Assessment of burn area
Assessment of burn area tends to be done badly, even by those who are expert at it. There are three commonly used methods of estimating burn area, and each has a role in different scenarios. When calculating burn area, erythema should not be included. This may take a few hours to fade, so some overestimation is inevitable if the burn is estimated acutely.
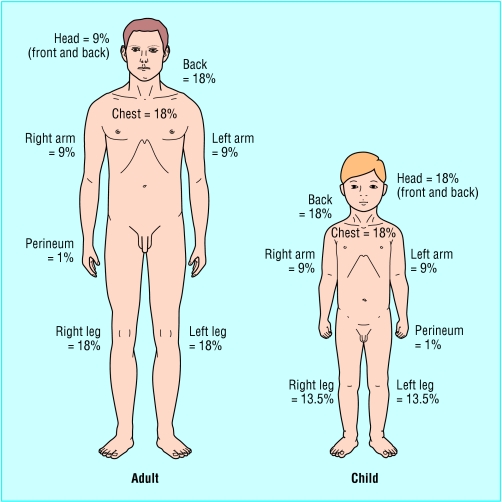
Figure 1.
Wallace rule of nines
Palmar surface—The surface area of a patient's palm (including fingers) is roughly 0.8% of total body surface area. Palmar surface are can be used to estimate relatively small burns (< 15% of total surface area) or very large burns (> 85%, when unburnt skin is counted). For medium sized burns, it is inaccurate.
Wallace rule of nines—This is a good, quick way of estimating medium to large burns in adults. The body is divided into areas of 9%, and the total burn area can be calculated. It is not accurate in children.
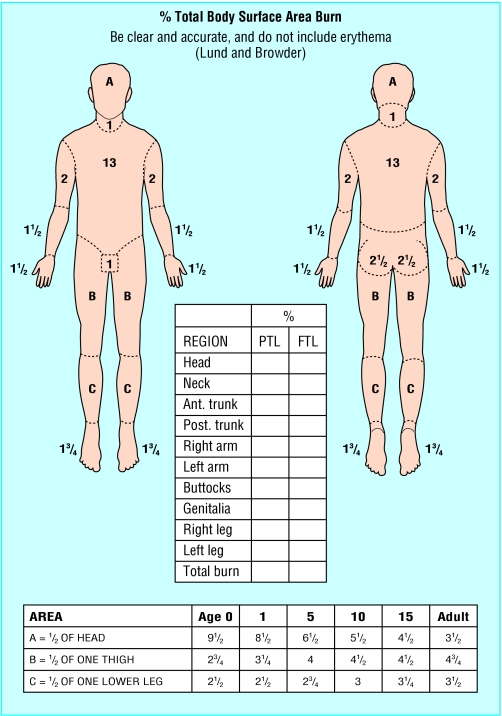
Lund and Browder chart—This chart, if used correctly, is the most accurate method. It compensates for the variation in body shape with age and therefore can give an accurate assessment of burns area in children.
It is important that all of the burn is exposed and assessed. During assessment, the environment should be kept warm, and small segments of skin exposed sequentially to reduce heat loss. Pigmented skin can be difficult to assess, and in such cases it may be necessary to remove all the loose epidermal layers to calculate burn size.
Resuscitation regimens
Fluid losses from the injury must be replaced to maintain homoeostasis. There is no ideal resuscitation regimen, and many are in use. All the fluid formulas are only guidelines, and their success relies on adjusting the amount of resuscitation fluid against monitored physiological parameters. The main aim of resuscitation is to maintain tissue perfusion to the zone of stasis and so prevent the burn deepening. This is not easy, as too little fluid will cause hypoperfusion whereas too much will lead to oedema that will cause tissue hypoxia.
The greatest amount of fluid loss in burn patients is in the first 24 hours after injury. For the first eight to 12 hours, there is a general shift of fluid from the intravascular to interstitial fluid compartments. This means that any fluid given during this time will rapidly leave the intravascular compartment. Colloids have no advantage over crystalloids in maintaining circulatory volume. Fast fluid boluses probably have little benefit, as a rapid rise in intravascular hydrostatic pressure will just drive more fluid out of the circulation. However, much protein is lost through the burn wound, so there is a need to replace this oncotic loss. Some resuscitation regimens introduce colloid after the first eight hours, when the loss of fluid from the intravascular space is decreasing.
Figure 2.
Lund and Browder chart
Burns covering more than 15% of total body surface area in adults and more than 10% in children warrant formal resuscitation. Again these are guidelines, and experienced staff can exercise some discretion either way. The most commonly used resuscitation formula is the Parkland formula, a pure crystalloid formula. It has the advantage of being easy to calculate and the rate is titrated against urine output. This calculates the amount of fluid required in the first 24 hours. Children require maintenance fluid in addition to this. The starting point for resuscitation is the time of injury, not the time of admission. Any fluid already given should be deducted from the calculated requirement.
At the end of 24 hours, colloid infusion is begun at a rate of 0.5 ml×(total burn surface area (%))×(body weight (kg)), and maintenance crystalloid (usually dextrose-saline) is continued at a rate of 1.5 ml×(burn area)×(body weight). The end point to aim for is a urine output of 0.5-1.0 ml/kg/hour in adults and 1.0-1.5 ml/kg/hour in children.
Table 1.
Parkland formula for burns resuscitation
| Total fluid requirement in 24 hours = |
| 4 ml×(total burn surface area (%)) × (body weight (kg)) |
| 50% given in first 8 hours |
| 50% given in next 16 hours |
| Children receive maintenance fluid in addition, at hourly rate of |
| 4 ml/kg for first 10 kg of body weight plus |
| 2 ml/kg for second 10 kg of body weight plus |
| 1 ml/kg for > 20 kg of body weight |
| End point |
| Urine output of 0.5-1.0 ml/kg/hour in adults |
| Urine output of 1.0-1.5 ml/kg/hour in children |
High tension electrical injuries require substantially more fluid (up to 9 ml×(burn area)×(body weight) in the first 24 hours) and a higher urine output (1.5-2 ml/kg/hour). Inhalational injuries also require more fluid.
Table 2.
Worked examples of burns resuscitation
| Fluid resuscitation regimen for an adult |
| A 25 year old man weighing 70 kg with a 30% flame burn was admitted at 4 pm. His burn occurred at 3 pm. |
| 1) Total fluid requirement for first 24 hours |
| 4 ml×(30% total burn surface area)×(70 kg) = 8400 ml in 24 hours |
| 2) Half to be given in first 8 hours, half over the next 16 hours |
| Will receive 4200 ml during 0-8 hours and 4200 ml during 8-24 hours |
| 3) Subtract any fluid already received from amount required for first 8 hours |
| Has already received 1000 ml from emergency services, and so needs further 3200 ml in first 8 hours after injury |
| 4) Calculate hourly infusion rate for first 8 hours |
| Divide amount of fluid calculated in (3) by time left until it is 8 hours after burn |
| Burn occurred at 3 pm, so 8 hour point is 11 pm. It is now 4 pm, so need 3200 ml over next 7 hours: |
| 3200/7 = 457 ml/hour from 4 pm to 11 pm |
| 5) Calculate hourly infusion rate for next 16 hours |
| Divide figure in (2) by 16 to give fluid infusion rate |
| Needs 4200 ml over 16 hours: |
| 4200/16 = 262.5 ml/hour from 11 pm to 3 pm next day |
| Maintenance fluid required for a child |
| A 24 kg child with a resuscitation burn will need the following maintenance fluid: |
| 4 ml/kg/hour for first 10 kg of weight = 40 ml/hour plus |
| 2 ml/kg/hour for next 10 kg of weight = 20 ml/hour plus |
| 1 ml/kg/hour for next 4 kg of weight = 1×4 kg = 4 ml/hour |
| Total = 64 ml/hour |
In Britain Hartman's solution (sodium chloride 0.6%, sodium lactate 0.25%, potassium chloride 0.04%, calcium chloride 0.027%) is the most commonly used crystalloid. Colloid use is controversial: some units introduce colloid after eight hours, as the capillary leak begins to shut down, whereas others wait until 24 hours. Fresh frozen plasma is often used in children, and albumin or synthetic high molecular weight starches are used in adults.
The above regimens are merely guidelines to the probable amount of fluid required. This should be continuously adjusted according to urine output and other physiological parameters (pulse, blood pressure, and respiratory rate). Investigations at intervals of four to six hours are mandatory for monitoring a patient's resuscitation status. These include packed cell volume, plasma sodium, base excess, and lactate.
Burns units use different resuscitation formulas, and it is best to contact the local unit for advice.
Escharotomies
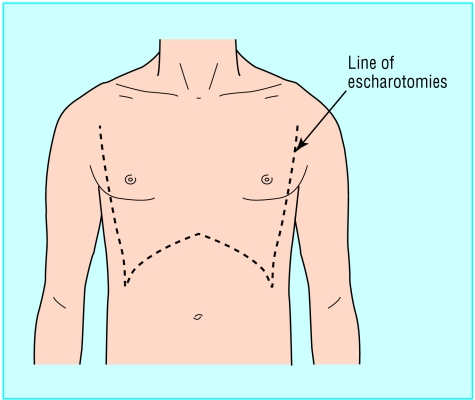
A circumferential deep dermal or full thickness burn is inelastic and on an extremity will not stretch. Fluid resuscitation leads to the development of burn wound oedema and swelling of the tissue beneath this inelastic burnt tissue. Tissue pressures rise and can impair peripheral circulation. Circumferential chest burns can also cause problems by limiting chest excursion and impairing ventilation. Both of these situations require escharotomy, division of the burn eschar. Only the burnt tissue is divided, not any underlying fascia, differentiating this procedure from a fasciotomy.
Incisions are made along the midlateral or medial aspects of the limbs, avoiding any underlying structures. For the chest, longitudinal incisions are made down each mid-axillary line to the subcostal region. The lines are joined up by a chevron incision running parallel to the subcostal margin. This creates a mobile breastplate that moves with ventilation. Escharotomies are best done with electrocautery, as they tend to bleed. They are then packed with Kaltostat alginate dressing and dressed with the burn.
Figure 3.

Escharotomy in a leg with a circumferential deep dermal burn
Although they are an urgent procedure, escharotomies are best done in an operating theatre by experienced staff. They should be discussed with the local burns unit, and performed under instruction only when transfer is delayed by several hours. Initially, at risk limbs should be elevated and observed.
Figure 4.
Diagram of escharotomies for the chest
Assessment of burn depth
The depth of burn is related to the amount of energy delivered in the injury and to the relative thickness of the skin (the dermis is thinner in very young and very old people).
Classification of burn depths
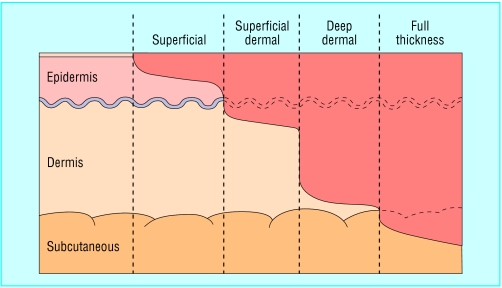
Burns are classified into two groups by the amount of skin loss. Partial thickness burns do not extend through all skin layers, whereas full thickness burns extend through all skin layers into the subcutaneous tissues. Partial thickness burns can be further divided into superficial, superficial dermal, and deep dermal:
Figure 5.
Diagram of the different burn depths
Superficial—The burn affects the epidermis but not the dermis (such as sunburn). It is often called an epidermal burn
Superficial dermal—The burn extends through the epidermis into the upper layers of the dermis and is associated with blistering
Deep dermal—The burn extends through the epidermis into the deeper layers of the dermis but not through the entire dermis.
Estimation of burn depth
Assessing burn depth can be difficult. The patient's history will give clues to the expected depth: a flash burn is likely to be superficial, whereas a burn from a flame that was not rapidly extinguished will probably be deep. On direct examination, there are four elements that should be assessed—bleeding on needle prick, sensation, appearance, and blanching to pressure.
Figure 6.
Full thickness burn in a black patient. In a white patient with extensive burns, such full thickness burns can easily be mistaken for unburnt skin
Bleeding—Test bleeding with a 21 gauge needle. Brisk bleeding on superficial pricking indicates the burn is superficial or superficial dermal. Delayed bleeding on a deeper prick suggests a deep dermal burn, while no bleeding suggests a full thickness burn.
Sensation—Test sensation with a needle also. Pain equates with a superficial or superficial dermal burn, non-painful sensation equates with deep dermal injury, while full thickness injuries are insensate. However, this test is often inaccurate as oedema also blunts sensation.
Appearance and blanching—Assessing burn depth by appearance is often difficult as burns may be covered with soot or dirt. Blisters should be de-roofed to assess the base. Capillary refill should be assessed by pressing with a sterile cotton bud (such as a bacteriology swab).
Table 3.
Assessment of burn depth
|
Burn type
|
||||
|---|---|---|---|---|
| Superficial | Superficial dermal | Deep dermal | Full thickness | |
| Bleeding on pin prick | Brisk | Brisk | Delayed | None |
| Sensation | Painful | Painful | Dull | None |
| Appearance | Red, glistening | Dry, whiter | Cherry red | Dry, white, leathery |
| Blanching to pressure | Yes, brisk return | Yes, slow return | No | No |
A red, moist wound that obviously blanches and then rapidly refills is superficial
A pale, dry but blanching wound that regains its colour slowly is superficial dermal
Deep dermal injuries have a mottled cherry red colour that does not blanch (fixed capillary staining). The blood is fixed within damaged capillaries in the deep dermal plexus
A dry, leathery or waxy, hard wound that does not blanch is full thickness. With extensive burns, full thickness burns can often be mistaken for unburnt skin in appearance.
Table 4.
Key points
| • Accurate assessment of burn area is crucial to calculate resuscitation formula |
| • Resuscitation formulas are only guidelines—monitor the patient |
| • Discuss resuscitation with a burns unit |
| • Be aware of the need for escharotomies |
| • Burn depth is difficult to estimate and changes with resuscitation |
Most burns are a mixture of different depths. Assessment of depth is important for planning treatment, as more superficial burns tend to heal spontaneously whereas deeper burns need surgical intervention, but is not necessary for calculating resuscitation formulas. Therefore, in acute situations lengthy depth assessment is inappropriate. A burn is a dynamic wound, and its depth will change depending on the effectiveness of resuscitation. Initial estimates need to be reviewed later.
Shehan Hettiaratchy is specialist registrar in plastic and reconstructive surgery, Pan-Thames Training Scheme, London; Remo Papini is consultant and clinical lead in burns,West Midlands Regional Burn Unit, Selly Oak University Hospital, Birmingham.
The ABC of burns is edited by Shehan Hettiaratchy; Remo Papini; and Peter Dziewulski, consultant burns and plastic surgeon, St Andrews Centre for Plastic Surgery and Burns, Broomfield Hospital, Chelmsford. The series will be published as a book in the autumn.
Competing interests: RP has been reimbursed by Johnson & Johnson, manufacturer of Integra, and Smith & Nephew, manufacturer of Acticoat and TransCyte, for attending symposiums on burn care.
Further reading and resources
- • Clarke J. Burns. Br Med Bull 1999;55: 885-94 [DOI] [PubMed] [Google Scholar]
- • Herndon D. Total burn care. 2nd ed. London: WB Saunders, 2002
- • Kao CC, Garner WL. Acute burns. Plast Reconstr Surg 2000;105: 2482-93 [PubMed] [Google Scholar]
- • Yowler CJ, Fratianne RB. The current status of burn resuscitation. Clin Plast Surg 2000;1: 1-9 [PubMed] [Google Scholar]
- • Collis N, Smith G, Fenton OM. Accuracy of burn size estimation and subsequent fluid resuscitation prior to arrival at the Yorkshire Regional Burns Unit. A three year retrospective study. Burns 1999;25: 345-51 [DOI] [PubMed] [Google Scholar]
- • Burnsurgery.org (see www.burnsurgery.org)