Abstract
Background
Contralateral prophylactic mastectomy (CPM) is increasingly chosen by breast cancer patients and may be related to increased use of immediate reconstruction. This study examines long-term patient satisfaction with CPM and reconstruction in a historical cohort.
Methods
621 unilateral breast cancer patients with a family history of breast cancer who underwent CPM between 1960–1993 were surveyed regarding QOL and satisfaction with CPM at two time points - approximately 10 years and 20 years after CPM.
Results
583 women responded to the first follow-up questionnaire (median 10.7 years, mean 11.9 years) after CPM. 403 (69%) underwent reconstruction and 180 (31%) did not. Women electing reconstruction were younger (mean age 47 vs 53 years, p=0.01) and more likely to be married (85% vs 78%, p=0.048). Most women reported satisfaction with CPM (83%), that they would choose CPM again (84%) and make the same choice regarding reconstruction (73%). However, reconstruction patients demonstrated significantly lower satisfaction (p=0.0001) and were less likely to choose CPM again (p<0.0001). Within the reconstruction group, 39% needed 1+ unplanned reoperation, and this was strongly associated with lower satisfaction (p=0.0001), lower likelihood of choosing CPM again (p=0.006) and lower likelihood of choosing reconstruction again (p<0.0001). 269 women responded to the second questionnaire (median 18.4 years, mean 20.2 years after CPM). Satisfaction with CPM remained high, with 92% of women stating they would choose CPM again.
Conclusions
Most women report stable long-term satisfaction with CPM. Women who had reconstruction and required reoperations in this historical cohort reported lower satisfaction.
Keywords: contralateral prophylactic mastectomy, satisfaction, quality of life, breast reconstruction
Background
Women diagnosed with breast cancer face multiple complex decisions regarding treatment. Some of the main surgical decisions are choosing between breast conservation surgery usually followed by radiation versus mastectomy for their index breast, if undergoing mastectomy deciding on whether or not to pursue immediate reconstruction, and deciding on contralateral prophylactic mastectomy (CPM).
CPM has been shown to substantially reduce risk of breast cancer development in the contralateral breast(1–5) and is increasingly chosen by patients.(6,7) However there are limited data on survival benefit (8,9) with the majority of studies showing no survival advantage.(10) Young patient age and family history of breast cancer are associated with use of CPM,(11–14) as are use of immediate reconstruction, preoperative magnetic resonance imaging and unsuccessful attempts at breast conservation.(15,16) Importantly physician’s advice has also been shown to be a key factor,(11) which indicates the importance of accurate and appropriate counseling regarding this choice and the potential outcomes. Patient desire for peace of mind regarding future breast cancer risk is also thought to play a role in the decision for CPM.(11) Often the choice for CPM is not associated with elevated risk for contralateral breast cancer.(6,15,17)
However, CPM is not without the potential for complications and decrease in quality of life. Several studies have evaluated the impact of CPM on quality of life, demonstrating overall satisfaction. The most common adverse side effects are related to changes in body appearance, feelings of femininity and sexual relationships.(16) Literature regarding morbidity of CPM is less abundant.(18) Studies have shown that the complication rate associated with CPM is similar to the rate of complication for surgery on the side of the index breast cancer and thus CPM at time of therapeutic mastectomy leads to a doubling of the complication rate.(19,20) The majority of women who elect CPM elect immediate breast reconstruction.(21) Immediate breast reconstruction is associated with higher rates of complications and reoperation(22,23) compared to mastectomy without reconstruction.(21)
Previous work from our institution has reported on satisfaction related to decision making regarding CPM and also reported on reoperation rates after CPM. However, to date the association of breast reconstruction after CPM with satisfaction and psychosocial impact has not been fully elucidated.
In the current study, we evaluate the long-term satisfaction of a cohort of women who underwent CPM and compare satisfaction between those with breast reconstruction and those without reconstruction. We also examine the adverse aspects patients attribute to reconstruction and the subsequent effect on psychosocial consequences.
Methods
With Institutional Review Board approval, a previously established cohort of women who underwent mastectomy between 1960 and 1993 was identified.(1,21) 621 women with unilateral breast cancer and a family history of breast cancer and who underwent CPM were surveyed with questionnaires evaluating QOL and satisfaction with CPM at two time points.
The first follow-up survey was conducted a mean of 10 years after CPM the second follow-up survey was performed approximately 10 years later and used a study specific questionnaire. All surveys were mailed to the patients and non-responders had a second mailing sent out with a subsequent telephone contact when needed.
Medical record review was performed to collect demographic, medical and procedure variables, and for follow-up information regarding any additional surgical procedures. Unanticipated reoperations were identified from both survey results and medical record review. All reoperations whether identified from survey, medical record or both were included (see details in previous report).(21) The cohort of patients has been previously described.(8,11,16,21)
Reasons for reoperation were classified as: immediate postoperative complications, implant-related issues, aesthetic concerns (non–implant related), nodule removal and other. Each reoperation could have multiple indications. We limited analysis to reoperations and complications on the CPM side.
Statistical Analysis
Data were summarized using mean or median (range) for continuous variables and frequency (percentage) for categorical variables. Patients with and without breast reconstruction following CPM were compared using two-sample t-tests, Wilcoxon rank-sum tests, or chi-square tests, as appropriate. Survey question comparisons used the original response scale although descriptive statistics were reported with collapsed categories for conciseness. Sample sizes varied across questions due to individual item non-response, which was <5% of the analysis sample for most questions and <10% in all cases. Multivariate analysis was performed using linear regression. P-values <0.05 were considered statistically significant. Analysis was performed using SAS (Version 9.2, SAS Institute Inc., Cary, NC). Open-ended questions were coded for themes and concepts by two coders who discussed any discrepancies and came to agreement and frequencies were tabulated.
Results
Patients
Of the 621 patients in the initial cohort, 583 women responded to the first follow-up questionnaire at a mean of 11.9 years (range 1.9–35.4 years, median 10.7 years) after CPM. Of these, 403 (69%) underwent immediate (389, 97%) or delayed (14, 3%) reconstruction. The type of reconstruction was implant in 397 (98.5%) and TRAM in the remainder (6, 1.5%).
Demographic and clinical variables for those with and without reconstruction appear in Table 1. Those undergoing reconstruction were significantly younger than those not undergoing reconstruction and were more likely to be married. Not surprisingly, type of mastectomy (simple or subcutaneous) in the CPM was strongly associated with reconstruction, with subcutaneous mastectomy more common in patients undergoing reconstruction.
Table 1.
Demographic and surgical variables compared between those with and without reconstruction.
| Variable | Reconstruction N = 403 | No Reconstruction N = 180 | p-value |
|---|---|---|---|
| Age at CPM, yrs, mean (range) | 46.6 (21, 71) | 52.7 (27, 85) | 0.01 |
| Age at Survey, yrs, mean (range) | 57.0 (28, 82) | 68.4 (29, 92) | <0.0001 |
| Marital status, n (%) | 0.0005 | ||
| Married | 341 (84.8) | 140 (77.8) | |
| Single | 14 (3.5) | 7 (3.9) | |
| Divorced/separated | 19 (4.7) | 5 (2.8) | |
| Widowed | 18 (4.5) | 27 (15.0) | |
| Unknown | 11 (2.7) | 1 (0.6) | |
| Stated reason(s) for electing CPM*, n (%) | |||
| Cancer in the index breast | 297 (73.7) | 145 (80.6) | 0.07 |
| Physician’s advice | 233 (57.8) | 110 (61.1) | 0.45 |
| Family history | 166 (41.2) | 68 (37.8) | 0.44 |
| Lumpy breasts | 101 (25.1) | 45 (25.0) | 0.99 |
| Alleviate worry | 97 (24.1) | 31 (17.2) | 0.06 |
| Others | 106 (26.3) | 59 (32.8) | 0.11 |
| Type of CPM, n (%) | <0.0001 | ||
| Subcutaneous | 244 (60.5) | 5 (2.8) | |
| Simple | 159 (39.5) | 175 (97.2) |
Categories are not mutually exclusive since patients could state more than one reason for electing CPM.
CPM – contralateral prophylactic mastectomy
Satisfaction and QOL at first questionnaire
Choice to have CPM and satisfaction
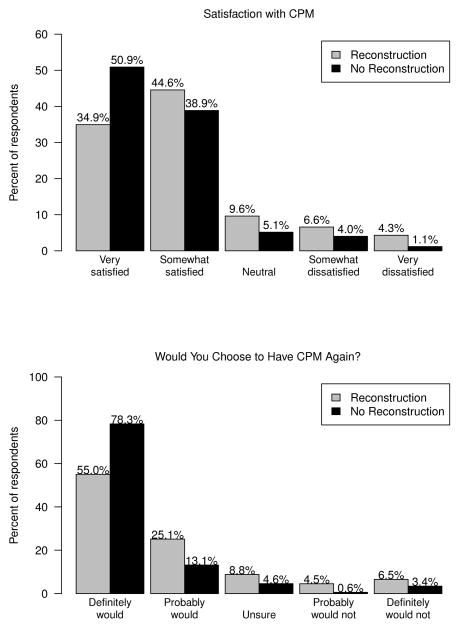
Patients undergoing reconstruction reported significantly lower satisfaction with CPM (p=0.0001) and were significantly less likely to report they would choose CPM again (p<0.0001) (Figure 1A–1B). Despite these differences, the majority of patients in both groups reported being satisfied or very satisfied (79% and 90% for reconstruction and no reconstruction, respectively) and reported that they definitely or probably would choose CPM again (80% and 91%, respectively).
Figure 1.
Figures 1a and 1b. Questionnaire responses regarding patient satisfaction with CPM (Fig 1a) and whether they would choose to have CPM again (Fig 1b) comparing those with and without reconstruction
Choice to have reconstruction
When asked whether patients would choose to have reconstruction if given the choice again, responses were strongly associated with their original decision, with 71% and 78% in the reconstruction and no reconstruction groups, respectively, answering in concordance with their original choice. Among those who had undergone reconstruction, 17% responded that they probably or definitely would not choose reconstruction again, while 13% of those who had not undergone reconstruction said they would choose reconstruction if given the option again (p=0.25). The remaining 12% in the reconstruction group and 9% in the no reconstruction group were unsure whether they would choose reconstruction if given the choice again.
Reoperations
Unplanned reoperation was more common in patients undergoing reconstruction than those not undergoing reconstruction (Table 2). Of the 403 patients in the reconstruction group, 157 (39%) required one or more unplanned reoperations on the CPM side during follow-up compared to only 10/180 (6%) among the no reconstruction group (p<0.0001). Among those with reoperation in the reconstruction group, the mean number of reoperations was 1.4 (range 1–4).
Table 2.
Unplanned reoperations by reconstruction
| Reconstruction N = 403 | No Reconstruction N = 180 | p-value | |
|---|---|---|---|
| Any reoperation, n (%) | <0.0001 | ||
| Yes | 157 (39.0) | 10 (5.6) | |
| No | 246 (61.0) | 170 (94.4) | |
| Number of reoperations, n (%) | <0.0001 | ||
| 0 | 246 (61.0) | 170 (94.4) | |
| 1 | 118 (29.3) | 9 (5.0) | |
| 2 | 24 (6.0) | 1 (0.6) | |
| 3 | 12 (3.0) | 0 | |
| 4 | 3 (0.7) | 0 | |
| Indication(s) for reoperation*, n (%) | |||
| Implant related issues | 152 (71.0) | 0 | |
| Postoperative complications | 34 (15.9) | 1 (9.1) | |
| Aesthetic concerns (non-implant related) | 64 (29.9) | 3 (27.3) | |
| Nodule removal | 25 (11.7) | 7 (63.6) | |
| Other | 9 (4.2) | 0 | |
For 214 reoperations in Reconstruction group and 11 reoperations in No Reconstruction group. Many had more than one indication for reoperation so categories do not sum to one hundred percent.
There were a total of 225 unplanned reoperations (214 in the reconstruction group, 11 in the no reconstruction group) during follow-up (Table 2). Implant related concerns were the most common indication (71%) in the reconstruction group with non-implant related aesthetic concerns as the distant second most common indication (30%). Postoperative complications were the indication for 34 (16%) of the reoperations. In the no reconstruction group, nodule removal (64%) was the most common indication for reoperation.
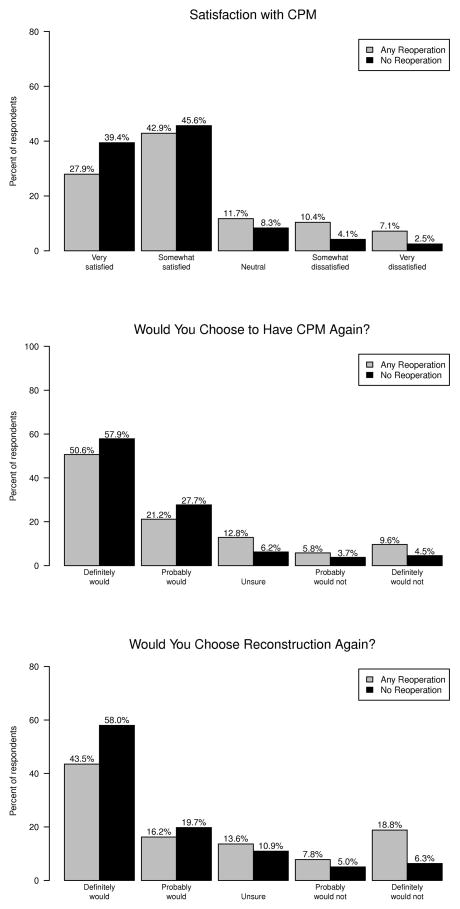
In the reconstruction group, reoperation was significantly associated with patient responses to questions regarding satisfaction with CPM (p=0.0001), choice to have CPM again (p=0.006), and choice to have reconstruction again (p<0.0001) with poorer scores in those who required one or more unplanned reoperation (Figures 2A–2C). Each of these differences remained statistically significant after adjusting for age at CPM, length of follow-up and marital status in multivariate analysis.
Figure 2.
Figures 2a–2c. Questionnaire responses regarding patient satisfaction with CPM (Fig 2a), whether they would choose to have CPM again (Fig 2b) and whether they would choose reconstruction again (Fig 2c) comparing those with and without any reoperation
Open-ended responses regarding choice of reconstruction
Patients were asked to explain the reason(s) for their responses regarding whether they would choose to have reconstruction again. In reconstruction patients who reported that they would not choose reconstruction again, 85% indicated that their reason was related to adverse symptoms or complications, 22% cited adverse body image effects including dissatisfaction with the cosmetic results, 15% cited concerns about the safety of silicone implants, and 13% described insufficient information or support, including lack of information about possible complications. Conversely, reconstruction patients who would choose reconstruction again most commonly cited positive effects to body image (94%) including improved self-esteem or self-concept.
Body image was also the most common reason cited (57%) in women who did not have reconstruction but said they would choose reconstruction if they could now. Women in the no reconstruction group who said they would still opt for no reconstruction frequently said they were comfortable with their body without reconstruction (42%) and cited a desire to avoid reconstruction complications (24%) and concerns regarding the safety of silicone implants (23%).
Satisfaction and QOL at second questionnaire
At the time of the second follow-up survey 96 women had died, leaving 487 to be surveyed. Survey response rate was 55% with 269 surveys returned at a mean of 20.2 years and median of 18.4 years (range 11.4 – 44.5 years) after CPM. Of 269 respondents, 210 (78%) had undergone reconstruction and 59 (22%) had not.
With longer follow-up, results for the questions regarding satisfaction with CPM, choice to have CPM, and choice to have reconstruction were largely consistent with generally positive scores for both groups but still a significant difference between the two groups regarding satisfaction. Among reconstruction patients, 89% reported being very or somewhat satisfied compared to 95% in the no reconstruction group (p=0.03). The vast majority of patients in both groups said they would choose CPM again (92% and 93%, respectively, p=0.10).
Regarding choice to have reconstruction, a smaller percentage of women at 20 years compared to at 10 years said they would change their decision. At 20 years, 10% of reconstruction patients and 16% of no reconstruction patients (p=0.16) said they would change their decision.
Psychosocial impact of CPM
Reconstruction was significantly associated with positive feelings regarding self-esteem (p=0.0002), body appearance (p=0.0005), and femininity (p=0.002) on the first follow-up survey (Table 3). Reconstruction patients were more likely to report that CPM had increased self-esteem, satisfaction with body appearance, and feelings of femininity. Those without reconstruction were more likely to report no change, and the percent of respondents reporting that CPM had diminished these aspects did not differ significantly between the groups. After adjusting for age at survey, marital status, and length of follow-up, each of the psychosocial aspects of self-esteem (p=0.0002), body appearance (p=0.0007), and femininity (p=0.0002) remained significantly improved for reconstruction compared to no reconstruction patients. The difference between groups also became significant for sexual relationships (p=0.03) after multivariate adjustment.
Table 3.
Comparing self-reported psychosocial aspects of CPM between patients with and without reconstruction.
| First survey | Second survey | |||||
|---|---|---|---|---|---|---|
| Reconstruction N = 403 | No Reconstruction N = 180 | p-value* | Reconstruction N = 210 | No Reconstruction N = 59 | p-value* | |
| Self esteem | ||||||
| Decreased | 67 (17.0) | 32 (18.5) | 0.0002 | 19 (9.4) | 7 (12.5) | 0.11 |
| No Change | 201 (51.1) | 120 (69.4) | 132 (65.0) | 40 (71.4) | ||
| Increased | 125 (31.8) | 21 (12.1) | 52 (25.6) | 9 (16.1) | ||
| Unanswered | 10 | 7 | 7 | 3 | ||
| Satisfaction with Body Appearance | ||||||
| Decreased | 123 (31.5) | 64 (37.9) | 0.0005 | 60 (29.4) | 19 (33.9) | 0.01 |
| No Change | 141 (36.1) | 82 (48.5) | 89 (43.6) | 34 (60.7) | ||
| Increased | 127 (32.5) | 23 (13.6) | 55 (27.0) | 3 (5.4) | ||
| Unanswered | 12 | 11 | 6 | 3 | ||
| Femininity | ||||||
| Decreased | 100 (25.6) | 44 (26.0) | 0.002 | 51 (24.9) | 11 (20.0) | 0.68 |
| No Change | 201 (51.5) | 118 (69.8) | 121 (59.0) | 40 (72.7) | ||
| Increased | 89 (22.8) | 7 (4.1) | 33 (16.1) | 4 (7.3) | ||
| Unanswered | 13 | 11 | 5 | 4 | ||
| Sexual Relationships | ||||||
| Decreased | 93 (24.3) | 35 (21.3) | 0.47 | 47 (23.5) | 10 (18.2) | 0.73 |
| No Change | 256 (67.0) | 126 (76.8) | 138 (69.0) | 42 (76.4) | ||
| Increased | 33 (8.6) | 3 (1.8) | 15 (7.5) | 3 (5.5) | ||
| Unanswered | 21 | 16 | 10 | 4 | ||
| Emotional Stability | ||||||
| Decreased | 47 (12.1) | 18 (10.7) | 0.10 | 15 (7.3) | 4 (7.0) | 0.98 |
| No Change | 241 (62.0) | 122 (72.6) | 142 (68.9) | 39 (68.4) | ||
| Increased | 101 (26.0) | 28 (16.7) | 49 (23.8) | 14 (24.6) | ||
| Unanswered | 14 | 12 | 4 | 2 | ||
P-value calculated using a Wilcoxon rank-sum test for the original 5-level response variable. Categories have been collapsed to three levels in reporting descriptive statistics for conciseness.
Results on the second follow-up survey were largely consistent with the first (Table 3) although the percentage reporting an improvement in these psychosocial aspects was generally lower than on the first survey and the no change category generally captured a larger percentage of respondents than on the first survey. In comparing reconstruction and no reconstruction patients, only satisfaction with body appearance remained significantly higher for reconstruction than no reconstruction patients (p=0.01).
Discussion
As rates of CPM are increasing across the US, it is important for patients and physicians to understand the long-term psychosocial consequences as this may help guide decision making. Overall the vast majority of women were happy with the decision to undergo CPM. This is reassuring information for women contemplating this option. However, satisfaction with CPM was higher in those choosing not to have reconstruction than those with reconstruction. The majority of women who underwent reconstruction were satisfied with the choice for CPM, however patients with reconstruction were less likely to choose CPM again. Unplanned reoperation is a dissatisfier for patients as well as physicians, and the increased reoperation rate seen in patients undergoing reconstruction was associated with lower satisfaction in our study.
Questionnaires regarding satisfaction with surgical decision making are open to bias, as many individuals when completing a questionnaire and reflecting on previous decisions they have made may tend to deny regret and prefer to believe they agree with their life choices. Acknowledging this limitation, we did observe a statistically significant difference between those women electing reconstruction and those that did not in terms of satisfaction with CPM decision and women did report areas of dissatisfaction, such as with body appearance and sense of femininity. The open ended answers elucidating the rationale for their satisfaction/dissatisfaction noted both favorable and negative aspects, indicating that patients were weighing the trade-offs involved.
One of the strengths of this study is the long-term follow up of these patients and the ability to assess satisfaction approximately 20 years after CPM. However, this also means that patient counseling as well as mastectomy techniques and reconstructive techniques have changed over time. There is a greater awareness of the option of bilateral mastectomy for women diagnosed with breast cancer, through friends, family, media and the internet. In the timeframe of this study most CPMs were subcutaneous mastectomies, whereas currently skin-sparing and nipple-sparing mastectomies are employed for most of these cases. Current reconstructive techniques increasingly allow single stage implant based reconstruction, which decreases the number of operations and recovery time for women undergoing immediate implant reconstruction.(24,25,26) It is likely that part of the increase in CPM rates across the country is driven by wider spread availability of immediate reconstruction as well as improvements in reconstructive techniques.
Interestingly and importantly, the majority of women who did not elect reconstruction during the time of this study would still make the same decision 20 years later despite all the advances in reconstructive options. This reinforces that the decision to pursue reconstruction or not is a personal choice and that many women who elect not to pursue the option of reconstruction remain comfortable with their choice for years to come.
Body image and complications related to surgery were the two main drivers for satisfaction or dissatisfaction with choice for or against reconstruction. CPM had significant psychosocial impact on self-esteem, satisfaction with body appearance, sexual relationships and feelings of femininity for up to a third of the patients. Patients without reconstruction were more likely to report no change in these factors, demonstrating that women were able to resume normal lives after CPM without reconstruction. Patients with reconstruction reported an increase in these factors. One can hypothesize that this may be due to improved cosmetic outcome from reconstruction due to a change in size (augmentation or reduction) or a lift of the breast. Another limitation is that this study focuses almost exclusively on implant reconstruction. Long-term satisfaction and need for reoperations may be different with autologous reconstruction and this warrants further investigation.
With an average of 20 years of follow up, over 92% of women would choose CPM again. In patients who undergo CPM, many years after surgery satisfaction with CPM is higher in those choosing not to have reconstruction than those with reconstruction although it was high in both groups. Unplanned reoperation was common after reconstruction and was associated with lower satisfaction. Current techniques that allow single stage reconstruction are important to improve long-term satisfaction with PM and reconstruction. Counseling patients regarding options and anticipated long-term course regarding number of operations and psychosocial consequences remains important. Reoperation is a major dissatisfier for patients and decreasing reoperation rates is likely to improve long-term satisfaction. This highlights the importance of patient education regarding the benefits and risks of breast reconstruction following CPM.
Footnotes
Manuscript has not been published nor is it being considered for publication elsewhere
Disclaimer: There are no financial disclosures or potential conflicts of interest
References
- 1.McDonnell SK, Schaid DJ, Myers JL, Grant CS, Donohue JH, Woods JE, et al. Efficacy of contralateral prophylactic mastectomy in women with a personal and family history of breast cancer. J Clin Oncol. 2001;19:3938–43. doi: 10.1200/JCO.2001.19.19.3938. [DOI] [PubMed] [Google Scholar]
- 2.Rebbeck TR, Friebel T, Lynch HT, Neuhausen SL, van’t Veer L, Garber JE, et al. Bilateral prophylactic mastectomy reduces breast cancer risk in BRCA1 and BRCA2 mutation carriers: the PROSE Study Group. J Clin Oncol. 2004;22:1055–62. doi: 10.1200/JCO.2004.04.188. [DOI] [PubMed] [Google Scholar]
- 3.Peralta EA, Ellenhorn JD, Wagman LD, Dagis A, Andersen JS, Chu DZ. Contralateral prophylactic mastectomy improves the outcome of selected patients undergoing mastectomy for breast cancer. Am J Surg. 2000;180:439–45. doi: 10.1016/s0002-9610(00)00505-5. [DOI] [PubMed] [Google Scholar]
- 4.Herrinton LJ, Barlow WE, Yu O, Greiger AM, Elmore JG, Barton MB, et al. Efficacy of prophylactic mastectomy in women with unilateral breast cancer: a cancer research network project. J Clin Oncol. 2005;23:4275–86. doi: 10.1200/JCO.2005.10.080. [DOI] [PubMed] [Google Scholar]
- 5.van Sprundel TC, Schmidt MK, Rookus MA, Brohet R, van Asperen CJ, Rutgers EJ, et al. Risk reduction of contralateral breast cancer and survival after contralateral prophylactic mastectomy in BRCA1 or BRCA2 mutation carriers. Br J Cancer. 2005;93:287–92. doi: 10.1038/sj.bjc.6602703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tuttle TM, Habermann EB, Grund EH, Morris TJ, Virnig BA. Increasing use of contralateral prophylactic mastectomy for breast cancer patients: a trend toward more aggressive surgical treatment. J Clin Oncol. 2007;25:5203–9. doi: 10.1200/JCO.2007.12.3141. [DOI] [PubMed] [Google Scholar]
- 7.Tuttle TM, Jarosek S, Habermann EB, Arrington A, Abraham A, Morris TJ, et al. Increasing rates of contralateral prophylactic mastectomy among patients with ductal carcinoma in situ. J Clin Oncol. 2009;27:1362–7. doi: 10.1200/JCO.2008.20.1681. [DOI] [PubMed] [Google Scholar]
- 8.Boughey JC, Hoskin TL, Degnim AC, Sellers TA, Johnson JL, Kasner MJ, et al. Contralateral prophylactic mastectomy is associated with a survival advantage in high-risk women with a personal history of breast cancer. Ann Surg Oncol. 2010;17:2702–9. doi: 10.1245/s10434-010-1136-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bedrosian I, Hu CY, Chang GJ. Population-based study of contralateral prophylactic mastectomy and survival outcomes of breast cancer patients. J Natl Cancer Inst. 2010;102:401–9. doi: 10.1093/jnci/djq018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lostumbo L, Carbine NE, Wallace J. Prophylactic mastectomy for the prevention of breast cancer. Cochrane Database Syst Rev. 2010;(11):CD002748. doi: 10.1002/14651858.CD002748.pub3. [DOI] [PubMed] [Google Scholar]
- 11.Frost MH, Slezak JM, Tran NV, Williams CI, Johnson JL, Woods JE, et al. Satisfaction after contralateral prophylactic mastectomy: the significance of mastectomy type, reconstructive complications, and body appearance. J Clin Oncol. 2005;23:7849–56. doi: 10.1200/JCO.2005.09.233. [DOI] [PubMed] [Google Scholar]
- 12.Yi M, Hunt KK, Arun BK, Bedrosian I, Barrera AG, Do KA, et al. Factors affecting the decision of breast cancer patients to undergo contralateral prophylactic mastectomy. Cancer Prev Res (Phila Pa) 2010;3:1026–34. doi: 10.1158/1940-6207.CAPR-09-0130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jones NB, Wilson J, Kotur L, Stephens J, Farrar WB, Agnese DM. Contralateral prophylactic mastectomy for unilateral breast cancer: an increasing trend at a single institution. Ann Surg Oncol. 2009;16:2691–6. doi: 10.1245/s10434-009-0547-9. [DOI] [PubMed] [Google Scholar]
- 14.Arrington AK, Jarosek SL, Virnig BA, Habermann EB, Tuttle TM. Patient and surgeon characteristics associated with increased use of contralateral prophylactic mastectomy in patients with breast cancer. Ann Surg Oncol. 2009;16:2697–704. doi: 10.1245/s10434-009-0641-z. [DOI] [PubMed] [Google Scholar]
- 15.King TA, Sakr R, Patil S, Gurevich I, Stempel M, Sampson M, et al. Clinical management factors contribute to the decision for contralateral prophylactic mastectomy. J Clin Oncol. 2011;29:2158–64. doi: 10.1200/JCO.2010.29.4041. [DOI] [PubMed] [Google Scholar]
- 16.Frost MH, Hoskin TL, Hartmann LC, Degnim AC, Johnson JL, Boughey JC. Contralateral prophylactic mastectomy: long-term consistency of satisfaction and adverse effects and the significance of informed decision-making, quality of life, and personality traits. Ann Surg Oncol. 2011;18:3110–6. doi: 10.1245/s10434-011-1917-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hawley ST, Jagsi R, Morrow M, Janz NK, Hamilton A, Graff JJ, Katz SJ. Social and clinical determinants of contralateral prophylactic mastectomy. JAMA Surg. doi: 10.1001/jamasurg.2013.5689. Published online May 21, 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Stefanek M, Hartmann L, Nelson W. Risk-reduction mastectomy: clinical issues and research needs. J Natl Cancer Inst. 2001;93:1297–306. doi: 10.1093/jnci/93.17.1297. [DOI] [PubMed] [Google Scholar]
- 19.Goldflam K, Hunt KK, Gershenwald JE, Singletary SE, Mirza N, Kuerer HM, et al. Contralateral prophylactic mastectomy. Predictors of significant histologic findings. Cancer. 2004;101:1977–86. doi: 10.1002/cncr.20617. [DOI] [PubMed] [Google Scholar]
- 20.Osman F, Saleh F, Jackson TD, Corrigan MA, Cil T. Increased postoperative complications in bilateral mastectomy patients compared to unilateral mastectomy: An analysis of the NSQIP database. Ann Surg Oncol. 2013;20:3212–7. doi: 10.1245/s10434-013-3116-1. [DOI] [PubMed] [Google Scholar]
- 21.Zion SM, Slezak JM, Sellers TA, Woods JE, Arnold PG, Petty PM, et al. Reoperations after prophylactic mastectomy with or without implant reconstruction. Cancer. 2003;98:2152–60. doi: 10.1002/cncr.11757. [DOI] [PubMed] [Google Scholar]
- 22.Gabriel SE, Woods JE, O’Fallon WM, Beard CM, Kurland LT, Melton LJ., 3rd Complications leading to surgery after breast implantation. N Engl J Med. 1997;336:677–82. doi: 10.1056/NEJM199703063361001. [DOI] [PubMed] [Google Scholar]
- 23.Crosby MA, Card A, Liu J, Lindstrom WA, Chang DW. Immediate breast reconstruction and lymphedema incidence. Plast Reconstr Surg. 2012;129:789e–95e. doi: 10.1097/PRS.0b013e31824a2ab1. [DOI] [PubMed] [Google Scholar]
- 24.Cassileth L, Kohanzadeh S, Amersi F. One-stage immediate breast reconstruction with implants: a new option for immediate reconstruction. Ann Plast Surg. 2012;69:134–8. doi: 10.1097/SAP.0b013e3182250c60. [DOI] [PubMed] [Google Scholar]
- 25.Topol BM, Dalton EF, Ponn T, Campbell CJ. Immediate single-stage breast reconstruction using implants and human acellular dermal tissue matrix with adjustment of the lower pole of the breast to reduce unwanted lift. Ann Plast Surg. 2008;61:494–9. doi: 10.1097/SAP.0b013e31816d82d9. [DOI] [PubMed] [Google Scholar]
- 26.Salzberg CA. Nonexpansive immediate breast reconstruction using human acellular tissue matrix graft (AlloDerm) Ann Plast Surg. 2006;57:1–5. doi: 10.1097/01.sap.0000214873.13102.9f. [DOI] [PubMed] [Google Scholar]