Abstract
Objectives
Underlying heterogeneity among individuals with cocaine dependence is widely postulated in the literature, however, identification of a group of factors that explain risk of cocaine use severity has yet to be confirmed.
Methods
Latent mixture modeling evaluated 338 cocaine-dependent individuals recruited from the community to assess the evidence for the presence of distinct subgroups. Variables included 5 baseline questionnaires measuring cognitive function (Shipley), impulsivity (BIS), mood (BDI), affective lability (ALS), and addiction severity (ASI). Results failed to suggest multiple subgroups. Given a lack of evidence for discrete latent classes, an exploratory factor analysis (EFA) followed by exploratory structural equation modeling (ESEM) was implemented to identify functional dimensions to enhance interpretation of these variables.
Results
Findings from the EFA indicated a 3-factor model as the best fit, and the subsequent ESEM solution resulted in associations with lifetime cocaine use. Factor 1, best characterized by demographic factors (gender, age), is associated with less lifetime cocaine use. Psychological problems best characterize factor 2, which is associated with higher lifetime cocaine use. Finally, factor 3 is characterized by other substance use (alcohol and marijuana). Although this factor did not demonstrate a statistically reliable relation with self-reported, lifetime cocaine use, it did indicate a potentially meaningful positive association.
Conclusions
These 3 factors delineate dimensions of functioning that likewise help characterize the variability found in previously established associations with self-reported cocaine use.
1. Introduction
The pharmacological and behavioral effects of cocaine have been well described in humans; a complex array of factors that contribute to the onset and maintenance of cocaine addiction. Many other factors such as genes, environment, and stress may play a role in substance use disorders, with little consensus regarding specific factors associated with drug use severity or long-term outcome [1]. Heterogeneity among this population likely contributes to inconsistent and ineffective results in treatment and high rates (>50%) of relapse in cocaine dependent individuals [2]. Characterizing the association between demographic and psychological variables and cocaine use may illuminate participants' vulnerability to, and maintenance of, cocaine addiction.
Examination of sex differences in cocaine use disorders have produced mixed findings: reports of higher prevalence of cocaine use in men than women [3] as well as a failure to find differences in cocaine use between men and women [4]. Further, among young adults there is evidence for higher rates of cocaine dependence in females [5]. Cocaine dependence commonly occurs with other substance use disorders (SUDs) with alcohol, cannabis, or nicotine dependence prevalent among cocaine users [6-8]. In addition, reports have indicated high rates of comorbidity with depression, stress and attention deficit disorders, as well as childhood psychological trauma among cocaine dependent individuals, which may be associated with increased severity of the disorder [9,10]. Other large scale analyses evaluating severity of cocaine dependence using self-report baseline measures found that substance use disorder comorbidities consistently correlated with severity of cocaine dependence, and psychiatric comorbidity was associated with increased severity of cocaine use during the heaviest period of use [11,12]. Although these studies have established a wide array of characteristics that describe the cocaine dependent population, more detailed characterization of factors that influence cocaine use will eventually result in establishing a credible profile of risk and protective factors for estimating the probability of cocaine use.
To that end, this exploratory study employed latent class and structural equation modeling to examine patterns of covariation between cocaine use and relevant variables gathered from a large population of cocaine dependent subjects. These analytic models were implemented to identify multivariate patterns among these variables and determine their association with cocaine use. Measured variables included: cognitive and affective function, demographics, and patterns of others illicit drug and alcohol use. The goal was to characterize heterogeneity among cocaine dependent participants using latent variable modeling, and estimate the relationships between identified subgroups and/or functional profiles/dimensions, and self-reported cocaine use both in the preceding 30 days and over the participant's lifetime.
2. Materials and Methods
2.1 Subjects
All participants signed an informed consent that was reviewed and approved by the Committee for the Protection of Human Subjects at The University of Texas Health Science Center at Houston. Subjects took part in a one-week intake evaluation process to determine study eligibility, which included a physical examination, laboratory work-up, and a structured clinical interview for DSM-IV (SCID-1) diagnoses [13]. Participants were admitted to behavioral and pharmacological treatment and non-treatment studies for cocaine dependence. Subjects were cocaine-dependent, English-speaking, between the ages of 18 and 60, and competent to give informed consent. All subjects provided a urine sample, which was tested for cocaine (benzoylegonine), tetrahydrocannabinol, opiates, amphetamine, methamphetamine, and benzodiazepines on each visit to the laboratory. All subjects displayed at least one cocaine-positive urine during screening. Participants were recruited from the greater Houston area using multiple advertising strategies, including newspaper articles, public service announcements, professional networks, and posters located throughout the community. Individuals were excluded if they met diagnostic criteria for current DSM-IV substance dependence other than cocaine (except nicotine and cannabis) or other Axis I disorders, used psychotropic medications, or experienced unstable or serious medical illnesses that affected the CNS or cardiovascular function.
The total sample, N = 338, had a mean age of 44 years (SD = 8.60). Data for this analysis were obtained from a database with subjects enrolled between 2008-2012. Inclusion was based on DSM-IV cocaine dependence and intake questionnaires including the Addiction Severity Index (ASI) [14], Shipley (scale of cognitive functioning) [15], Beck Depression Inventory (BDI) [16], BIS Barrett Impulsiveness Scale (BIS) [17], and Affective Lability Scale (ALS) [18]. Twenty-two subjects were dropped due to lack of completion of any questionnaire other than the Shipley.
All subjects were assessed at baseline, prior to the start of any medication or therapy. Participants seeking treatment for cocaine use comprised 92.2% of the sample, with the remainder enrolled in non-treatment studies. Within the population of treatment seeking participants, the majorities were African American (75.9%), male (77.4%), and unemployed (32.7%) with a mean age of 43.9 years (SD = 8.8) and mean education level of 12.2 years (SD = 1.9). Mean reported use of cocaine in the 30 days prior to treatment was 13.5 days (SD = 9.27). Mean number of years of reported use of cocaine in the subjects' lifetime prior to intake was 13.6 years (SD = 7.46). The majority of subjects (79.8%) reported smoking cocaine as their primary route of administration, and 63.8% previously participated in drug abuse treatment.
Within the population of non-treatment seeking participants, the majority were African American (70.8%), male (71.4%), and unemployed (41.7%) with a mean age of 39.4 years (SD = 9.3) and mean education level of 12.9 years (SD = 1.9). Mean number of days of reported use of cocaine in the preceding 30 days prior to intake was 10.7 days (SD = 9.74). Mean number of years of reported use of cocaine in the subjects' lifetime prior to intake was 9.0 years (SD = 7.17). The majority of subjects (69.6%) reported smoking cocaine as their primary route of administration, and 62.5% previously participated in drug abuse treatment.
2.2 Questionnaires
2.2.1 Addiction Severity Index (ASI)
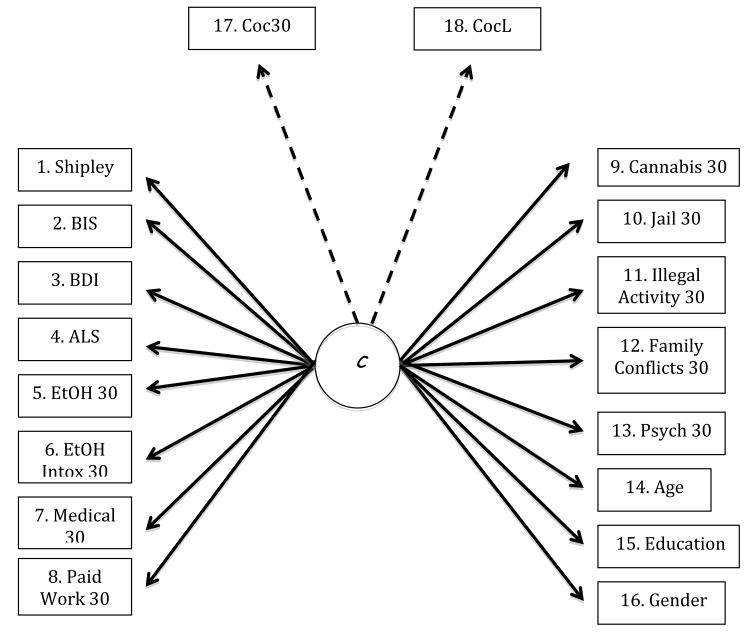
The ASI is a semi-structured interview that addresses seven problem areas in individuals with substance abuse: drug use, alcohol use, legal status, medical status, employment and support, family/social status, and psychiatric status [14]. Nine subjective responses were selected from the ASI that captured salient information on participant function in the past 30 days (Figure 1): Days of any alcohol use (EtOH 30), Days of alcohol to intoxication (EtOH Intox 30), Days of cocaine use (Coc30), Days experienced medical problems (Medical 30), Days paid for work (Paid Work 30), Days of Cannabis Use (Cannabis 30), Days detained or incarcerated (Jail 30), Days engaged in illegal activities for profit (Illegal Activity 30), Serious conflict with family (Family Conflicts 30), and Number of psychiatric problems (Psych 30). The number of lifetime years of cocaine (CocL) was also included in the analyses.
Figure 1. Path Diagram of Questionnaire Factor Model.
1. Shipley Total Score
2. Barratt Impulsiveness Scale (BIS) Total Score
3. Beck Depression Inventory (BDI) Total Score
4. Affective Lability Scale (ALS) Total Score
5. Days of any alcohol use in past 30days
6. Days of alcohol to intoxication in past 30 days
7. Days experienced medical problems in the last 30
8. Days paid for working in the past 30 days
9. Cannabis Use in past 30 days
10. Days in the past 30 you were detained or incarcerated
11. Days in the past 30 you have engaged in illegal activities for profit
12. Serious conflicts with family in past 30 days (0=None; 1=Yes)
13. # Psychiatric problems during the past 30 days 0=None; 1=At least 1 problem [Depression, Anxiety, Hallucinations; Trouble Concentrating, Violent Behavior; Thoughts of Suicide; Attempted Suicide]
14. Age (years)
15. Education (years)
16. Gender
17. Cocaine use in the past 30 days
18. Cocaine use in lifetime (years)
Violation of distributional assumptions required dichotomizing the following variables: Jail 30, Illegal Activity 30, Family Conflicts 30, and Psych 30 into 0-15 days and 16-30 days. Likewise distributions required trichotomizing the variables: EtOH 30, EtOH Intox 30, Medical 30, Paid Work 30, and Cannabis 30 into 1-6 days, 7-15 days, and 16-30 days.
2.2.2. Shipley
To obtain a standardized measure of cognitive ability, two components of the Shipley were tested, crystallized knowledge and logical reasoning, which are reflected by Shipley verbal and abstract/block scores respectively. [15] Scores from both the Shipley I and II were included in this data set, however, scoring ranges were different for each version. In order to establish a uniform standardized metric for this analysis, a z score was calculated for the Shipley I and Shipley II separately, which accounted for both verbal and block scores (total score). Then, all of the Shipley scores were combined under one variable.
2.2.3 Beck Depression Inventory (BDI)
One of the most commonly used self-report methods for measuring depression, the BDI shows high reliability and good correlation with measures of depression and anxiety [16]. The log transform of the total score was used for the analysis to render this distribution normal.
2.2.4 Barrett Impulsiveness Scales (BIS)
This is a widely used 30-item self-report measure of impulsive traits. Cocaine-dependent subjects have a well-established history of elevated impulsivity related to chronic drug use. The BIS consists of three subscales (attentional, motor, and non-planning impulsiveness) and a total score [17] however, the Total BIS Score was used in the current analysis.
2.2.5 Affective Lability Scale (ALS)
This 54-question self-report questionnaire, with items rated from 0-3, is divided into six sections that examine a range of affective states. The first four scales (depression, elation, anxiety, and anger) measure changeability between those mood states and euthymic (normal) mood. The other two scales (depression-elation and depression-anger) measure changeability between the two mood states [18]. The total score, which is the sum of all the question's scores divided by 54, was used in the analysis.
2.3 Statistical Analyses
We examined the heterogeneity of the baseline questionnaire data in order to characterize the data. All analyses were completed with SEM software MPlus 7 [19]. Initially, the analysis began with a latent variable mixture model to identify potential subgroups as characterized by multivariate profiles of the observed variables [20]. Inspection of solutions for 1-4 classes used Bayesian information criterion (BIC), bootstrap likelihood ratio testing, Vuong-Lo-Mendell-Rubin (VLMR) likelihood ratio testing, entropy and, ultimately, the interpretability of any resulting multivariate profiles. [21] Examination of these indices suggested that any putative groups reflected continuous quantitative variation of multivariate profiles rather than discrete, qualitatively distinct classes. No clear delineations between the variables established coherent multivariate profiles for any number of classes, suggesting this approach was not optimal.
Next, an exploratory factor model (Figure 1) was implemented to identify a set of underlying latent constructs that might characterize the sample as a whole. Fit indices used in identifying the best factor solution included: Root mean square error of approximation (RMSEA), the Tucker Lewis index (TLI), and the Comparative Fit Index (CFI) [22-24] The majority of the variables in the dataset were categorical, however, age, education, Shipley, BIS, BDI, and ALS were continuous. The WLSMV estimator in MPlus was utilized to define an optimal factor solution. Fit indices suggested a 3-factor solution was the most parsimonious model. Subsequently, an Exploratory Structural Equation Model (ESEM) regressed lifetime cocaine use (years) and cocaine use in the past 30 days, on the obtained factors.
3. Results
3.1 Latent Class Analysis
A latent class analysis (LCA) partitions individuals into subgroups based on their multivariate profiles [25]. Examination of the fit statistics for the LCA for 2 through 4-class models (Table 1) failed to identify distinct class profiles. Fit indices failed to present a coherent picture that delineated subgroups: all classes appeared to be a variation on the same continuous dimension. This suggested that characterization of the entire sample in terms quantitative dimensions might be more informative, prompting the use of exploratory factory analysis.
Table 1. Latent Class Analysis (LCA) Model Fitting.
| Model | BIC | VLMR | VLMR p-value | Entropy |
|---|---|---|---|---|
| 2 class | 13168.47 | -6552.51 | 0.00 | 0.81 |
| 3 class | 13141.89 | -6428.25 | 0.00 | 0.80 |
| 4 class | 13170.00 | -6343.98 | 0.00 | 0.78 |
(BIC: Baysian Information Criteria; VLMR: Vuong-Lo-Mendell-Rubin Fit Criteria)
3.2 Exploratory Factor Analysis and ESEM
Exploratory factor analysis remains a well-established technique for multivariate analysis [26]. This analysis implemented an EFA by clustering 16 observed variables from the data set into corresponding factors. The estimator, WLSMV, was the best method for this sample [27]. EFA evaluated factor solutions with one through seven dimensions. Extraction of factors used inspection of the resulting scree plot followed by evaluation of the chi-square test of model fit, degrees of freedom, 90% confidence interval, RMSEA, CFI, and TLI (Table 2). After inspection of all fit statistics for each solution, the model favored the 3-factor solution.
Table 2. Exploratory Factor Analysis (EFA) Model Fitting.
| Factors | Chi-square | Chi p-value | Degrees of Freedom | RMSEA | 90% CI | 90% CI | CFI | TLI |
|---|---|---|---|---|---|---|---|---|
| 1 | 391.13 | 0.00 | 135.00 | 0.08 | 0.07 | 0.08 | 0.69 | 0.65 |
| 2 | 262.19 | 0.00 | 118.00 | 0.06 | 0.05 | 0.07 | 0.83 | 0.77 |
| 3 | 176.46 | 0.00 | 102.00 | 0.05 | 0.35 | 0.06 | 0.91 | 0.87 |
| 4 | 134.17 | 0.00 | 87.00 | 0.04 | 0.03 | 0.05 | 0.94 | 0.90 |
| 5 | 113.97 | 0.00 | 73.00 | 0.04 | 0.03 | 0.06 | 0.95 | 0.90 |
| 6 | 88.07 | 0.01 | 60.00 | 0.04 | 0.02 | 0.05 | 0.97 | 0.91 |
(RMSEA: Root mean square error of approximation; 90% CI: 90% Confidence Interval; CFI: Comparative fit index; TLI: Tucker-Lewis index)
Standardized Rotated loadings for Factor 1 (Table 3a) indicated an association of higher factor scores with increased probability of female gender, cannabis use, incarceration time, family conflict, decreased age and education. This factor was associated with lower levels of self-reported lifetime cocaine use. Based on the standardized weights, the variables age and gender carried the most weight resulting in be labeling Factor 1 as demographic.
Table 3. ESEM Standardized Rotated Factor Loadings.
| (a) | F1 | Estimate | p-value |
| Gender | 0.420 | 0.000 | |
| Cannabis 30 | 0.225 | 0.008 | |
| Jail 30 | 0.425 | 0.046 | |
| Family Conflicts 30 | 0.251 | 0.015 | |
| Age | -0.613 | 0.000 | |
| Education | -0.350 | 0.000 | |
| (b) | F2 | Estimate | p-value |
| Medical 30 | 0.316 | 0.004 | |
| Illegal Activity 30 | 0.294 | 0.020 | |
| Family Conflicts 30 | 0.239 | 0.026 | |
| Psych 30 | 0.456 | 0.000 | |
| BIS | 0.661 | 0.000 | |
| BDI | 0.637 | 0.000 | |
| ALS | -0.664 | 0.000 | |
| (c) | F3 | Estimate | p-value |
| EtOH 30 | 0.842 | 0.000 | |
| EtOH Intox 30 | 0.906 | 0.000 | |
| Cannabis 30 | 0.260 | 0.001 | |
| (d) | CocL on | Estimate | p-value |
| F1 | -0.477 | 0.000 | |
| F2 | 0.281 | 0.049 | |
| F3 | 0.055 | 0.424 | |
| Coc30 on | Estimate | p-value | |
| F1 | -0.075 | 0.412 | |
| F2 | 0.078 | 0.359 | |
| F3 | 0.121 | 0.072 |
(F1, F2, F3: Factor 1, 2, & 3 respectively. All variable definitions- refer to Figure 1 Legend)
Standardized rotated loadings for Factor 2 (Table 3b) indicated that higher scores corresponded to higher medical, legal, family and psychological difficulties. Also associated with the highest Factor 2 scores were increased impulsivity and depression coupled with decreased affective lability. Given these standardized weights, this factor may be designated as psychological difficultly, suggesting these variables were a strong predictor of higher cocaine use. The interpretation of the loading from the ALS variable remains inconclusive. Given the lack of utilization of the ALS in the substance use field, and the fact that it was constructed and validated on individuals with personality disorders as well as excluded for substance abuse, its loading on Factor 2 is difficult to interpret [18].
Standardized rotated loadings for Factor 3 (Table 3c) indicate higher scores were associated with higher alcohol use, alcohol use to the point of intoxication, as well as higher cannabis use. The alcohol variables carried the highest weight in this factor and therefore drive interpretability of this factor description as other substance use/abuse. The factor portrays a well-established pattern of concomitant substance use among cocaine-dependent individuals.
Subsequently, an exploratory structural equation model (ESEM) combined the 3-factor solution and two cocaine-use variables (CocL and Coc30) to determine if the observed factors predicted cocaine use (Table 3d). The results indicated an association of less lifetime cocaine use with higher scores on Factor 1 (p≤0.001) and more lifetime cocaine use with increasing scores on Factor 2 (p<0.05). Lower levels of use associated with higher scores on Factor 1 may reflect reduced opportunity for use (i.e. younger age, increased probability of jail in the past thirty days). Factor 3, while not reliably associated with cocaine use in the previous thirty days, or with lifetime use, did demonstrate a potentially clinically meaningful, positive relationship with these variables.
4. Discussion
This study examined cognitive and substance use components from baseline intake questionnaires from cocaine dependent subjects, and evaluated these variables in order to advance understanding of the heterogeneity present in this population. Initially a latent class model was tested, however, it suggested that the data was not well characterized by discrete subgroups. Given that the extracted profiles appeared to form a continuum, application of exploratory factor analysis identified a 3-factor solution as the most parsimonious. Subsequent exploratory structural equation modeling demonstrated associations between Factors 1 and 2 and lifetime cocaine use at baseline and proximal to treatment initiation.
Factor 1 demonstrates a protective relationship with respect to cocaine use: younger, less educated, female have lower levels of recent and lifetime cocaine use. Decreased educational level is likely a correlate of lower age. Younger age, as well as a higher probability of incarceration suggests that Factor 1 may also capture some measure of opportunity. Factor 1's protective benefit is also associated with higher cannabis use. Among individuals presented with the opportunity to use cocaine, those who have only used marijuana in the past are less likely to use other illicit substances unless they had prior exposure to alcohol and tobacco in conjunction with marijuana [28]. Increased family conflict may reflect that individuals scoring higher on this factor might be earlier in chronic abuse, or more involved with their families, that might be reacting negatively to the participant's cocaine use. Another explanation for the loadings on Factor 1 is that lower use of cocaine by these individuals after incarceration could be a direct response to the contingencies of drug monitoring that are imposed by the legal system.
Factor 2 loadings indicate psychological difficulties were predictive of higher lifetime cocaine use. Increased impulsivity and depression exhibit the greatest weights on this factor. Other studies corroborate impulsivity predicting cocaine use as well as shorter retention in clinical studies [29]. High levels of depressive symptoms correlate with a higher craving for cocaine, and therefore a higher risk of relapse risk [30]. It is possible that cocaine is used as a way to improve depressive states, which may follow bouts of binge cocaine use [31]. With regard to the negative association with the ALS, this instrument has not been well established in the substance abuse literature, nor was any association with substance use included during development of this scale. The ALS was primarily created to look at affective instability in personality disorders. The population in the current study is limited only to individuals with substance dependence, in which individuals with other DSM VI Axis I disorders were excluded. Therefore this scale was not created with this population in mind and interpretation of its results are inconclusive.
Although ESEM findings for factor 3 did not significantly predict the positive association with cocaine use, other literature links use of alcohol and marijuana with the abuse of other illegal drugs such as cocaine. Alcohol given prior or simultaneously with cocaine led to greater perception of a cocaine ‘high’, and the intensity and length of the increase in ‘high’ was confirmed by EEG indices of intoxication [32-34]. In addition, subjects who were given the alcohol-cocaine combination produced cocethylene, which may play a role in enhanced autonomic effects and the subsequent increase in subjective ‘high’ perceived by these subjects when using both substances [35,36]. Studies have posited that marijuana use leads to sensitization and therefore increases a neurobiological response within addiction circuitry to other drugs [37]. Furthermore, individuals who more frequently used cannabis (>50times/year) significantly increased their likelihood of onset of other illicit drug use compared to non-users [38]. This enhanced euphoric feeling and increased persistence of use of alcohol and marijuana may provide explanation for this third factor ESEM association of higher cocaine use due to prior comorbid substance use.
Limitations of this study include demographic composition, mostly African-American males, and lack of longitudinal evaluation due to sole administration of these assessments only at baseline. Individuals with a clinical diagnosis of any Axis I disorders were excluded from participation, and therefore limitations of applicability to a more mentally ill patient population remain. All study variables were self-report, which may not give the most accurate portrayal of the severity of cocaine dependence. The absence of prospective longitudinal data limited the potential for causal inference and interpretability for many of these findings. Replication of these factor results is needed, and a more diverse sample of cocaine dependent individuals should be used for optimal generalizability.
References
- 1.Grasing K, Mathur D, Newton TF, et al. Individual predictors of the subjective effects of intravenous cocaine. Psychiatry Res. 2013;208:245–251. doi: 10.1016/j.psychres.2013.05.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Green CE, Moeller FG, Schmitz JM, et al. Evaluation of Heterogeneity in Pharmacotherapy Trials for Drug Dependence: A Bayesian Approach. Am J Drug Alcohol Abuse. 2009;35:95–102. doi: 10.1080/00952990802647503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lev-Ran S, Imtiaz S, Rehm J, et al. Exploring the association between lifetime prevalence of mental illness and transition from substance use to substance use disorders: Results from the National Epidemiologic Survey of Alcohol and Related Conditions (NESARC) The American Journal on Addictions. 2013;22:93–98. doi: 10.1111/j.1521-0391.2013.00304.x. [DOI] [PubMed] [Google Scholar]
- 4.Wagner FA, Anthony JC. Male-female differences in the risk of progression from first use to dependence upon cannabis, cocaine, and alcohol. Drug and Alcohol Dependence. 2007;86:191–198. doi: 10.1016/j.drugalcdep.2006.06.003. [DOI] [PubMed] [Google Scholar]
- 5.Kasperski SJ, Vincent KB, Caldeira KM, et al. College students' use of cocaine: Results from a longitudinal study. Addictive Behaviors. 2011;36:408–411. doi: 10.1016/j.addbeh.2010.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bierut LJ, Strickland JR, Thompson JR, et al. Drug use and dependence in cocaine dependent subjects, community-based individuals, and their siblings. Drug and Alcohol Dependence. 2008;95:14–22. doi: 10.1016/j.drugalcdep.2007.11.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lopez-Quintero C, Pérez de los Cobos J, Hasin DS, et al. Probability and predictors of transition from first use to dependence on nicotine, alcohol, cannabis, and cocaine: Results of the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) Drug and Alcohol Dependence. 2011;115:120–130. doi: 10.1016/j.drugalcdep.2010.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Redner R, White TJ, Harder VS, et al. Vulnerability to Smokeless Tobacco Use Among Those Dependent on Alcohol or Illicit Drugs. Nicotine Tob Res. 2013;16:216–23. doi: 10.1093/ntr/ntt150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sartor CE, Kranzler HR, Gelernter J. Rate of progression from first use to dependence on cocaine or opioids: A cross-substance examination of associated demographic, psychiatric, and childhood risk factors. Addict Behav. 2013;39:473–9. doi: 10.1016/j.addbeh.2013.10.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Falck RS, Wang J, Siegal HA, et al. The prevalence of psychiatric disorder among a community sample of crack cocaine users: an exploratory study with practical implications. J Nerv Ment Dis. 2004;192:503–507. doi: 10.1097/01.nmd.0000131913.94916.d5. [DOI] [PubMed] [Google Scholar]
- 11.Ford JD, Gelernter J, DeVoe JS, et al. Association of psychiatric and substance use disorder comorbidity with cocaine dependence severity and treatment utilization in cocaine-dependent individuals. Drug Alcohol Depend. 2009;99:193–203. doi: 10.1016/j.drugalcdep.2008.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Carroll KM, Nich C, Rounsaville BJ. Variability in treatment-seeking cocaine abusers: Implications for clinical pharmacotherapy trials. NIDA Res Monogr. 1997;175:137–157. [PubMed] [Google Scholar]
- 13.First MB, Spitzer RL, Gibbon M, et al. Structured Clinical Interview for DSM-IV Axis I Disorders–Patient Edition. New York: Biometrics Research Department, New York State Psychiatric Institute; 1996. [Google Scholar]
- 14.McLellan AT, Luborsky L, Woody GE, et al. An Improved Diagnostic Evaluation Instrument for Substance Abuse Patients The Addiction Severity Index. Journal of Nervous and Mental Disease. 1980;168:8. doi: 10.1097/00005053-198001000-00006. [DOI] [PubMed] [Google Scholar]
- 15.Shipley WC. A self administering scale for measuring intellectual impairment and deterioration. Journal of Psychology. 1940;9:371–377. [Google Scholar]
- 16.Beck AT, Ward CH, Mendelson M, et al. An inventory for measuring depression. Arch Gen Psychiatry. 1961;4:561–7. doi: 10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- 17.Barratt ES. Anxiety and impulsiveness related to psychomotor efficiency. Perceptual and Motor Skills. 1959;9:191–198. [Google Scholar]
- 18.Harvey PD, Greenburg BR, Serper MR. The affective lability scales: development, reliability, and validity. J Clin Psychol. 1989;45:786–793. doi: 10.1002/1097-4679(198909)45:5<786::aid-jclp2270450515>3.0.co;2-p. [DOI] [PubMed] [Google Scholar]
- 19.Mplus statistical modeling software: Version 6.11. Los Angeles, CA: Muthén & Muthén; 2011. [Google Scholar]
- 20.Masyn KE, Henderson CE, Greenbaum PE. Exploring the Latent Structures of Psychological Constructs in Social Development Using the Dimensional-Categorical Spectrum: The Dimensional-Categorical Spectrum. Soc Dev. 2010;19:470–93. doi: 10.1111/j.1467-9507.2009.00573.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Nylund KL, Asparouhov T, Muthén BO. Deciding on the number of classes in latent class analysis and growth mixture modeling: A Monte Carlo simulation study. Struct Equ Model. 2007;14:535–69. [Google Scholar]
- 22.Holtzman Steven. Confirmatory Factor Analysis and Structural Equation Modeling of Noncognitive Assessments using PROC CALIS. [Accessed Dec 10, 2013];2011 Available at http://www.nesug.org/Proceedings/nesug11/sa/sa07.pdf.
- 23.Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure. Struct Equ Model. 1999;6:1–55. [Google Scholar]
- 24.Bentler PM, Bonett DG. Significance tests and goodness-of-fit in the analysis of covariance structures. Psychological Bulletin. 1980;88:588–600. [Google Scholar]
- 25.McCutcheon AL. Latent Class Analysis. Newbury Park, CA: Sage Publications; 1987. [Google Scholar]
- 26.Tihomir AsparouhovT, Muthen B. Weighted Least Squares Estimation with Missing Data. [Accessed December 10, 2013];2010 Available at http://www.statmodel.com/download/GstrucMissingRevision.pdf.
- 27.Maydeu-Olivares A. Limited information estimation and testing of Thurstonian models for paired comparison data under multiple judgment sampling. Psychometrika. 2001;66:209–27. [Google Scholar]
- 28.Wagner FA, Anthony JC. Into the world of illegal drug use: exposure opportunity and other mechanisms linking the use of alcohol, tobacco, marijuana, and cocaine. Am J Epidemiol. 2002;155:918–25. doi: 10.1093/aje/155.10.918. [DOI] [PubMed] [Google Scholar]
- 29.Moeller FG, Dougherty DM, Barratt ES, et al. The impact of impulsivity on cocaine use and retention in treatment. J Subst Abuse Treat. 2001;21:193–8. doi: 10.1016/s0740-5472(01)00202-1. [DOI] [PubMed] [Google Scholar]
- 30.Brown RA, Monti PM, Myers MG, et al. Depression among cocaine abusers in treatment: relation to cocaine and alcohol use and treatment outcome. Am J Psychiatry. 1998;155:220–5. doi: 10.1176/ajp.155.2.220. [DOI] [PubMed] [Google Scholar]
- 31.Khantzian EJ. The self-medication hypothesis of addictive disorders: focus on heroin and cocaine dependence. Am J Psychiatry. 1985;142:1259–1264. doi: 10.1176/ajp.142.11.1259. [DOI] [PubMed] [Google Scholar]
- 32.Perez-Reyes M, Jeffcoat AR. Ethanol/cocaine interaction: cocaine and cocaethylene plasma concentrations and their relationship to subjective and cardiovascular effects. Life Sciences. 1992;51:553–563. doi: 10.1016/0024-3205(92)90224-d. [DOI] [PubMed] [Google Scholar]
- 33.Farré M, De La Torre R, Llorente M, et al. Alcohol and cocaine interactions in humans. Journal of Pharmacology and Experimental Therapeutics. 1993;266:1364–1373. [PubMed] [Google Scholar]
- 34.Mannelli P, Janiri L, Tempesta E, et al. Prediction in drug abuse: Cocaine interactions with alcohol and buprenorphine. British Journal of Psychiatry. 1993;163:39–45. [PubMed] [Google Scholar]
- 35.Jatlow P, Elsworth JD, Bradberry CW, et al. Cocaethylene: A neuropharmacologically active metabolite associated with concurrent cocaine-ethanol ingestion. Life Sciences. 1991;48:1787–1794. doi: 10.1016/0024-3205(91)90217-y. [DOI] [PubMed] [Google Scholar]
- 36.Landry MJ. An overview of cocaethylene, an alcohol- derived, psychoactive, cocaine metabolite. Journal of Psycho- active Drugs. 1992;24:273–276. doi: 10.1080/02791072.1992.10471648. [DOI] [PubMed] [Google Scholar]
- 37.Vanyukov MM, Tarter RE, Kirillova GP, et al. Common liability to addiction and “gateway hypothesis”: Theoretical, empirical and evolutionary perspective. Drug Alcohol Depend. 2012;123:S3–S17. doi: 10.1016/j.drugalcdep.2011.12.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Fergusson DM, Horwood LJ. Does cannabis use encourage other forms of illicit drug use? Addiction. 2000;95:505–20. doi: 10.1046/j.1360-0443.2000.9545053.x. [DOI] [PubMed] [Google Scholar]