Abstract
Background:
In children, community-acquired pneumonia is a frequent cause of emergency department (ED) presentation and hospital admission. Quality primary care may prevent some of these hospital visits.
Aims:
The aim of this study was to identify primary care factors associated with ED presentation and hospital admission of preschool-aged children with community-acquired pneumonia.
Methods:
A case–control study was conducted by enrolling three groups: children presenting to the ED with pneumonia and admitted (n=326), or discharged home (n=179), and well-neighbourhood controls (n=351). Interviews with parents and primary care staff were conducted and health record review was performed. The association of primary care factors with ED presentation and hospital admission, controlling for available confounding factors, was determined using logistic regression.
Results:
Children were more likely to present to the ED with pneumonia if they did not have a usual general practitioner (GP) (odds ratio (OR)=2.50, 95% confidence interval (CI)=1.67–3.70), their GP worked ⩽20 h/week (OR=1.86, 95% CI=1.10–3.13) or their GP practice lacked an immunisation recall system (OR=5.44, 95% CI=2.26–13.09). Lower parent ratings for continuity (OR=1.63, 95% CI=1.01–2.62), communication (OR=2.01, 95% CI=1.29–3.14) and overall satisfaction (OR=2.16, 95% CI=1.34–3.47) increased the likelihood of ED presentation. Children were more likely to be admitted when antibiotics were prescribed in primary care (OR=2.50, 95% CI=1.43–4.55). Hospital admission was less likely if children did not have a usual GP (OR=0.22, 95% CI=0.11–0.40) or self-referred to the ED (OR=0.48, 95% CI=0.26–0.89).
Conclusions:
Accessible and continuous primary care is associated with a decreased likelihood of preschool-aged children with pneumonia presenting to the ED and an increased likelihood of hospital admission, implying more appropriate referral. Lower parental satisfaction is associated with an increased likelihood of ED presentation.
Introduction
Assessing the quality of primary care is complex, and it includes dimensions describing different aspects of care. Donabedian described quality of primary care in terms of (i) structure (organisational factors of care within the health care system); (ii) process (the delivery and receipt of care); and (iii) outcome (the consequences of care).1 Campbell reduced the quality dimensions to the domains of (i) access (structure and process) and (ii) effectiveness (outcome).2,3 Quality primary care is believed to improve the health of the community and to reduce avoidable hospital admissions.4,5
Primary care in New Zealand (NZ) underwent significant reform in 2001, with the introduction of the Primary Health Care Strategy.6 Three major organisational and policy changes occurred as a result of this reform. Primary Health Organisations (PHOs) were developed as local non-government agencies serving the health needs of an enrolled group of people. Doctors working in general practice became a part of PHOs, into which patients registered.7 Government funding of primary care was increased so that patient co-payments could decrease, and it was changed from a fee-for-service payment at the individual practitioner level to a capitated payment at the PHO level.8 More capitation was introduced into the primary care system.6 The aim was to improve health equity by decreasing financial and other access barriers, and, particularly, improving access to care for children was a focus.
The primary care received by a child in the community is a determinant of their health and, as such, contributes to the risk of them experiencing poor health from common childhood illnesses, such as pneumonia. Pneumonia is a common cause of both primary and secondary health care utilisation. Pneumonia, asthma, cellulitis, gastroenteritis and dehydration, seizures and some upper airway conditions represent the six ambulatory care–sensitive conditions specific to children.9
Hospitalisation rates for childhood pneumonia and bronchiolitis in NZ are two to three times higher than in England or the USA.10–14 New Zealand’s Primary Health Care Strategy was intended to reduce the burden of diseases such as pneumonia by improving the quality of primary care.15
Our objectives were to describe the quality of primary care received by preschool-aged NZ children and to determine the extent to which the well-child and acute primary care received was accessible, comprehensive and coordinated; promoted a continuous doctor–patient relationship; and was consistent with evidence-based guidelines.
We used this information to investigate the hypothesis that receiving high-quality primary care decreases the likelihood of children with pneumonia presenting to the ED, but it increases the likelihood of these children requiring inpatient hospital care.
Materials and methods
Study design and setting
Our study was completed within a larger case–control study of risk factors for pneumonia and hospitalisation with pneumonia.16 Three groups of children <5 years old, from central and west Auckland, were enrolled between August 2002 and December 2004: (i) those presenting to the Emergency Department (ED) with pneumonia and admitted to Starship Children’s Hospital; (ii) those diagnosed with pneumonia in the ED but not admitted; and (iii) those without pneumonia but living in the same urban areas as those with pneumonia. Each year, approximately 1,100 preschool-aged children present to the Starship Children’s Hospital ED with pneumonia, of whom approximately 500 (45%) are admitted.11
Primary care risk factors for ED presentation with pneumonia were identified by comparing all children with pneumonia (both admitted and ED-discharged cases) with community controls. Primary care risk factors for hospitalisation with pneumonia were determined by comparing children presenting to the ED with pneumonia and admitted to the hospital with children with pneumonia discharged home from the ED.
Ethical approval was granted by the Ministry of Health Auckland Regional Ethics Committee (application number AKY/02/00/135). Written informed consent was obtained from each child’s caregiver.
Participants
All children with pneumonia fulfilled the World Health Organisation pneumonia case definition of having an acute illness with cough or difficulty breathing plus indrawing or tachypnoea.17 The decision to admit a child presenting to the ED with pneumonia was made by doctors who were not involved in the research project. Indications for admission include any of the following: ill or toxic appearance; age <3 months; hypoxaemia (O2 saturation <93% on air); respiratory distress interfering significantly with feeding; significant dehydration; complicated pneumonia; deterioration despite appropriate oral antibiotics; significant comorbidity; and social concerns, for example, no car, no phone and presence of language or communication barrier.18
Community controls were a sample of ‘well’ children recruited from households that were identified using residential address start points, as described previously.16 Stratification of sampling by age and ethnicity was used to create a control group with a similar age and ethnic distribution to that anticipated for the children hospitalised with pneumonia.11,16 Controls were not individually matched to cases and were ineligible if they were diagnosed with pneumonia in the previous month.
Children were ineligible if they had acute asthma, congenital heart disease, chronic lung disease, neurological disease affecting respiratory function, immunodeficiency or acute aspiration of a foreign body or liquid. Children with a history of asthma were eligible.
Data sources/measurement
Three methods of data collection were used: (i) face-to-face interview with the child’s caregiver (all groups); (ii) review of the primary care practice and medical records (all groups); and (ii) review of the hospital medical records (hospitalised and ED-discharged pneumonia cases) (Supplementary Figure 1). Variables describing the primary care received by the child, including well-child care, immunisations, acute-illness care and the use of complementary health care providers; the demographics and medical history of the child and family; and the household composition and internal living environment were collected.
The General Practice Assessment Survey19 was used to assess caregiver satisfaction with their child’s primary care. Additional interview questions ascertained the caregiver’s primary care beliefs, health-seeking behaviour and utilisation of primary care with respect to their child (Supplementary Figure 1, Section A).
The primary care review determined the features of both the family and acute general practices via face-to-face interview with practice staff and a review of the practice medical records (Supplementary Figure 1, Section B). Primary care medical records were reviewed for the 2 months preceding the date of hospital admission or ED presentation for those with pneumonia and the consent date for community controls. The hospital medical records were reviewed for all children with pneumonia (Supplementary Figure 1, Section C). Linkage to both primary and secondary care health records was established using the National Health Index (NHI) number, a unique identifier assigned to every person having contact with health services in NZ.
Seasonal bias
The study was conducted over a 29-month period from August 2002 to December 2004. In Auckland, 80% of paediatric pneumonia hospitalisations occur from June to November.11 Owing to funding restrictions, it was not possible to recruit controls at the same rate as the pneumonia cases during these months. Therefore, seasonal differences in enrolment between those with pneumonia and community controls were controlled for in the multiple-variable logistic regression analyses.
Sample size and study power
Power calculations (for a non-clustered sample) assumed samples of 300 children in each of the three groups. This number could detect an OR of 2 for control exposures from 11% to 80% (power 80%, alpha-error 5%).20 We anticipated that clustering of community controls by residential address would result in some reduction in study power. For this reason, our recruitment strategy was designed to keep the size of the clusters small to reduce the size of this design effect.16
Quantitative variables
Separate multiple-variable models were created for the case–control analyses that determined risk factors for pneumonia and for hospitalisation with pneumonia. The potentially confounding variables were identified in a previous study.16 For the comparison of all children with pneumonia with the community controls, these variables were season of enrolment, year of admission, age, weight-for-height z-score, gender, ethnicity, household crowding, mold and mildew in the child’s bedroom, household deprivation score, previous chest infections and history of maternal pneumonia. For the comparison of children with pneumonia who were hospitalised versus those discharged from the ED, these variables were season of enrolment, year of admission, age, weight-for-height z-score, ethnicity, household crowding, household smoking, mold and mildew in the child’s bedroom, household deprivation score, previous chest infections and history of sibling and maternal pneumonia. Weight-for-height z-scores were calculated using World Health Organization Anthro v 2.0.4 software.21
Statistical methods
Analyses that included the community control group adjusted for the effect of stratification and clustering of the community control sample on the OR estimates. Chi-squared tests were used to test for univariate associations with the odds of pneumonia and hospitalisation with pneumonia. Multiple-variable logistic regression analysis was used to determine independent associations between the variables measured and the odds of ED presentation with pneumonia or hospital admission with pneumonia. Associations were described using ORs with 95% confidence intervals (CIs). Analyses were performed using SAS version 9.122 and SAS—callable Sudaan version 9.23
Results
Participants
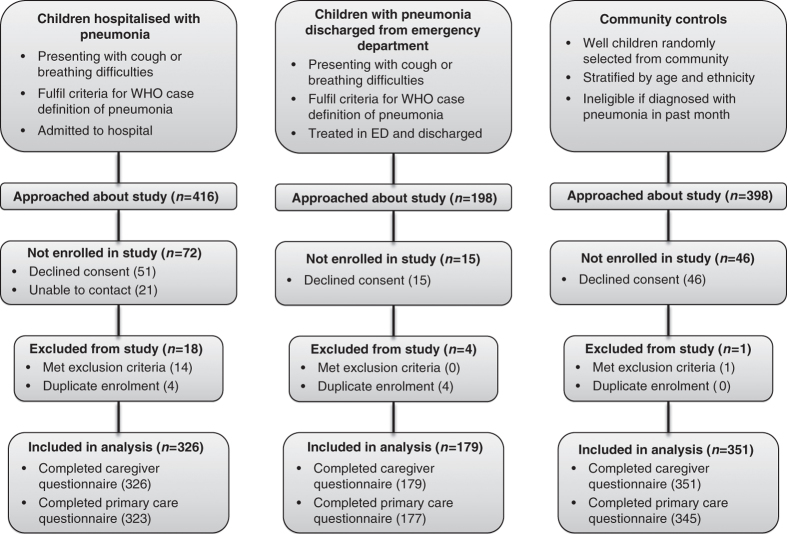
During the recruitment period, caregivers of 1,012 children were approached (Figure 1). Of the 133 children not enrolled in the study, 112 declined consent and 21 could not be contacted. A further 23 children met the exclusion criteria or were duplicate enrolments. Therefore, a total of 856 participants were included in the analysis (326 children hospitalised with pneumonia, 179 children with pneumonia discharged home from the ED and 351 community controls).
Figure 1.
Flow diagram describing the study design, participant enrolment and data collection. ED, Emergency Department; WHO, World Health Organization.
Child demographics
The demographics of children enrolled in the study have been described previously.16 Median (interquartile range) age was 19 (11–28) months and weight-for-height z-score was +0.5 (−0.3 to +1.3). Children admitted to the hospital with pneumonia were younger (OR=0.73, 95% CI=0.62–0.87) than those with pneumonia discharged from the ED. Children with pneumonia had lower weight-for-height z-scores compared with community controls (OR=0.88, 95% CI=0.79–0.9).
Primary care risk factors associated with presenting to hospital ED with pneumonia
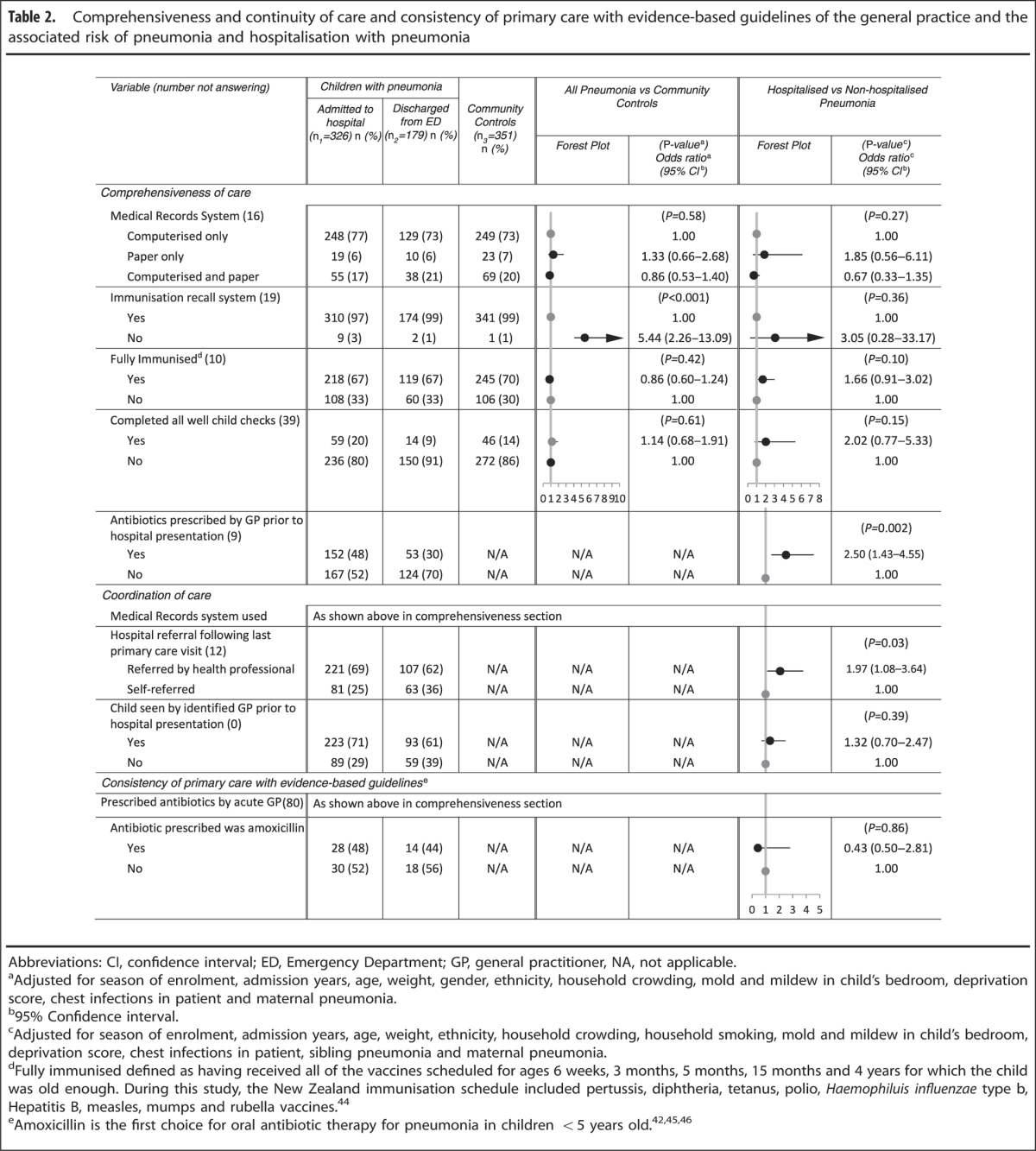
Objective measures of accessibility, continuity and comprehensiveness of primary care were associated with the likelihood of ED presentation with pneumonia. Children without a single, identified GP (OR=2.50, 95% CI=1.67–3.70) or whose GP worked part-time ⩽20 h/week (OR=1.86, 95% CI=1.10–3.13) rather than for >20 to <40 h or full time were more likely to present to the ED with pneumonia (Table 1). Having a general practice with no immunisation recall system also increased the likelihood of ED presentation with pneumonia (OR=5.44, 95% CI=2.26–13.09); however, only 2% of practices lacked an immunisation recall system (Table 2).
Table 1. Accessibility and continuity of care of the general practice and the associated risk of pneumonia and hospitalisation with pneumonia.
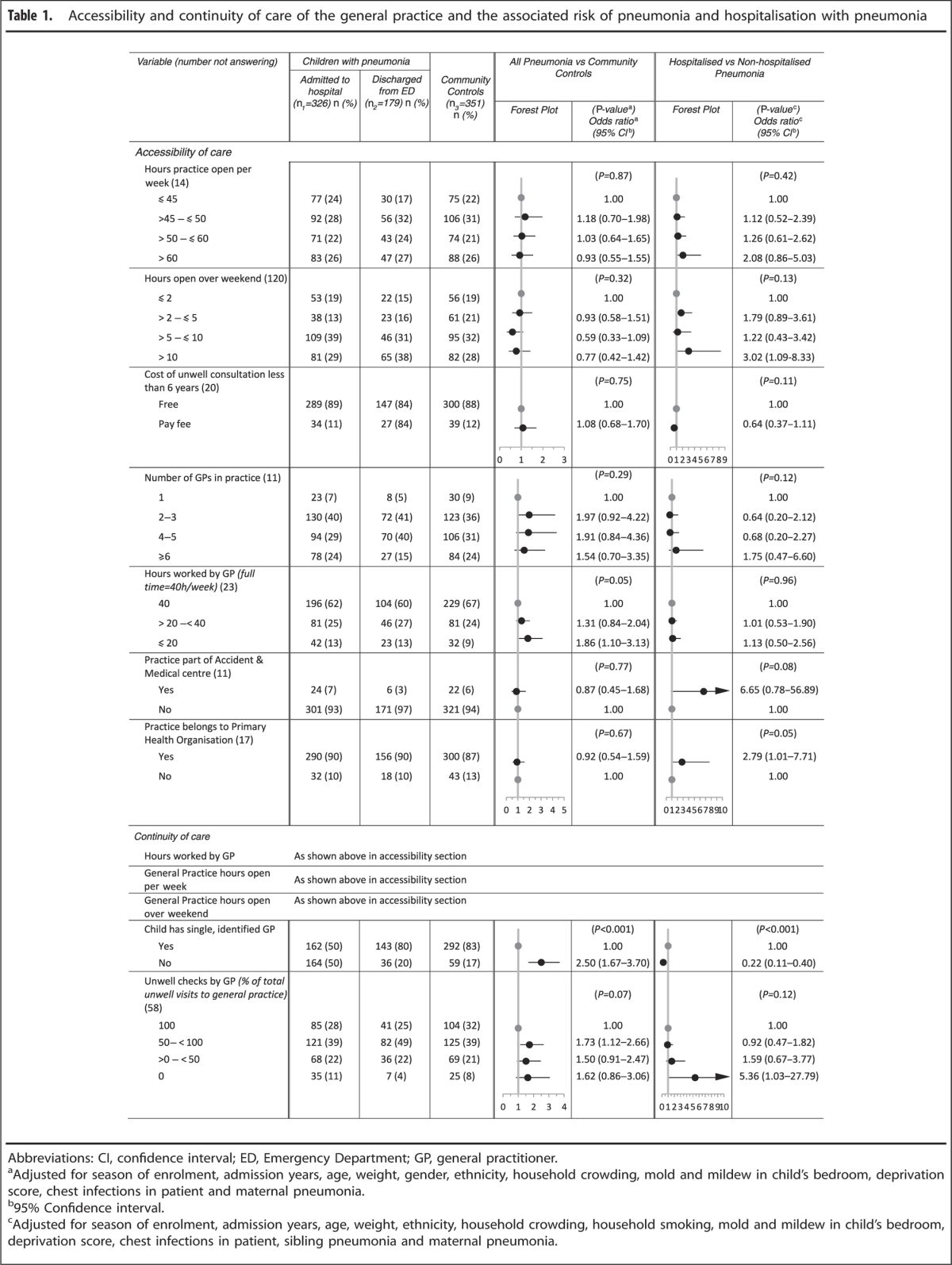
Table 2. Comprehensiveness and continuity of care and consistency of primary care with evidence-based guidelines of the general practice and the associated risk of pneumonia and hospitalisation with pneumonia.
The primary care beliefs and health-seeking behaviour of the caregiver were associated with a decreased likelihood of ED presentation with pneumonia (Supplementary Table 1). Children whose caregivers would take them back to the same doctor (OR=0.52, 95% CI=0.28–0.97) or to an after-hours accident and medical centre (OR=0.65, 95% CI=0.45–1.44) when still unwell with a cough and fever, following a visit to the GP on the previous day, were less likely to present to the ED with pneumonia.
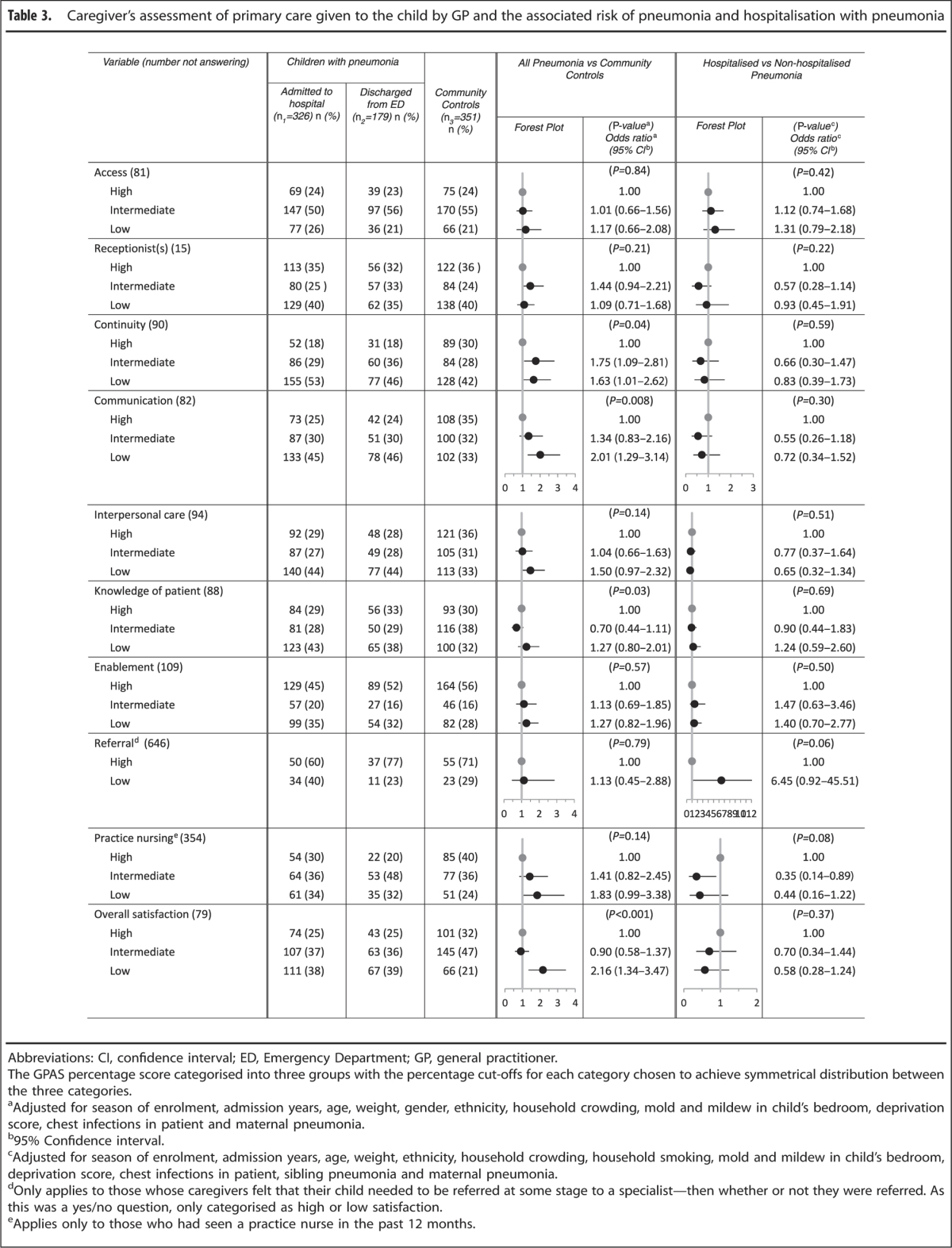
Subjective measures of caregiver satisfaction with the primary care received by the child were associated with the risk of ED presentation with pneumonia (Table 3). Lower scores for continuity of care (OR=1.63, 95% CI=1.01–2.62), communication between the caregiver and GP (OR=2.01, 95% CI=1.29–3.14) and overall caregiver satisfaction with care (OR=2.16, 95% CI=1.34–3.47) were associated with an increased likelihood of ED presentation with pneumonia.
Table 3. Caregiver’s assessment of primary care given to the child by GP and the associated risk of pneumonia and hospitalisation with pneumonia.
Primary care risk factors associated with hospitalisation with pneumonia after ED presentation
Objective measures of primary care accessibility, comprehensiveness, coordination, continuity and consistency with evidence-based guidelines were associated with the likelihood of admission with pneumonia (Tables 1 and 2). The likelihood of admission with pneumonia was increased when the child’s general practice belonged to a PHO (OR=2.79, 95% CI=1.01–7.71) and when antibiotics were prescribed by the GP before ED presentation (OR=2.50, 95% CI=1.43–4.55). In comparison with self-referral, referral that was by a health professional (OR= 1.97, 95% CI=1.08–3.64) was associated with an increased likelihood of admission with pneumonia. Children without a single, identified GP (OR=0.22, 95% CI=0.11–0.40) were less likely to be admitted with pneumonia.
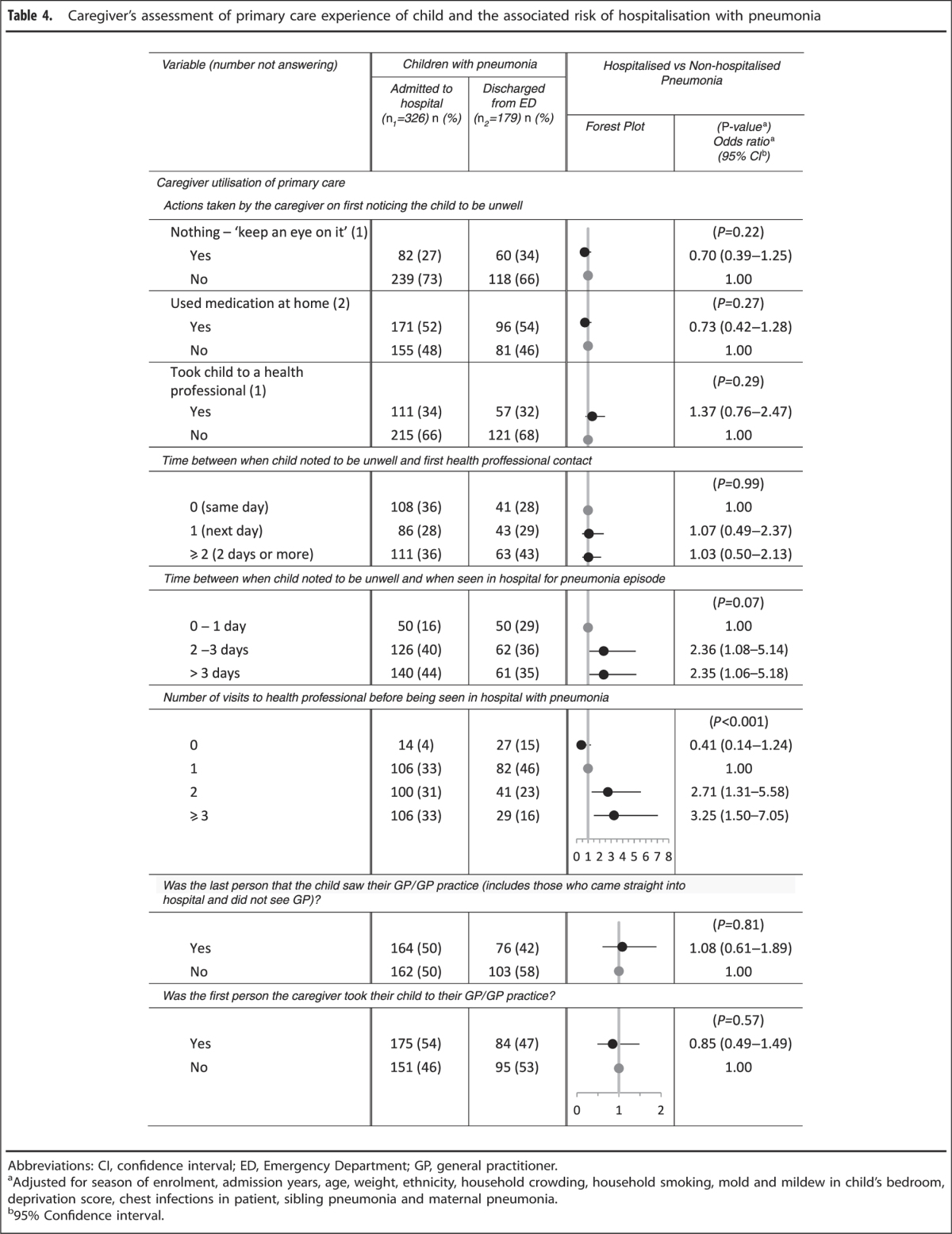
Aspects of caregiver utilisation of primary care during the child’s pneumonia illness episode increased the likelihood of hospital admission (Table 4). Children who had made more health professional visits before presentation (two visits, OR=2.71, 95% CI=1.31–5.58; three or more visits, OR=3.25, 95% CI=1.50–7.05) had an increased likelihood of admission with pneumonia. The small number of children whose caregivers would seek care from a complementary healer if their child was unwell with a cough or fever were less likely to be admitted with pneumonia (OR=0.08, 95% CI=0.01–0.41). Children whose caregivers would take them to a hospital ED if they had been seen the previous day by their GP and were still unwell were less likely to be admitted with pneumonia (OR=0.60, 95% CI=0.41–0.88).
Table 4. Caregiver’s assessment of primary care experience of child and the associated risk of hospitalisation with pneumonia.
No associations were evident between the measures of caregiver satisfaction with the primary care of the child by the GP and the likelihood of admission with pneumonia (Table 3).
Discussion
Main findings
In preschool-aged children, primary care that was less accessible (fewer hours worked by GP) or less continuous (fewer hours worked by GP and not having a single, identified GP) was associated with an increased likelihood of ED presentation with pneumonia. Among children with pneumonia presenting to the hospital ED, those whose primary care was more accessible (practice belonging to a PHO), more comprehensive (antibiotics prescribed before ED presentation), more coordinated (referral by health professional) and more continuous (having a single identified GP) were more likely to be admitted. The increased likelihood of hospital admission in this context implies a referral from primary care to the ED that was more appropriate.
Children whose caregivers would return to the same doctor if their child was unwell, or would take them to an after-hours practice, were less likely to present to the ED with pneumonia. Children making more health professional visits before ED presentation with pneumonia were more likely to be admitted. Those who, if unwell, would be taken to a hospital ED or complementary health provider were less likely to be admitted.
Patterns of ED presentation and then subsequent hospital admission were consistent with the concept that for some parents the hospital ED is used as an alternative to primary care, whereas for others, who perhaps had better access to primary care, hospital ED presentation was a clear step up in the level of care being sought. Those children who, if unwell, would be taken to a hospital ED or complementary health provider were less likely to be admitted. In contrast, children whose caregivers would return to the same doctor if their child was unwell or would take them to an after-hours practice were less likely to present to the ED with pneumonia, and children making more health professional visits before ED presentation with pneumonia were more likely to be admitted.
Caregiver satisfaction with primary care, which was lower specifically for continuity and communication and overall, was associated with an increased risk of ED presentation with pneumonia.
Strengths and limitations of this study
We obtained both objective and subjective measures of the quality of primary care and collected data from caregivers, primary care practices and the hospital. Statistical power was achieved, with 820 children recruited to the study. However, distribution between the three study groups was uneven, with 326 hospital-admitted pneumonia cases (40%), 179 ED-discharged pneumonia cases (22%) and 315 community controls (38%) recruited. It was an ethics committee requirement that children and their caregivers in the ED were initially approached by ED staff about the study. Study recruitment was therefore adversely affected by ED staff workloads, particularly during the winter months when more pneumonia cases are in the ED. To maintain study power, additional pneumonia cases and community controls were enrolled.
Budgetary constraints limiting the number of interviewers resulted in an inability to maintain a comparable rate of recruitment of community controls, particularly during winter and spring. Seasonal variation was controlled for in the analysis.
We used the World Health Organization pneumonia case definition, thus enabling generalisability of our study findings. Chest radiograph abnormalities were not included in our case definition owing to the acknowledged poor inter-observer agreement in defining which chest radiograph abnormalities are indicative of pneumonia and lack of a radiological definition of pneumonia that is both sensitive and specific.24 In Australian children, interpretation of chest radiographs using the World Health Organization definition of primary end-point pneumonia has been shown to have low sensitivity.25
Although the data were collected for this study in 2002–2004, the study findings remain relevant to the current situation in NZ. Infectious diseases remain the most frequent cause of acute hospital admission in NZ and have increased as a proportion of all hospital admissions over the past 20 years.26 Hospital admission rates of acute respiratory infections in NZ have continued to increase over the past 20 years, with these increases being most marked in preschool-aged children.26 The need for improved quality, accessibility and applicability of health care in NZ remains one of the main areas of health care reform focus. Our study findings are of particular relevance to the more recent health care reform initiatives, which seek to improve the integration of primary and secondary care in NZ.27
Interpretation of findings in relation to previously published work
Consultation costs are known to be an important barrier to accessing primary health care, adversely affecting patient utilisation, especially those of lower socioeconomic status.2,28–32 However, consultation cost was not associated with the likelihood of ED presentation or hospital admission with pneumonia in the present study. In NZ, primary care consultation is free for most children <6 years old.33,34 It is possible, therefore, that the financial barriers impeding caregivers’ access for their child to the GP have been reduced to such a level that this is no longer an obstacle in the preschool age group.
Children whose primary care was less accessible or less continuous were more likely to present to the ED with pneumonia. In England, the emergency admission rate for children has increased by 28% from 1999 to 2010, with much of this increase being for acute respiratory infections.35 These increases are explained entirely by an increase in the number of hospital admissions of <1 day’s duration. These increases in England have been attributed to changes in the provision of both primary care (dividing in-hours and out-of-hours care) and secondary care (reduction in patient time in ED).35 A similar division between in-hours and after-hours primary care provision has been present in NZ for a longer time.36 Our findings suggest that the evolution of primary care in this direction, with the resultant decrease in quality of care, is likely to contribute both to the higher hospital admission rates for pneumonia in NZ compared with other developed countries and the large increases in hospital admission rates for serious infections that have occurred in NZ over the past two decades.26,37 The fact that the children in our study who presented to the ED with pneumonia were more likely to be admitted to hospital if their primary care was more accessible, comprehensive and coordinated indicates that such higher quality primary care reduces unnecessary presentations to the hospital ED.
Consistent with the present study findings, the doctor–patient relationship has been shown to be important for the effective primary care management of acute illness in children in NZ.38–40 A qualitative study of the families of Pacific children admitted with pneumonia, the NZ ethnic group with the highest childhood pneumonia admission rates,11 showed that mistrust, resulting in fragmentation of care rather than delayed presentation to care, was the primary reason cited for presentation to the hospital ED.38 Poor satisfaction with the primary care doctor–patient relationship may adversely affect several aspects of primary care quality—for example, continuity of care and self-referral—because the patient will be more likely to either not attend their GP or to seek advice from a different GP.41
Children presenting at the hospital with a GP referral letter or already taking antibiotics were at an increased likelihood of hospital admission with pneumonia. These findings are expected, as a lack of response to oral antibiotics would, in itself, also be an indication for referral to hospital.42 In a similar manner, self-referral may be indicative of a more rapidly progressing illness and hence one where primary care has less opportunity to influence the need for hospital admission.43
Implications for future research, policy and practice
The 2001 Primary Health Care Strategy goal of improving health equity in NZ by decreasing financial and other access barriers appears to have been achieved.6 However, a deeper understanding of the doctor–patient relationship, particularly as it relates to the different ethnicities and socioeconomic groups present in NZ, is required to adequately inform policy around removing barriers to, and improving the quality of, primary health care, and thus effectively managing the use of expensive hospital resources.
Conclusions
In preschool-aged children with pneumonia, primary care that is more accessible and more continuous is associated with a decreased likelihood of ED presentation and hospital admission. Primary care that is more accessible and comprehensive is associated with more appropriate use of ED resources, as demonstrated by a greater likelihood that ED presentation will lead to hospital admission. Lower parental satisfaction with primary care, specifically with continuity and communication, is associated with an increased likelihood of preschool-aged children with pneumonia presenting to the ED.
Acknowledgments
The authors thank the children and parents who participated in this study, as well as the staff of the Emergency Department and inpatient wards of Starship Children’s Hospital and at all of the participating primary care practices.
The authors declare no conflict of interest.
References
- Donabedian A. Evaluating the quality of medical care. Milbank Mem Fund Q. 1966;44:166–206. [PubMed] [Google Scholar]
- Campbell SM, Roland MO, Buetow SA. Defining quality of care. Soc Sci Med. 2000;51:1611–1625. doi: 10.1016/s0277-9536(00)00057-5. [DOI] [PubMed] [Google Scholar]
- Stewart AL, Grumbach K, Osmond DH, Vranizan K, Komaromy M, Bindman AB. Primary care and patient perceptions of access to care. J Fam Pract. 1997;44:177–185. [PubMed] [Google Scholar]
- Parchman ML, Culler S. Primary care physicians and avoidable hospitalizations. J Fam Pract. 1994;39:123–128. [PubMed] [Google Scholar]
- Starfield B, Shi L, Macinko J. Contribution of primary care to health systems and health. Milbank Q. 2005;83:457–502. doi: 10.1111/j.1468-0009.2005.00409.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ministry of Health . The Primary Health Care Strategy. Ministry of Health: Wellington, New Zealand; 2001. [Google Scholar]
- Ministry of Health . A Guide for Establishing Primary Health Organisations. Ministry of Health: Wellington, New Zealand; 1999. [Google Scholar]
- Cumming J, Raymont A, Gribben B, Horsburgh M, Kent B, McDonald J. Evaluation of the Implementation and Intermediate Outcomes of the Primary Health Care Strategy. Victoria University of Wellington: Wellington, New Zealand; 2005. [Google Scholar]
- Parker JD, Schoendorf KC. Variation in hospital discharges for ambulatory care-sensitive conditions among children. Pediatrics. 2000;106 (4 Suppl):942–948. [PubMed] [Google Scholar]
- Cheung CR, Smith H, Thurland K, Duncan H, Semple MG. Population variation in admission rates and duration of inpatient stay for bronchiolitis in England. Arch Dis Child. 2013;98:57–59. doi: 10.1136/archdischild-2012-302277. [DOI] [PubMed] [Google Scholar]
- Grant CC, Scragg R, Tan D, Pati A, Aickin R, Yee RL. Hospitalization for pneumonia in children in Auckland, New Zealand. J Paediatr Child Health. 1998;34:355–359. doi: 10.1046/j.1440-1754.1998.00237.x. [DOI] [PubMed] [Google Scholar]
- Craig E, Adams J, Oben G, Reddington A, Wicken A, Simpson J. The Health Status of Children and Young People in New Zealand. University of Otago: Dunedin, New Zealand; 2013. [Google Scholar]
- Hasegawa K, Tsugawa Y, Brown DF, Mansbach JM, Camargo CA., Jr Trends in bronchiolitis hospitalizations in the United States, 2000–2009. Pediatrics. 2013;132:28–36. doi: 10.1542/peds.2012-3877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Griffin MR, Zhu Y, Moore MR, Whitney CG, Grijalva CG. U.S. hospitalizations for pneumonia after a decade of pneumococcal vaccination. N Engl J Med. 2013;369:155–163. doi: 10.1056/NEJMoa1209165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vogel AM, Trenholme AA, Stewart JM, Best E, McBride C, Lennon DR. Impact of pneumococcal vaccine on hospital admission with lower respiratory infection in children resident in South Auckland, New Zealand. N Z Med J. 2013;126:26–35. [PubMed] [Google Scholar]
- Grant CC, Emery D, Milne T, Coster G, Forrest CB, Wall CR. Risk factors for community-acquired pneumonia in pre-school-aged children. J Paediatr Child Health. 2012;48:402–412. doi: 10.1111/j.1440-1754.2011.02244.x. [DOI] [PubMed] [Google Scholar]
- World Health Organization . Technical Bases for the WHO Recommendations on the Management of Pneumonia in Children at First-Level Health Facilities. World Health Organization: Geneva, Switzerland; 1991. [Google Scholar]
- Best E, Brabyn C, Grant CC, Shepherd M, Twiss J . Pneumonia acute in infants and chlidren Auckland: Starship Children’s Health; 2010. Available from http://www.adhb.govt.nz/starshipclinicalguidelines/Pneumonia.htm . Accessed 30 November 2014.
- National Primary Care Research and Development Centre . General Practice Assessment Survey (GPAS) Manual. University of Manchester: Manchester, UK; 1999. [Google Scholar]
- Dean AG, Arner TG, Sangam S, Sunki GG, Friedman R, Lantinga M. Epi Info 2000, a Database and Statistics Program for Public Health Professionals for use on Windows 95, 98, NT, and 2000 Computers. Centers for Disease Control and Prevention: Atlanta, GA, USA; 2000. [Google Scholar]
- de Onis M, Garza C, Victora CG, Onyango AW, Frongillo EA, Martines J. The WHO Multicentre Growth Reference Study: planning, study design, and methodology. Food Nutr Bull. 2004;25:S15–S26. doi: 10.1177/15648265040251S103. [DOI] [PubMed] [Google Scholar]
- SAS Institute Incorporated. SAS
- Research Triangle Institute . SAS-Callable SUDAAN Version 9.0.1. Research Triangle Institute: Research Triangle Park, NC, USA; 2005. [Google Scholar]
- Johnson J, Kline JA. Intraobserver and interobserver agreement of the interpretation of pediatric chest radiographs. Emerg Radiol. 2010;17:285–290. doi: 10.1007/s10140-009-0854-2. [DOI] [PubMed] [Google Scholar]
- O’Grady KA, Torzillo PJ, Ruben AR, Taylor-Thomson D, Valery PC, Chang AB. Identification of radiological alveolar pneumonia in children with high rates of hospitalized respiratory infections: comparison of WHO-defined and pediatric pulmonologist diagnosis in the clinical context. Pediatr Pulmonol. 2012;47:386–392. doi: 10.1002/ppul.21551. [DOI] [PubMed] [Google Scholar]
- Baker MG, Barnard LT, Kvalsvig A, Verrall A, Zhang J, Keall M. Increasing incidence of serious infectious diseases and inequalities in New Zealand: a national epidemiological study. Lancet. 2012;379:1112–1119. doi: 10.1016/S0140-6736(11)61780-7. [DOI] [PubMed] [Google Scholar]
- Ministry of Health . Better, Sooner, More Convenient Health Care in the Community. Ministry of Health: Wellington, New Zealand; 2011. [Google Scholar]
- Robinson T. The cost to the New Zealand Government of providing 'free' primary medical care: an estimate based upon the Rand Health Insurance Experiment. N Z Med J. 2003;116:U419. [PubMed] [Google Scholar]
- Clarkson JE, Lafferty ARA. Changing access to primary health care for children in Otago 1980-1983. NZ Fam Physician. 1984;11:172–175. [Google Scholar]
- Woodward A, Kawachi I. Why reduce health inequalities? J Epidemiol Community Health. 2000;54:923–929. doi: 10.1136/jech.54.12.923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brook RH, Ware JE, Jr, Rogers WH, Keeler EB, Davies AR, Donald CA. Does free care improve adults' health? Results from a randomized controlled trial. N Engl J Med. 1983;309:1426–1434. doi: 10.1056/NEJM198312083092305. [DOI] [PubMed] [Google Scholar]
- Starfield B. Primary Care: Comcept, Evolution, and Policy. Oxford University Press: New York, NY, USA; 1992. [Google Scholar]
- Ministry of Health . Reducing Inequalities in Health. Ministry of Health: Wellington, New Zealand; 2002. [Google Scholar]
- Easton B. The New Zealand health reforms of the 1990s in context. Appl Health Econ Health Policy. 2002;1:107–112. [PubMed] [Google Scholar]
- Gill PJ, Goldacre MJ, Mant D, Heneghan C, Thomson A, Seagroatt V. Increase in emergency admissions to hospital for children aged under 15 in England, 1999-2010: national database analysis. Arch Dis Child. 2013;98:328–334. doi: 10.1136/archdischild-2012-302383. [DOI] [PubMed] [Google Scholar]
- Murdoch C. Not being there. NZ Fam Physician. 2002;29:74–77. [Google Scholar]
- Grant CC, Wall CR, Gibbons MJ, Morton SM, Santosham M, Black RE. Child nutrition and lower respiratory tract disease burden in New Zealand: a global context for a national perspective. J Paediatr Child Health. 2011;47:497–504. doi: 10.1111/j.1440-1754.2010.01868.x. [DOI] [PubMed] [Google Scholar]
- Young N. The pre-hospital experiences of Samoan families in New Zealand who have had a child admitted to hospital with pneumonia: a qualitative exploratory study. Pacific Health Dialog. 2001;8:20–28. [PubMed] [Google Scholar]
- Mitchell EA. Racial inequalities in childhood asthma. Soc Sci Med. 1991;32:831–836. doi: 10.1016/0277-9536(91)90309-z. [DOI] [PubMed] [Google Scholar]
- Gribben B. Satisfaction with access to general practitioner services in south Auckland. N Z Med J. 1993;106:360–362. [PubMed] [Google Scholar]
- Murray J, Corney R. Not a medical problem? An intensive study of the attitudes and illness behaviour of low attenders with psychosocial difficulties. Social Psychiatry Psychiatr Epidemiol. 1990;25:159–164. doi: 10.1007/BF00782746. [DOI] [PubMed] [Google Scholar]
- Bradley JS, Byington CL, Shah SS, Alverson B, Carter ER, Harrison C. The management of community-acquired pneumonia in infants and children older than 3 months of age: clinical practice guidelines by the Pediatric Infectious Diseases Society and the Infectious Diseases Society of America. Clin Infect Dis. 2011;53:e25–e76. doi: 10.1093/cid/cir531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant CC, Harnden A, Mant D, Emery D, Coster G. Why do children hospitalised with pneumonia not receive antibiotics in primary care? Arch Dis Child. 2012;97:21–27. doi: 10.1136/archdischild-2011-300604. [DOI] [PubMed] [Google Scholar]
- Ministry of Health . Immunisation Handbook 2006. Ministry of Health: Wellington, New Zealand; 2006. [Google Scholar]
- Grant CC, Ingram RJ. Outpatient treatment of pneumonia. N Z Med J. 2000;113:58–62. [PubMed] [Google Scholar]
- T British BTS Guidelines for the Management of Community Acquired Pneumonia in Childhood. Thorax. 2002;57 (Suppl 1):i1–i24. doi: 10.1136/thorax.57.90001.i1. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.