Abstract
Accurate interpretation of cervical spine imagining can be challenging, especially in children and the elderly. The biomechanics of the developing pediatric spine and age-related degenerative changes predispose these patient populations to injuries centered at the craniocervical junction. In addition, congenital anomalies are common in this region, especially those associated with the axis/dens, due to its complexity in terms of development compared to other vertebral levels. The most common congenital variations of the dens include the os odontoideum and a persistent ossiculum terminale. At times, it is necessary to distinguish normal development, developmental variants, and developmental anomalies from traumatic injuries in the setting of acute traumatic injury. Key imaging features are useful to differentiate between traumatic fractures and normal or variant anatomy acutely; however, the radiologist must first have a basic understanding of the spectrum of normal developmental anatomy and its anatomic variations in order to make an accurate assessment. This review article attempts to provide the basic framework required for accurate interpretation of cervical spine imaging with a focus on the dens, specifically covering the normal development and ossification of the dens, common congenital variants and their various imaging appearances, fracture classifications, imaging appearances, and treatment options.
Keywords: Cervical vertebrae, dens axis, odontoid process, spinal anatomy, spinal injuries
INTRODUCTION

Imaging evaluation of the cervical spine can be difficult at times, especially when dealing with a skeletally immature child or in the setting of variations in normal anatomic development. This is most evident at the craniocervical junction, where there is a higher incidence of injuries in young children and the elderly, as well as an increased incidence of congenital bony anomalies, particularly at the C-2 level. A basic understanding of normal development, developmental variants, and traumatic injury patterns is vital to correctly interpret cervical spine imaging studies. This review will focus on the normal and variant development of the axis (C-2) and the patterns of traumatic injury involving the dens.
NORMAL DEVELOPMENT
In the developing spine, vertebral bodies begin as focal ossification centers separated by synchondroses, which serve as cartilaginous bridges.[1] Somatic growth of the vertebrae continues well after fusion of the ossification centers and into early adulthood. In evaluating imaging studies in skeletally immature patients, ossification centers within the spine occur in predictable locations, have a typical appearance, and present at fairly predictable time intervals in terms of both ossification and fusion. Knowledge of the characteristic locations and imaging appearances will help ascertain normal development from both anatomic variants or anomalies and traumatic injury, especially in the acute setting.
In terms of development, the axis (C-2) is by far the most intricate of all the vertebral bodies, mainly due to the inclusion of the dens in addition to development of the underlying C-2 vertebral body. As with the remaining cervical spine vertebrae, the base of the axis consists of one anterior ossification center for the body and paired neural arch ossification centers posterolaterally [Figure 1a]. The body articulates with the adjacent intervertebral discs, while the neural arches form the posterior elements. Compared to other cervical levels, the body of C-2 normally has increased thickness and a square shape.[2] It plays an integral role in cervical spine mobility, as well as stability of the craniocervical junction and upper cervical spine.
Figure 1.
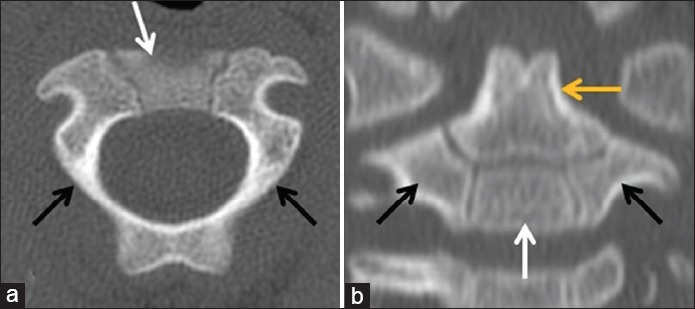
38-month-old child with normal ossification centers. (a) Axial CT image through the base of the dens shows the ossification centers of the lateral neural arches (black arrows) and anterior body (white arrow) of the axis. The posterior neural arches have already fused. (b) Coronal reformatted CT image through the anterior aspect of the C-2 vertebral body shows the lateral neural arch. (black arrows) and anterior body. (white) ossification centers, as well as the ossification center of the dens superiorly. (yellow arrow). The ossiculum terminale has yet to ossify.
The odontoid or dens develops from a primary ossification center along the superior margin of the anterior body [Figure 1b]. A secondary ossification center – ossiculum terminale – occurs along the tip of the dens; the ossiculum terminale typically does not ossify until the mid to latter half of the first decade of life [Figure 2].[1,3] The neural arches fuse posteriorly by around 3 years of age; the anterior body fuses to the neural arches and primary ossification center of the dens between 3 and 6 years of age, typically toward the latter end of the age range.[4] A persistent remnant of the synchondrosis between the anterior body and dens can be seen throughout adolescence and into early adulthood, especially on magnetic resonance (MR) imaging. The ossiculum terminale typically fuses to the remainder of the dens by the early portion of the second decade of life.[4,5]
Figure 2.
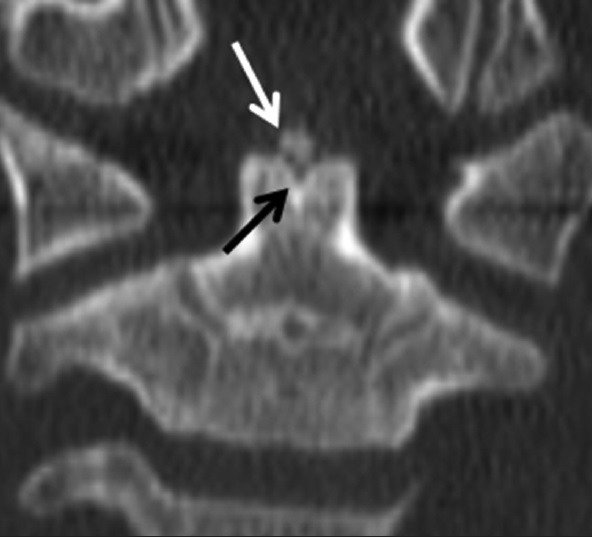
7-year-old child with a normal ossiculum terminale. Coronal reformatted CT image through the anterior aspect of the C-2 vertebral body shows ossification of the ossiculum terminale along the superior margin of the dens (white arrow). A characteristic “V”-shaped cartilaginous cleft is seen underlying the ossiculum terminale (black arrow).
On imaging, ossification centers are smooth and corticated, which helps differentiate them from irregular, lucent fractures in the setting of acute trauma. Synchondroses are symmetric and bordered by the cortical margins of the ossifications centers on either side.
DEVELOPMENTAL VARIANTS AND ANOMALIES
Os odontoideum
Os odontoideum refers to a well-corticated ossific density along the superior margin of a relatively hypoplastic or foreshortened base of the dens. There is continued debate as to its etiology – congenital or traumatic – with studies and reports supporting the pathogenesis of both.[6,7,8,9] Whether congenital or post-traumatic, the anomaly occurs early enough in development of the spine for secondary findings to be seen, including a relatively foreshortened base of the dens and a hypertrophied anterior arch of C-1 [Figure 3].
Figure 3.
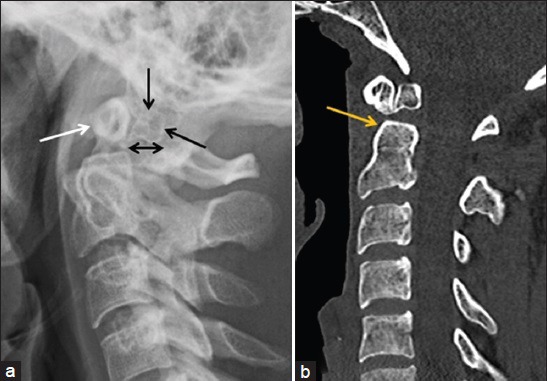
26-year-old man with chronic neck pain and an os odontoideum. (a) Lateral radiograph of the cervical spine shows posterior displacement of a well-corticated os odontoideum (black arrows), as well as hypertrophy of the anterior arch of C-1 (white arrow). (b) Reformatted sagittal CT image in the same patient demonstrates similar findings with restoration of normal alignment in the supine position. The margins of the os odontoideum are smooth and well-corticated, and the base of dens is relatively foreshortened (yellow arrow). The variation in alignment with positioning and posterior displacement of the os odontoideum on the plain radiograph confirms instability.
In the acute post-traumatic setting, an os odontoideum can be readily distinguished from a Type II dens fracture by the presence of smooth, well-corticated margins [Figure 4a]. Acute fractures, on the other hand, have lucent and somewhat irregular margins corresponding to the site of fracture [Figure 4b]. The morphology of the base of the dens and that of the anterior arch of the atlas are useful secondary findings to support an os odontoideum.
Figure 4.
26-year-old man with chronic neck pain and an os odontoideum versus an elderly woman with an acute Type. II dens fracture. (a) Reformatted sagittal CT image in the same young adult as Figure 3a demonstrates well-corticated margins of an os odontoideum. (white arrow) with characteristic secondary features, to include a hypertrophied anterior arch of C-1 and a relatively foreshortened base of the dens. (b) Coronal reformatted CT image through the upper cervical spine in an elderly woman with a fall demonstrates a fracture through the base of the dens with lucent margins. (yellow arrow).
Os odontoideum is characterized as one of two types: Orthotopic or dystopic. An orthotopic os is located in the expected anatomic location along the superior margin of the base of the dens. When unstable, it often articulates with the anterior arch of C-1 independent of the base of the dens; atlanto-dental instability may also be seen [Figures 3 and 5]. A dystopic os odontoideum refers to an os that is not in the expected anatomic location. Often, a dystopic os is fused to the basion (inferior margin of the clivus).
Figure 5.
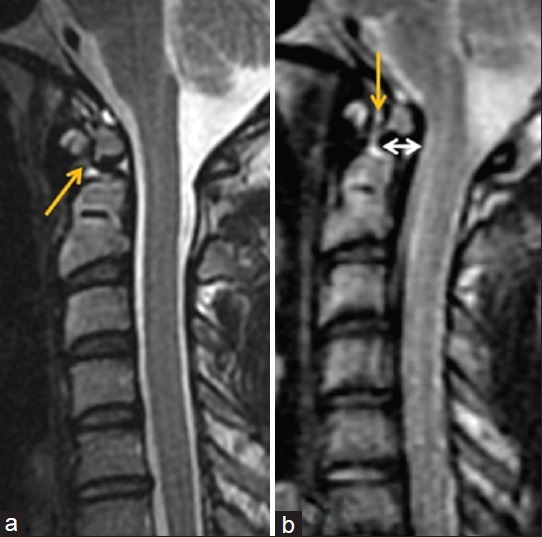
28-year-old man with chronic neck pain and an os odontoideum with instability. (a) Sagittal T2 MR image through the cervical spine in the neutral position shows normal alignment of the os odontoideum with respect to the C-2 body and a normal atlanto-dental interval (yellow arrow). (b) Repeat imaging with passive flexion shows posterior displacement of the os odontoideum (white arrow) and widening of the atlanto-dental interval (yellow arrow).
The clinical manifestations of an os odontoideum are variable, ranging from relatively asymptomatic to unstable with significant neurological deficits. Instability may lead to central canal stenosis at the craniocervical junction with associated cord compression. When incidentally found and stable, conservative management may be appropriate. If symptomatic and/or unstable, however, surgical intervention is often indicated with decompression and fixation.[7]
Persistent ossiculum terminale
A persistent ossiculum terminale refers to failure of fusion of the secondary ossification center along the superior margin of dens. As discussed previously, the ossiculum terminale typically ossifies during the mid to latter half of the first decade of life and fuses during the early portion of the second decade of life.[1,3,4,5] A persistent ossiculum terminale is an incidental finding that may mimic a Type I dens fracture, both of which are typically stable. In the setting of acute trauma, an ossiculum terminale or persistent ossiculum terminale can be distinguished from a fracture by the presence of smooth, corticated margins [Figure 6a]. In contrast, a fracture will have irregular, lucent margins [Figure 6b].
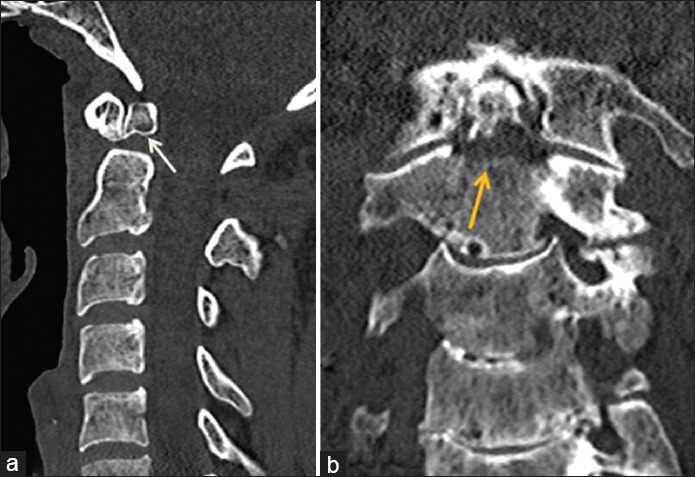
Figure 6.
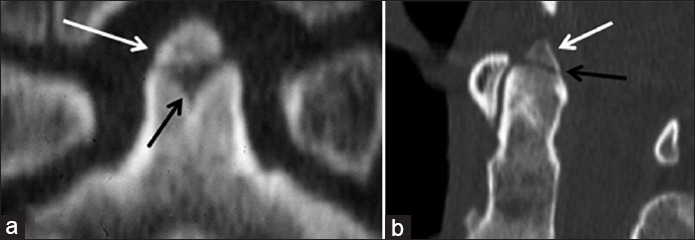
10-year-old boy with a normal ossiculum terminale versus an elderly gentleman post-trauma with an acute Type I dens fracture. (a) Coned-down reformatted coronal CT image of the C-2 vertebral body in the young boy shows a smooth, corticated ossification along the superior margin of the dens (white arrow) with an underlying “V”-shaped cartilaginous cleft. (b) Sagittal reformatted CT image in the elderly trauma patient demonstrates an ossific fragment along the superior margin of the dens (white arrow) with a subjacent lucent fracture line (black arrow).
In the chronic setting, it may be difficult to distinguish a persistent ossiculum terminale from a remote Type I dens fracture with nonunion, since both will demonstrate well-corticated margins. Helpful secondary findings to suggest a congenital variant as opposed to a remote fracture include a bony fragment that is of a disproportionate size compared to the expected bony fragment from a prior fracture, as well as the presence a “V”-shaped cartilaginous cleft along the superior margin of the dens subjacent to the persistent ossiculum terminale [Figure 6a].[5]
DENS FRACTURES
Dens fracture classification
Odontoid fractures are classically divided into three groups, as introduced by Anderson and D’Alonzo.[10] Type I fractures represent an avulsion fracture of the odontoid tip at the insertion of the alar ligament, Type II fractures occur through the base of dens, and Type III fractures extend into the C-2 vertebral body [Figure 7].
Figure 7.
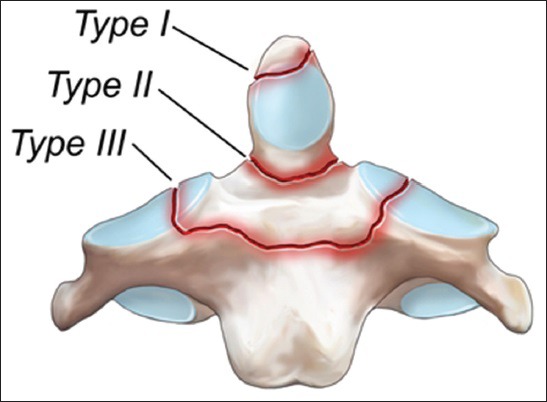
Illustration in the coronal plane demonstrates the odontoid fracture classification, as introduced by Anderson and D’Alonzo. Courtesy of Gilbert Gardner, Medical Illustrator.
Type I Dens fractures
Type I avulsion fractures are exceedingly rare (1–3%) with a limited number of case reports in the medical literature.[10,11] The fracture in isolation is typically described as stable.[12] Often, an alar ligament avulsion fracture (Type I) is confused with a smaller Type II fracture fragment, which is far more common. A true Type I fracture consists of a tiny bony fragment of the odontoid tip at the attachment site of the alar ligament [Figure 8]. Acutely, the fracture lacks corticated margins, which is a helpful distinguishing feature from a persistent ossiculum terminale. Chronically, however, the two may be indistinguishable on imaging. Based upon multiple case-controlled studies, Class III data (American Medical Association data classification) suggest that cervical immobilization for 6–8 weeks is the treatment of choice.[12]
Figure 8.
Elderly gentleman post-trauma with neck pain and a Type I dens fracture. (a) Sagittal and. (b) coronal reformatted CT images through the cervical spine show an ossific fragment along the superior aspect of the dens (white arrows) with a subjacent lucent fracture line. (black arrows).
Type II Dens fractures
Type II odontoid fractures represent the most common pattern of dens injury (54–60%) and occur through the base of dens at the junction of the C-2 vertebral body [Figure 9].[13,14,15] In children, the fracture may occur through the synchondrosis between the dens and body of C-2 [Figure 10]. The Type II fracture is traditionally considered unstable [Figure 11], often requiring immediate surgical stabilization; however, the decision between external fixation immobilization and surgical internal fixation currently remains controversial. The most common etiologies of Type II fractures include motor vehicle accidents (MVAs), followed by falls. This fracture pattern is more prevalent in the elderly, with a higher incidence in patients over 70 years of age. It has been hypothesized that osteoarthritis at the atlanto-dental and atlantoaxial articulations predisposes elderly patients to limited mobility and additional torque centered at the base of the dens, thus resulting in the increased incidence in this patient population.[16]
Figure 9.
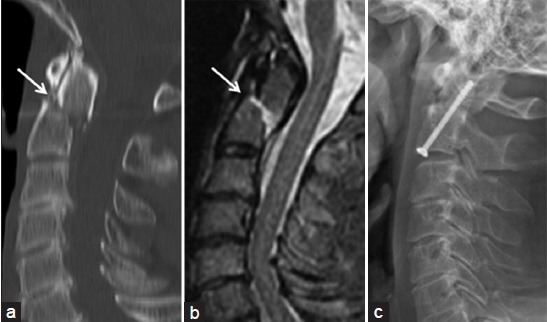
Middle-aged man post-trauma with multiple injuries, including a Type II dens fracture. (a) Sagittal reformatted CT image through the cervical spine demonstrates a displaced fracture through the base of the dens. (arrow) with small ossific fragments posteriorly. There is posterior displacement of the superior dens fragment and C-1 with respect to the base of the C-2 vertebral body. (b) Sagittal T2 MR image through the cervical spine shows the fracture. (arrow) with associated edema. (c) Lateral plain radiograph post internal anterior reduction and fixation demonstrates improved anatomic alignment.
Figure 10.

Young child post-trauma with a dens fracture through the synchondrosis. (a) Lateral radiograph of the cervical spine demonstrates abnormal anterior displacement and angulation of the dens with respect to the body of C-2 (arrow). (b) Sagittal reformatted CT image shows similar findings with the injury occurring through the synchondrosis (arrow). (c) Lateral radiograph post non-surgical external reduction and halo fixation reveals significantly improved alignment.
Figure 11.

Middle-aged adult with a history of ankylosing spondylitis and a Type II dens fracture with instability after trauma. (a) Sagittal reformatted CT image through the cervical spine reveals a displaced, comminuted fracture through the base of the dens. (white arrow), as well as comminuted posterior element fractures at C-2 and C-3 (black arrows). (b) Sagittal T2 MR image in the same patient demonstrates similar findings, along with severe central canal stenosis and cord compression with underlying cord signal abnormality (yellow arrow). There is also disruption of the anterior longitudinal ligament (white arrow).
Although controversial, management options for Type II odontoid fractures currently include external reduction and fixation with halo immobilization (non-surgical) and internal reduction and fixation (surgical) [Figures 9c and 10c].[12] Surgical fixation involves the inherent risk of surgery, but avoids the risk of nonunion which is relatively common with Type II dens fractures. Studies report an incidence of nonunion with non-surgical immobilization in roughly 26–30% of cases.[12,13] Risk factors of developing nonunion after non-surgical treatment include an age greater than 50 years at the time of injury (21 times more likely to fail immobilization compared to younger patients, Class II data),[17] greater than 6 mm dens displacement in any direction,[11,18] and moderate fracture comminution. Thus, halo immobilization is most successful in younger patients (<50 years of age) with minimal fracture displacement and no or minimal comminution. If surgical internal fixation is recommended, anterior fixation appears to have increased fusion rates compared to posterior fixation (90% and 74%, respectively).[12]
Since the original odontoid fracture classifications by Anderson and D’Alonzo in 1974, several authors have suggested an additional comminuted subtype of Type II fracture, designated as IIA.[19,20,21] Though this subtype is limited in the reported literature, moderate comminution and fracture fragment size >3 mm at the base of dens are more likely to develop nonunion without surgical reduction and internal fixation.[19,20,21] However, the clinical importance of mild comminution and smaller splinter fragments with regards to stability remains unknown.
Type III Dens fractures
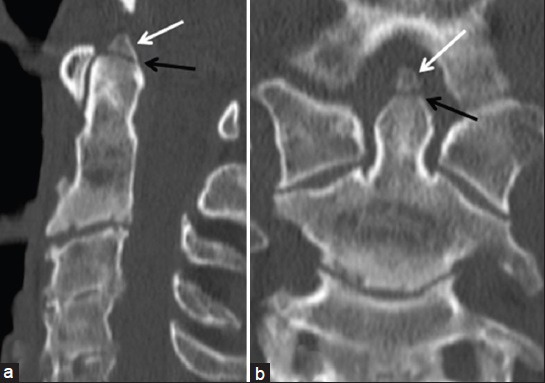
Type III dens fractures extend through the axis body and account for approximately 39–42% of dens fractures [Figure 12].[15] Fracture displacement is common (78%);[13,14] however, fewer than 8% of patients with Type III fractures develop nonunion after non-surgical immobilization alone.[12] Thus, Class III data support halo immobilization for 6–8 weeks as a first-line management.
Figure 12.
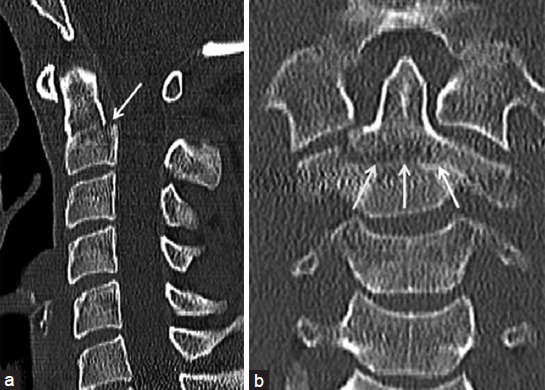
Young adult post-trauma with a Type III dens fracture. (a) Sagittal reformatted CT image through the cervical spine shows a mildly displaced dens fracture with extension into the body of C-2 (arrow) with anterior angulation of the dens. (b) Coronal reformatted CT image better depicts the extension into the C-2 body (arrows).
CONCLUSION
Imaging evaluation of the cervical spine in the setting of trauma can be difficult, especially when dealing with children or when confronted with potential underlying congenital abnormalities. This is especially true with the dens/C-2, which is developmentally the most intricate of the cervical vertebrae. Therefore, it is important for radiologists interpreting spine imaging to have an understanding of the normal appearance of the developing odontoid/dens, as well as the variant anatomy and anomalies, in order to be able to distinguish these from traumatic injuries. This knowledge will help ensure proper diagnosis and guide appropriate management for these patients.
Financial support and sponsorship
Nil.
Conflict of interest
The views expressed in this material are those of the authors, and do not reflect the official policy or position of the U.S. Government, the Department of Defense, or the Department of the Air Force.
Footnotes
Available FREE in open access from: http://www.clinicalimagingscience.org/text.asp?2015/5/1/38/159565
REFERENCES
- 1.Karwacki GM, Schneider JF. Normal ossification patterns of atlas and axis: A CT study. AJNR Am J Neuroradiol. 2012;33:1882–7. doi: 10.3174/ajnr.A3105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Castellana C, Kósa F. Morphology of the cervical vertebrae in the fetal-neonatal human skeleton. J Anat. 1999;194:147–52. doi: 10.1046/j.1469-7580.1999.19410147.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Piatt JH, Jr, Grissom LE. Developmental anatomy of the atlas and axis in childhood by computed tomography. J Neurosurg Pediatr. 2011;8:235–43. doi: 10.3171/2011.6.PEDS11187. [DOI] [PubMed] [Google Scholar]
- 4.Lustrin ES, Karakas SP, Ortiz AO, Cinnamon J, Castillo M, Vaheesan K, et al. Pediatric cervical spine: Normal anatomy, variants, and trauma. Radiographics. 2003;23:539–60. doi: 10.1148/rg.233025121. [DOI] [PubMed] [Google Scholar]
- 5.Ogden JA. Radiology of postnatal skeletal development. XII. The second cervical vertebra. Skeletal Radiol. 1984;12:169–77. doi: 10.1007/BF00361083. [DOI] [PubMed] [Google Scholar]
- 6.Sankar WN, Willis BP, Dormans JP, Drummond DS. Os odontoideum revisited: The case for a multifactorial etiology. Spine (Phila Pa 1976) 2006;31:979–84. doi: 10.1097/01.brs.0000214935.70868.1c. [DOI] [PubMed] [Google Scholar]
- 7.Arvin B, Fournier-Gosselin MP, Fehlings MG. Os odontoideum: Etiology and surgical management. Neurosurgery. 2010;66(Suppl):22–31. doi: 10.1227/01.NEU.0000366113.15248.07. [DOI] [PubMed] [Google Scholar]
- 8.White IK, Mansfield KJ, Fulkerson DH. Sequential imaging demonstrating os odontoideum formation after a fracture through the apical odontoid epiphysis: Case report and review of the literature. Childs Nerv Syst. 2013;29:2111–5. doi: 10.1007/s00381-013-2132-6. [DOI] [PubMed] [Google Scholar]
- 9.McHugh BJ, Grant RA, Zupon AB, DiLuna ML. Congenital os odontoideum arising from the secondary ossification center without prior fracture. J Neurosurg Spine. 2012;17:594–7. doi: 10.3171/2012.9.SPINE12824. [DOI] [PubMed] [Google Scholar]
- 10.Anderson LD, D’Alonzo RT. Fractures of the odontoid process of the axis. J Bone Joint Surg Am. 1974;56:1663–74. [PubMed] [Google Scholar]
- 11.Greene KA, Dickman CA, Marciano FF, Drabier JB, Hadley MN, Sonntag VK. Acute axis fractures. Analysis of management and outcome in 340 consecutive cases. Spine (Phila Pa 1976) 1997;22:1843–52. doi: 10.1097/00007632-199708150-00009. [DOI] [PubMed] [Google Scholar]
- 12.Julien TD, Frankel B, Traynelis VC, Ryken TC. Evidence-based analysis of odontoid fracture management. Neurosurg Focus. 2000;8:e1. doi: 10.3171/foc.2000.8.6.2. [DOI] [PubMed] [Google Scholar]
- 13.Hadley MN, Browner C, Sonntag VK. Axis fractures: A comprehensive review of management and treatment in 107 cases. Neurosurgery. 1985;17:281–90. doi: 10.1227/00006123-198508000-00006. [DOI] [PubMed] [Google Scholar]
- 14.Hadley MN, Dickman CA, Browner CM, Sonntag VK. Acute axis fractures: A review of 229 cases. J Neurosurg. 1989;71:642–7. doi: 10.3171/jns.1989.71.5.0642. [DOI] [PubMed] [Google Scholar]
- 15.Pryputniewicz DM, Hadley MN. Axis fractures. Neurosurgery. 2010;66(Suppl):68–82. doi: 10.1227/01.NEU.0000366118.21964.A8. [DOI] [PubMed] [Google Scholar]
- 16.Lakshmanan P, Jones A, Howes J, Lyons K. CT evaluation of the pattern of odontoid fractures in the elderly--relationship to upper cervical spine osteoarthritis. Eur Spine J. 2005;14:78–83. doi: 10.1007/s00586-004-0743-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lennarson PJ, Mostafavi H, Traynelis VC, Walters BC. Management of type II dens fractures: A case-control study. Spine (Phila Pa 1976) 2000;25:1234–7. doi: 10.1097/00007632-200005150-00006. [DOI] [PubMed] [Google Scholar]
- 18.Ekong CE, Schwartz ML, Tator CH, Rowed DW, Edmonds VE. Odontoid fracture: Management with early mobilization using the halo device. Neurosurgery. 1981;9:631–7. doi: 10.1227/00006123-198112000-00004. [DOI] [PubMed] [Google Scholar]
- 19.Hadley MN, Browner CM, Liu SS, Sonntag VK. New subtype of acute odontoid fractures (type IIA) Neurosurgery. 1988;22:67–71. doi: 10.1227/00006123-198801010-00010. [DOI] [PubMed] [Google Scholar]
- 20.Koc RK, Akdemir H, Oktem IS, Kurtsoy A, Menkü A. Posterolaterally displaced type IIA odontoid fractures. Neurosurg Rev. 2001;24:143–6. doi: 10.1007/pl00012399. [DOI] [PubMed] [Google Scholar]
- 21.Koivikko MP, Kiuru MJ, Koskinen SK. Occurrence of comminution (type IIA) in type II odontoid process fractures: A multi-slice CT study. Emerg Radiol. 2003;10:84–6. doi: 10.1007/s10140-003-0294-3. [DOI] [PubMed] [Google Scholar]


