Abstract
Research scientists and clinicians should be aware that missed diagnoses of mild-moderate traumatic brain injuries in post-acute patients having spinal cord injuries may approach 60–74% with certain risk factors, potentially causing clinical consequences for patients, and confounding the results of clinical research studies. Factors leading to a missed diagnosis may include acute trauma-related life-threatening issues, sedation/intubation, subtle neuropathology on neuroimaging, failure to collect Glasgow Coma Scale scores or duration of posttraumatic amnesia, or lack of validity of this information, and overlap in neuro-cognitive symptoms with emotional responses to spinal cord injuries. Strategies for avoiding a missed diagnosis of mild-moderate traumatic brain injuries in patients having a spinal cord injuries are highlighted in this perspective.
Keywords: traumatic brain injury, spinal cord injuries, dual diagnosis, diagnosis, complications, rehabilitation, post-concussion syndrome, brain concussion
Missed diagnoses of co-occurring concussions in post-acute patients having spinal cord injuries would have clinical consequences for patients, and would confound the results of clinical research studies. Research scientists and clinicians, including physicians, nurses, and therapists, should always be aware that there is a possibility of a missed diagnosis of a traumatic brain injury (TBI), and particularly of a concussion in patients having a spinal cord injury (SCI). Incidence of a dual diagnosis of SCI with a co-occurring TBI may approach 60–74% with certain risk factors that may include a motor vehicle collision (MVC) or a fall as the mechanism of injury, cervical level SCI particularly at C1 through C4, complete SCI level trauma, and trauma associated with alcohol intoxication (Tolonen et al., 2007; Macciocci et al., 2008; Kushner and Alvarez, 2014). Reportedly the frequency of missed TBI diagnoses may be higher in non-MVC trauma patients than in MVC patients, 75% versus 42.9% respectively (Sharma et al., 2014). Mild traumatic brain injury (MTBI), which is also known as a concussion, occurs most commonly in 64–73% of dual diagnosis cases (Macciocci et al,, 2008; Kushner and Alvarez, 2014). The presence of acute trauma-related life-threatening issues and/or the need for sedation or intubation during acute care hospitalizations of SCI patients may result in a missed diagnosis of mild-moderate severity TBIs (Kushner and Alvarez, 2014; Sharma et al., 2014). In addition other factors that may lead to a missed diagnosis may include: (1) the subtle neuropathology of mild TBI to which computed tomography (CT) and conventional magnetic resonance imaging (MRI) are not sensitive or specific, (2) the necessary focus in acute care on management of SCI, (3) failure to collect Glasgow Coma Scale (GCS) scores, and the duration of posttraumatic amnesia (PTA) or loss of consciousness (LOC), or lack of validity of this information; and (4) the overlap in symptoms of mild-moderate TBIs such as attentional disturbance, impaired concentration and cognition, emotional lability/dysregulation and anxiety with (a) emotional response to SCI and (b) effects of psychoactive medications used for SCI patients (Sharma et al., 2014). Furthermore, a mechanism for SCI trauma other than a MVC, such as a fall or an assault, may increase the likelihood of a missed diagnosis perhaps due to a lessened expectation for a TBI in non-MVC patients (Sharma et al., 2014).
The diagnosis of a concomitant concussion and particularly of a mild-moderate severity TBI, in a SCI patient is important for planning rehabilitation interventions, to maximize functional returns, and for the prevention, anticipation, and early treatment of possible related medical complications. In addition, clinical research protocol outcomes may be confounded by a missed dual diagnosis of a TBI in SCI patients. Simple strategies to help clinicians and clinical researchers to avoid a missed diagnosis of a co-occurring concussion or mild-moderate TBI in patients having a spinal cord injury will be highlighted in this perspective including the careful review of medical records looking for specific diagnostic criteria, vigilance for post concussion symptoms/signs, neuroimaging assessment, observation for possible medical complications, and clinicians/researchers should re-visit the possibility of persisting concussion/MTBI later in course of injury when some of the acute matters that either redirect attention away from patients or confound diagnosis have resolved.
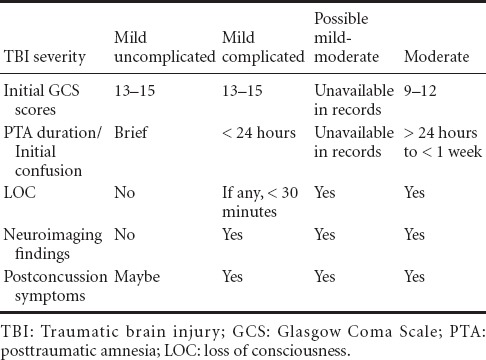
On admission to any post-acute SCI care setting such as an inpatient or outpatient rehabilitation program clinicians should obtain a careful patient history that would include a thorough review of the medical records looking for any indication of a co-occurring TBI. Similarly, clinical researchers must screen SCI patients’ history and records looking for classification criteria and/or signs for a TBI. TBI may be defined as head trauma involving an alteration of consciousness having signs that may include confusion, loss of consciousness (LOC), and amnesia with or without other neurologic deficits (Kushner and Alvarez, 2014). The standard classifications of TBI severity that range from mild to moderate and severe, are diagnosed by the initial GCS scores and the duration of posttraumatic amnesia (PTA) and/or LOC. The diagnostic criteria for a MTBI/concussion are given in Table 1 (Kushner, 1998, 2014; Macciocci et al., 2008). However, intubation, sedation, seizures, and/or alcohol or other drug/substance intoxication may confound the initial assessment of GCS scores, PTA durations, and LOC in trauma patients complicating the diagnosis and classification of a brain injury and the initial severity. Thus a concussion may be simply defined as an acute trauma induced alteration of mental function (PTA) lasting fewer than 24 hours, with or without preceding LOC (Kushner, 2001). If there is evidence for an acute trauma induced alteration of mental function lasting greater than 24 hours, then there may be a moderate severity TBI. Clinicians and researchers may establish a diagnosis of a mild-moderate TBI during post-acute care in based on a careful review of the patient's history/records if there was evidence for LOC at the scene of trauma or subsequent PTA, confusion, behavioral issues, seizures and/or abnormal results of any brain imaging studies. The records review should include paramedic/emergency rescue notes, acute care emergency department documentation, intensive care unit notes, consultation reports, therapy notes, nursing notes, attending physician notes, psychology reports and all radiology neuroimaging.
Table 1.
Classification criteria for mild to moderate TBIs
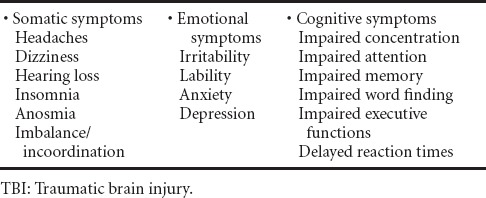
The occurrence of postconcussion symptoms in an SCI patient should also raise clinical suspicion for a dual diagnosis concussion or a mild-moderate TBI. SCI patients, family members, and/or interdisciplinary therapy staff may report or observe physical, behavioral, and/or cognitive symptoms. Somatic, affective, and/or cognitive symptoms resulting from brain injury and/or from trauma involving other head/neck structures may occur as part of a postconcussion syndrome that is well described in the medical literature, which may complicate the recovery after a mild-moderate TBI, and which may be a presenting feature of a mild-moderate TBI (Kushner, 1998, 2014). Possible postconcussion symptoms in mild-moderate TBIs are shown in Table 2. Headache and dizziness are the most common of the somatic postconcussion symptoms, and these symptoms have multiple possible etiologies. For example, among the many potential causes for headache are posttraumatic migraines, radiculopathy involving the second and/or third nerve root in patients with a cervical spine injury, and inner ear injuries, such as benign positional vertigo or a perilymphatic fistula in patients also having posttraumatic dizziness (Kushner, 1998, 2014). Similarly, there are many possible causes for the other somatic symptoms, including dizziness, hearing loss, anosmia, insomnia, and neck pain. Affective symptoms may include irritability, lability, anxiety, and depression. Cognitive symptomsmay include difficulties with concentration, attention, memory, and executive functions. Neuropsychological symptoms, that may include affective and/or cognitive manifestations, become increasingly likely in patients at the worse end of the clinical spectrum of concussion in which there are pathologic findings on neuroimaging studies, including those patients having complicated concussion, or a mild-moderate TBI. Importantly, postconcussion symptoms may be multifactorial in etiology including psychogenic and/or biologic in origin. For example, somatic and neuropsychological symptoms may be premorbid and/or rooted in post-injury psychological factors such as anxiety, depression or a posttraumatic stress disorder (Kushner, 1998; Auxéméry et al., 2012; Shenton et al., 2012;). An experienced neuropsychologist may clarify the etiology of neuropsychological symptoms with the use of standard neuropsychological testing measures that are adapted for upper extremity weakness in cervical SCIs (Sharma et al., 2014). Patients having neuropsychological symptoms associated with brain trauma are more likely to have unilateral or multifocal brain lesions on neuroimaging studies (Levin et al., 1990, 1992). In general, the presence of a postconcussion symptom complex involving somatic, affective and cognitive symptoms in an SCI patient who was asymptomatic prior to trauma is highly suggestive of a co-occurring concussion or mild-moderate TBI.
Table 2.
Possible “postconcussion” symptoms in mild to moderate TBIs
Neuroimaging studies may help to confirm a diagnosis of a complicated concussion or a mild-moderate TBI, particularly in SCI patients having postconcussion symptoms, especially when the records review may have been inconclusive. Symptomatic patients who may have had an initial negative brain CT scan may have findings consistent with areas of axonal shear injury and/or small contusions or hemorrhages on brain MRI scans for up to 2–3 months after trauma (Levin et al., 1992). MRI sensitivity to micro-bleeds associated with MTBI and axonal injury may be best on a T2 gradient echo sequence and a T2 FLAIR sequence (Sharma et al., 2014). Also, though still somewhat controversial, diffusion tensor MRI (DTI) is increasingly useful in showing lesions of specific brain white-matter pathway tract lesions that could be contributing to postconcussion symptoms (Aoki et al., 2012; Choi et al., 2012; Shenton et al., 2012; Wäljas et al., 2015). However DTI imaging may have resolution limitations in clarifying areas of injury in certain areas of the brain such as in regions of multiple tract crossings (Shin et al., 2014). Recent studies suggest that a combination of multiple neuroimaging modalities may improve the diagnostic accuracy for mild-moderate TBI, such as theuse of DTI with magnetic resonance spectroscopy (Xiong et al., 2014) and the use of DTI with a newer modality known as magnetoencephalography (Huang et al., 2015).
Concussion and mild-moderate TBIs may be complicated by seizures, skull fractures, cerebrospinal fluid fistulas, pneumocephalusand cavernous sinus fistulas, the findings of which may indicate the presence of a dual diagnosis TBI in an SCI patient. Seizures and epilepsy may occur in post-acute patients having MTBIs (Webb et al., 2014). Areas of intracerebral bleeding, cortical contusions, or depressed skull fractures increase the risk of posttraumatic epilepsy (Kushner, 1998, 2014). Any skull fracture is associated with traumatic forces sufficient to produce at least a concussion. Dural membrane lacerations can occur in association with fractures at the skull base or frontal bone and these may present as a cerebrospinal fluid fistula leak that may manifest withcomplaints of a chronic running nose or fluid in an ear. Pneumocephalus seen on neuroimaging may be a sign of a frontal bone fracture and which may also be a cause of headaches. Fractures of the skull base may be associated with injury of the cavernous sinus which may cause a cavernous sinus syndrome manifesting with diplopia, unilateral facial pain and/or numbness, Horner syndrome, and unilateral scleral erythema. The occurrence of any of these complications in an SCI patient would be associated with a dual diagnosis TBI.
Lastly, a back-up strategy for the prevention of a missed diagnosis of mild-moderate TBI would be for clinicians and/or researchers to re-visit the possibility of persisting symptoms and/or signs of a mild-moderate TBI prior to discharge from acute-care or early in post-acute care after an SCI patient has been stabilized and after all life-threatening matters that either redirect attention away from patients or confound diagnosis have resolved.
In summary, strategies that clinicians and clinical research scientists may use to avoid a missed diagnosis of co-occurring concussion or mild-moderate TBI in post-acute patients having a SCI mayinclude the following actions:
There should be a thorough review of the patient history and records looking for any of the classification criteria and/or signs for a concussion or mild-moderate TBI.
There should be vigilance for a postconcussion symptom complex.
There should be standard neuropsychological testing measures that are adapted for upper extremity weakness in cervical SCIs administered by an experienced neuropsychologist to help clarify the source of any unexplained neuropsychological symptoms.
Neuroimaging studies, including DTI, should be reviewed and/or ordered to help in the confirmation of a diagnosis of a concussion or a mild-moderate TBI, particularly in SCI patients having postconcussion symptoms.
There should be awareness that in SCI patients seizures, skull fractures, cerebrospinal fluid fistulas, pneumocephalus and cavernous sinus fistulas could be associated at a minimum with a complicated concussion or a mild-moderate TBI.
Clinicians/researchers should re-visit the possibility of persisting symptoms and/or signs of a mild-moderate TBI later in course of injury when some of the acute matters that either redirect attention away from patients or confound diagnosis have resolved.
Footnotes
Funding: Department of Physical Medicine & Rehabilitation funding by the United States Department of Education, National Institute of Disability Research and Rehabilitation # H133A120099 (TBI Model Systems grant).
Conflicts of Interest: The author of this perspective has no disclosures or conflicts of interest. Dr Kushner is the first author on the recently published review article: Kushner DS, Alvarez G (2014) Dual diagnosis: traumatic brain injury with spinal cord injury. Phys Med Rehabil Clin N Am 25:681-696.
References
- Aoki Y, Inokuchi R, Gunshin M, Yahagi N, Suwa H. Diffusion tensor imaging studies of mild traumatic brain injury: a meta-analysis. J Neurol Neurosurg Psychiatry. 2012;83:870–876. doi: 10.1136/jnnp-2012-302742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Auxéméry Y. Mild traumatic brain injury and postconcussive syndrome: a re-emergent questioning. Encephale. 2012;38:329–335. doi: 10.1016/j.encep.2011.07.003. [DOI] [PubMed] [Google Scholar]
- Choi GS, Kim OL, Kim SH, Ahn SH, Cho YW, Son SM, Jang SH. Classification of cause of motor weakness in traumatic brain injury using diffusion tensor imaging. Arch Neurol. 2012;69:363–367. doi: 10.1001/archneurol.2011.1930. [DOI] [PubMed] [Google Scholar]
- Huang M, Risling M, Baker DG. The role of biomarkers and MEG-based imaging markers in the diagnosis of post-traumatic stress disorder and blast-induced mild traumatic brain injury. Psychoneuroendocrinology. 2015 doi: 10.1016/j.psyneuen.2015.02.008. doi: 10.1016/j.psyneuen.2015.02.008. [DOI] [PubMed] [Google Scholar]
- Kushner DS, Alvarez G. Dual diagnosis: traumatic brain injury with spinal cord injury. Phys Med Rehabil Clin N Am. 2014;25:681–696. doi: 10.1016/j.pmr.2014.04.005. [DOI] [PubMed] [Google Scholar]
- Kushner DS. Concussion in sports: minimizing the risk for complications. Am Fam Physician. 2001;64:1007–1014. [PubMed] [Google Scholar]
- Kushner D. Mild traumatic brain injury: toward understanding manifestations and treatment. Arch Intern Med. 1998;158:1617–1624. doi: 10.1001/archinte.158.15.1617. [DOI] [PubMed] [Google Scholar]
- Levin HS, Williams DH, Eisenberg HM. Mild head injury classification. Neurosurgery. 1990;27:422–428. doi: 10.1097/00006123-199009000-00014. [DOI] [PubMed] [Google Scholar]
- Levin HS, Williams DH, Eisenberg HM, High WM, Jr, Guinto FC., Jr Serial MRI and neurobehavioural findings after mild to moderate closed head injury. J Neurol Neurosurg Psychiatry. 1992;55:255–262. doi: 10.1136/jnnp.55.4.255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Macciocchi S, Seel RT, Thompson N, Byams R, Bowman B. Spinal cord injury and co-occurring traumatic brain injury: assessment and incidence. Arch Phys Med Rehabil. 2008;89:1350–1357. doi: 10.1016/j.apmr.2007.11.055. [DOI] [PubMed] [Google Scholar]
- Sharma B, Bradbury C, Mikulis D, Green R. Missed diagnosis of traumatic brain injury in patients with traumatic spinal cord injury. J Rehabil Med. 2014;46:370–373. doi: 10.2340/16501977-1261. [DOI] [PubMed] [Google Scholar]
- Shenton ME, Hamoda HM, Schneiderman JS, Bouix S, Pasternak O, Rathi Y, Vu MA, Purohit MP, Helmer K, Koerte I, Lin AP, Westin CF, Kikinis R, Kubicki M, Stern RA, Zafonte R. A review of magnetic resonance imaging and diffusion tensor imaging findings in mild traumatic brain injury. Brain Imaging Behav. 2012;6:137–192. doi: 10.1007/s11682-012-9156-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shin SS, Pathak S, Presson N, Bird W, Wagener L, Schneider W, Okonkwo DO, Fernandez-Miranda JC. Detection of white matter injury in concussion using high-definition fiber tractography. Prog Neurol Surg. 2014;28:86–93. doi: 10.1159/000358767. [DOI] [PubMed] [Google Scholar]
- Tolonen A, Turkka J, Salonen O, Ahoniemi E, Alaranta H. Traumatic brain injury is under-diagnosed in patients with spinal cord injury. J Rehabil Med. 2007;39:622–626. doi: 10.2340/16501977-0101. [DOI] [PubMed] [Google Scholar]
- Wäljas M, Iverson GL, Lange RT, Hakulinen U, Dastidar P, Huhtala H, Liimatainen S, Hartikainen K, Öhman J. A Prospective Biopsychosocial Study of the Persistent Post-Concussion Symptoms following Mild Traumatic Brain Injury. J Neurotrauma. 2015;32:534–547. doi: 10.1089/neu.2014.3339. [DOI] [PubMed] [Google Scholar]
- Webb TS, Whitehead CR, Wells TS, Gore RK, Otte CN. Neurologically-related sequelae associated with mild traumatic brain injury. Brain Inj. 2014;26:1–8. doi: 10.3109/02699052.2014.989904. [DOI] [PubMed] [Google Scholar]
- Xiong KL, Zhu YS, Zhang WG. Diffusion tensor imaging and magnetic resonance spectroscopy in traumatic brain injury: a review of recent literature. Brain Imaging Behav. 2014;8:487–496. doi: 10.1007/s11682-013-9288-2. [DOI] [PubMed] [Google Scholar]


