothers’ depressive symptoms. Maternal depressive symptoms were associated with higher levels of mother-reported involvement, but were unrelated to teen-reported involvement. Thus, mothers were less involved in older versus younger adolescents’ diabetes care, and mothers with more depressive symptoms reported being more involved than mothers with fewer depressive symptoms.
Table II.
Regression Analyses Examining Maternal Depressive Symptoms × Adolescent-Age interactions predicting Maternal Involvement
| Mother-reported involvement |
Teen-reported involvement |
|||||||
|---|---|---|---|---|---|---|---|---|
| Predictors | b | t | ΔR2 | f2 | b | t | ΔR2 | f2 |
| Cross-sectional data-predicting maternal involvement at Time 1 | ||||||||
| Step 1 | .49**** | .46**** | ||||||
| CESD1 | .01 | 3.16*** | .07 | .00 | 0.82 | – | ||
| Age1 | −.02 | −7.78**** | .64 | −.02 | −8.05**** | .79 | ||
| Step 2 | .00 | .01 | ||||||
| CESD1 × Age1 | .00 | −0.01 | – | .00 | 0.92 | – | ||
| Longitudinal data-predicting change in maternal involvement (Time 2 − 1) | ||||||||
| Step 1 | .44**** | .32**** | ||||||
| Involvement | −.60 | −7.67**** | .72 | −.49 | −5.60**** | .39 | ||
| CESD1 | .00 | 1.18 | – | .01 | 2.75** | .08 | ||
| Age1 | −.10 | −4.50**** | .18 | −.09 | −3.25*** | .10 | ||
| Step 2 | .05** | .00 | ||||||
| CESD1 × Age1 | .00 | 2.74** | .05 | .00 | 0.21 | – | ||
Note. CESD1 = maternal depressive symptoms at Time 1; Age1 = adolescent age at Time 1.
*p < .05, **p < .01, ***p < .005, ****p < .001.
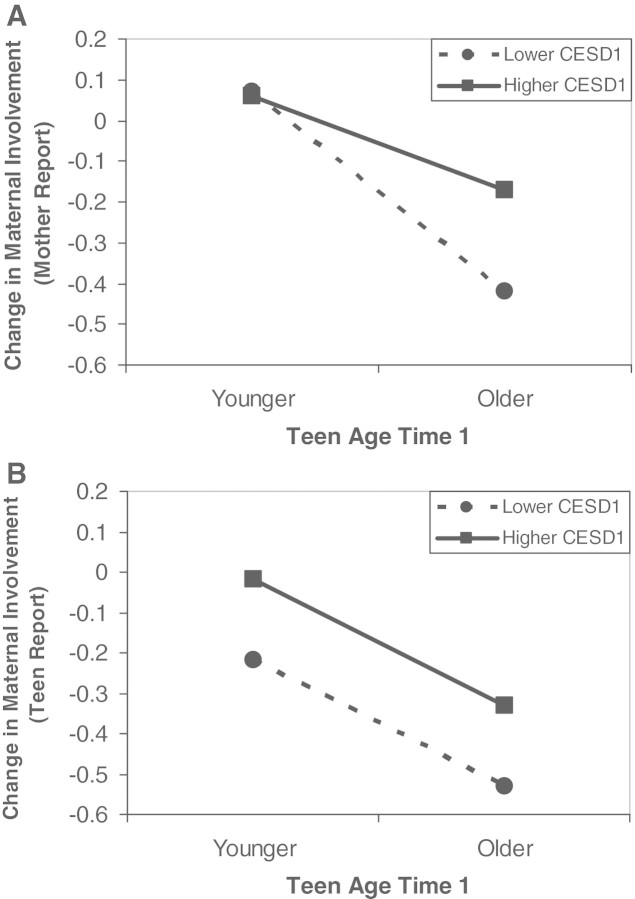
Results from the longitudinal analyses are displayed in the bottom section of Table II. Changes in maternal involvement were computed by subtracting Time 1 from Time 2 involvement, and then regressed upon Time 1 involvement, child age, and maternal depression (i.e., negative change scores indicate declines in involvement across time; positive change scores indicate increases in involvement across time). On average, both mothers (M = −0.12, SD = 0.34) and adolescents (M = −0.26, SD = 0.37) reported declines in maternal involvement from Times 1 to 2, but the strength of this decline differed as a function of adolescent age and maternal depressive symptoms. Older youth at Time 1 displayed larger declines in involvement across time than did younger youth. Symptoms of maternal depression moderated this association for mother-reported involvement, and exerted an additional main effect for changes in teen-reported involvement. Predicted means in Figure 1A indicate age was associated with clear declines in mother-reported involvement when mothers reported fewer depressive symptoms at baseline, but less so when mothers reported more depressive symptoms. Figure 1B displays associations for teen-reported involvement. The two main effects revealed older adolescents reported larger declines in involvement than younger adolescents, regardless of mothers’ depression, and adolescents of mothers with more depressive symptoms reported higher involvement, regardless of their age. In summary, maternal depressive symptoms appeared related to higher involvement and slower declines in involvement across time.
Figure 1.
Predicted means for the maternal depressive symptoms × adolescent age at Time 1 predicting change in maternal involvement from Time 1 to Time 2. Negative change scores indicate declines in involvement across time; 0 indicates no change. (A) Reflects changes in mother-reported involvement, and (B) reflects changes in adolescent-reported involvement. CESD1 = maternal depressive symptoms at Time 1.
Maternal Depressive Symptoms, Maternal Involvement, and Adolescent Adjustment
Cross-sectional Measures at Time 1
Hierarchical regression analyses were conducted to examine whether maternal involvement was differentially associated with adolescent outcomes when mothers had more versus fewer symptoms of depression. Illness duration, maternal involvement, and maternal depressive symptoms were entered on Step 1, and the maternal involvement × maternal depression interaction was entered on Step 2. All significant main effects and interactions involving maternal depressive symptoms are reported below.
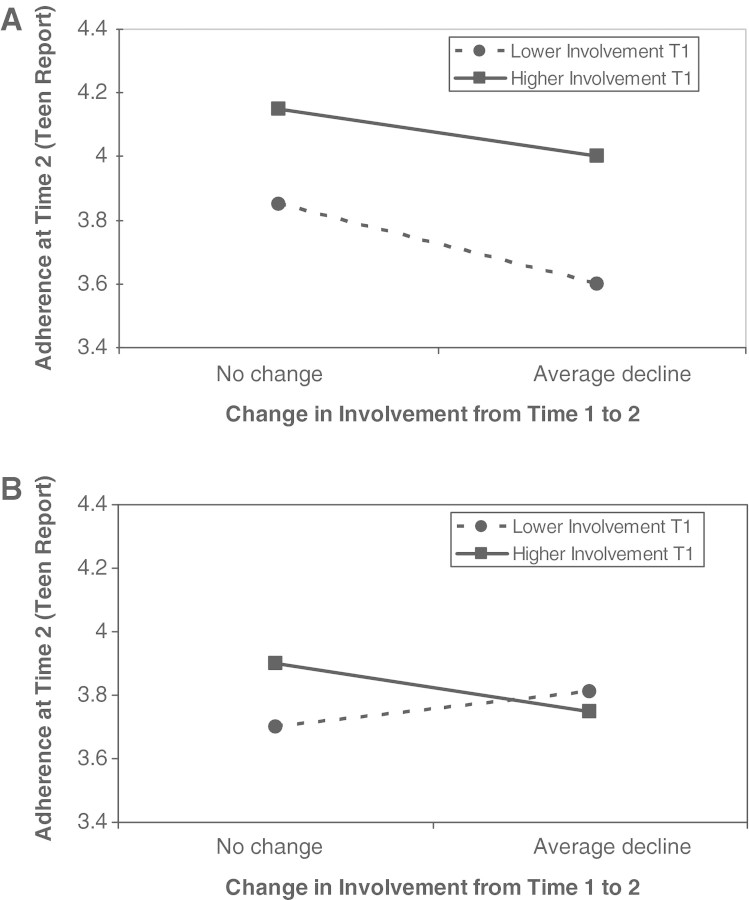
Mothers’ depressive symptoms interacted with teen reports of involvement to predict adolescent depression, b = .26, t (77) = 2.21, p < .05, f2 = .06, but did not exert main effects or interact with mother reports of involvement to predict adolescent depression, p > .27. Mother’s depressive symptoms predicted lower (i.e., better) HbA1c, b = −.04, t (61) = −2.22, p < .05, f2 = .06. This main effect was moderated by a significant interaction with mother-reported involvement, b = .06, t (60) = 2.05, p < .05, f2 = .06, and a marginally significant interaction with teen-reported involvement, b = .05, t (60) = 1.76, p < .10, f2 = .04. Predicted means for adolescents’ depression and the HbA1c outcomes are displayed in Figure 2. In each case, maternal involvement was associated more strongly with adolescent adjustment (i.e., lower depression, lower metabolic control) when mothers reported fewer depressive symptoms. There were no main or interacting effects of maternal depressive symptoms on adherence, regardless of reporter, p > .16. Thus, maternal involvement was associated with fewer emotional and physical benefits for the adolescent when mothers experienced heightened symptoms of depression.
Figure 2.
Predicted means for cross-sectional analyses of the maternal involvement × maternal depressive symptoms interaction predicting adolescent adjustment at Time 1.
Longitudinal Data across Times 1 and 2
Longitudinal analyses extended these findings in two ways. First, we examined how mothers’ depressive symptoms at Time 1 predicted adolescent outcomes at Time 2 (while covarying outcomes at Time 1) to limit the possibility that mothers’ depressive symptoms were simple responses to her adolescent’s poorer adjustment. Second, we examined whether the smaller declines in involvement evidenced by more depressed mothers had additional associations with adolescent adjustment. Regressions were conducted by entering on Step 1 the Time 1 measures of illness duration, the relevant adolescent adjustment measure, maternal depressive symptoms, and maternal involvement, as well as the change in involvement from Times 1 to 2. Two-way interactions between maternal depressive symptoms and both involvement scores were entered at Step 2, and the three way interaction was entered at Step 3. Significant effects for maternal depression are reported below.
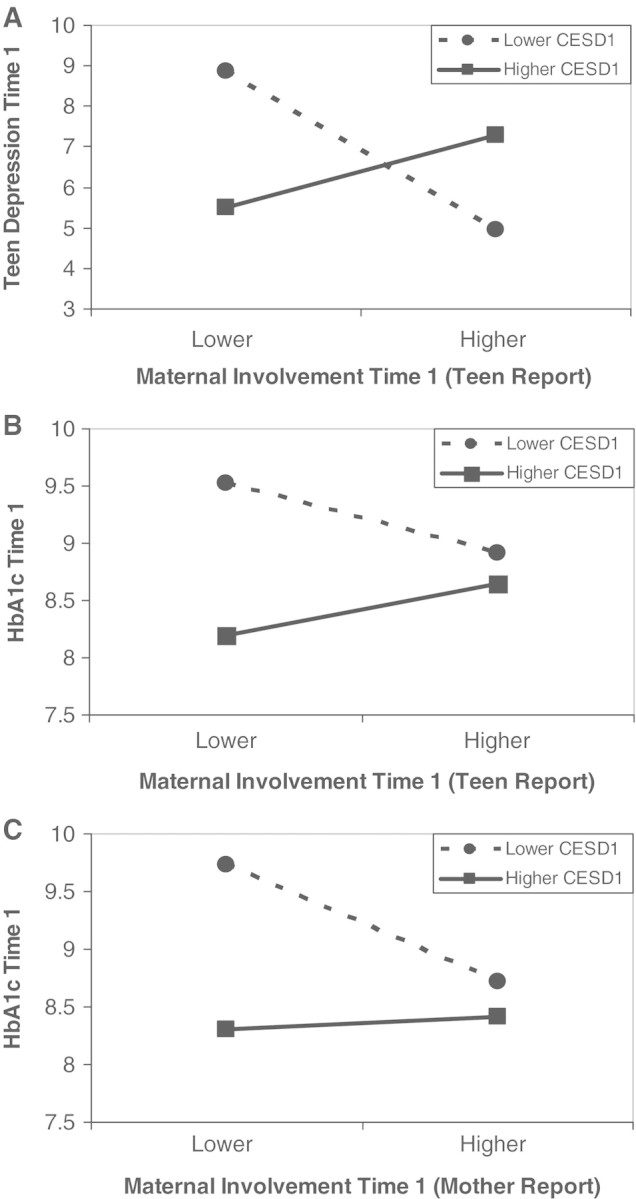
Three-way interactions (i.e., maternal depressive symptoms × involvement × change in involvement) predicted adolescent reports of adherence, b = .07, t (71) = 3.29, ΔR2 = .11, p < .005, f2 = .12, and marginally predicted mother reports of adherence, b = .03, t (70) = 1.86, ΔR2 = .03, p = .066, f2 = .03, when teen-reported involvement was analyzed. When mother reports of involvement were analyzed, this interaction did significantly predict mother reports of adherence, b = .04, t (70) = 2.09, ΔR2 = .04, p < .05, f2 = .04. Predicted means were computed by substituting scores ± 1 SD into the regression equation for the mean centered variables, and scores of 0 (representing no change in involvement) or −.26 (representing the average decline in involvement) for change in involvement. Predicted means for adolescent reports of adherence are displayed in Figure 3; means for mother reports of adherence are not shown due to space limitations but revealed an identical pattern. Results suggested maternal involvement was related to better subsequent adherence primarily when mothers reported fewer depressive symptoms. That is, among mothers with fewer depressive symptoms (Figure 3A), lower involvement at Time 1 and larger declines in involvement across time appeared associated with poorer subsequent adherence. These associations were weaker or nonexistent when mothers had more depressive symptoms (Figure 3B). Maternal depressive symptoms did not have main or interactive associations with Time 2 adolescent depression or HbA1c.
Figure 3.
Predicted means for the maternal depressive symptoms × maternal involvement × change in involvement interaction predicting teen adherence at Time 2, controlling for teen adherence at Time 1. (A) means for mothers with lower depressive symptoms; (B) means for mothers with higher depressive symptoms. T1 = Time 1.
Discussion
Symptoms of maternal depression were associated with mothers being more involved in adolescents’ diabetes management tasks, and with slower declines in involvement across adolescence. Such involvement is typically associated with better diabetes management outcomes (Anderson et al., 1997; Palmer et al., 2004). In the present study, however, involvement appeared less beneficial when mothers reported more depressive symptoms. In both cross-sectional and longitudinal analyses, mothers’ higher involvement in adolescent diabetes care tasks was associated with better outcomes (lower adolescent depression scores, better metabolic control) when mothers reported fewer depressive symptoms, but less so when mothers reported more depressive symptoms. Findings suggest mothers’ emotional well-being should be considered when promoting her involvement in adolescent diabetes management tasks.
Goodman and Gotlib (1999) argued that the mechanisms by which maternal depression confers risk reflect children’s current developmental tasks. Consistent with this idea, associations between maternal depressive symptoms and adolescent-diabetes management appeared to reflect the adolescent’s assumption of independence in diabetes management. Mothers with higher depressive symptoms reported taking more responsibility for diabetes management at baseline, and both these mothers and their teens reported smaller declines in involvement over the subsequent 16 months. These longitudinal associations are important because they suggest that the direction of effects occurred from maternal depressive symptoms to involvement. That is, symptoms of maternal depression at Time 1 predicted subsequent levels of involvement, but maternal involvement at Time 1 was unrelated to subsequent depressive symptoms. The findings suggest that the process by which families renegotiate diabetes responsibilities during adolescence differs when mothers are more depressed.
Associations between mothers’ depressive symptoms and adolescent outcomes were complex and not completely anticipated. We were surprised, for example, to find no direct association between maternal depression and poorer adolescent adjustment. Nevertheless, maternal depressive symptoms did moderate associations between maternal involvement and adolescent outcomes, suggesting that depressive symptoms limited mothers’ ability to be an effective partner in managing diabetes. For example, maternal depressive symptoms were associated concurrently with better metabolic control (i.e., lower HbA1c), but statistical interactions suggested adolescents of more depressed mothers did not experience the metabolic benefits of heightened involvement that was evident among those of less depressed mothers. Unmeasured contextual factors that are more likely when mothers are depressed may have influenced these findings (e.g., other caregivers may step in when mothers experience depressive symptoms).
It is important to distinguish whether maternal involvement conferred risk or was simply less beneficial when mothers had more depressive symptoms, because such patterns have different treatment implications. If the involvement of more depressed mothers confers risk, one would expect it to be negatively associated with teen well-being. This could occur if her involvement exposes her adolescent to maladaptive cognitions and behaviors, or increases conflict in parent–teen interactions (Downey & Coyne, 1990; Webster-Stratton & Hammond, 1988). Interventions in this case may focus not only on treating mothers’ depressive symptoms, but also on altering how adolescents and mothers interact to manage diabetes. If the involvement is primarily conferring fewer benefits, one would expect a positive association between involvement and well-being among teens with less depressed mothers, and a weaker association among teens with more depressed mothers. This could occur if depressive symptoms undermine mothers’ collaborative care-giving or diabetes problem-solving skills. Interventions in this case might focus on enhancing parenting and diabetes-management skills in the more depressed mother, or on skill-development in the teen. Our findings appear consistent with depressed mothers’ involvement conferring fewer benefits, but research to clarify these findings is needed.
The pattern of longitudinal associations between maternal depressive symptoms and different aspects of adolescent adjustment may reveal how the effects of maternal depressive symptoms unfold across development. Symptoms of maternal depression were associated concurrently with metabolic control and adolescent depression, but showed longitudinal associations only with adherence. The concurrent associations with adolescent depression may further contribute to these longitudinal patterns, given that heightened symptoms of depression mediate age-related declines in adherence during adolescence (Korbel, Wiebe, Berg, & Palmer, 2007). Mothers who were more depressed may have had difficulty facilitating adolescents’ self-management skills, and such deficits may accumulate over time, becoming increasingly evident as the teen matures. Longitudinal examination of these short and long cycles of influence between maternal depressive symptoms and adolescent adjustment may identify the best approaches for intervening to promote maternal and adolescent adjustment.
There are limitations to the study that need to be considered in future research. First, although a strength of the study is that variables were examined across two points in time, data were nonetheless correlational. Unmeasured variables (e.g., marital conflict) may have simultaneously been associated with heightened maternal depression and involvement in diabetes care, and poorer adolescent adjustment. Second, we focused only on mothers’ involvement and depressive symptoms, but recent findings suggest fathers’ involvement in diabetes care (Berg et al., 2008; Wysocki & Gavin, 2006) and depressive symptoms may be uniquely important for adolescent well-being (Reeb & Conger, 2009). Third, mothers’ depressive symptoms were relatively mild and based on a self-report measure that reflects distress factors beyond just general depression (Watson, 2009). Different findings may have occurred if mothers with clinically diagnosed depression had been examined, or if measures that clearly differentiate distress symptoms (e.g., depression from anxiety) had been utilized. Fourth, we have suggested that maladaptive parenting contributed to the findings that involvement was more weakly associated with adolescent adjustment when mothers were more depressed, but we did not measure parenting practices. We also measured only instrumental aspects of maternal involvement. Different relationships may have been found if other aspects of involvement in diabetes care had been measured (e.g., parent–adolescent relationship quality, parental monitoring; Eckshtain et al., 2010; Palmer et al., in press). Finally, results may not generalize beyond the small and fairly homogeneous sample that was studied, especially given evidence that different processes may be involved in explaining maternal depression associations with child adjustment across racial ethnic groups (Pachter, Auinger, Palmer, & Weitzman, 2006).
Depressive symptoms appeared to undermine mothers’ ability to be effective partners in managing diabetes during adolescence. Although mothers with more depressive symptoms were more instrumentally involved in their adolescent’s diabetes management tasks, such involvement was relatively ineffective. Future research is necessary to replicate these findings and to understand the processes by which they occur. If supported by future research, clinicians may facilitate adolescent diabetes management by monitoring and treating parental depressive symptoms, promoting more effective diabetes management and parenting skills in the affected parent, facilitating the teen’s own diabetes management skills, and identifying additional caregivers who may support the developing teen’s diabetes management.
Funding
Funding for this work was provided by a grant from the Primary Children’s Medical Center Research Foundation, Salt Lake City, UT, awarded to D.J.W. (PI) and C.A.B. (co-PI).
Conflicts of interest: none declared.
Acknowledgments
We thank the staff and families at the pediatric endocrinology clinics at Primary Children’s Medical Center and the Utah Diabetes Center, Salt Lake City, UT, USA. Portions of these data were presented at the annual meetings of the Society of Behavioral Medicine. The baseline methods and measures reported in this study were first reported in Palmer et al. (2004). The role of autonomy and pubertal status in understanding age differences in maternal involvement in diabetes responsibility across adolescence. Journal of Pediatric Psychology, 29, 35–46.
References
- Aiken L, West S. Multiple regression: Testing and interpreting interactions. Thousand Oaks, CA: Sage Publications, Inc; 1991. [Google Scholar]
- Anderson B, Ho J, Brackett J, Laffel L. Parental involvement in diabetes management tasks: Relationships to blood glucose monitoring adherence and metabolic control in young adults with insulin dependent diabetes mellitus. The Journal of Pediatrics. 1997;130:257–265. doi: 10.1016/s0022-3476(97)70352-4. [DOI] [PubMed] [Google Scholar]
- Arnett J A. Emerging adulthood: A theory of development from the late teens through the twenties. American Psychologist. 2000;55:469–480. [PubMed] [Google Scholar]
- Berg C A, Butler J, Osborn P, King G, Palmer D, Butner J, Murray M, Lindsay R, Donaldson D, Foster C, Swinyard M, Wiebe D J. The role of parental monitoring in understanding the benefits of parental acceptance on adolescent adherence and metabolic control of type 1 diabetes. Diabetes Care. 2008;31:678–683. doi: 10.2337/dc07-1678. [DOI] [PubMed] [Google Scholar]
- Berg C, Wiebe D J, Beveridge R, Palmer D, Korbel C, Upchurch R, Upchurch R, Swinyard M T, Lindsay R, David L, Donaldson D L, Donaldson D L. Mother-child appraised involvement in coping with diabetes stressors and emotional adjustment. Journal of Pediatric Psychology. 2007;3:995–1005. doi: 10.1093/jpepsy/jsm043. [DOI] [PubMed] [Google Scholar]
- Butler J, Berg C, King P, Gelfand D, Fortenberry K, Foster C, Wiebe D J. Parental negative affect and adolescent efficacy for diabetes management. Journal of Family Psychology. 2009;23:611–614. doi: 10.1037/a0016141. [DOI] [PubMed] [Google Scholar]
- Cameron L, Young M, Wiebe D. Maternal trait anxiety and diabetes control in adolescents with type 1 diabetes. Journal of Pediatric Psychology. 2007;32:733–744. doi: 10.1093/jpepsy/jsl053. [DOI] [PubMed] [Google Scholar]
- Cohen J. Statistical power analysis for the behavioral sciences. 2nd. New York: Lawrence Erlbaum; 1988. [Google Scholar]
- Downey G, Coyne J. Children of depressed parents: An integrative review. Psychological Bulletin. 1990;108:50–76. doi: 10.1037/0033-2909.108.1.50. [DOI] [PubMed] [Google Scholar]
- Eckshtain D, Ellis D, Kolmodin K, Naar-King S. The effects of parental depression and parenting practices on depressive symptoms and metabolic control in urban youth with insulin dependent diabetes. Journal of Pediatric Psychology. 2010;35:426–435. doi: 10.1093/jpepsy/jsp068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gelfand D, Teti D. The effects of maternal depression on children. Clinical Psychology Review. 1990;10:329–353. [Google Scholar]
- Goodman S, Gotlib I. Risk for psychopathology in the children of depressed mothers: A developmental model for understanding mechanisms of transmission. Psychological Review. 1999;106:458–490. doi: 10.1037/0033-295x.106.3.458. [DOI] [PubMed] [Google Scholar]
- Jaser S, Grey M. A pilot study of observed parenting and adjustment in adolescents with type 1 diabetes and their mothers. Journal of Pediatric Psychology. 2010;35:738–747. doi: 10.1093/jpepsy/jsp098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jaser S, Whittemore R, Ambrosino J, Lindemann E, Grey M. Mediators of depressive symptoms in children with type 1 diabetes and their mothers. Journal of Pediatric Psychology. 2008;33:509–519. doi: 10.1093/jpepsy/jsm104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kochanska G, Kuczynski L, Radke-Yarrow M, Welsh J. Resolutions of control episodes between well and affectively ill mothers and their young children. Journal of Abnormal Child Psychology. 1987;15:441–456. doi: 10.1007/BF00916460. [DOI] [PubMed] [Google Scholar]
- Korbel C, Wiebe D, Berg C, Palmer D. Gender differences in adherence to type 1 diabetes management across adolescence: The mediating role of depression. Children’s Health Care. 2007;36:83–98. [Google Scholar]
- Kovacs M. The Children’s Depression Inventory (CDI) Psychopharmacology Bulletin. 1985;21:995–998. [PubMed] [Google Scholar]
- Kovacs M, Goldston D, Obrosky D, Bonar L. Psychiatric disorders in youths with IDDM: Rates and risk factors. Diabetes Care. 1997;20:36–44. doi: 10.2337/diacare.20.1.36. [DOI] [PubMed] [Google Scholar]
- Lewin A B, LaGreca A M, Geffken G R, Williams L B, Duke D C, Storch E A, Silverstein J H. Validity and reliability of an adolescent and parent rating scale of type 1 diabetes adherence behaviors: The Self-Care Inventory (SCI) Journal of Pediatric Psychology. 2009;34:999–1007. doi: 10.1093/jpepsy/jsp032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nolen-Hoeksema S. The role of rumination in depressive disorders and mixed anxiety/depressive symptoms. Journal of Abnormal Psychology. 2000;109:504–511. [PubMed] [Google Scholar]
- Pachter L M, Auinger P, Palmer R, Weitzman M. Do parenting and the home environment, maternal depression, neighborhood and chronic poverty affect child behavioral problems differently in different racial-ethnic groups? Pediatrics. 2006;117:1329–1338. doi: 10.1542/peds.2005-1784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palmer D, Berg C, Wiebe D, Beveridge R, Korbel C, Upchurch R, Swinyard M T, Lindsay R, Donaldson D L. The role of autonomy and pubertal status in understanding age differences in maternal involvement in diabetes responsibility across adolescence. Journal of Pediatric Psychology. 2004;29:35–46. doi: 10.1093/jpepsy/jsh005. [DOI] [PubMed] [Google Scholar]
- Palmer D, Osborn P, King P S, Berg C A, Butler J, Butner J, Horton D, Wiebe D J. The structure of parental involvement and relations to disease management for youth with type 1 diabetes. Journal of Pediatric Psychology. 2010 doi: 10.1093/jpepsy/jsq019. Advance online publication. doi:10.1093/jpepsy/jsq019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Radloff L. The CES-D Scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:385–401. [Google Scholar]
- Reeb B, Conger K. The unique effect of paternal depressive symptoms on adolescent functioning: Associations with gender and father–adolescent relationship closeness. Journal of Family Psychology. 2009;23:758–761. doi: 10.1037/a0016354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rubin R R, Young-Hyman D, Peyrot M. Parent–child responsibility and conflict in diabetes care [Abstract] Diabetes. 1989;38(Suppl. 2):28A. [Google Scholar]
- Scalzo C, Williams P, Holmbeck G. Maternal self-assessed health and emotionality predict maternal response to child illness. Children’s Health Care. 2005;34:61–79. [Google Scholar]
- Watson D. Differentiating the mood and anxiety disorders: A quadripartite model. Annual Review of Clinical Psychology. 2009;5:221–247. doi: 10.1146/annurev.clinpsy.032408.153510. [DOI] [PubMed] [Google Scholar]
- Webster-Stratton C, Hammond M. Maternal depression and its relationship to life stress, perceptions of child behavior problems, parenting behaviors, and child conduct problems. Journal of Abnormal Child Psychology. 1988;16:299–315. doi: 10.1007/BF00913802. [DOI] [PubMed] [Google Scholar]
- Wiebe D, Berg C, Korbel C, Palmer D, Beveridge R, Upchurch R, Lindsay R, Swinyard M T, Donaldson D. Children’s appraisals of maternal involvement in coping with diabetes: Enhancing our understanding of adherence, metabolic control, and quality of life across adolescence. Journal of Pediatric Psychology. 2005;30(2):167–178. doi: 10.1093/jpepsy/jsi004. [DOI] [PubMed] [Google Scholar]
- Wysocki T, Gavin L. Parental involvement in the management of pediatric chronic diseases: Associations with adherence, quality of life, and health status. Journal of Pediatric Psychology. 2006;31:501–511. doi: 10.1093/jpepsy/jsj042. [DOI] [PubMed] [Google Scholar]
- Wysocki T, Iannotti R, Weissberg-Benchell J, Laffel L, Hood K, Anderson B, Chen R. Diabetes problems solving by youths with type 1 diabetes and their caregivers: Measurment, validation, and longitudinal associations with glycemic control. Journal of Pediatric Psychology. 2008;33:875–884. doi: 10.1093/jpepsy/jsn024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wysocki T, Nansel T R, Holmbeck G N, Chen R, Laffel L, Anderson B J, Weissberg-Benchell J. Collaborative involvement of primary and secondary caregivers: Associations with youth outcomes. Journal of Pediatric Psychology. 2009;34:869–881. doi: 10.1093/jpepsy/jsn136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wysocki T, Taylor A, Hough B S, Linscheid T R, Yeates K O, Naglieri J A. Deviation from developmentally appropriate self-care autonomy: Association with diabetes outcomes. Diabetes Care. 1996;19:119–125. doi: 10.2337/diacare.19.2.119. [DOI] [PubMed] [Google Scholar]