Abstract
Background
Onset of disability, risk for future falls, frailty, functional decline, and mortality are strongly associated with a walking speed of less than 1.0 m/s.
Objective
The study objective was to determine whether there were differences in slow walking speed (<1.0 m/s) between community-dwelling African American and white American adult women with osteoarthritis symptoms. An additional aim was to examine whether racial differences in walking speed can be attributed to age, obesity, socioeconomic factors, disease severity, or comorbidities.
Design
A cross-sectional design was used.
Methods
Community-dwelling adults were recruited from Baltimore, Maryland; Columbus, Ohio; Pittsburgh, Pennsylvania; and Pawtucket, Rhode Island. Participants were 2,648 women (23% African American) who were 45 to 79 years of age and had a self-selected baseline walking speed of 20 m/s in the Osteoarthritis Initiative Study. Mixed-effects logistic regression models were used to examine racial differences in walking speed (<1.0 m/s versus ≥1.0 m/s), with adjustments for demographic factors, socioeconomic factors, disease severity, and comorbidities.
Results
Walking speed was significantly slower for African American women than for white American women (mean walking speed=1.19 and 1.33 m/s, respectively). The prevalence of a walking speed of less than 1.0 m/s in this cohort of middle-aged women was 9%; about 50% of the women with a walking speed of less than 1.0 m/s were younger than 65 years. Women with a walking speed of less than 1.0 m/s had lower values for socioeconomic factors, higher values for disease severity, and higher prevalences of obesity and comorbidities than those with a walking speed of ≥1.0 m/s. After controlling for these covariates, it was found that African American women were 3 times (odds ratio=2.9; 95% confidence interval=2.0, 4.1) more likely to have a walking speed of less than 1.0 m/s than white American women.
Limitations
The study design made it impossible to know whether a walking speed of less than 1.0 m/s in women who were 45 years of age or older was a predictor of future poor health outcomes.
Conclusions
In this study, race was independently associated with a walking speed of less than 1.0 m/s in community-dwelling women who had or were at risk for osteoarthritis, with African American women having 3 times the risk for slow walking as white American women. This finding suggests that middle-aged African American women have an increased risk for poor health outcomes. Further longitudinal evaluations are needed to confirm the long-term health outcomes in a middle-aged population and to establish walking speed as a useful tool for identifying middle-aged women at high risk for poor health outcomes.
Knee osteoarthritis (OA) is a progressive chronic disease, affects over 9 million adults in the United States,1 and is a leading cause of disability among adults who are not living in institutions.2 Women who are 55 to 64 years old and are obese have the highest risk for a new knee OA diagnosis.3 African American women have more than twice the prevalence of knee OA as white American women (23.1% versus 8.5%, respectively).4 Compared with men, women have more debilitating knee pain and disability,5,6 and, although women are twice as likely to need joint replacement surgery, they are 3 times less likely to receive it.7 Because women are more likely to present with advanced knee OA, greater disability, and delayed treatment, it is important to identify the onset of disease and disability early to reduce disease progression and health-related disparities and to improve health outcomes for women with OA.
Walking speed is a simple, clinical indicator that can reliably evaluate health and functional status in older adults.8 Walking speed is consistent from 20 to 60 years of age and then declines.9 In women, the normal walking speed ranges from 1.30 to 1.40 m/s at 40 to 69 years of age and declines to 1.06 to 1.13 m/s by 70 to 79 years of age.9–11 Older adults with walking speeds of less than 1.0 m/s are considered to be at risk for poor health outcomes (ie, frailty, disability, increased risk for future falls, and mortality).12–17
It is well established that women walk more slowly than men.18–21 Preliminary evidence suggests that race differences in walking speed also exist.22–24 In a cohort of African American and white American women who were middle-aged (mean age=46.9 years), 12% of the population walked more slowly than 1.0 m/s, a walking speed considered to be normal for a woman 3 decades older than the mean age in the study.25 Blanco et al22 found that older African American adults walked significantly more slowly than older white American adults. In another study of people with knee OA, African American men and women walked more slowly than white American men and women, although disease severity (radiographic evidence of OA) did not differ between the races.24 Other studies evaluating older adults have related differences in African American and white American populations to socioeconomic status,26,27 disability,28 and frailty,29 highlighting the importance of these factors. The evaluation of factors (eg, socioeconomic status, disability, and frailty) that may influence walking speed in middle-aged African American and white American adults remains an area for further investigation.
Racial and ethnic differences in health outcomes exist.30 Determining whether these differences are true differences or are due to cultural differences has been poorly explored.31,32 Recent efforts by the National Quality Forum introduced the concept of disparity-sensitive measurement to effectively evaluate health-related disparities.33 The National Quality Forum defined disparity-sensitive measures as those “that serve to detect not only differences in quality across institutions or in relation to certain benchmarks, but also differences in quality among populations or social groupings (race/ethnicity, language, etc).”33 Disparity-sensitive measurement has not been applied to health outcomes but represents an improved cultural measurement method that may lead to more accurate identification of health-related disparities—which is important if these disparities are to be reduced.34 Measurement tools, such as walking speed, must be evaluated in different races and cultures to accurately assess health outcomes.31,32,34 The evaluation of walking speed in people with knee OA may be a method for identifying those at risk for poor health outcomes and confirming that the observed differences in health outcomes are true differences and not a reflection of cultural norms, beliefs, and values.34
The purpose of this study was to determine whether there were differences in slow walking speed (<1.0 m/s) between community-dwelling African American and white American adult women with OA symptoms. An additional aim was to examine whether racial differences in walking speed can be attributed to age, obesity, socioeconomic factors, disease severity, or comorbidities.
Method
Data Source
The Osteoarthritis Initiative (OAI) is a longitudinal, multicenter public-private partnership, observational study of knee OA in men and women who were 45 to 79 years of age, were enrolled between February 2004 and May 2006, and who either had or were at risk for developing knee OA (N=4,796). Participants were recruited from Baltimore, Maryland; Columbus, Ohio; Pittsburgh, Pennsylvania; and Pawtucket, Rhode Island. Recruitment focused on 2 subcohorts (progression and incidence). The progression subcohort (n=1,390) included people who had prevalent symptoms of OA in one or both knees, frequent pain (pain on most days of a month in the preceding year), or definite osteophytes in the same knee. The incidence subcohort (n=3,284) included people who were at risk for developing symptomatic knee OA, defined as having one or more of the following risk factors: frequent knee pain without radiographic evidence of OA, radiographic evidence of OA without frequent pain, infrequent knee pain, overweight for age and sex, history of knee injury/surgery, family history of knee replacement, Heberden nodes, or age of 70 to 79 years. People with inflammatory or rheumatoid arthritis, bilateral end-stage knee OA (defined as radiographically evident Kellgren-Lawrence [K/L] grade 4), or bilateral total knee replacement were excluded.
Data used in the preparation of this article were obtained from the OAI database, which is available for public access at http://www.oai.ucsf.edu/. Because of the differences in advanced knee OA between men and women, only women in both the progression and incidence subcohorts for whom baseline walking speed data were available were included in the present study (n=2,648).
Outcome Measures
Walking speed was the average of 2 timed 20-m walk tests of “usual walking” performed at baseline. Using a standardized protocol, certified site assessors adjudicated the timed 20-m walk tests for the OAI study. The 20-m test has norm-based values for adults older than 18 years. Calculated in meters per second, a poor health outcome was defined as a walking speed of less than 1.0 m/s.8,12–14 The primary outcome variable was whether a participant had a walking speed of less than 1.0 m/s compared with a walking speed of ≥1.0 m/s.
The explanatory variables that were considered for the model were categorized as demographic, socioeconomic, disease severity, and comorbidity. Demographic variables included age categories (<55, 55–64, 65–74, and 75–80 years), race/ethnicity (African American or white American), body mass index (BMI) by group (healthy weight and underweight: BMI of less than 24.9 kg/m2; overweight: BMI of 25.0–29.9 kg/m2; obese: BMI of ≥30.0 kg/m2). One of the socioeconomic factors was medical care access (yes/no), defined by the following question in the OAI database: “Do you currently have any kind of health care coverage? This would include private health insurance (such as Blue Cross), prepaid plans (such as HMOs [health maintenance organizations], PPOs [preferred provider organizations], or any government-sponsored plans (such as Medicare, Medicaid, or VA coverage).” Other socioeconomic factors were level of education (high school and less/more than high school) and annual income (<$50,000/≥$50,000), defined by the following statement: “The following question refers to your personal family income for the last year, including all sources, such as wages, salaries, Social Security or retirement benefits, help from relatives, and rent from property.”
Clinical and radiological discordance exists in the diagnostic criteria for OA.35 Both radiological and clinical symptoms are included to determine radiological and symptom severity. The baseline K/L grade was used to report radiographically evident knee OA severity. Although a K/L grade of less than 2 usually is defined as “normal,” the OAI uses comprehensive admission criteria for participation and defines a K/L grade of less than 2 as “mild” knee OA.36 For radiological severity in the present study, a K/L grade of ≤2 was defined as “mild/moderate” knee OA, and a K/L grade of greater than 2 was defined as “severe” knee OA. Clinical severity was based on participant-reported knee pain in the preceding 30 days and 12 months. Participants reporting either “no pain in past 12 months” or “pain in past 12 months that did not occur on most days of month” were categorized as having no knee pain, and those categorized as having knee pain were participants reporting “pain most days of a month in past 12 months.”
Comorbidities included back pain (the presence of any back pain in the preceding 30 days [yes/no]), diabetes (yes/no), cancer (yes/no), heart failure (yes/no), hypertension (yes/no) (hypertension was defined as systolic blood pressure of 140–159 mm Hg or diastolic blood pressure of 90–99 mm Hg, and not having hypertension was defined as normal blood pressure [systolic blood pressure of <120 mm Hg or diastolic blood pressure of <80 mm Hg] or prehypertension blood pressure [systolic blood pressure of 120–139 mm Hg or diastolic blood pressure of 80–89 mm Hg]), rheumatoid arthritis (yes/no), stroke (yes/no), ulcer (yes/no), asthma (yes/no), lung disease (yes/no), and depression measured with the Center for Epidemiologic Studies Depression Scale (CES-D). The CES-D is a 20-item measure rating depression symptoms over the preceding week. Cutoff scores of ≥16 have been reliably used to identify people at risk for depression.37 We categorized participants with a CES-D score of less than 16 as having no depression and those with a CES-D score of ≥16 as having depression. Because variations at recruitment sites may have influenced outcomes, recruitment sites were given letter designations (A–E) and treated as nominal variables in the analysis.
Data Analysis
Descriptive analyses (frequency and percentage) were performed to characterize the explanatory variables by race (African American or white American) and primary outcome (walking speed of <1.0 m/s or ≥1.0 m/s). Associations between walking speed and the interaction variables age and race, age and BMI, age and recruitment site, race and BMI, and race and recruitment site were statistically evaluated.
Missing values for each variable are shown in Table 1. The variable rheumatoid arthritis had a high frequency of missing values (16.3%) and few positive responses (1.4%) in the study population; therefore, it was excluded from the analyses. On the basis of the observed variables (age, race, and walking speed), multiple imputation38 (PROC MI procedure with a fully conditional specification method for class variables) was used to manage the missing explanatory variable values (<6% imputed) (Tab. 1). In the fully conditional specification method, a separate conditional distribution is used for each imputed variable; the imputation procedure is considered to be robust for study data.39
Table 1.
Descriptive Characteristics of the Participants
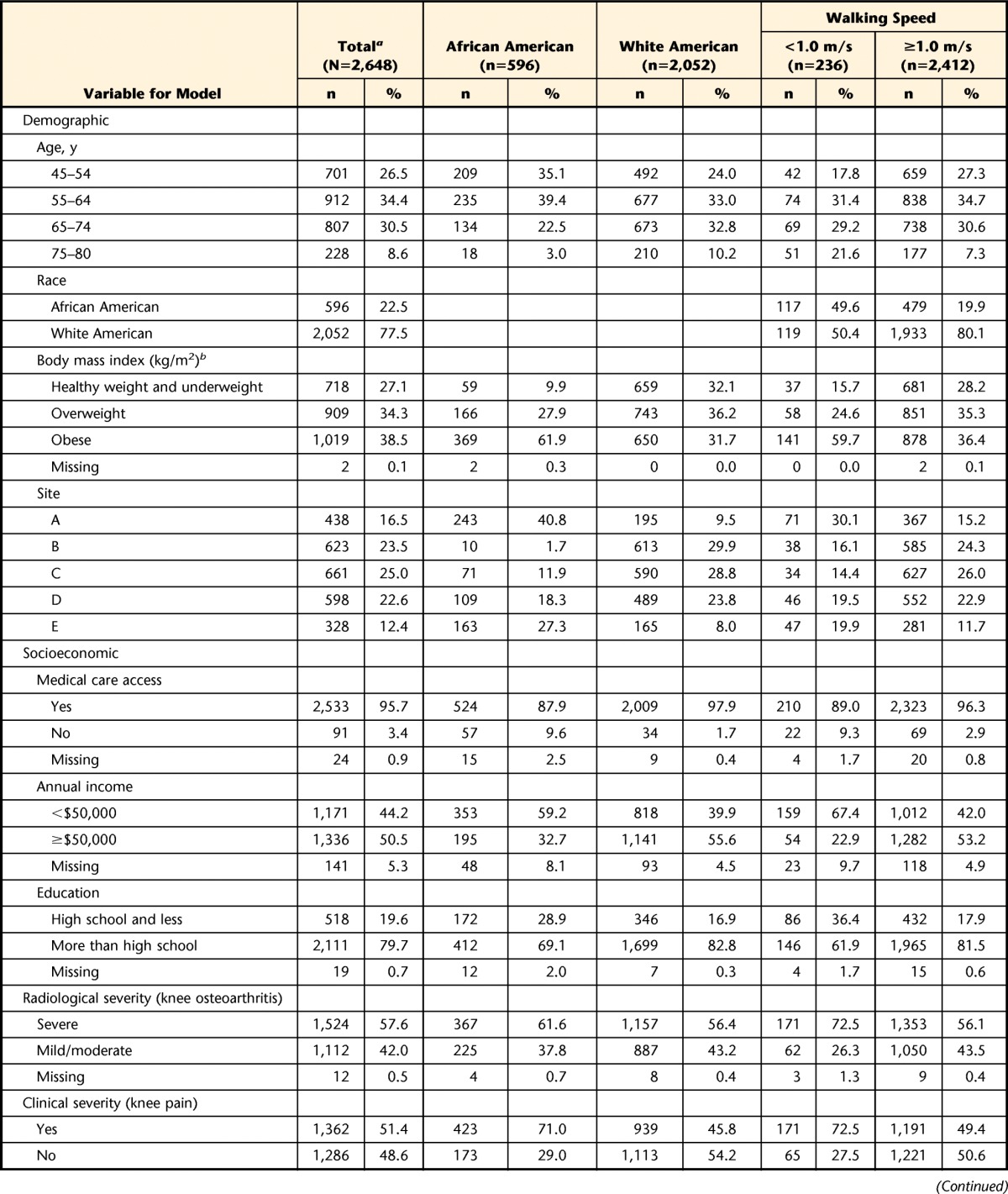
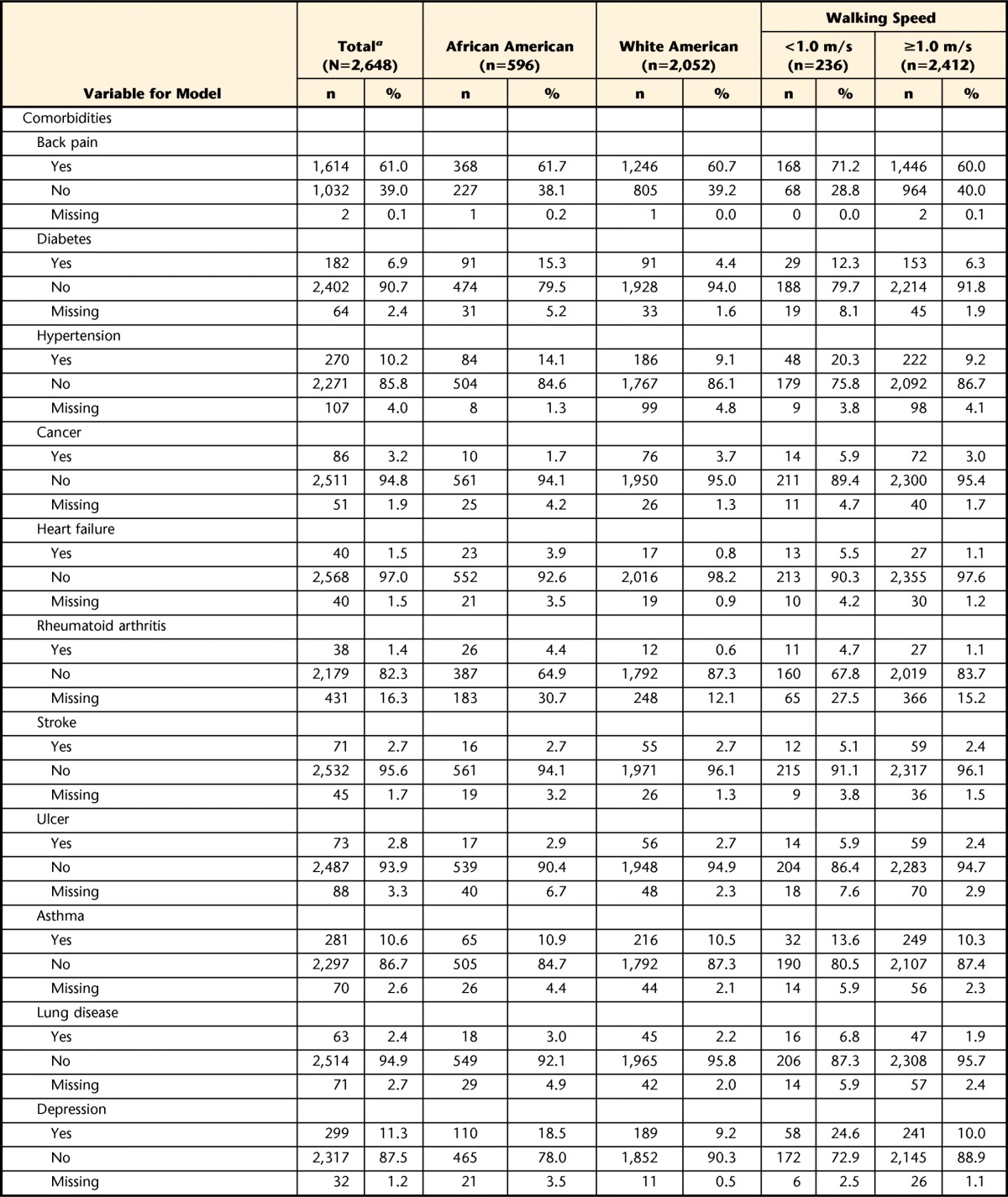
a The 0.1% error for radiological severity, back pain, cancer, and asthma is related to rounding.
b Healthy weight and underweight=body mass index of less than 24.9 kg/m2, overweight=body mass index of 25.0–29.9 kg/m2, obese=body mass index of ≥30.0 kg/m2.
Mixed-effects logistic regression models, with the recruitment site as a random effect, were used to estimate the association between walking speed and race, given the following model conditions (models 0–4): model 0 included only race as an explanatory variable; model 1 included all demographic variables (race, age, and BMI); model 2 included model 1 and socioeconomic factors (medical care access, annual income, and education); model 3 included model 2 and disease severity (knee OA and knee pain); and model 4 included model 3 and comorbidity. The statistical significance level was set at .05. All statistics were computed with SAS 9.4 (SAS Institute Inc, Cary, North Carolina).
Role of the Funding Source
The data used in the preparation of this article were obtained from the OAI database. The OAI is a public-private partnership comprising 5 contracts (N01-AR-2-2258, N01-AR-2-2259, N01-AR-2-2260, N01-AR-2-2261, and N01-AR-2-2262) funded by the National Institutes of Health, a branch of the US Department of Health and Human Services, and conducted by the OAI study investigators. Private funding partners include Merck Research Laboratories, Novartis Pharmaceuticals Corporation, GlaxoSmithKline, and Pfizer Inc. Private sector funding for the OAI is managed by the Foundation for the National Institutes of Health. This manuscript was prepared using an OAI public use data set and does not necessarily reflect the opinions or views of the OAI investigators, the NIH, or the private funding partners.
Results
A total of 2,648 women (23% African American) ranging in age from 45 to 79 years were included in the present study (Tab. 1). The mean walking speed was significantly (P<.001) slower for African American women (1.19 m/s) than for white American women (1.33 m/s), despite African American women being significantly younger than white American women (mean ages: 59.0 years [SD=8.0 years] and 62.4 years [SD=9.1 years], respectively).
A total of 9% (n=236) of the middle-aged women (n=2,648) had a walking speed of less than 1.0 m/s. Of these, approximately half were younger than 65 years, approximately half were African American, and the majority (60%) were considered obese. Furthermore, those with a walking speed of less than 1.0 m/s had lower levels of education, annual income, and medical care access; a higher level of knee OA disease severity; and a higher frequency of comorbidities than those walking at speeds of ≥1.0 m/s.
Differences in comorbidities by race suggested that, relative to white American women, a higher proportion of African American women with or at risk for OA were managing chronic conditions. The majority (62%) of African American women and one third (32%) of white American women were considered obese (BMI ≥30 kg/m2). Diabetes, heart failure, and hypertension were more prevalent in African American women than in white American women.
Table 2 shows that the addition of demographic, socioeconomic, disease severity, and comorbidity factors slightly attenuated the unadjusted model (model 0) and that the associations between race and a walking speed of less than 1.0 m/s were similar. The unadjusted results (model 0) indicated that African American women were 3.5 times more likely to have a walking speed of less than 1.0 m/s than white American women (odds ratio [OR]=3.47; 95% confidence interval [CI]=2.55, 4.71). When only age and BMI were added to the model, the likelihood of African American women walking less than 1.0 m/s increased slightly (OR=3.79; 95% CI=2.68, 5.37). None of the interaction dyads (age and race, age and BMI, age and recruitment site, race and BMI, and race and recruitment site) were found to be significantly (P<.05) associated with walking speed. After controlling for demographic factors, socioeconomic factors, and comorbidities, we found that African American women were 3 times more likely to have a low walking speed (<1.0 m/s) than white American women (OR=2.83; 95% CI=1.96, 4.08) (Tab. 3).
Table 2.
Association Between Race and Walking at Slow Speed (<1.0 m/s)
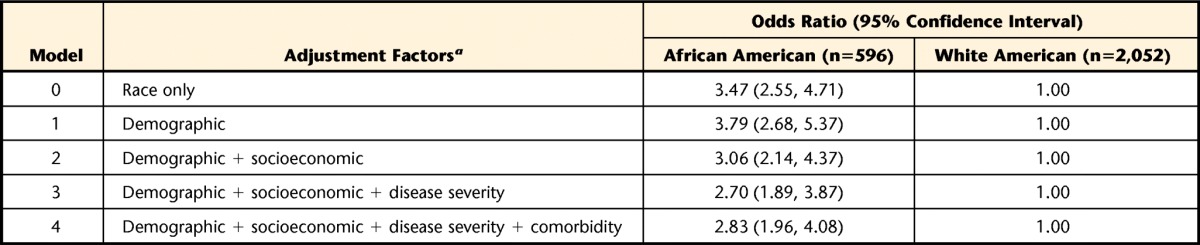
a Demographic=race, age, and body mass index; socioeconomic=medical care access, annual income, and education; disease severity=knee osteoarthritis and knee pain.
Table 3.
Association Between Race and Walking Speed (<1.0 m/s and ≥1.0 m/s), as Determined by Multivariable Mixed-Effects Logistic Regression (N=2,648)a
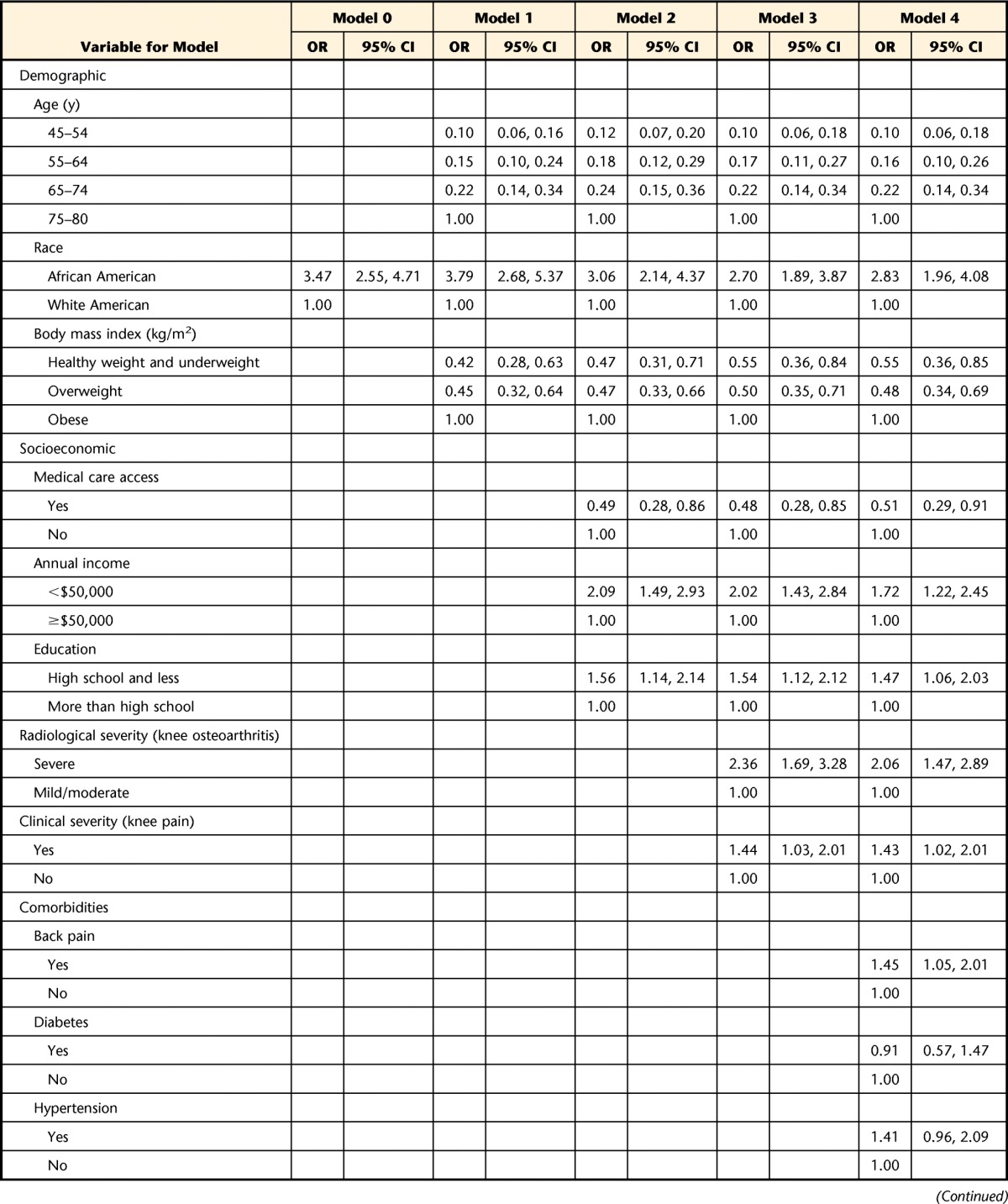
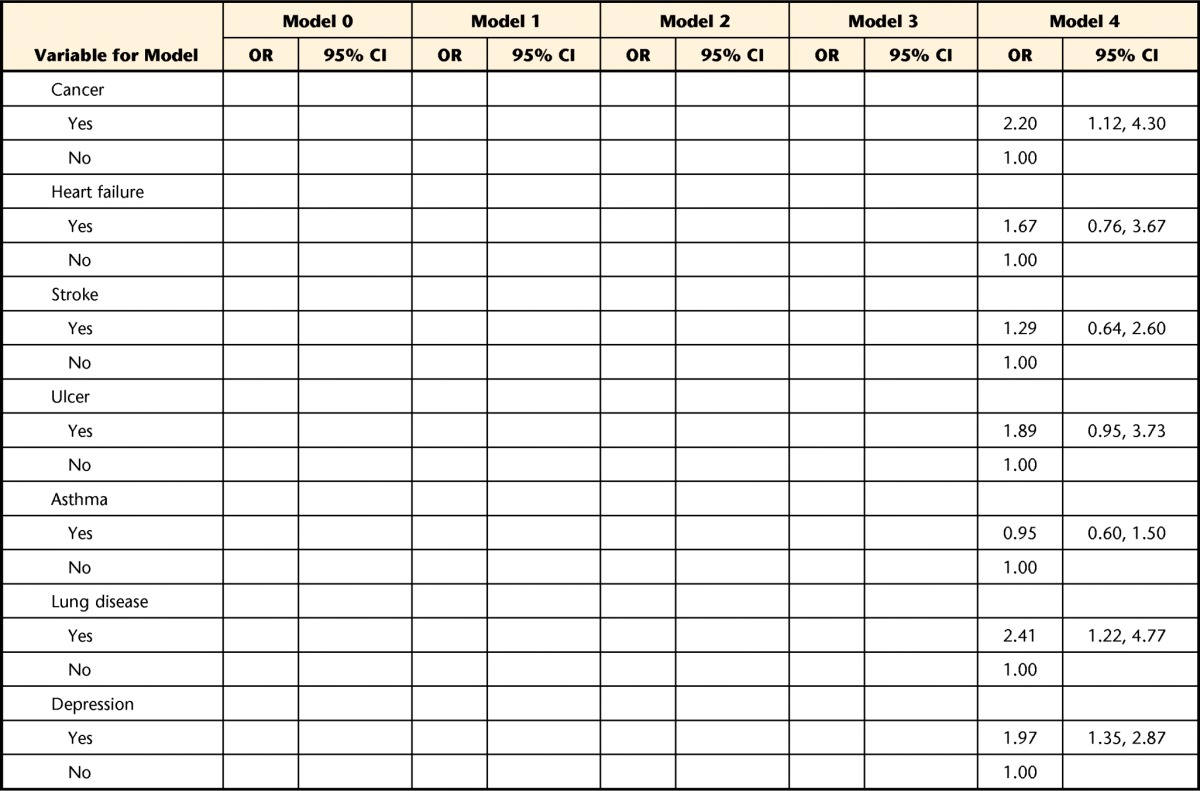
OR=odds ratio, CI=confidence interval.
Discussion
Among women who lived in the community, were 45 years of age or older, and had knee OA symptoms, race was associated with being at risk for a walking speed of less than 1.0 m/s. This association was independent of numerous potential confounding variables, including age, obesity, socioeconomic factors, disease severity, and comorbidities. A walking speed of less than 1.0 m/s has been shown to be a general indicator of overall health that can predict future adverse health events in older adults.8,9 On the basis of norms established primarily for white American populations,8–11 the results of the present study suggest that middle-aged African American women with knee OA may have an increased risk for future poor health outcomes and present a rationale to determine whether a link between walking speed and poor health outcomes in middle-aged women exists.
The evaluation of walking speed may be useful for managing population health. Such an evaluation is simple, inexpensive, easy to perform and interpret, crosses all cultures, and can be implemented across a variety of community and clinical settings. The criterion establishing slow walking speed as a predictor of poor outcomes in an older population was based on primarily white populations; validation of this criterion for different races, ages, and health conditions needs to be considered.
Differences in walking speed by race may have serious consequences for policy and service deliveries that are developed on the basis of walking speed evaluation.34,40 For the advancement of knowledge about health-related disparities in women with or at risk for OA, normative values for walking speed by race need to be confirmed and compared with the walking speeds of our cohort. Without this knowledge, it is not possible to determine whether differences between African American and white American women are attributable to cultural norms and beliefs or to true differences in health outcomes. For example, in the present study of middle-aged women, the majority of African American women were younger than 65 years (75%) and walked at a mean speed of 1.2 m/s. On the basis of normative data for this age,9–11 the expected walking speed is 1.3 m/s. If the current walking speed criterion is not confirmed for the African American population, African American women with OA and a slow walking speed may be inappropriately identified as being below the normative criterion because their natural walking speed is slower than that of white American women with OA. Alternatively, our data support previous reports of significant differences in disability and disease progression between African American and white American women.28 If the current walking speed criterion is valid for African American women, the findings of the present study suggest that African American women with a walking speed of less than 1.0 m/s may be at high risk for poor health outcomes and a loss of independence.17 Further efforts to validate the use of walking speed evolution for different middle-aged racial populations are needed.
Mobility is a large part of independent living and may be considered one of the most important functional requirements for maintaining social roles among older adults.41 Independence with daily activities and stair climbing are mobility skills that require a high level of function and pose the greatest risk to independence in people with knee OA.2 For people to independently continue their daily activities, a minimum walking speed of 1.11 m/s is considered necessary.2,17 This information suggests that our cohort of women (African American and white American) were independent with activities of daily living. The ability to climb stairs (1.33 m/s) is considered to be an advanced mobility skill.17,42 The results of the present study suggest that only white American women had a mean walking speed that indicated independence with this skill.
The findings of the present study support the influence of demographic, socioeconomic, disease severity, and comorbidity factors on walking speed, as previously reported for older populations.24,26 Differences and influences of these factors were shown by the sequential addition of grouped factors in the models. For example, the addition of demographic factors created a higher likelihood that African American women walked at speeds of less than 1.0 m/s; however, in the full model, the strength of the association between race and walking speed was slightly reduced, but the relationship was retained. The complexity of the multifactorial components (demographic factors, socioeconomic factors, disease severity, and comorbidities) provides direction on potential areas for targeting interventions. Coexisting with obesity are cardiovascular comorbidities, such as hypertension, and diabetes, which often occur concurrently with OA and are highly prevalent in African American women.43 Hypertension is 9 times more prevalent, occurs earlier, and is more severe in African American women than in white American women.43 These competing health priorities in people with multiple conditions have been shown to result in less-than-ideal management of the conditions.44 Walking speed provides an opportunity to evaluate these conditions with one simple, clinical measure and link their effects with a simple measure of independence, essentially providing a means for people and communities to recognize their own health needs.
The present study was cross-sectional; therefore, the study findings are limited to a point in time. Further evaluation is needed to determine whether middle-aged women with a walking speed of less than 1.0 m/s are at high risk for future poor health outcomes and to determine whether a change in walking speed (improvement, no change, or decline) over time affects the rate at which these changes occur.
The generalizability of the findings is limited to middle-aged women, and the findings cannot be extrapolated to men. Recent evidence supports sex differences in the management of knee OA.5 Although women have more pain and disability than men, conservative treatments—such as exercise, activity modification, and weight loss—have not been evaluated in men and women separately. With regard to knee OA treatments for which sex differences have been evaluated, women are more likely than men to use alternative medicine and less likely than men to undergo a total knee arthroplasty for end-stage knee OA management.5,7 Understanding the sex differences is instrumental in reducing disparities in OA disease management in women.
Although we used established walking speed normative values,9–11 these normative values have not been extensively evaluated for different races. Further research should substantiate whether a walking speed of less than 1.0 m/s predicts poor health outcomes in African American women.
Previous studies showed that older African American women have increased frailty, disability, and socioeconomic status. The small proportion (3%) of African American women older than 75 years in the present study suggests that we may have underestimated the incidence of frailty and disability in African American women in this age group. Because we do not have walking speed information for this age group, we cannot generalize our findings to an older population of African American women with or at risk for knee OA. This topic remains an area for future evaluation.
In conclusion, walking at a speed of less than 1.0 m/s is associated with an increased risk for poor health outcomes and a loss of independent mobility in older adults. From a clinical perspective, the identification of women at high risk for future poor health outcomes is critical so that efforts to reduce the burden of illness due to OA have intention. In the present study of middle-aged women with or at risk for knee OA, African American women walked more slowly than white American women, and race was independently associated with walking at a speed of less than 1.0 m/s. There is great potential for walking speed to become an important disparity-sensitive instrument for middle-aged women with OA in that it may be able to identify early disability and predict health outcomes for this population. For this potential to be realized, longitudinal predictive studies need to be done and normative walking speeds for different races need to be confirmed.
Footnotes
Dr Kirkness provided concept/idea/research design and project management. Both authors provided writing and data analysis.
The study protocol, amendments, and informed consent documentation were reviewed and approved by local institutional review boards.
The data used in the preparation of this article were obtained from the Osteoarthritis Initiative (OAI) database. The OAI is a public-private partnership comprising 5 contracts (N01-AR-2-2258, N01-AR-2-2259, N01-AR-2-2260, N01-AR-2-2261, and N01-AR-2-2262) funded by the National Institutes of Health, a branch of the US Department of Health and Human Services, and conducted by the OAI study investigators. Private funding partners include Merck Research Laboratories, Novartis Pharmaceuticals Corporation, GlaxoSmithKline, and Pfizer Inc. Private sector funding for the OAI is managed by the Foundation for the National Institutes of Health. This manuscript was prepared using an OAI public use data set and does not necessarily reflect the opinions or views of the OAI investigators, the NIH, or the private funding partners.
References
- 1. Lawrence RC, Felson DT, Helmick CG, et al. Estimates of the prevalence of arthritis and other rheumatic conditions in the United States, part II. Arthritis Rheum. 2008;58:26–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Guccione AA, Felson DT, Anderson JJ, et al. The effects of specific medical conditions on the functional limitations of elders in the Framingham Study. Am J Public Health. 1994;84:351–358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Losina E, Weinstein AM, Reichmann WM, et al. Lifetime risk and age at diagnosis of symptomatic knee osteoarthritis in the US. Arthritis Care Res (Hoboken). 2013;65:703–711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Sowers MR, Lachance L, Hochberg M, Jamadar D. Radiographically defined osteoarthritis of the hand and knee in young and middle-aged African American and Caucasian women. Osteoarthritis Cartilage. 2000;8:69–77. [DOI] [PubMed] [Google Scholar]
- 5. Hame SL, Alexander RA. Knee osteoarthritis in women. Curr Rev Musculoskeletal Med. 2013;6:182–187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Centers for Disease Control and Prevention. Prevalence of doctor-diagnosed arthritis and arthritis-attributable activity limitation: United States, 2007–2009. MMWR Morb Mortal Wkly Rep. 2010;59:1261–1265. [PubMed] [Google Scholar]
- 7. Hawker GA, Wright JG, Coyte PC, et al. Differences between men and women in the rate of use of hip and knee arthroplasty. N Engl J Med. 2000;342:1016–1022. [DOI] [PubMed] [Google Scholar]
- 8. Studenski S, Perera S, Patel K, et al. Gait speed and survival in older adults. JAMA. 2011;305:50–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Bohannon RW, Andrews AW. Normal walking speed: a descriptive meta-analysis. Physiotherapy. 2011;97:182–189. [DOI] [PubMed] [Google Scholar]
- 10. Bohannon RW. Comfortable and maximum walking speed of adults aged 20-79 years: reference values and determinants. Age Ageing. 1997;26:15–19. [DOI] [PubMed] [Google Scholar]
- 11. Bohannon RW, Andrews AW, Thomas MW. Walking speed: reference values and correlates for older adults. J Orthop Sports Phys Ther. 1996;24:86–90. [DOI] [PubMed] [Google Scholar]
- 12. Purser JL, Weinberger M, Cohen HJ, et al. Walking speed predicts health status and hospital costs for frail elderly male veterans. J Rehabil Res Dev. 2005;42:535–546. [DOI] [PubMed] [Google Scholar]
- 13. Montero-Odasso M, Schapira M, Soriano ER, et al. Gait velocity as a single predictor of adverse events in healthy seniors aged 75 years and older. J Gerontol A Biol Sci Med Sci. 2005;60:1304–1309. [DOI] [PubMed] [Google Scholar]
- 14. Ostir GV, Kuo YF, Berges IM, et al. Measures of lower body function and risk of mortality over 7 years of follow-up. Am J Epidemiol. 2007;166:599–605. [DOI] [PubMed] [Google Scholar]
- 15. Rolland Y, Lauwers-Cances V, Cesari M, et al. Physical performance measures as predictors of mortality in a cohort of community-dwelling older French women. Eur J Epidemiol. 2006;21:113–122. [DOI] [PubMed] [Google Scholar]
- 16. Middleton A, Fritz SL, Lusardi M. Walking speed: the functional vital sign. J Aging Phys Act. 2015;23:314–322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Lusardi M. Using walking speed in clinical practice. Top Geriatr Rehabil. 2012;28:77–90. [Google Scholar]
- 18. Ayis S, Ebrahim S, Williams S, et al. Determinants of reduced walking speed in people with musculoskeletal pain. J Rheumatol. 2007;34:1905–1912. [PubMed] [Google Scholar]
- 19. Beckett LA, Brock DB, Lemke JH, et al. Analysis of change in self-reported physical function among older persons in four population studies. Am J Epidemiol. 1996;143:766–778. [DOI] [PubMed] [Google Scholar]
- 20. Ferrucci L, Penninx BW, Leveille SG, et al. Characteristics of nondisabled older persons who perform poorly in objective tests of lower extremity function. J Am Geriatr Soc. 2000;48:1102–1110. [DOI] [PubMed] [Google Scholar]
- 21. Murtagh KN, Hubert HB. Gender differences in physical disability among an elderly cohort. Am J Public Health. 2004;94:1406–1411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Blanco I, Verghese J, Lipton RB, et al. Racial differences in gait velocity in an urban elderly cohort. J Am Geriatr Soc. 2012;60:922–926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Sowers MR, Crutchfield M, Richards K, et al. Sarcopenia is related to physical functioning and leg strength in middle-aged women. J Gerontol A Biol Sci Med Sci. 2005;60:486–490. [DOI] [PubMed] [Google Scholar]
- 24. Sims EL, Keefe FJ, Kraus VB, et al. Racial differences in gait mechanics associated with knee osteoarthritis. Aging Clin Exp Res. 2009;21:463–469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Sowers MR, Jannausch ML, Gross M, et al. Performance-based physical functioning in African-American and Caucasian women at midlife: considering body composition, quadriceps strength, and knee osteoarthritis. Am J Epidemiol. 2006;163:950–958. [DOI] [PubMed] [Google Scholar]
- 26. Thorpe RJ, Jr, Koster A, Kritchevsky SB, et al. Race, socioeconomic resources, and late-life mobility and decline: findings from the Health, Aging, and Body Composition study. J Gerontol A Biol Sci Med Sci. 2011;66:1114–1123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Thorpe RJ, Jr, Kasper JD, Szanton SL, et al. Relationship of race and poverty to lower extremity function and decline: findings from the Women's Health and Aging Study. Soc Sci Med. 2008;66:811–821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Mendes de Leon CF, Barnes LL, Bienias JL, et al. Racial disparities in disability: recent evidence from self-reported and performance-based disability measures in a population-based study of older adults. J Gerontol B Psychol Sci Soc Sci. 2005;60:S263–S271. [DOI] [PubMed] [Google Scholar]
- 29. Hirsch C, Anderson ML, Newman A, et al. The association of race with frailty: the Cardiovascular Health Study. Ann Epidemiol. 2006;16:545–553. [DOI] [PubMed] [Google Scholar]
- 30. Stith AY, Nelson AR. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health. Washington, DC: Institute of Medicine; 2002. [Google Scholar]
- 31. Snowden LR. Bias in mental health assessment and intervention: theory and evidence. Am J Public Health. 2003;93:239–243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Scholderer J, Grunert KG, Brunso K. 2005. A procedure for eliminating additive bias from cross-cultural survey data. Journal of Business Research. 2005;58:72–78. [Google Scholar]
- 33. National Quality Forum. Healthcare Disparities and Cultural Competency Consensus Standards: Commissioned Paper, Healthcare Disparities Measurement. Santa Monica, CA: Rand Corp; 2011:6. [Google Scholar]
- 34. Ramirez M, Ford ME, Stewart AL, Teresi JA. Measurement issues in health disparities research. Health Serv Res. 2005;40:1640–1657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Berger MJ, Kean CO, Goela A, Doherty TJ. Disease severity and knee extensor force in knee osteoarthritis: data from the Osteoarthritis Initiative. Arthritis Care Res (Hoboken). 2012;64:729–734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Duncan R, Peat G, Thomas E, et al. How do pain and function vary with compartmental distribution and severity of radiographic knee osteoarthritis? Rheumatology (Oxford). 2008;47:1704–1707. [DOI] [PubMed] [Google Scholar]
- 37. Lewinsohn PM, Seeley JR, Roberts RE, Allen NB. Center for Epidemiologic Studies Depression Scale (CES-D) as a screening instrument for depression among community-residing older adults. Psychol Aging. 1997;12:277–287. [DOI] [PubMed] [Google Scholar]
- 38. Rubin DB. Multiple Imputation for Nonresponse in Surveys. New York, NY: Wiley; 1987. [Google Scholar]
- 39. Enders CK. Applied Missing Data Analysis. New York, NY: Guilford Press; 2010. [Google Scholar]
- 40. Arcia E, Skinner M, Bailey D, Correa V. Models of acculturation and health behaviors among Latino immigrants to the US. Soc Sci Med. 2001;53:41–53. [DOI] [PubMed] [Google Scholar]
- 41. Allman RM, Baker PS, Maisiak RM, et al. Racial similarities and differences in predictors of mobility change over eighteen months. J Gen Intern Med. 2004;19:1118–1126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Studenski S, Perera S, Wallace D, et al. Physical performance measures in the clinical setting. J Am Geriatr Soc. 2003;51:314–322. [DOI] [PubMed] [Google Scholar]
- 43. Hajjar I, Kotchen TA. Trends in prevalence, awareness, treatment, and control of hypertension in the United States, 1988–2000. JAMA. 2003;290:199–206. [DOI] [PubMed] [Google Scholar]
- 44. Fongwa MN, Evangelista LS, Hays RD, et al. Adherence treatment factors in hypertensive African American women. Vasc Health Risk Manag. 2008;4:157–166. [DOI] [PMC free article] [PubMed] [Google Scholar]


