Abstract
Objective
To review the available knowledge on epidemiology and diagnoses of acute infections in children aged 2 to 59 months in primary care setting and develop an electronic algorithm for the Integrated Management of Childhood Illness to reach optimal clinical outcome and rational use of medicines.
Methods
A structured literature review in Medline, Embase and the Cochrane Database of Systematic Review (CDRS) looked for available estimations of diseases prevalence in outpatients aged 2-59 months, and for available evidence on i) accuracy of clinical predictors, and ii) performance of point-of-care tests for targeted diseases. A new algorithm for the management of childhood illness (ALMANACH) was designed based on evidence retrieved and results of a study on etiologies of fever in Tanzanian children outpatients.
Findings
The major changes in ALMANACH compared to IMCI (2008 version) are the following: i) assessment of 10 danger signs, ii) classification of non-severe children into febrile and non-febrile illness, the latter receiving no antibiotics, iii) classification of pneumonia based on a respiratory rate threshold of 50 assessed twice for febrile children 12-59 months; iv) malaria rapid diagnostic test performed for all febrile children. In the absence of identified source of fever at the end of the assessment, v) urine dipstick performed for febrile children <2years to consider urinary tract infection, vi) classification of ‘possible typhoid’ for febrile children >2 years with abdominal tenderness; and lastly vii) classification of ‘likely viral infection’ in case of negative results.
Conclusion
This smartphone-run algorithm based on new evidence and two point-of-care tests should improve the quality of care of <5 year children and lead to more rational use of antimicrobials.
Introduction
The rapid spread of resistant pathogens worldwide calls for urgent action to improve the rational use of antimicrobials. In low and middle income countries, where infectious diseases childhood mortality is high[1], substandard drugs, auto-medication and health workers (HWs)’ over-prescription of antimicrobials are driving the rapid spread of antimicrobial resistance. [2,3] Recent experience in malaria case management has shown that using appropriate diagnostic tools (malaria rapid diagnostic tests—mRDT) has the potential to improve rational use of antimalarial[4–6] without negative impact on health outcome. [4,7–10] Unfortunately it has often been accompanied with an increased antibiotics prescription[4,5,11], reflecting the challenge faced by HWs in front of a negative malaria test result, where diagnostic tools and skills to rule out bacterial diseases are scarce.
To support HWs’ decision making in the management of a sick child in low resource settings, WHO and UNICEF have developed the Integrated Management of Childhood Illness (IMCI) clinical algorithm in the mid 90’s[12]. The IMCI guidelines rely on the classification of patients based on clinical signs that can be recognized by trained HWs even if their educational background is limited[12]; no laboratory test was included in the IMCI version of 2008: presumptive malaria treatment was recommended for all febrile children (in high malaria risks area). Other causes of fever were not considered (except if the child presented also a complaint leading to another branch of the algorithm). With the advent of new evidence on etiologies and management of childhood illness and reliable point-of-care tests (POCTs), there is a need to rethink the IMCI guidelines and to propose a new algorithm for the management of acute medical illness for children aged 2 to 59 months living in low resource settings. This new algorithm should integrate reliable POCTs and, when the latter are not available, clinical predictors for acute illnesses, so that guidance based on best available evidence is provided to clinicians to decide on withholding antimalarials and antibiotics when not beneficial to the child. When no tool or strong evidence is available to propose appropriate procedures, expert opinion should be sought.
An algorithm developed for HWs in remote primary health care facilities (PHCF) should rely on simple clinical signs and easy-to-perform POCTs. Its structure should remain simple, although addressing a larger set of diseases may require a more complex one. The use of hand-held electronic technology to deliver the algorithm may facilitate the use of a complex clinical algorithm by HWs of varying backgrounds. Smartphones and tablets have the potential to facilitate the scale-up of standard recommendations in low resource settings.
Methods
Structured literature reviews
In order to identify the relevant diseases to be addressed in the algorithm, estimated data on the causes of global childhood mortality and morbidity from the Child Health Epidemiology Reference Group (CHERG)[13] publications, and from the Global Burden of Disease website[14] were reviewed to assess the burden of diseases in African children. A structured literature review (SLR) was also conducted to understand the clinical presentation (accurate clinical predictors) and diseases’ distribution in children under 5 years of age (U5) attending PHCFs in developing countries, as well as appropriate POCTs for the diagnosis of the targeted diseases.
Medline (PubMed), Embase (Ovid), and the Cochrane Database of Systematic Reviews (CDSR) were explored from inception to December 31st 2010, looking for articles assessing i) the prevalence of diseases and clinical features in U5 attending outpatient facilities in developing countries, and ii) the accuracy of diagnostic procedures for each of the targeted diseases. The detailed search strategy is described in Table 1. Papers involving U5 managed for acute medical conditions in ambulatory settings were selected. Studies involving only infants below 3 months of age or only adults were excluded. For prevalence of syndromes and diseases at PHCF, studies describing the clinical presentation and/or diagnoses presented by U5 attending outpatients facilities in developing countries were selected. For diagnostic procedures of targeted diseases, studies assessing accuracy of either clinical predictors or POCT were chosen. Systematic reviews addressing the questions of interest were also considered. An additional hand searching of reference lists of selected papers completed these searches. In order to better explore the accuracy of the clinical diagnosis for pneumonia, a systematic review of the literature and meta-analyses of studies assessing the diagnostic accuracy of clinical predictors was conducted, reported elsewhere (Rambaud Althaus et al, submitted).
Table 1. Structured literature reviews: search strategy.
| Pubmed | Embase | |
|---|---|---|
| 1 | "primary health care" OR "outpatients" OR "family practice" OR "emergency service" OR "ambulatory care" | |
| 2 | "fever/etiology"[MeSH Terms] OR "fever/diagnosis"[MeSH Terms] OR "fever/epidemiology"[MeSH Terms] | |
| 3 | "developing countries" | |
| 4 | prevalence OR epidemiology OR incidence | |
| 5 | "predictive value of tests"[MeSH Terms] OR "sensitivity and specificity"[MeSH Terms] OR "reproducibility of results"[MeSH Terms] OR diagnostic test OR diagnostic tests OR "physical examination"[MeSH Terms] OR"medical history taking"[MeSH Terms] | 'diagnostic accuracy'/exp OR 'predictor variable'/exp |
| 6 | "pneumonia"[MeSH Terms] | 'pneumonia'/exp OR 'lower respiratory tract infection'/exp OR 'respiratory tract infection'/exp |
| 7 | “typhoid fever” [MeSH Terms] | 'typhoid fever'/exp |
| 8 | “urinary tract infections”[MeSH Terms] | 'urinary tract infection'/exp |
| 9 | “otitis media”[MeSH Terms] | 'otitis media'/exp |
| 10 | “shigella”[MeSH Terms] OR “dysentery”[MeSH Terms] | 'shigellosis'/exp |
| 11 | Filters: Infant: 1–23 months; Preschool Child: 2–5 years | 'child'/exp |
| Prevalence | [ 1 AND ( 2 OR {3 AND 4} ) ] AND 11 | |
| Diagnostics | 6 AND 5 AND 11 | 6 AND 5 AND 11 |
| 7 AND 5 AND 11 | 7 AND 5 AND 11 | |
| 8 AND 5 AND 11 | 8 AND 5 AND 11 | |
| 9 AND 5 AND 11 | 9 AND 5 AND 11 | |
| 10 AND 5 AND 11 | 10 AND 5 AND 11 |
Findings of the study on causes of fever in outpatient Tanzanian children
In a recently published study on etiologies of fever conducted in outpatient clinics in Tanzania (Tanzanian fever study), clinical assessments and laboratory tests were performed in 1005 febrile children aged 2 months to 10 years (95% were U5) to establish the most probable causes of fever[15]. The distribution of diagnoses, overall and stratified by age, was taken into account to select the targeted disease included in the final algorithm. The clinical predictors for the targeted diseases identified in the Tanzanian fever study were also used to build the new algorithm (De Santis et al, in preparation).
Algorithm construction
With the IMCI algorithm for children 2–59 months of age as departure point, the evidence retrieved from the SLRs and from the Tanzanian fever study was used to propose modifications and new recommendations when relevant, and to design a new decision tree. Diseases were included in the algorithm if they were treatable, and responsible for i) high child mortality and morbidity, ii) high attendance rate at outpatient facilities, and, iii) high antimicrobial prescription rate. Clinical features that could easily be assessed by HWs of varying background and POCT easy to deploy in low resource ambulatory settings were integrated in the classification procedures, when its use improved the classification accuracy. The treatment options proposed in ALMANACH were in line with the 2008 WHO IMCI [16] and the Tanzanian National Standard Treatment guidelines [17] since the algorithm was intended to be used in Tanzania and had to comply with local policies. Once the new algorithm was finalized, both a paper booklet and an electronic software running on android smartphones and tablets were developed. For the paper booklet, the IMCI structure in 3 steps was kept—“Assess, Classify, and Treat”—, as well as the color-coded triage system: red for conditions that require urgent referral, orange for conditions requiring specific treatment, and green for condition needing simple counseling and symptomatic home management[12].
Results
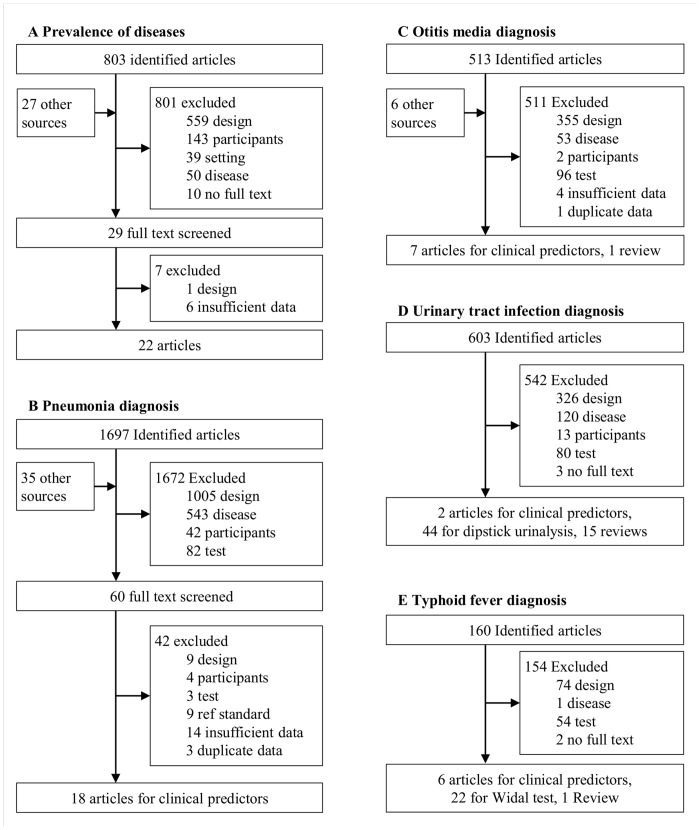
Flow diagrams of studies selection for the SLRs are available in Fig 1.
Fig 1. Flow diagrams of study selection process in the structured literature reviews.
All modifications made to the IMCI content based on new findings are presented in Table 2. The major changes concerned: malaria and pneumonia diagnosis; otitis media treatment; the addition of urinary tract infection (UTI) and possible typhoid fever; and a new classification entitled “likely viral infection”. The most important modifications are discussed below.
Table 2. Major changes in ALMANACH as compared to IMCI algorithm based on evidence and experts’ opinion.
| Location | Topic | IMCI | ALMANACH | Rationale |
|---|---|---|---|---|
| Management of very severe diseases section | Very severe diseases | “A child with any general danger signs needs URGENT attention; complete the assessment and pre-referral treatment immediately so that referral is not delayed” | If the child has any general danger sign, HWs are not asked to complete the assessment of all symptoms, but rather to “Give pre-referral treatment and REFER URGENTLY” | To complete the assessment would delay pre-referral treatment, and impair prognosis. In presence of general danger sign, the priority is to give rapidly presumptive AB/AM treatment[42,43] and to refer to hospital, where further etiological investigations will allow adapting the treatment. |
| List of general danger signs | “Lethargic; Convulsing; Unable to drink/breastfeed; Vomits everything; History of convulsion” | “Convulsing; Lethargic; Unable to drink/breastfeed; Vomits everything; History of convulsion; Jaundice; Cyanosis; Stiff neck; Severe pallor; Severe wasting” | Stiff neck, severe pallor, and severe wasting (assessed later on in IMCI) are part of the ALMANACH initial assessment, in order to facilitate and fasten the detection and management of very severe diseases. Jaundice and cyanosis that are strong predictors for serious bacterial diseases and severe respiratory conditions [15], have been added to the general danger signs. | |
| Pre-referral treatment | Available in the “TREAT THE CHILD” section in the middle of the booklet | Available in the “Management of very severe diseases” section in the first pages of the booklet | To facilitate and fasten the management of severe patients, the first section “Management of very severe diseases” has all assessment, classification and treatment charts together. | |
| Management of children with no general danger signs | Fever § | Fever § is one of the 4 “Main symptoms”. | Fever is a crossing point in ALMANACH: different recommendations are made for children (non-severe) with or without fever § . | In children having no underlying chronic condition, and no danger signs, only few bacterial infections should be considered. Apart from dysentery and soft tissue infection, antibiotics are not recommended in the treatment of non-severe non-febrile conditions in ALMANACH. |
| Fever | Classifications considered in the Fever chart are: “Very severe disease”, “Malaria” and “Measles”. Additional classification in low malaria risk contexts: “Fever, malaria unlikely” | Classifications considered in the Fever algorithm: “Malaria”, Acute respiratory infections, including “Pneumonia”; Diarrhea related classifications; Ear related classification; Measles; Skin infections; “UTI”, “Typhoid fever”, “Likely viral infection” | Designing a specific chart for patients with fever allows considering more fever related classifications than in IMCI, thus to address relevant non-malaria fever. This design allow also to consider “Likely Viral infections” after having excluded potentially life threatening conditions | |
| Febrile chart | Malaria | Presumptive diagnosis of malaria for all children with fever in high malaria risk contexts | Test-based malaria diagnosis is recommended, using mRDTs in all children with fever. Antimalarials only recommended in test positive patients | The accuracy, the performance and the safety[7] of a diagnostic strategy based on mRDTs have been evaluated and demonstrated in U5. |
| FebrileCough chart | Pneumonia | Pneumonia diagnosis rely on increased respiratory rate (RR) above age specific threshold: 50 breath/min if aged 2–11 months; 40/min if aged 12–59 months | Pneumonia is considered in children aged 2–59 months, if they report the presence of fever and have a RR above 50 breaths/min | The need of antibiotics in children aged 2–59 months with non-severe pneumonia as defined in IMCI is questioned[76]. In children aged 12–59 months the gain in sensitivity doesn’t balance the loss of specificity for the diagnosis of pneumonia when using the threshold 40 instead of 50 breath/min. (see results section) |
| Ear problem chart | Acute ear infection | Oral antibiotics are recommended for “Acute ear infection” defined as either “ear pain” or “ear pus/ discharge for less than 14 days” | Oral antibiotics are only recommended for children with fever and “ear pus/ discharge for less than 14 days” | The need for antibiotics for otitis media is questioned[56]. Ear pain is a weak predictor of otitis media[53,55,77] especially in children below 2 years of age. AB are most useful for children with otitis media and ear discharge[56]. |
| Skin problem chart | Skin and soft tissue infections | Some guidance provided in an annex and not integrated with the complaints of the main algorithm | Referral to hospital is recommended for febrile skin lesions with a size >4 cm or associated with red streaks or tender nodes, and for multiple abscesses. Local treatment and home management is recommended for impetigo and minor abscesses | Severe soft tissue infections require in hospital treatment and injectable antibiotics. Limited skin infections can be safely managed by topical treatment. |
| Febrile chart for “Fever with no identified cause” after symptom charts assessment | Urinary tract infection | Not considered in IMCI | Considered in non-severe febrile children, under 2 years of age, with no primary focus identified; and in children, above 2 years of age, with dysuria. Urinalysis using a dipstick is recommended for the diagnostic. | UTI is most frequent in children under 2 years of age. Above 2 years of age, the specificity of dysuria symptoms is low. The accuracy and performance of dipstick for UTI diagnosis have been demonstrated. Dipsticks for pregnancy follow-up were already broadly available in PHCFs in Tanzania; dipsticks for urinalyses were available in Health Centers. |
| Typhoid fever | Not considered in IMCI | In non-severe febrile children above 2 years of age, with no primary focus identified, abdominal palpation is recommended. In presence of tenderness, a presumptive treatment for typhoid fever and invasive intestinal bacterial infections is recommended. | Typhoid fever and other invasive enteric infections are life threatening conditions. In low resource care facilities, HWs fear to miss these diagnoses and tend to overprescribe antibiotics to children with no identified causes of fever. In the Tanzanian fever study, abdominal tenderness was associated with invasive bacterial infections and typhoid[15], in children above 2 years of age. |
AB: antibiotics, AM: antimalarials, HW: health worker, IMCI: Integrated Management of Childhood Illness, PHCF: primary health care facility, U5: children under 5 years of age, UTI: urinary tract infection.
§Fever is defined by either history of fever or axillary temperature above 37.5°C or child feels hot.
Selection of syndromes or diseases to be addressed by the algorithm
Estimations of burden of diseases by CHERG[1] and IHME[14,18] reported that low respiratory tract infections/pneumonia, malaria, and diarrhea were the leading causes of child mortality in 2010, globally and in Sub Saharan Africa (SSA). These 3 infectious diseases were estimated to be responsible for more than 40% of U5 deaths in SSA. They were also the leading causes of morbidity, responsible for 41% of the total 2010 DALYs in SSA[14]. Other frequent causes of child mortality were HIV/AIDS (3.5 to 4% of U5 deaths in SSA[1,14]), meningitis (3 to 4%[1,14]), measles (1%[1,14]), and tuberculosis (0.8%[14]). In infants aged 1 to 11 months, pertussis (2.8% of deaths in 1–11months infant in SSA) and syphilis (2.3%) were also frequent causes of death[14]. In children aged 1 to 4 years, typhoid fever was estimated to be responsible for 0.6% of both DALYs and deaths, and bacterial skin diseases for 0.7% of DALYs, and 0.2% of deaths[14].
The SLR identified 22 articles assessing either symptoms or diagnoses distributions, or both, in children attending outpatient facilities in developing countries. In all selected papers assessing symptoms, fever (by history or measured, hereafter referred as fever), cough and diarrhea were the most frequent symptoms reported, respectively by 65 to 93%[19–24], 44 to 82%[19–21,23,24], and 22% to 45%[19–21,23] of children. Diseases of potential bacterial origin reported in the studies retrieved by the SLR were: pneumonia (reported in 5 to 30% of children[15,19–21,24–31]), typhoid fever (3 to 13%[15,24,26]), dysentery (3 to 12% [19,28,29]), otitis media (2 to 12%[7,19–21,28–31]), UTI (1 to 7%[15,24,28,30,32,33]); and meningitis (0 to 3%[19,25,28]). Tonsillitis was reported in 1% of 1005 children in the Tanzanian fever study; all had a negative streptococcal diagnostic test[15]. Another study reported tonsillitis or pharyngitis in 10% of the children, but no streptococcal test was performed[30].
Among the bacterial infections frequently reported, only typhoid fever, UTI and tonsillitis were not yet addressed in IMCI. The fear of these 3 infections is often a reason to prescribe antibiotics in low resource setting. With regards to tonsillitis, early recognition and treatment of streptococcal tonsillitis is of high importance to prevent rheumatic fever and its complications, but prevalence of group A β-hemolytic streptococcus is much lower in U5 than in older children[34], and close to zero in children under 2 years of age[35]. Moreover, acute rheumatic fever and rheumatic heart disease are rare in U5[36,37]. Therefore addressing streptococcal tonsillitis in the management of U5 was considered not to be necessary. UTI and typhoid fever were thus selected to be addressed in the new algorithm, together with the other diseases already addressed in IMCI.
Identification of severe illnesses
In the IMCI algorithm, urgent referral to hospital is recommended in the presence of any of 5 general danger signs (difficulty in drinking, repeated vomiting, had convulsion, lethargy or unconsciousness, convulsing) or in presence of any of the 8 symptom-related danger signs (danger sign related to fever: stiff neck; related to cough: stridor or chest indrawing; related to measles features: clouding of cornea or extensive mouth ulcers; related to malnutrition: severe wasting or oedema of both feet; related to pallor: severe palmar pallor). The usefulness of these IMCI referral criteria were evaluated in two studies[38,39]. These studies estimated the accuracy of the presence of any of the danger signs to predict hospital referral. Estimates of sensitivity and specificity were 46% and 79% respectively in the Kenyan study [38] and 86% and 64% respectively in the study conducted in Bangladesh [39]. In the Kenyan study, accuracy of these criteria to predict death in admitted U5 patients was also assessed (sensitivity 89%, specificity 44%)[38]. A systematic review for children in developed countries[40] has also identified reduced consciousness, convulsions, cyanosis, rapid breathing, and slow capillary refill as the strongest predictors of severe illness. Meningeal irritation was also a strong predictor of serious bacterial infection in 3 reported studies [likelihood ratio (LR) ranging from 2.57 to 275] [40]. While reviewing the underlying evidence used to build the recommendations for referral in IMCI, only very few studies were identified. As for IMCI, one of the main aims of the present algorithm is to allow early identification and referral of children with severe conditions and serious bacterial infections; therefore, to ensure good sensitivity, all the IMCI referral criteria were kept although underlying evidence was scarce, and 2 signs predicting serious infections were added to the IMCI general danger signs, i.e. cyanosis that is broadly recognized as a sign of severe hypoxemia [40] and jaundice that was shown to be predictive of bacterial disease in the Tanzanian fever study[15] and can also be associated with severe malaria [41]. In order to improve and fasten the identification of severe patients, all general danger signs, were grouped together with stiff neck, severe wasting, and severe pallor at the beginning of the assessment chart, instead of having some of them included in the branches for each syndrome. Danger signs related to specific symptoms were kept within the symptoms related charts, such as chest indrawing with cough, or tender swelling behind the ear with ear problem. Children with general danger signs are classified as having ‘Very severe disease’. These children with general danger signs are at risk of severe sepsis. In ALMANACH, acknowledging that early antimicrobials can improve the outcome of these children prognosis[42,43], and realizing that the full assessment would not modify this recommendation, a separate management chart was developed for patients with danger signs, allowing prompt presumptive treatments, and skipping assessment tasks that would only delay the rapid management and referral these children require.
Malaria diagnosis
Decline in the proportion of fevers due to malaria [44] together with the availability of easy-to-use, reliable POCTs—i.e. mRDTs—have driven the WHO recommendations to shift in 2010 from presumptive to test-based malaria case management[45]. The safety of a mRDT-based malaria case management in U5 has been demonstrated[7–10,46–48]. Several African countries have now changed their malaria diagnosis policy and adopted the use of mRDTs in their national programs. Following the new WHO malaria treatment guidelines, the use of mRDTs was integrated in present algorithm. mRDTs were also recently added officially to the WHO/UNICEF generic IMCI algorithm[49].
Pneumonia diagnosis
In a recent meta-analysis of clinical predictors for radiological pneumonia (Rambaud Althaus et al, submitted), the clinical features with the higher pooled LR were respiratory rate ≥50 breaths/min (LR 1.90; 95%CI 1.45–2.48), grunting (1.78; 1.10–2.88), lower chest indrawing (1.76; 0.86–3.58), and nasal flaring (1.75; 1.20–2.56). The best features to rule out the diagnosis (having the lowest pooled LR) were: no history of fever (0.53; 0.41–0.69), and respiratory rate ≥40 breaths/min (0.43; 0.23–0.83). Cough had also a low but heterogeneous LR (0.30; 0.09–0.96). The IMCI criterion for pneumonia classification, i.e. age-related fast breathing (≥50/min from 2 to 11 months, and ≥40/min from 12 to 59 months) showed low diagnostic performance in the meta-analysis, both to rule in the disease (presence of fast breathing had a pooled LR of 1.55 (0.44–5.42)) and to rule it out (absence of fast breathing had a pooled LR of 0.63 (0.16–2.55)). In the Tanzanian fever study, the best predictors to rule in radiological pneumonia among all febrile children were difficult breathing (LR 7.9, 2.8–22.1), chest indrawing (7.1; 2.9–17.6), nasal flaring (7.0; 2.5–19.4), respiratory rate ≥50/min (6.1; 3.5–10.4) and abnormal chest auscultation (5.5; 3.7–8.1). No feature was good at ruling out the diagnosis. In the present algorithm, in the absence of a reliable point-of-care diagnostic test, we decided to combine the best available clinical predictors (history of fever, cough, difficult breathing and fast breathing), except nasal flaring and grunting, and abnormal chest auscultation because most IMCI trained clinicians are not familiar with these features. Chest indrawing was kept but to decide on referral to hospital rather than to diagnose pneumonia, because of the relatively high proportion of these children that harbor hypoxemia[50] Regarding fast breathing, because using an age-related threshold did not improve the diagnostic test accuracy in the meta-analysis (Rambaud Althaus et al, submitted), a single threshold of ≥50/min for all age groups was chosen; 50/min rather than 40/min was chosen to ensure a reasonable specificity, knowing that most of pneumonias in young children are due to viruses[51]. The recommendation in the present algorithm is thus to prescribe antibiotics for pneumonia to children with [history of fever or elevated temperature] AND [cough or difficult breathing] AND respiratory rate ≥50/min, regardless of the malaria test result.
Otitis Media
In the SLR 7 articles and a systematic review that addressed the question of the accuracy of symptoms and signs for the diagnosis of otitis media were retrieved[52]. In these studies, some otoscopic signs were strongly associated with otitis media diagnosis[52], but in low resource settings otoscopy is not available in ambulatory care. Other symptoms, such as earache, ear rubbing, and fever, although reported as associated with otitis media in 4 old studies (LR 3.03 to 7.3[53–55]), were not associated with this diagnosis when reported by parents of children aged 6 to 36 months attending primary care offices in a more recent study(52). Otitis media is often a self-limiting condition in young children. The 2010 Coker[52] and Sanders’ Cochrane[56] reviews, looking at available evidence of the benefit of antibiotic treatment for otitis media, report that there is little benefit (compared to placebo) and no evidence that antibiotics reduce complications or recurrence[52,56]. An individual patient data meta-analysis from 6 randomised trial reported that antibiotics were more beneficial in children aged less than 2 years with bilateral otitis media, and in those with both otitis media and otorrhoea. In children with otorrhoea, 60% of controls and 25% of those on antibiotics still had pain, fever or both at 3–7 days, with a rate difference of -36% (95%CI -53% to -19%) and a number needed to treat of 3, whereas in children without otorrhoea the rate difference and NNT were respectively -14% (-23% to -5%) and 8[57].
Otitis media being often a self-limiting condition in young children, in the absence of accurate non-otoscopic clinical predictors the new algorithm propose to limit antibiotic prescription to children presenting with ear discharge.
Urinary tract infection
Two articles and 12 reviews assessing the accuracy of clinical predictors for the diagnosis of UTI in children were retrieved from the SLR. No additional article since the most recent review published in 2007 was found[58]. The following predictors were identified: temperature >40°C (2 studies, LR 3.3; 1.3–8.3[59] and LR 3.2; 0.7–15.6[60]), jaundice (LR 2.1; 0.3–17.4)[61], and suprapubic tenderness (LR 4.4; 1.6–12.4)[62]. The absence of another source of fever on examination increased the probability of UTI (3 studies, summary LR 2.8; 1.9–4.3)[58]. Among children ≥2 years, abdominal pain (LR: 6.3; 2.5–16.0) [61], dysuria (LR 2.4; 1.8–3.1)[63] and new-onset of urinary incontinence (LR 4.6; 2.8–7.6)[63] also increased the probability of UTI.
In the Tanzanian fever study, the following predictors to rule in UTI were found: pollakiuria (LR 3.5; 1.4–8.8), temperature >40°C (3.1; 1.4–7.1), fever for more than 3 days (2.1; 1.2–3.6) and age<2 years (1.4, 1.22–1.57); the best predictors to exclude UTI were: age≥3 years (LR 0.22; 0.07–0.66), headache (0.27; 0.04–1.89) and diarrhea (0.33; 0.08–1.32) (De Santis et al, in preparation). Based on these predictors, several national and international guidelines recommend to consider this condition in febrile children below 2 years of age, with no obvious cause of fever[32,64]. No symptom or sign, nor combination of them is predictive enough in this age group to appropriately identify children with UTI. The gold standard (urine culture) is generally not available in low resources ambulatory setting. Urinalysis with urine dipsticks detecting leucocyte esterase and nitrite has been evaluated in many settings: 4 systematic reviews with meta-analyses estimated sensitivities for leucocyte esterase and/or nitrites to be 81%[65], 88%[66,67], and 93%[32] and specificities 72%[32], 79%[67], 93%[66] and 97%[65]. A dipstick urinalysis negative for both nitrites and leukocyte esterase had a LR of 0.2 (95% CI, 0.16–0.26)[58]. With either leucocyte esterase or nitrite positive the LR was 6.1 (95% CI, 4.3–8.6), increasing to 28 (95% CI, 17–46) when both leucocyte esterase and nitrite were positive[65]. In 2005, the WHO department of Child and Adolescent Health and Development recommended the use of urinalysis by urine dipstick for the diagnosis of UTI in children wherever dipstick were feasible[64]. With the implementation of the WHO focused antenatal care guidelines, urine dipstick for proteinuria detection have been implemented and are thus available in PHCFs in many African countries. Based on the good diagnostic performance of urine dipstick, and it’s feasibility in low resource setting, the new algorithm proposes to perform urine dipstick for the diagnostic of UTI in the patients at higher risk of UTI, i.e. children below 2 years of age having fever with no cause identified during the assessment (but regardless of the malaria test result, due to the possibility that the parasites might only correspond to an incidental infection and not the actual cause of the acute illness). For children from 2 to 5 years of age, only those complaining of dysuria are proposed a dipstick urinalysis. Antibiotic treatment for UTI is recommended when either leucocyte esterase or nitrite, or both are positive.
Typhoid fever
Regarding the diagnosis of enteric fever, 6 articles assessing clinical predictors of enteric fever were retrieved [68–73]. Only 2 were conducted in outpatients: one included patients above 15 years of age[71] and the other patients above 4 years of age[70]. None of the studies thus included our target population of U5 outpatients. In the Tanzanian fever study[15], the following predictors to rule in typhoid where identified: liver pain (LR 9.8; 2.7–35.5), abdominal tenderness (7.0; 3.3–15.2), jaundice (6.2; 3.1–12.4) and age >2 years (2.0; 1.6–2.4). To rule out typhoid, only ‘not during rainy season’ was predictive (LR 0.50; 0.27–0.92) (De Santis et al, in preparation). Jaundice being already included as danger sign and liver pain being difficult to assess in a child, the new algorithm recommends looking for abdominal tenderness in children ≥2 years of age having fever with no cause identified during the child’s assessment (regardless of the malaria test result). When present, antibiotic treatment for typhoid fever is indicated.
Likely viral infection
Likely viral infection is a classification proposed in the present algorithm that does not exist in IMCI. Unnecessary antibiotics are often prescribed in febrile children by HWs when they do not manage to reach a diagnosis after their assessment, because they fear to have potentially missed a life-threatening bacterial infection. Because in the present algorithm most of the frequent bacterial infections have been assessed for, the probability that the child is still suffering from one is low if all findings are negative. Therefore, in the absence of danger signs, cough or fast breathing, diarrhea, ear discharge, symptoms of measles, infected skin lesion, abdominal tenderness, a positive dipstick urinalysis and a positive malaria RDT, the child is classified as having a “Likely viral infection”. HWs are then proposed to withhold antibiotics and antimalarials, prescribe symptomatic treatment for fever if any, and advise the caretaker on when to come back if symptoms persist or worsen.
Design of the algorithm
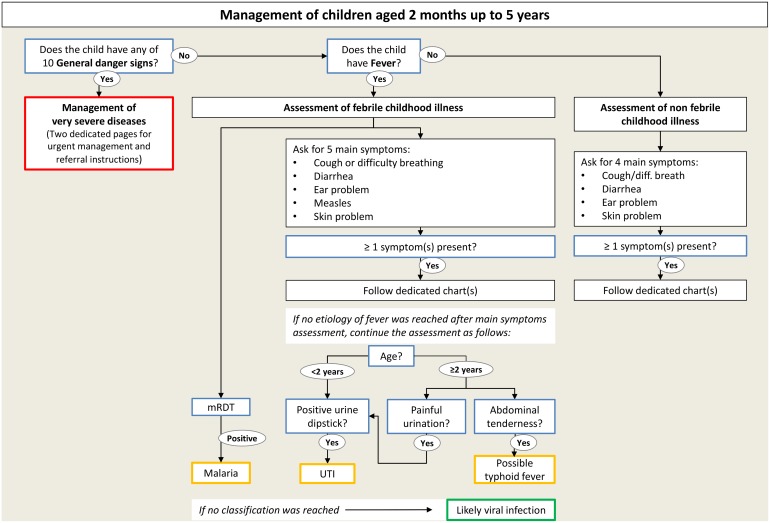
Based on the modifications and adjunctions to IMCI that were retained, a new algorithm for the management of childhood illnesses (ALMANACH) was designed. Efforts were made to keep the ALMANACH structure simple and graphically easy to follow by HWs. Therefore the IMCI 3 steps assessment and color codes were kept. However, in order to increase the number of conditions addressed, ALMANACH has been divided into 3 charts. The first chart provides recommendations for assessment of general danger signs and management of severe patients, the second chart provides recommendations for patients with fever, and the last one for patients without fever (see Fig 2 for an overview of ALMANACH’s structure). This 3-charts structure allows i) fastening the assessment and management of severe children, for whom all recommendations are available in the very first part of the algorithm and ii) a more comprehensive and specific assessment of children, with pneumonia, malaria, UTI and typhoid fever being considered only in febrile children. In the IMCI algorithm, fever is one of the main symptoms. The IMCI fever box only considers malaria and measles for a child with acute fever (≤7 days) without danger signs. Within ALMANACH, the aim was to address non-malaria fever causes. Although parts of the algorithms, such as the diarrhea chart, are the same in both the ‘febrile’ and ‘non-febrile’ algorithms, replacing the fever box by a full algorithm for children with fever or history of fever was necessary to propose meaningful considerations of fever causes in sequential pathways, allowing considering some conditions in a subset of patients only. In addition, this categorization allowed limiting antibiotic treatment in children without fever or history of fever.
Fig 2. Overview of ALMANACH's structure.
mRDT: malaria rapid diagnostic test. UTI: urinary tract infection.
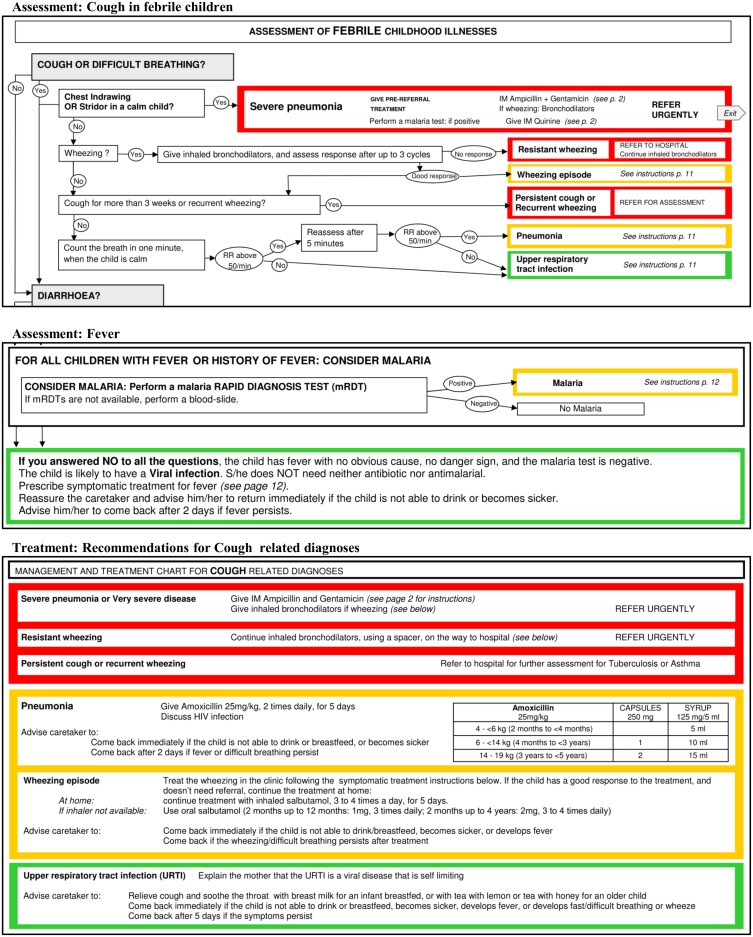
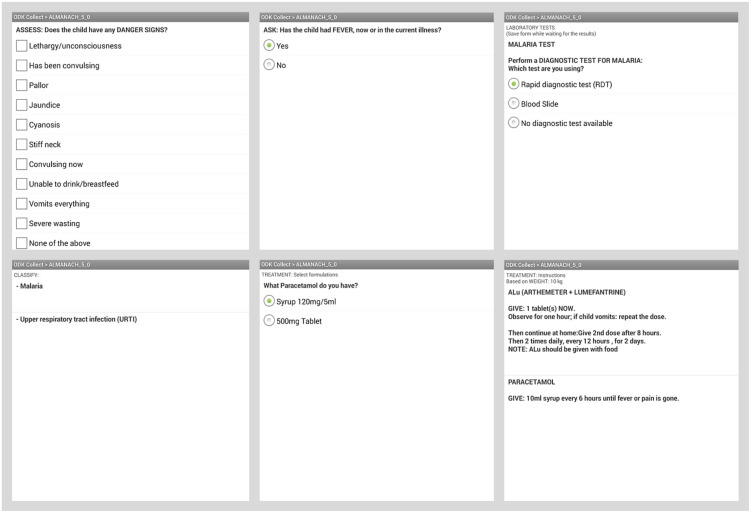
ALMANACH was first designed as a paper booklet (Fig 3 and S1 Fig), it was then developed as an android application for smartphones, coding the different steps of the algorithm into a Java-Rosa X form run by OpenDataKit and OpenMRS software[74,75]. The electronic ALMANACH (e-ALMANACH) guides HWs through the child’s assessment up to the classification and treatment recommendations (Fig 4). Treatment dosages are computed according to the body weight or age when weight is not available. Moreover e-ALMANACH collects in real time information on child demographic characteristics, disease classification and treatment prescribed. This information is stored by the mobile device, can be sent to a server and feed health information systems.
Fig 3. Samples of ALMANACH in paper format.
Fig 4. Samples of ALMANACH in electronic format.
Discussion
The aim of ALMANACH is to provide guidance to health workers on antimicrobial prescription, in order to treat only children aged 2 to 59 months who will potentially benefit from them. Apart from malaria, IMCI was not directly addressing causes of fever, leaving HWs with their fear of life-threatening conditions once malaria was ruled out by mRDT. On the other hand, viral infections that represent the vast majority of the causes of fever in U5 children[15] are never explicitly mentioned or proposed as diagnosis in IMCI, giving a wrong impression to health workers that bacterial infections are frequent and that children should often be prescribed antibiotics. Using the best available and feasible diagnostic procedures for the main causes of acute illness in children attending PHCFs, the present new algorithm should address most of the concerns of HWs regarding bacterial infections and remind them that children often suffer from self-limited viral conditions that do not warrant any specific treatment beside antipyretics. By providing tools to rule out malaria, UTI, and typhoid fever and by proposing a new ‘Likely viral infection’ classification, the use of ALMANACH has thus the potential to improve the health outcome of febrile children and at the same time decrease unnecessary antimalarial and antibiotic prescriptions. The content of ALMANACH was based on literature reviews and expert opinions. The level of evidence provided by the literature was generally low and no formal process was followed to reach a broad expert consensus. Within the current project, only the POCTs currently available in low resource settings were considered, constraining the new algorithm to rely mostly on the best available simple clinical predictors. To further improve the quality of the management of pediatric illnesses and the rational use of medicines, accurate and affordable POCTs for bacterial or even viral infections are highly needed.
While broadening the spectrum of diseases to be addressed, the algorithm became more complex than IMCI. This might be an issue for the targeted audience, i.e. HWs of different background working in low resource ambulatory settings. In order to facilitate understanding and usability of the decision chart, the 3 steps IMCI structure (Assess, Classify and Treat) and the color coded triage, already known by IMCI trained HWs, were kept. Electronic algorithms, by guiding HWs step by step through the algorithm, allow to using a more complex structure with lower risk of misuse. The electronic version of ALMANACH running on smartphones and tablets was designed to address these needs.
Although ALMANACH broadened the spectrum of diseases addressed in the algorithm, some aspects of childhood illness were left uncovered. Indeed ALMANACH does not provide recommendations for the management of chronic or non-infectious conditions. Within the current project, only identifiable and treatable acute infections were targeted because the objective was to improve the use of antimicrobials in order to tackle both the risk of resistance development due to their overuse and the high childhood mortality related to infectious diseases. Because the algorithm was meant for remote PHCF, full algorithms for the management of severe conditions, for HIV-infected and/or malnourished children were not developed; only recommendations on how to identify children suffering from these conditions and advice to refer them to the second level of care were provided. We foresee that developing and integrating additional algorithms for the management of these conditions, but also for other patients, either at primary or secondary level of health care systems, would allow further improvement of the quality of health services, but also better acceptability of the tool by HWs. However this was out of the scope of the present project. The paper and electronic ALMANACH have the potential to improve the management of the sick child. This has been demonstrated in a recently completed feasibility study, which showed the ALMANACH algorithm to improve health outcome of children managed with this tool and to drastically reduce antibiotic prescription (Shao et al, companion paper submitted). These results were obtained in two settings, urban and rural, albeit with a limited number of patients enrolled. They do not represent a definite validation of ALMANACH, but show great promise and should invite researchers to further explore the potentials of this new approach for a rational management of children aged 2–59 months. Further improvement could be brought by integrating other POCT detecting key pathogens once they become available, or even better, by integrating host biomarkers able to predict children in need of antibiotics or at risk of dying.
Supporting Information
(PDF)
Acknowledgments
We would like to thank Wilson Were, MD and Mario Gehri, MD for useful discussions and comments on the content and design of the clinical algorithm, and Fabrice Althaus for his participation to the literature reviews and input on methodology.
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
The study was part of a larger project which aimed at improving the quality of health care and rational use of drugs for children in Tanzania (PeDiAtrick project), funded by the Swiss National Science Foundation (www.snf.ch; Grant Number IZ70Z0 – 124023). The funders played no role in study design, collection, analysis, interpretation of data, writing the report, or in the decision to submit the paper for publication. Pan Africa Clinical Trial registration number PACTR201011000262218.
References
- 1. Liu L, Johnson HL, Cousens S, Perin J, Scott S, Lawn JE, et al. Global, regional, and national causes of child mortality: an updated systematic analysis for 2010 with time trends since 2000. Lancet. 2012;379: 2151–2161. 10.1016/S0140-6736(12)60560-1 [DOI] [PubMed] [Google Scholar]
- 2. World Health Organization M. Medicines use in primary care in developing and transitional countries [Internet]. World Health Organization (WHO); 2009. Available: http://www.who.int/medicines/publications/who_emp_2009.3/en/ [Google Scholar]
- 3. Mayor S. Better access to drugs in developing countries is accelerating resistance. BMJ. 2010;340: c3234 10.1136/bmj.c3234 [DOI] [PubMed] [Google Scholar]
- 4. Msellem MI, Mårtensson A, Rotllant G, Bhattarai A, Strömberg J, Kahigwa E, et al. Influence of rapid malaria diagnostic tests on treatment and health outcome in fever patients, Zanzibar: a crossover validation study. PLoS Med. 2009;6: e1000070 10.1371/journal.pmed.1000070 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. D’Acremont V, Kahama-Maro J, Swai N, Mtasiwa D, Genton B, Lengeler C. Reduction of anti-malarial consumption after rapid diagnostic tests implementation in Dar es Salaam: a before-after and cluster randomized controlled study. Malar J. 2011;10: 107 10.1186/1475-2875-10-107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Thiam S, Thior M, Faye B, Ndiop M, Diouf ML, Diouf MB, et al. Major reduction in anti-malarial drug consumption in Senegal after nation-wide introduction of malaria rapid diagnostic tests. PloS One. 2011;6: e18419 10.1371/journal.pone.0018419 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. D’Acremont V, Malila A, Swai N, Tillya R, Kahama-Maro J, Lengeler C, et al. Withholding Antimalarials in Febrile Children Who Have a Negative Result for a Rapid Diagnostic Test. Clin Infect Dis Off Publ Infect Dis Soc Am. 2010; 10.1086/655688 [DOI] [PubMed] [Google Scholar]
- 8. Mtove G, Hendriksen IC, Amos B, Mrema H, Mandia V, Manjurano A, et al. Treatment guided by rapid diagnostic tests for malaria in Tanzanian children: safety and alternative bacterial diagnoses. Malar J. 2011;10: 290 10.1186/1475-2875-10-290 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Baiden F, Webster J, Tivura M, Delimini R, Berko Y, Amenga-Etego S, et al. Accuracy of rapid tests for malaria and treatment outcomes for malaria and non-malaria cases among under-five children in rural Ghana. PloS One. 2012;7: e34073 10.1371/journal.pone.0034073 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Senn N, Rarau P, Manong D, Salib M, Siba P, Robinson LJ, et al. Rapid diagnostic test-based management of malaria: an effectiveness study in Papua New Guinean infants with Plasmodium falciparum and Plasmodium vivax malaria. Clin Infect Dis Off Publ Infect Dis Soc Am. 2012;54: 644–651. 10.1093/cid/cir901 [DOI] [PubMed] [Google Scholar]
- 11. Baiden F, Webster J, Owusu-Agyei S, Chandramohan D. Would rational use of antibiotics be compromised in the era of test-based management of malaria? Trop Med Int Health. 2011;16: 142–144. 10.1111/j.1365-3156.2010.02692.x [DOI] [PubMed] [Google Scholar]
- 12. Gove S. Integrated management of childhood illness by outpatient health workers: technical basis and overview. The WHO Working Group on Guidelines for Integrated Management of the Sick Child. Bull World Health Organ. 1997;75 Suppl 1: 7–24. [PMC free article] [PubMed] [Google Scholar]
- 13.Child Health Epidemiology Reference Group. CHERG | Publications [Internet]. [cited 25 Jul 2013]. Available: http://cherg.org/publications.html
- 14.Institute for Health Metrics and Evaluation. Global Burden of Disease (GBD) Compare [Internet]. [cited 21 Nov 2013]. Available: http://viz.healthmetricsandevaluation.org/gbd-compare/
- 15. D’Acremont V, Kilowoko M, Kyungu E, Philipina S, Sangu W, Kahama-Maro J, et al. Beyond Malaria—Causes of Fever in Outpatient Tanzanian Children. N Engl J Med. 2014;370: 809–817. 10.1056/NEJMoa1214482 [DOI] [PubMed] [Google Scholar]
- 16. WHO (Geneva). Integrated management of childhood illness for high HIV settings. Geneva: World health organization (WHO). Department of child and adolescent health and development (CAH); 2008. [PubMed] [Google Scholar]
- 17.Ministry of Health and Social Welfare (MoHSW). Standard Treatment Guidelines (STG) and the National Essential Medicines List (NEMLIT) for Mainland Tanzania [Internet]. 2007 [cited 22 Jan 2015]. Available: http://ihi.eprints.org/812/
- 18. Lozano R, Naghavi M, Foreman K, Lim S, Shibuya K, Aboyans V, et al. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380: 2095–2128. 10.1016/S0140-6736(12)61728-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Kolstad PR, Burnham G, Kalter HD, Kenya-Mugisha N, Black RE. The integrated management of childhood illness in western Uganda. Bull World Health Organ. 1997;75 Suppl 1: 77–85. [PMC free article] [PubMed] [Google Scholar]
- 20. Perkins BA, Zucker JR, Otieno J, Jafari HS, Paxton L, Redd SC, et al. Evaluation of an algorithm for integrated management of childhood illness in an area of Kenya with high malaria transmission. Bull World Health Organ. 1997;75 Suppl 1: 33–42. [PMC free article] [PubMed] [Google Scholar]
- 21. Weber MW, Mulholland EK, Jaffar S, Troedsson H, Gove S, Greenwood BM. Evaluation of an algorithm for the integrated management of childhood illness in an area with seasonal malaria in the Gambia. Bull World Health Organ. 1997;75 Suppl 1: 25–32. [PMC free article] [PubMed] [Google Scholar]
- 22. Barat L, Chipipa J, Kolczak M, Sukwa T. Does the availability of blood slide microscopy for malaria at health centers improve the management of persons with fever in Zambia? Am J Trop Med Hyg. 1999;60: 1024–1030. [DOI] [PubMed] [Google Scholar]
- 23. Rowe SY, Olewe MA, Kleinbaum DG, McGowan JE Jr, McFarland DA, Rochat R, et al. Longitudinal analysis of community health workers’ adherence to treatment guidelines, Siaya, Kenya, 1997–2002. Trop Med Int Health TM IH. 2007;12: 651–663. 10.1111/j.1365-3156.2007.01824.x [DOI] [PubMed] [Google Scholar]
- 24. Van Hemelrijck MJ, Lindblade KA, Kubaje A, Hamel MJ, Odhiambo F, Phillips-Howard PA, et al. Trends observed during a decade of paediatric sick visits to peripheral health facilities in rural western Kenya, 1997–2006. Trop Med Int Health. 2009;14: 62–9. 10.1111/j.1365-3156.2008.02184.x [DOI] [PubMed] [Google Scholar]
- 25. Salaria M, Singhi SC. Profile of patients attending pediatric emergency service at Chandigarh. Indian J Pediatr. 2003;70: 621–624. [DOI] [PubMed] [Google Scholar]
- 26. Animut A, Mekonnen Y, Shimelis D, Ephraim E. Febrile illnesses of different etiology among outpatients in four health centers in Northwestern Ethiopia. Jpn J Infect Dis. 2009;62: 107–10. [PubMed] [Google Scholar]
- 27. Chanda P, Hamainza B, Mulenga S, Chalwe V, Msiska C, Chizema-Kawesha E. Early results of integrated malaria control and implications for the management of fever in under-five children at a peripheral health facility: a case study of Chongwe rural health centre in Zambia. Malar J. 2009;8: 49 10.1186/1475-2875-8-49 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Factor SH, Schillinger JA, Kalter HD, Saha S, Begum H, Hossain A, et al. Diagnosis and management of febrile children using the WHO/UNICEF guidelines for IMCI in Dhaka, Bangladesh. Bull World Health Organ. 2001;79: 1096–1105. [PMC free article] [PubMed] [Google Scholar]
- 29. Simoes EA, Desta T, Tessema T, Gerbresellassie T, Dagnew M, Gove S. Performance of health workers after training in integrated management of childhood illness in Gondar, Ethiopia. Bull World Health Organ. 1997;75 Suppl 1: 43–53. [PMC free article] [PubMed] [Google Scholar]
- 30. Njama-Meya D, Clark TD, Nzarubara B, Staedke S, Kamya MR, Dorsey G. Treatment of malaria restricted to laboratory-confirmed cases: a prospective cohort study in Ugandan children. Malar J. 2007;6: 7 10.1186/1475-2875-6-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Khallaf N, el-Ansary S, Hassan M. Acute respiratory infections: sentinel survey in Egypt. World Health Forum. 1996;17: 297–300. [PubMed] [Google Scholar]
- 32. Downs SM. Technical Report: Urinary Tract Infections in Febrile Infants and Young Children. Pediatrics. 1999;103: e54–e54. [DOI] [PubMed] [Google Scholar]
- 33. Shaikh N, Morone NE, Bost JE, Farrell MH. Prevalence of Urinary Tract Infection in Childhood: A Meta-Analysis. Pediatr Infect Dis J. 2008;27: 302–308. 10.1097/INF.0b013e31815e4122 [DOI] [PubMed] [Google Scholar]
- 34. Shaikh N, Leonard E, Martin JM. Prevalence of Streptococcal Pharyngitis and Streptococcal Carriage in Children: A Meta-analysis. Pediatrics. 2010;126: e557–e564. 10.1542/peds.2009-2648 [DOI] [PubMed] [Google Scholar]
- 35. Woods WA, Carter CT, Schlager TA. Detection of group A streptococci in children under 3 years of age with pharyngitis. Pediatr Emerg Care. 1999;15: 338–340. [DOI] [PubMed] [Google Scholar]
- 36. Carapetis JR, Currie BJ, Mathews JD. Cumulative incidence of rheumatic fever in an endemic region: a guide to the susceptibility of the population? Epidemiol Infect. 2000;124: 239–244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Tibazarwa KB, Volmink JA, Mayosi BM. Incidence of acute rheumatic fever in the world: a systematic review of population-based studies. Heart. 2008;94: 1534–1540. 10.1136/hrt.2007.141309 [DOI] [PubMed] [Google Scholar]
- 38. Paxton LA, Redd SC, Steketee RW, Otieno JO, Nahlen B. An evaluation of clinical indicators for severe paediatric illness. Bull World Health Organ. 1996;74: 613–618. [PMC free article] [PubMed] [Google Scholar]
- 39. Kalter HD, Schillinger JA, Hossain M, Burnham G, Saha S, de Wit V, et al. Identifying sick children requiring referral to hospital in Bangladesh. Bull World Health Organ. 1997;75 Suppl 1: 65–75. [PMC free article] [PubMed] [Google Scholar]
- 40. Van den Bruel A, Haj-Hassan T, Thompson M, Buntinx F, Mant D, European Research Network on Recognising Serious Infection investigators. Diagnostic value of clinical features at presentation to identify serious infection in children in developed countries: a systematic review. Lancet. 2010;375: 834–845. 10.1016/S0140-6736(09)62000-6 [DOI] [PubMed] [Google Scholar]
- 41. World Health Organization, Communicable Diseases Cluster. Severe falciparum malaria. World Health Organization, Communicable Diseases Cluster. Trans R Soc Trop Med Hyg. 2000;94 Suppl 1: S1–90. [PubMed] [Google Scholar]
- 42. Dellinger RP, Levy MM, Carlet JM, Bion J, Parker MM, Jaeschke R, et al. Surviving Sepsis Campaign: International guidelines for management of severe sepsis and septic shock: 2008. Crit Care Med. 2008;36: 296–327. 10.1097/01.CCM.0000298158.12101.41 [DOI] [PubMed] [Google Scholar]
- 43. Gaieski DF, Mikkelsen ME, Band RA, Pines JM, Massone R, Furia FF, et al. Impact of time to antibiotics on survival in patients with severe sepsis or septic shock in whom early goal-directed therapy was initiated in the emergency department*. Crit Care Med. 2010;38: 1045–1053. 10.1097/CCM.0b013e3181cc4824 [DOI] [PubMed] [Google Scholar]
- 44. D’Acremont V, Lengeler C, Genton B. Reduction in the proportion of fevers associated with Plasmodium falciparum parasitaemia in Africa: a systematic review. Malar J. 2010;9: 240 10.1186/1475-2875-9-240 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. World Health Organization. Guidelines for the treatment of malaria. 2nd ed Geneva: World Health Organization; 2010. 10.1186/1475-2875-9-212 [DOI] [Google Scholar]
- 46. Faucher J-F, Makoutode P, Abiou G, Béhéton T, Houzé P, Ouendo E, et al. Can treatment of malaria be restricted to parasitologically confirmed malaria? A school-based study in Benin in children with and without fever. Malar J. 2010;9: 104 10.1186/1475-2875-9-104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Mubi M, Janson A, Warsame M, Mårtensson A, Källander K, Petzold MG, et al. Malaria rapid testing by community health workers is effective and safe for targeting malaria treatment: randomised cross-over trial in Tanzania. PloS One. 2011;6: e19753 10.1371/journal.pone.0019753 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Ukwaja KN, Aina OB, Talabi AA. Outcome of presumptive versus rapid diagnostic tests-based management of childhood malaria—pneumonia overlap in urban Nigeria: a pilot quasi-experimental study. Ethiop J Health Sci. 2010;20: 179–183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.World Health Organization, UNICEF. Integrated Management of Childhood Illness. Chart booklet. [Internet]. 2014. Available: http://apps.who.int/iris/bitstream/10665/104772/16/9789241506823_Chartbook_eng.pdf?ua=1
- 50. Subhi R, Adamson M, Campbell H, Weber M, Smith K, Duke T. The prevalence of hypoxaemia among ill children in developing countries: a systematic review. Lancet Infect Dis. 2009;9: 219–227. 10.1016/S1473-3099(09)70071-4 [DOI] [PubMed] [Google Scholar]
- 51. Feikin DR, Njenga MK, Bigogo G, Aura B, Aol G, Audi A, et al. Viral and bacterial causes of severe acute respiratory illness among children aged less than 5 years in a high malaria prevalence area of western Kenya, 2007–2010. Pediatr Infect Dis J. 2013;32: e14–19. 10.1097/INF.0b013e31826fd39b [DOI] [PubMed] [Google Scholar]
- 52. Coker TR, Chan LS, Newberry SJ, Limbos MA, Suttorp MJ, Shekelle PG, et al. Diagnosis, microbial epidemiology, and antibiotic treatment of acute otitis media in children. JAMA J Am Med Assoc. 2010;304: 2161–2169. [DOI] [PubMed] [Google Scholar]
- 53. Niemela M, Uhari M, Jounio-Ervasti K, Luotonen J, Alho OP, Vierimaa E. Lack of specific symptomatology in children with acute otitis media. Pediatr Infect Dis J. 1994;13: 765–768. [DOI] [PubMed] [Google Scholar]
- 54. Heikkinen T, Ruuskanen O. Signs and symptoms predicting acute otitis media. Arch Pediatr Adolesc Med. 1995;149: 26–29. [DOI] [PubMed] [Google Scholar]
- 55. Uhari M, Niemelä M, Hietala J. Prediction of acute otitis media with symptoms and signs. Acta Paediatr Oslo Nor 1992. 1995;84: 90–92. [DOI] [PubMed] [Google Scholar]
- 56. Sanders S, Glasziou PP, Del Mar CB, Rovers MM. Antibiotics for acute otitis media in children In: The Cochrane Collaboration, Sanders S, editors. Cochrane Database of Systematic Reviews. Chichester, UK: John Wiley & Sons, Ltd; 2010. Available: 10.1002/14651858.CD000219.pub2 [DOI] [Google Scholar]
- 57. Rovers MM, Glasziou P, Appelman CL, Burke P, McCormick DP, Damoiseaux RA, et al. Antibiotics for acute otitis media: a meta-analysis with individual patient data. The Lancet. 2006;368: 1429–1435. [DOI] [PubMed] [Google Scholar]
- 58. Shaikh N, Morone NE, Lopez J, et al. DOes this child have a urinary tract infection? JAMA. 2007;298: 2895–2904. 10.1001/jama.298.24.2895 [DOI] [PubMed] [Google Scholar]
- 59. Hoberman A, Chao HP, Keller DM, Hickey R, Davis HW, Ellis D. Prevalence of urinary tract infection in febrile infants. J Pediatr. 1993;123: 17–23. [DOI] [PubMed] [Google Scholar]
- 60. Krober MS, Bass JW, Powell JM, Smith FR, Seto DS. Bacterial and viral pathogens causing fever in infants less than 3 months old. Am J Dis Child 1960. 1985;139: 889–892. [DOI] [PubMed] [Google Scholar]
- 61. Musa-Aisien AS, Ibadin OM, Ukoh G, Akpede GO. Prevalence and antimicrobial sensitivity pattern in urinary tract infection in febrile under-5s at a children’s emergency unit in Nigeria. Ann Trop Paediatr. 2003;23: 39–45. 10.1179/000349803125002850 [DOI] [PubMed] [Google Scholar]
- 62. Shaw KN, Gorelick M, McGowan KL, Yakscoe NM, Schwartz JS. Prevalence of urinary tract infection in febrile young children in the emergency department. Pediatrics. 1998;102: e16 [DOI] [PubMed] [Google Scholar]
- 63. Heale WF. Management of urinary infections in children. Drugs. 1973;6: 230–236. [DOI] [PubMed] [Google Scholar]
- 64. WHO Department of Child and Adolescent Health and Development. Urinary Tract Infections in Infants and Children in Developing Countries in the Context of IMCI [Internet]. World Health Organization (WHO); 2005. Available: http://whqlibdoc.who.int/hq/2005/WHO_FCH_CAH_05.11.pdf [Google Scholar]
- 65. Whiting P, Westwood M, Watt I, Cooper J, Kleijnen J. Rapid tests and urine sampling techniques for the diagnosis of urinary tract infection (UTI) in children under five years: a systematic review. BMC Pediatr. 2005;5: 4 10.1186/1471-2431-5-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Gorelick MH, Shaw KN. Screening Tests for Urinary Tract Infection in Children: A Meta-analysis. Pediatrics. 1999;104: e54–e54. [DOI] [PubMed] [Google Scholar]
- 67. Williams GJ, Macaskill P, Chan SF, Turner RM, Hodson E, Craig JC. Absolute and relative accuracy of rapid urine tests for urinary tract infection in children: a meta-analysis. Lancet Infect Dis. 2010;10: 240–250. 10.1016/S1473-3099(10)70031-1 [DOI] [PubMed] [Google Scholar]
- 68. Khan M, Coovadia YM, Connoly C, Sturm AW. The early diagnosis of typhoid fever prior to the Widal test and bacteriological culture results. Acta Trop. 1998;69: 165–173. [DOI] [PubMed] [Google Scholar]
- 69. Davis TM, Makepeace AE, Dallimore EA, Choo KE. Relative bradycardia is not a feature of enteric fever in children. Clin Infect Dis. 1999;28: 582–586. [DOI] [PubMed] [Google Scholar]
- 70. Vollaard AM, Ali S, Widjaja S, van Asten HAGH, Visser LG, Surjadi C, et al. Identification of typhoid fever and paratyphoid fever cases at presentation in outpatient clinics in Jakarta, Indonesia. Trans R Soc Trop Med Hyg. 2005;99: 440–450. 10.1016/j.trstmh.2004.09.012 [DOI] [PubMed] [Google Scholar]
- 71. Hosoglu S, Geyik MF, Akalin S, Ayaz C, Kokoglu OF, Loeb M. A simple validated prediction rule to diagnose typhoid fever in Turkey. Trans R Soc Trop Med Hyg. 2006;100: 1068–1074. 10.1016/j.trstmh.2005.12.007 [DOI] [PubMed] [Google Scholar]
- 72. Neopane A, Poudel M, Pradhan B, Dhakal R, Karki DB. Enteric fever: diagnostic value of clinical features. Kathmandu Univ Med J KUMJ. 2006;4: 307–15. [PubMed] [Google Scholar]
- 73. Kuvandik C, Karaoglan I, Namiduru M, Baydar I. Predictive value of clinical and laboratory findings in the diagnosis of enteric fever. New Microbiol. 2009;32: 25 [PubMed] [Google Scholar]
- 74.Open Data Kit [Internet]. [cited 23 Aug 2013]. Available: http://opendatakit.org/
- 75.OpenMRS [Internet]. [cited 4 Aug 2013]. Available: http://openmrs.org/
- 76. Hazir T, Nisar YB, Abbasi S, Ashraf YP, Khurshid J, Tariq P, et al. Comparison of oral amoxicillin with placebo for the treatment of world health organization-defined nonsevere pneumonia in children aged 2–59 months: a multicenter, double-blind, randomized, placebo-controlled trial in pakistan. Clin Infect Dis. 2011;52: 293–300. 10.1093/cid/ciq142 [DOI] [PubMed] [Google Scholar]
- 77. Ingvarsson L. Acute otalgia in children—findings and diagnosis. Acta Paediatr Scand. 1982;71: 705–710. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(PDF)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.