Abstract
Condomless sex is a key driver of sexually transmitted diseases. In this study, we assess the long-term changes (2000–2013) of the occurrence of condomless sex among human immunodeficiency virus (HIV)-infected individuals enrolled in the Swiss HIV Cohort study. The frequencies with which HIV-infected individuals reported condomless sex were either stable or only weakly increasing for 2000–2008. For 2008–2013, these rates increased significantly for stable relationships among heterosexuals and men who have sex with men (MSM) and for occasional relationships among MSM. Our results highlight the increasing public health challenge posed by condomless sex and show that condomless sex has been increasing even in the most recent years.
Keywords: condomless sex, HIV transmission, STI prevention, STI transmission
Antiretroviral therapy (ART) has dramatically reduced mortality and has also been shown to block human immunodeficiency virus (HIV) transmission from individuals on ART [1]. According to the statement from the Swiss Federal Commission on HIV/acquired immune deficiency syndrome in 2008, persons on ART with undetectable virus load and no other sexually transmitted infections (STIs) can have condomless sex in a stable relationship without risking the infection of their partner (“Swiss statement”) [2]. This was also one of the first worldwide recommendations based on the now accepted effect of treatment as prevention [3]. Accordingly, it has been suggested that this recommendation would lead to an increase in condomless sex [4]. Such an increase was indeed found in a previous publication from the Swiss HIV Cohort Study (SHCS) [5]. However, this analysis was limited to the years 2007–2009 because of administrative censoring in 2009 and because one of its main aims was to identify determinants of condomless sex (many of which were not measured in the SHCS before 2007).
In this study, we aim to complement the analysis from Hasse et al [5] by reporting the temporal changes of condomless sex for the entire time range from 2000 (start of systematic reporting of risk behavior) to 2013. This allowed us to address whether risk behavior was already increasing before 2008 and whether it kept increasing in recent years.
METHODS
The SHCS enrolls HIV-infected adults and has been approved by ethics committees of all participating institutions. Written informed consent for all participants was obtained.
Because this study aims to determine the level of condomless sex in the entire HIV-infected population captured by the SHCS, individuals were included in the analysis independently of their time of recruitment. In accordance with Hasse et al [5], we distinguish between sex with occasional and stable partners. For simplicity, but in contrast to Hasse et al [5], we consider only 2 transmission groups: heterosexuals and men who have sex with men [MSM]. In the analysis presented, we do not distinguish between male and female heterosexuals; in a sensitivity analysis, we found the same time trends for both sexes (results not shown). Individuals can contribute to the analysis with several follow-up visits. In each of the biannual follow-up visits, individuals were asked by a physician or a study-nurse if in the preceding 6 months (a) they had occasional partners, (b) they had sex with an occasional partner, and (c) how often they used condoms. If a and b were affirmed and c was not answered with “always”, this indicates condomless sex with an occasional partner for the corresponding time period. The analogous definition is used for condomless sex with a stable partner.
We use logistic regression models with calendar time as an explanatory variable to explain the temporal changes of condomless sex. In contrast to Hasse et al [5], we do not aim to assess the factors driving the changes in condomless sex but merely to capture the temporal changes over the entire time window for which data on condomless sex were available. Accordingly, we only use univariable models (note that missing data of covariates in the multivariable model was one main reason for the limited time window in Hasse et al [5]). Calendar time is included as a linear covariate in the logistic regression. To allow different effects of time before and after the Swiss-statement (2008), we also fit a variant of the model in which (1) the impact of calendar time can change in 2008 and (2) the odds for condomless sex can increase discontinuously in 2008. Technically, this is modeled as a piece-wise linear model for the log odds. Because most individuals could contribute several time points, we use robust standard errors (with clusters corresponding to follow-up visits from the same individual).
RESULTS
We analyzed responses to 162 405 questionnaires from 12 328 patients from the SHCS. Patients contributed a median (interquartile range [IQR]) of 12 (5–21) questionnaires and 6.8 (IQR, 2.6–12.5) years between the first and the last questionnaire. Overall, we find that the increase in condomless sex, previously observed for the time window of 2007–2009 [5], continues beyond this time window, but that this trend varies substantially across transmission groups and type of contact (occasional/stable partnership).
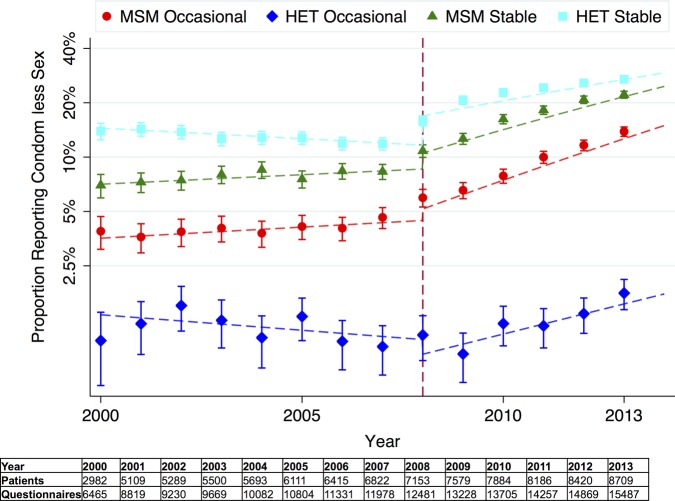
Both MSM and heterosexual HIV transmission groups exhibit increasing frequencies with which they report condomless sex in stable relationships after 2008 (see Figure 1). It is notable that the rates of condomless sex in stable relationships continue to increase substantially up to the end of the observation period (2013). Including calendar-year as a continuous variable in the logistic regression for the entire time range (2000–2013), yields an increase of the odds for condom-less sex in stable relationships of 1.14 [1.12–1.15]/year for MSM and 1.10 [1.08–1.11]/year for heterosexuals. If we allow for a different rate of increase for the years before and after the Swiss statement (2000–2007 vs 2008–2013), we find that the Swiss statement indeed is associated with an accelerated increase in condomless sex in stable relationships. For MSM, the odds of condomless sex increased by a factor of 1.03 (IQR, 1.00–1.05)/year before 2008 and by a factor of 1.19 (IQR, 1.16–1.21)/year from 2008 onwards. For heterosexuals, the odds for condomless sex decreased before 2008 (0.97 [IQR, 0.95–0.99]/year) and increased only from 2008 onwards (1.13 [IQR, 1.11–1.15]/year). Thus, in stable relationships, the Swiss statement has led to an accelerated increase of condomless sex in MSM and to a switch from decreasing to increasing rates of condomless sex in heterosexuals.
Figure 1.
Frequency with which human immunodeficiency virus-infected individuals report unprotected sex over time (yearly average and 95% confidence interval). Dashed lines correspond to the fit of the piece-wise linear model to the frequencies of unprotected sex. Occasional and Stable refer to type of sexual partnership). The vertical dashed line indicates the level of condomless sex in 2008 (year of the Swiss Statement): 10.8% (men who have sex with men [MSM], stable), 6.0% (MSM, occasional), 15.9% (heterosexuals [HET], stable), and 1.0% (HET, occasional). The table displays the number of questionnaires evaluated for a given year and the number of patients responding to questionnaires in that year.
For sex in occasional partnerships, we observed a more pronounced increase of condomless sex for MSMs than for heterosexuals (see Figure 1). Assuming the same slope for the entire time period 2000–2013, the odds for condomless occasional sex remained almost stable (change by a factor of 1.02 [IQR, 0.99–1.05]/year) for heterosexuals and increased by a factor 1.15 (IQR, 1.13–1.17)/year for MSM. If we allow for a different slope before and after 2008, the model detects again a stronger increase of condomless sex after 2008: for MSM, the odds for condomless sex increase by a factor 1.03 (IQR, 1.00–1.06)/year before 2008 and 1.22 (IQR, 1.18–1.25)/year after 2008. By contrast, the odds of condomless sex decreases in heterosexuals before 2008 (0.96 [IQR, 0.91–1.02]/year) and increase only weakly (1.14 [IQR, 1.06–1.22]/year) after 2008. Overall, for occasional relationships, only MSM exhibit a substantial increase of condomless sex over time and reach high levels of ∼15% in 2013, whereas rates of condomless sex in occasional partnerships remain low for heterosexuals (<2%) and exhibit only a weak increase over time.
DISCUSSION
Overall, our results show a switch from a slow temporal increase or even a decrease in rates of condomless sex before the Swiss statement to an accelerated increase after the Swiss statement. For sex in stable relationships, this effect occurs in both MSM and heterosexuals, but for occasional sex, a substantial increase occurs only in MSMs. It is notable that the increase of condomless sex has continued until the end of the observation period and has reached values above 10% in all groups except occasional sex in heterosexuals. For MSM, we also observed (weak) increases in condomless sex before the Swiss Statement. This result suggests that the Swiss statement accelerated and catalyzed changes in condomless sex that were already taking place in the community before 2008. In other words, the Swiss statement may have captured a change in the perception of HIV that was already developing previously, but it arguably also led to a substantial acceleration of this development. It is interesting to note that our analysis finds this effect to be most pronounced in the subgroup that was excluded from the statement, namely the group of MSM within nonstable partnerships.
A limitation of this analysis is that it depends on the reliability of the participants′ answers to the questionnaire (especially since the questionnaire is not self-completed). Therefore, in this study, the increase in reported condomless sex could, at least in part, also reflect an increase in the participants′ readiness to report such events because of a changed perception of the risk of HIV transmission. On the other hand, the increase of condomless sex has been accompanied by an increase in STIs [6] (even though the causal link remains to be explored), and a significant association between self-reported condomless sex and hepatitis C virus (HCV) and syphilis incidence has been shown previously [7, 8]. These results support the overall reliability of self-reported data on condomless sex and indicate that the pattern observed here does not merely reflect changes in social desirability and the associated changes in the reliability of patient responses. Moreover, despite the strong temporal association reported here, our results do not necessarily prove a causal association between the Swiss-Statement and condom use. For example, condom-use may also have decreased because of the success of ART in decreasing morbidity and mortality and the resulting perception that HIV is no longer a deadly threat for sexual partners.
Finally, it should be noted that the reported levels of condomless sex are not necessarily a proxy for the risk of HIV transmission, because in the SHCS, more than 90% of treated individuals have an undetectable virus load (see Hasse et al [5] for an assessment of risk factors associated with condomless sex). More generally, the reason behind the recent change of condomless sex is most likely multifactorial and complex, involving factors such as risk perceptions, treatment rates, and the demography of HIV-infected individuals. However, independently of HIV virus load and independently of the causality behind its increase, condomless sex is a strong risk factor for the transmission of other STIs. Hence, the observed patterns of condomless sex in occasional partnerships may have driven the recent increase in STIs [6] and the emergence of a sex-associated transmission route for HCV [7, 9–11].
Acknowledgments
We thank the patients who participated in the Swiss HIV Cohort Study (SHCS); the physicians and study nurses for excellent patient care; Brigitte Remy, Martin Rickenbach, F. Schoeni-Affolter, and Yannick Vallet from the SHCS Data Center in Lausanne for data management; and Danièle Perraudin and Mirjam Minichiello for administrative assistance.
The Swiss HIV Cohort Study. The members of the SHCS are: Aubert V, Battegay M, Bernasconi E, Böni J, Bucher HC, Burton-Jeangros C, Calmy A, Cavassini M, Dollenmaier G, Egger M, Elzi L, Fehr J, Fellay J, Furrer H (Chairman of the Clinical and Laboratory Committee), Fux CA, Gorgievski M, Günthard H (President of the SHCS), Haerry D (deputy of “Positive Council”), Hasse B, Hirsch HH, Hoffmann M, Hösli I, Kahlert C, Kaiser L, Keiser O, Klimkait T, Kouyos R, Kovari H, Ledergerber B, Martinetti G, Martinez de Tejada B, Metzner K, Müller N, Nadal D, Nicca D, Pantaleo G, Rauch A (Chairman of the Scientific Board), Regenass S, Rickenbach M (Head of Data Centre), Rudin C (Chairman of the Mother & Child Substudy), Schöni-Affolter F, Schmid P, Schüpbach J, Speck R, Tarr P, Telenti A, Trkola A, Vernazza P, Weber R, Yerly S.
Disclaimer. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Financial support. This study has been financed within the framework of the Swiss HIV Cohort Study, supported by the Swiss National Science Foundation (SNF grant #148522) and by the SHCS research foundation. R. K. was supported by SNF grant number PZ00P3-142411, and H. F. G. was supported by SNF grant number 320030_159868.
Potential conflicts of interest. H. F. G. has been an adviser and/or consultant for the following companies: GlaxoSmithKline, Abbott, Gilead, Novartis, Boehringer Ingelheim, Roche, Tibotec, Pfizer, and Bristol-Myers Squibb. He has also received unrestricted research and educational grants from Roche, Abbott, Bristol-Myers Squibb, Gilead, Astra-Zeneca, GlaxoSmithKline, and Merck Sharp & Dohme (all money went to institution).
All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
Contributor Information
Collaborators: and the Swiss HIV Cohort Study, V Aubert, M Battegay, E Bernasconi, J Böni, HC Bucher, C Burton-Jeangros, A Calmy, M Cavassini, G Dollenmaier, M Egger, L Elzi, J Fehr, J Fellay, H Furrer, CA Fux, M Gorgievski, H Günthard, D Haerry, B Hasse, HH Hirsch, M Hoffmann, I Hösli, C Kahlert, L Kaiser, O Keiser, T Klimkait, R Kouyos, H Kovari, B Ledergerber, G Martinetti, B Martinez de Tejada, K Metzner, N Müller, D Nadal, D Nicca, G Pantaleo, A Rauch, S Regenass, M Rickenbach, C Rudin, F Schöni-Affolter, P Schmid, J Schüpbach, R Speck, P Tarr, A Trkola, P Vernazza, R Weber, and S Yerly
References
- 1.Günthard HF, Aberg JA, Eron JJ et al. Antiretroviral treatment of adult HIV infection: 2014 recommendations of the International Antiviral Society-USA Panel. JAMA 2014; 312:410–25. [DOI] [PubMed] [Google Scholar]
- 2.Vernazza P, Hirschel B, Bernasconi E, Flepp M. Les personnes séropositives nesouffrant d'aucune autre MST et suivant un traitement antirétroviral efficace ne transmettent pas le VIH par voie sexuelle. Bull Med Suisse 2008; 89:165–9. [Google Scholar]
- 3.Cohen MS, Chen YQ, McCauley M et al. Prevention of HIV-1 infection with early antiretroviral therapy. N Engl J Med 2011; 365:493–505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cohen MS. HIV treatment as prevention and “The Swiss Statement”: in for a dime, in for a dollar? Clin Infect Dis 2010; 51:1323–4. [DOI] [PubMed] [Google Scholar]
- 5.Hasse B, Ledergerber B, Hirschel B et al. Frequency and determinants of unprotected sex among HIV-infected persons: the Swiss HIV cohort study. Clin Infect Dis 2010; 51:1314–22. [DOI] [PubMed] [Google Scholar]
- 6.Federal Office of Public Health - HIV/STI statistics, analyses and trends. Available at: http://www.bag.admin.ch/hiv_aids/12472/12480/12481/12484/index.html. Accessed 11 June 2015.
- 7.Wandeler G, Gsponer T, Bregenzer A et al. Hepatitis C virus infections in the Swiss HIV Cohort Study: a rapidly evolving epidemic. Clin Infect Dis 2012; 55:1408–16. [DOI] [PubMed] [Google Scholar]
- 8.Braun D, Kouyos R, Ghenzi R et al. Increasing rates of STI are linked to reduced condom use in patients with primary HIV-1 infection. Boston, Conference on Retroviruses and Opportunistic Infections, 2014. [Google Scholar]
- 9.Kouyos RD, Rauch A, Böni J et al. Clustering of HCV coinfections on HIV phylogeny indicates domestic and sexual transmission of HCV. Int J Epidemiol 2014; 43:887–96. [DOI] [PubMed] [Google Scholar]
- 10.Kouyos RD, Rauch A, Braun DL et al. Higher risk of incident hepatitis C virus coinfection among men who have sex with men, in whom the HIV genetic bottleneck at transmission was wide. J Infect Dis 2014; 210:1555–61. [DOI] [PubMed] [Google Scholar]
- 11.Vogel M, Boesecke C, Rockstroh JK. Acute hepatitis C infection in HIV-positive patients. Curr Opin Infect Dis 2011; 24:1–6. [DOI] [PubMed] [Google Scholar]