Abstract
Transactional models of analysis can examine both moment-to-moment interactions within a dyad and dyadic patterns of influence across time. This study used data from a prospective adoption study to test a transactional model of parental depressive symptoms and mutual negativity between mother and child over time, utilizing contingency analysis of second-by-second behavioral data. To consider both genetic and environmental influences on mutual negativity, depressive symptoms were examined in both adoptive and birth mothers. Adoptive mother depressive symptoms at 9 months increased the likelihood that, at 18 months, children reacted negatively to their mothers' negative behavior, which in turn predicted higher levels of adoptive mother depressive symptoms at 27 months, suggesting that over time, mothers' depressive symptoms influence and are influenced by moment-to-moment mutual negativity with their toddlers. Birth mother depressive symptoms moderated the association between mutual negativity at 18 months and adoptive mother depressive symptoms at 27 months, suggesting a child-driven contribution to maternal depressive symptoms that can be measured by a genetic sensitivity.
Keywords: transaction, dyadic interaction, depressive symptoms, adoption, behavioral genetics, mother–child interaction
Transactional models of socialization regard parent and child behaviors as recurrent, reciprocal exchanges over time, through which each partner influences the other (Sameroff, 1975). Reciprocal exchanges between partners occur at a moment-to-moment level and over time become patterned interactions. Although research from a transactional perspective has focused on children's outcomes, the dynamic and dyadic nature of transactional patterns can have long-term effects on parents as well. This study used both microanalysis of moment-to-moment interactions and longitudinal analysis across infancy to examine mother and child interactions. We examined these interactions in an adoption sample, which permits the consideration of genetic relatedness within the transactional patterns.
Two lines of research support the transactional view of moment-to-moment interactions and the development of these as stable interaction patterns over early childhood. First, research examining moment-to-moment contingencies in mother–infant interactions demonstrates that mothers and young children influence one another's subsequent behaviors within seconds during brief interactions (e.g. Cohn & Tronick, 1989) and that the nature of these contingencies may vary as a function of maternal depressive symptoms (e.g. Field, Healy, Goldstein, & Guthertz, 1990). Second, longitudinal research shows parent and child characteristics, such as maternal depressive symptoms and child behavior problems, are correlated across time, in which early child behaviors are associated with later parental depression, which in turn predicts later child behavior problems (Bagner, Pettit, Lewinsohn, Seeley, & Jaccard, 2013; Gross, Shaw, Burwell, & Nagin, 2009; Gross, Shaw, Moilanen, Dishion, & Wilson, 2008). Together, these findings suggest that mothers and young children mutually influence each other's behaviors in everyday interactions and influence each other's development across time.
A large body of research has examined maternal depression and children's outcomes, with the premise that effects are predominantly unidirectional from negative and insensitive parenting behaviors to the development of negative and oppositional behaviors in children. In one exception, Gross et al. (2009) found higher levels of child noncompliance at 18 months of age to predict more chronic and elevated trajectories of maternal depression across 8 years than did lower levels of noncompliance. Highlighting the transactional nature of parent–child interaction, the current study used contingency analysis of the second-by-second behaviors of mothers and their toddlers during a teaching task to evaluate the influence of maternal depressive symptoms on mutual negativity in mother–child interactions over time and the influence of mutual negativity on maternal depressive symptoms over time. Moreover, because studies of maternal depression and its effects on children's development typically do not control for potential genetic influences, the current study used a prospective adoption design in which birth and adoptive parent characteristics were measured, which permits parsing of both genetic and environmental influences.
Elevated maternal depressive symptoms are associated with a wide range of mental health problems for offspring (Goodman et al., 2011) and may be uniquely challenging for parents of toddlers. Parents of toddlers, because of their young children's lack of expressive language and reasoning skills coupled with their newfound physical mobility and increasing oppositionality, face daily care-giving challenges that require interest, energy and flexibility (Brownell & Kopp, 2007; Shaw & Bell, 1993) anchored in a strong sense of efficacy and well-being (e.g. Dix, 1991; Teti & Gelfand, 1991). The demanding nature of toddlerhood challenges mothers to cope with their own negative emotions—for example, frustration and exasperation—while trying to manage and socialize difficult toddler behaviors.
One of the features of interactions between mothers who report elevated depressive symptoms and their infants is mutual negative emotion (Field et al., 1990). Mutual negative emotion is a critical area of study, as it is associated with later child behavior problems (Cole, Teti, & Zahn-Waxler, 2003; Dumas, LaFreniere, & Serketich, 1995). Mothers with higher levels of depressive symptoms may respond to their infants in ways that are less contingent, attuned and synchronized with infant signals (Cohn & Tronick, 1989; Field, Healy, & LeBlanc, 1989; Gelfand & Teti, 1990; Leadbeater, Bishop, & Raver, 1996). Maternal depressive symptoms may also interfere with maintaining interaction and joint attention (e.g. Henderson & Jennings, 2003). Together, these studies suggest that maternal depressive symptoms contribute to greater negativity in the parent–child interaction.
A transactional model, however, underscores the bidirectional nature of social interaction. Thus, it is critical to consider the child's contributions to mother–child interaction and the long-term effects that mutual negativity may have on mothers' development. During toddlerhood, children tend to be more emotionally negative (Bridgett et al., 2009; Lipscomb et al., 2011), such that this is a period of development that may be particularly sensitive to mutual negativity. Child behavior problems contribute to later parental stress and depressive symptoms (e.g. Gross et al., 2008; Hammen, Burge, & Stansbury, 1990). Thus, it follows that the interactions of toddlers and their mothers with depressive symptoms could be highly mutually negative because of contributions from both mothers and children.
The qualities of dyadic interaction itself could also influence later parent and child characteristics. For example, Leadbeater et al. (1996) found that positive contingent interactions between mothers and their 20-month-old children about a new toy were negatively correlated with maternal depressive symptoms 8–16 months later. Despite the normative increase in negativity during toddlerhood and the key role that negative affect plays in depression, to date, the specific impact of mutual negative exchanges over time between mothers and children in early childhood on maternal depressive symptoms remains unexamined. Although the literature is clear that there is a concurrent association between maternal depressive symptoms and negative dyadic exchanges, the longitudinal directionality of these associations is less clear. Transactional influences could occur through intersecting and overlapping pathways (e.g. genetics, parent–child facial, vocal and physical behaviors, parenting strategies and parent–child symptomatology); thus, beginning to tease apart the primary contributors to transactional influence could prove critical in informing targets for interventions.
Genetically Informed Samples
Given known genetic influences on depression and negative temperament, it is difficult to disentangle the child's contributions to dyadic interaction in studies of biologically related families. Children reared by their biological parent(s) share genes with their parent(s); thus, it is impossible to determine whether children's patterns of responses to the parent reflect shared genes with the parent or the effect of parenting behaviors associated with depression. For example, if a toddler of a depressed parent were to cry and fuss more often than other children, in biologically related families, we could not discern whether this child behavior was due to shared genetic risk with the parent's psychopathology (e.g. crying as an early expression of the same genetic liability expressed in adults as depressive symptoms), environmental risk (e.g. withdrawn or negative parenting) or an interaction of risk factors. By clarifying the roles of genetic and environmental factors, targeted intervention strategies and goals such as promotion of child regulation, treatment of parental depression, or promotion of positive parent–child interaction patterns can be focused to maximize their potential efficacy.
In one genetically informed study with adoptive families, with both adoptive and biological children, in dyads where mothers and children had greater reciprocity, regardless of whether the reciprocity was between adopted or biological children, the children had fewer behavior problems, demonstrating a link between reciprocity and outcomes unrelated to genetic similarity (Deater-Deckard & Petrill, 2004). Genetically informed studies, such as adoption designs, can aid in understanding the child-driven contributions to parent–child interactions and can help to identify those contributions that are more likely to be associated with the early rearing environment.
Participants in the current study were from a longitudinal, prospective adoption study, the Early Growth and Development Study (EGDS; Leve et al., 2013). Previous work from the EGDS has found that both birth parent depressive symptoms and adoptive parent depressive symptoms were linked with child behavior, suggesting both genetic and environmental influences on children's behavior (Kerr et al., 2013; Laurent et al., 2013; Natsuaki et al., 2010; Natsuaki et al., 2014; Pemberton et al., 2010; Rhoades et al., 2011). Birth mother depressive symptoms, indicative of genetic risk, have been associated specifically with later child externalizing problems in toddlerhood (Kerr et al., 2013; Pemberton et al., 2010) and have been implicated in the association between child fussiness and adoptive mother (AM) responsiveness (Natsuaki et al., 2010). However, this prior research has relied on questionnaire measures of child and parent behavior, which provides information about broad characteristics of individuals. Longitudinal transactions between maternal depressive symptoms and mutual negativity in mother–child interaction may be found only for children with certain genetic risk. Previous studies from the EGDS have found that children at genetic risk for depression may be more reactive, fussy and emotionally dysregulated in toddlerhood (Natsuaki et al., 2010; Pemberton et al., 2010), which could potentiate the effects of maternal depressive symptoms on parent–child interaction. Moreover, child behaviors associated with genetic risk may exacerbate parents' stress, frustration and rejection felt in negative parent–child interactions that could contribute to an increase in maternal depressive symptoms. We expected that adopted children's genetic risk for depression, indexed by birth mothers' depressive symptoms, would moderate the transactional associations between adoptive mothers' depressive symptoms and the mutual negativity in mother–child interaction. Specifically, we hypothesized that in dyads with children at greater genetic risk, the bidirectional associations between adoptive mothers' depressive symptoms and mutual negativity in moment-to-moment interactions would be stronger than in dyads with children at lower genetic risk.
Microanalytic Dyadic Interactions
Similar to other approaches focused on the intensive study of parent–child interactions (e.g. Cole et al., 2003; Dix, Meunier, Lusk, & Perfect, 2012; Dumas et al., 1995), the current study used microanalytic coding. Microanalytic coding refers to coding discrete behaviors on a moment-to-moment basis. Brief periods of dyadic interaction analysed microanalytically have significant associations with a variety of parent and child characteristics, such as between child physiological regulation and dyadic synchrony (Moore & Calkins, 2004), prenatal cocaine exposure and dyadic engagement (Tronick et al., 2005), child conduct problems and greater mutual negative emotion (Cole et al., 2003) and maternal depression and greater matched negative affect (Field et al., 1990). We expected that analysis of behaviors that had been observed at the microanalytic level would better capture the reciprocal quality of parent–child interactions than broad questionnaire measures and illuminate developmental pathways not evident when measured by ratings describing either individual alone (i.e. checklists of child problem behaviors, parent depression symptomatology questionnaires and observations of the child or parent alone). For example, if a child expressed negative affect from the start to the end of the interaction, a global rating of child behavior would be likely to describe the entire interaction as negative but would not provide information about the context of the child's behavior by accounting for the contribution of the parent's behavior. Studies comparing micro-level and macro-level coding are quite rare, although two studies from one research group found micro-coded and macro-coded ratings of maternal responsiveness to be unrelated (Lohaus, Keller, Ball, Elben, & Voelker, 2001; Voelker, Keller, Lohaus, Cappenberg, & Chasiotis, 1999), and some suggest that the two coding systems do not represent the same underlying concept (Mesman, 2010). We utilized the microanalytic approach, which we expected to illuminate how mood and affective state (depressive symptoms) associated with everyday, specific and contingent behaviors between parent and child could have long-term effects.
In the current study, we coded each second of a brief parent–child interaction and determined, through the use of contingency analyses, to what degree one partner's behaviors were related to the other's. This methodological strategy also allowed us to control for within-person continuity of behavior (autocorrelation) so that change in one person's behavior could be attributed solely to the other person's prior behavior. Thus, a child factor (e.g. being more generally fussy) would not be mistaken as a parent–child dyadic factor.
There are various ways to quantify contingency in dyadic interaction. In this study, we focused on mutual contingent negative behaviors, based on the theory that maternal depressive symptoms have been shown to lead to more mutually negative parent–child interactions (e.g. Cohn & Tronick, 1989; Field et al., 1989) and that negative parent–child interactions are often cascading in nature (e.g. Patterson, 2002) and can lead to poor child outcomes (e.g. Cole et al., 2003). The current study examined the likelihood of a child's negative behavior following the mother's negative behavior in the next second, and the reverse—the likelihood of a mother's negative behavior following the child's negative behavior. This type of analysis captures the temporal unfolding of mutual negativity and goes beyond determining whether the interaction is broadly negative to describe more specifically in what way and in what temporal pattern. We expected that maternal depressive symptoms would increase the likelihood that children would respond negatively to mothers' negative behaviors and the likelihood that mothers would respond negatively to their children's negative behaviors. Similarly, we expected that mutual negativity could exacerbate later maternal depressive symptoms.
We controlled for child negative temperament, a phenotypic trait observed by the child's adoptive mother. Past research has found concurrent associations between parent-rated temperament and observations of parent–child interaction (e.g. Webster-Stratton & Eyberg, 1982). Child negative temperament was considered as a possible factor in predicting the later quality of the parent–child interaction, as well as contributing to later maternal depressive symptoms. As mentioned earlier, it is critical to consider child factors contributing to maternal depressive symptoms and the parent–child interaction in transactional models.
This study adds to previous findings from this sample by examining how maternal depressive symptoms may influence mutual negativity in parent–child interaction during toddlerhood and how, in turn, mutual negativity of parent–child interaction might influence changes in subsequent maternal depressive symptoms. By examining transactional patterns over time in an adoption sample, where the rearing (adoptive) parents and children do not share genes, associations between maternal depressive symptoms and parent–child interaction cannot be driven by shared genetics. This study also explored whether BM depressive symptoms, an index of genetic influences on liability to problems in the child, moderated the association between adoptive mothers' depressive symptoms and mutual negativity between child and adoptive mother.
We hypothesized the following: (1) higher levels of adoptive mother depressive symptoms when the child was 9 months of age would predict greater mutual negativity in mother–child interaction at child age 18 months; (2) greater mutual negativity in mother–child interaction at child age 18 months would be associated with higher levels of maternal depressive symptoms at child age 27 months; and (3) mutual negativity in mother–child interaction of children who are at risk due to birth mother depressive symptoms would be more strongly predicted by earlier adoptive mother depressive symptoms and would more strongly predict later adoptive mother depressive symptoms than children who are at a lower risk owing to birth mother depressive symptoms.
Method
Participants
Participants were from the longitudinal, multisite EGDS (Leve et al., 2013). The sample consisted of 361 adopted children who participated in Cohort I, each linked to adoptive parents and birth parents. Most (N = 343, 95%) of the adoptive parent couples were mothers and fathers; 18 (5%) were same-sex couples. Prior to testing this study's hypotheses, differences between opposite-sex and same-sex couples in depressive symptoms, parent behaviors in the parent–child interaction and the relations between depressive symptoms and parent–child factors were systematically examined. No significant differences were found; therefore, same-sex couples were included in the analyses, and the included parents will be referred to as mothers for parsimony throughout.
Participants met the following eligibility criteria: (1) the adoption placement was domestic; (2) the infant was placed within 3 months postpartum; (3) the infant was placed with a nonrelative adoptive family; (4) the infant had no known major medical conditions such as extreme prematurity or extensive surgeries; and (5) the birth and adoptive parents were able to read or understand English at the eighth-grade level. Retention rates remained high throughout the course of the study (97% for adoptive families and 95% for birth mothers). Additional details about the study design and sample description can be found elsewhere (Leve et al., 2013).
The data used to test hypotheses were drawn from the first three waves of assessment. Approximately half of the children (43%) were female. The median child age at placement was 3 days (SD = 13 days). Table 1 provides additional demographic information.
Table 1. Demographics for birth parents and adoptive parents.
| Variable | BM | BF | AM | AF |
|---|---|---|---|---|
| Mean age (years) at first wave of data collection | 23.83 ± 6.12 | 25.31 ± 7.42 | 36.96 ± 5.55 | 37.89 ± 5.93 |
| Race (%) | ||||
| Caucasian | 78 | 63 | 93 | 92 |
| African American | 11 | 20 | 4 | 5 |
| Hispanic/Latino | 4 | 8 | 1 | 1 |
| Multi-ethnic | 5 | 5 | 2 | 2 |
| Othera | 2 | 4 | 1 | 1 |
| Mean education level | 5 | 5 | 9 | 9 |
| Median annual house income | $14 000 | $21 000 | $100 000 | |
| Mean number of individuals in home | 3.6 | 3.5 | 3.7 | |
BM, birth mother; BF, birth father; AM, adoptive mother; AF, adoptive father. Education scores were as follows: 1 (less than eighth grade), 2 (completed eighth grade), 3 (completed 12th grade), 4 (some trade school), 5 (completed trade school), 6 (some junior college), 7 (completed junior college), 8 (some college), 9 (completed college), 10 (some graduate/professional school) and 11 (completed graduate/professional school).
Includes Asian, Native American/Pacific Islander, American Indian/Alaskan Native and unknown.
Study Design
Birth parent and adoptive family in-person assessments were conducted by interviewers who completed a minimum of 40 h of training, including a 2-day group session, pilot interviews, and videotaped feedback prior to administering interviews with study participants. All birth parent assessments were conducted in a location convenient to the participant, most often at home. The first birth parent interview occurred 3–6months (average of 4 months) postpartum, and the second was at 18 months. Adoptive family assessments occurred at child ages 9, 18 and 27 months. All in-person assessments lasted 2–3 h and included a collection of mailed self-report booklets, computer-assisted personal interview questions and interviewer impressions. The first birth parent assessment also included a pregnancy history calendar about the birth mother's drug use, mental health and stress during pregnancy, and each adoptive family assessment included a series of videotaped interaction and standardized tasks. For brevity, BM will refer to birth mother, BF to birth father, AM to adoptive mother and AF to adoptive father.
Measures
Mother depressive symptoms
AM depressive symptoms were assessed at all three measurement occasions (child ages 9, 18 and 27 months) using the Beck Depression Inventory (BDI; Beck & Steer, 1993). BM depressive symptoms were assessed at 4 months using the BDI. The BDI is a commonly used instrument that assesses the presence of 21 symptoms of depression. In the present study, 20 of the 21 items were administered. The suicidal ideation item was removed to minimize situations where emergency clinical follow-up would be needed, because of the difficulty in providing effective clinical follow-up in a timely and effective manner in a nationally distributed sample (Leve et al., 2010).
AM and BM depressive symptoms were calculated as the sum of the 20 BDI items (α = 0.71, 0.79 and 0.84); 0–13 is considered minimal range, 14–19 is considered mild, 20–28 is considered moderate and 29–63 is severe. See Table 2 for means and standard deviations.
Table 2. Descriptive statistics of and correlations among dependent and independent variables.
| Variable | Mean | SD | 1 | 2 | 3 | 4 | 5 | 6 |
|---|---|---|---|---|---|---|---|---|
| 1. AM depressive symptoms (9 months) | 3.59 | 3.15 | 1 | |||||
| 2. AM depressive symptoms (18 months) | 3.75 | 3.85 | 0.61** | 1 | ||||
| 3. AM depressive symptoms (27 months) | 3.87 | 4.30 | 0.57** | 0.61** | 1 | |||
| 4. CHNeg to AMNeg (18 months) | 0.01 | 0.07 | 0.12* | 0.01 | 0.10 | 1 | ||
| 5. AMNeg to CHNeg (18 months) | 0.01 | 0.08 | 0.07 | 0.03 | −0.07 | 0.07 | 1 | |
| 6. BM depressive symptoms (4 months) | 11.18 | 9.78 | −0.05 | −0.06 | −0.10 | 0.00 | −0.01 | 1 |
AM, adoptive mother; BM, birth mother; CHNeg to AMNeg, the degree of likelihood that a child responds negatively to AM's negative behavior; AMNeg to CHNeg, the degree of likelihood that AM responds negatively to child's negative behavior.
p < 0.05;
p < 0.01.
Adoptive mother and child interaction
To examine parent and child behaviors during social interaction, AMs and their children were observed in a 3-min Parent–Child Teaching task at 18 months. Dyads were presented with a toy that is challenging for most children at 18 months to play with (a puzzle with large puzzle pieces) and instructed to complete the task together. The task was completed on a large square mat in families' homes, and attempts to minimize distractions (e.g. other children, pets and toys) were made. Observational studies frequently use teaching tasks in which parents are instructed to show their children toys and to encourage parent–child engagement (e.g. NICHD Early Child Care Research Network, 2006). In most previous research, the teaching task procedure has been used to assess parenting using global ratings of constructs including support for children's engagement, sensitivity, positive regard, intrusiveness and supportive presence (Egeland & Hiester, 1993).
The task was coded using a microcoding system (Moore, Teti, & Roben, 2009) adapted from existing parent–child interaction rating scales (Cohn & Tronick, 1988; Moore & Calkins, 2004; Moore, Cohn, & Campbell, 2001). Discrete parent and child behaviors were coded in domains of object interaction (e.g. approach and explore), physical activity (e.g. throw and cuddle), attention (e.g. look at parent) and social–emotional (e.g. social initiation, resistance and negative touch). Codes were assigned at 1-s intervals and were not mutually exclusive.
Teams of coders, naïve to the hypotheses of the study, were trained by the first author, and separate teams conducted the coding for parent and child behaviors using an observational coding and analysis software package (Interact with p.a.t.t.e.r.n. analysis module; Mangold International) to facilitate coding and provide sophisticated data management and analysis functionality. To establish inter-rater reliability of codes, subsets of the cases were double-coded. For child behaviors, 19% of cases were double-coded (κ = 0.74), for codes used in this study. For mother behaviors, 22% were double-coded (κ = 0.79).
One of the advantages of discrete microcoding is that behaviors can be combined in modular ways to create constructs of interest. The focus of the current study was the positive and negative contingent responsiveness. To create variables of interest for contingency analysis, theoretically relevant mother and child codes were combined to create scores for data analysis. For the mother, the combined variables were the following: (1) Mother Positive (codes included engage child with the toy, scaffold child's use of the toy, and positive touch) and (2) Mother Negative (codes included negative touch, take toy away from child, explore toy without child, look away from child and toy, and disengaged). For the child, combined variables were the following: (1) Child Positive (look at parent, play appropriately with toy, approach toy, and social initiation) and (2) Child Negative (move outside of reach of parent, look away from toy or parent, off-task, and resist parent physically).
Time domain time-series methods were used to compute indices of contingent responsiveness for both AMs and their children. Contingent responsiveness was measured using dynamic factor models (Molenaar, 1985). Using LISREL 8.80 (Scientific Software International, Inc.), models were run for each dyad, in which contemporaneous and 1-s lagged associations within and between partners' behaviors were computed. Multiple indices of contingent responsiveness were computed, which represented variation in one person's behavior that was explained by the other person's behavior in the previous second, controlling for autocorrelation in each person's behavior.
Because the aim of the current study was to understand the role of mutual negativity, this study focused on contingent responsiveness indices that were computed to represent the degree to which child negative behaviors were contingent on mother negative behaviors in the previous second (CHNeg to AMNeg; i.e. child negative response to AM negative behavior) and the degree to which mother negative behaviors were contingent on child negative behaviors (AMNeg to CHNeg). In addition, indices were computed to examine the degree to which a child responded negatively to any mother behavior and a mother responded negatively to any child behavior. These overall contingency indices were used as control variables. Controlling for the degree to which any mother behavior predicted child negative behavior (and vice versa) highlighted mutual negativity rather than general negative contingency. The details on calculating these variables are presented in the Results section.
Missing data
There were some missing data, with no more than 7% missing for any variable except for the videoed observational Teaching Task. Some video problems included missing video discs (N = 5) and some recordings that were unable to be coded because of video malfunction (N = 16). Furthermore, if there was no positive or negative behavior from the initiating partner for the examined behavior, then the score was computed as missing, leaving an N of 298 for the teaching task. Thus, because of non-overlapping missingness, our analytical sample ranged from 282 to 264.
Additional covariates
Child sex (coded as 0 for male and 1 for female) was a covariate. In addition, several other factors that could confound or result in misinterpretation of the findings were entered as covariates.
Infant fussiness
At 9 months, AMs and AFs completed an abridged version of the 24-month Infant Characteristics Questionnaire (ICQ; Bates, Freeland, & Lounsbury, 1979), which consists of 24 items rated on a seven-point scale with values of 7 indicating a very difficult temperament. The fussiness scale, which sums 6 out of the 24 items, was used in the present analyses (AM α = 0.81; AF α = 0.82). AM report of child fussiness was used in the current study.
Prenatal and neonatal complications
To disentangle prenatal and/or neonatal complications from genetic influences, a score was created that was adapted from the McNeil–Sjöström Scale for Obstetric Complications (Kotelchuck, 1994; McNeil & Sjöström, 1994). The level of prenatal risk was assigned to distinct risk factors, categorizing risk from 1 (not harmful or relevant) to 6 (very great harm or deviation to offspring) (Marceau et al., 2013). The items that comprised the score were taken from five categories of complications: (1) toxin exposure (exposure to radiation, X-ray, lead and chemicals); (2) drug and alcohol use (cigarettes, second-hand cigarette smoke, alcohol, marijuana, cocaine, amphetamines, heroin, prescription pain killers, inhalants, sedatives and tranquilizers); (3) pregnancy risk (circulatory problems, infections, maternal age, prenatal care, weight gain and loss, nausea, bleeding and foetal movement); (4) preeclampsia risk (e.g. high blood pressure); and (5) neonatal risk factors (e.g. low birthweight). The scale generated a score for each BM based on retrospective self-report of pregnancy and neonatal events. Events meeting a minimum threshold of being at least potentially harmful or relevant to infant outcome were summed to form a total score. The McNeil–Sjöström Scale has been shown to have predictive validity (Nicodemus et al., 2008) and to be more sensitive than other common measures of obstetric complications (McNeil, Cantor-Graae, & Sjöström, 1994). In the EGDS data, prenatal risk was found to relate to BM mental health characteristics and adopted toddler internalizing problems (Marceau et al., 2013).
Results
Descriptive statistics of primary study variables were computed with SPSS 20.0. The study variables' N's, means, standard deviations and ranges are presented in Table 2. Analyses were completed with participants who had completed all measures in each regression, resulting in N's ranging from 264 to 282. Correlations among primary independent and dependent variables are presented in Table 2.
The first step in data preparation was to compute indices that represented mutual negativity, which would be used to test the degree to which AM depressive symptoms contributed to this dyadic process. Of the multiple approaches one can take to assess contingency in dyadic interaction, we chose dynamic factor analysis, one idiographic method for examining causal relations in a time series. (Fisher, Newman, & Molenaar, 2011; Molenaar, 1985). We chose this method because it accounts for within-time associations between partners and within-subject continuity or autocorrelation, which then allows for the causal effects between partners to be estimated, provided there is not a third unknown variable that explains the association. A vector autoregressive (VAR) model with a lag of 1 s was tested. A VAR analysis was run for each AM–child pair in lisrel 8.80, and the causal effects between partners were extracted. That is, variables were extracted that represented how one partner's behavior at time t predicted the other partner's behavior at time t + 1. The λ matrix of factor loadings was set to identity matrix, and the θ matrix of measurement error variances was fixed at zero, restrictions that are necessary in LISREL for analysing relations between latent variables with single manifest variables. The cross-lagged parameters from the β matrix were then extracted from each dyad. Because each model was saturated, the fit of each of the models cannot be evaluated.
The extracted β's for each dyad were the indices computed to represent the likelihood that one partner's negative behavior would follow the other's, accounting for within-time similarity and each partner's own autocorrelation. That is, if CHNeg to AMNeg for one dyad has a positive β, it is likely that the AM's negative behaviors are followed by negative behaviors from the child. Higher β values indicate greater likelihood. If CHNeg to AMNeg is negative, then it is unlikely that the AM's negative behaviors are followed by child negative behaviors.
Do Adoptive Mother Depressive Symptoms at 9 Months Predict Child Negative Response to Adoptive Mother Negative Behavior (CHNeg to AMNeg) at 18 Months and is the Effect Moderated by Birth Mother Depressive Symptoms?
Negative contingency was examined for longitudinal associations with AM depressive symptoms. We tested whether AM depressive symptoms at 9 months was associated with CHNeg to AMNeg at 18 months after controlling for concurrent depressive symptoms (18 months), perceived child temperament at 9 months, child sex, prenatal risk factors and the degree to which the child responded negatively to any AM behavior (i.e. a measure of child's overall negative contingent responsiveness). The degree to which AM depressive symptoms at 9 months predicted CHNeg to AMNeg at 18 months was tested using hierarchical linear regression. The first step included all controls. The second step added AM depressive symptoms at 9 months to test if it was longitudinally associated with CHNeg to AMNeg over and above the control variables added on the first step. The second step also included BM depressive symptoms in order to include the main effect for the moderation term in Step 3. Step 3 included the moderation term between AM depressive symptoms at 9 months and BM depressive symptoms. Step 1 of the model was not significant, R = 0.19, Adj. R2 = 0.02, F(5, 271) = 2.00, p < 0.10. With the unique variance added by the inclusion of the maternal depression in Step 2, the model reached significance. In Step 2, only AM depressive symptoms at 9 months and the degree to which the child responded negatively to any AM behavior were significant predictors. Step 3 was not significant, and no unique variance was added by the moderation term (see Table 3).
Table 3. Regression coefficients for AM depressive symptoms at 9 months predicting child negative response to mother negative behaviors at 18 months.
| β | B | F change | R2 change | |
|---|---|---|---|---|
| Step 1 | ||||
| Child gender | −0.04 | −0.00 | ||
| IBQ fussiness (9 months) | 0.01 | 0.00 | ||
| Prenatal risk factors | −0.03 | −0.00 | ||
| AM depressive symptoms (18 months) | −0.02 | −0.00 | ||
| Child negative response to any AM behaviors | 0.18** | 0.01** | ||
| Step 2 | ||||
| AM depressive symptoms (9 months) | 0.15* | 0.01* | ||
| BM depressive symptoms (4 months) | −0.04 | 0.00 | 2.33† | 0.02† |
| Step 3 | ||||
| AM depressive symptoms (9 months) by BM depressive symptoms (4 months) | 0.01 | 0.00 | 0.03 | 0.00 |
| Total model F and adj. R2 for Step 2 | F = 2.11* | Adj. R2 = 0.03* |
β is the standardized regression coefficient at entry; B is the unstandardized regression coefficient at entry. N = 277.
IBQ, Infant Behavior Questionnaire; AM, adoptive mother; BM, birth mother.
p < 0.10;
p < 0.05;
p < 0.01.
Does Child Negative Response to Adoptive Mother Negative Behavior (CHNeg to AMNeg) at 18 Months Predict AM Depressive Symptoms at 27 Months and is the Effect Moderated by Birth Mother Depressive Symptoms?
Next, CHNeg to AMNeg at 18 months was examined as a predictor of later AM depressive symptoms at 27 months using hierarchical regression. BM depressive symptoms were tested as a moderator of this association. The first step included all controls: AM depressive symptoms at 18 months, perceived child temperament at 9 months, child sex, prenatal risk factors and the degree to which the child responded negatively to any AM behavior. The second step added CHNeg to AMNeg to test if it was associated with AM depressive symptoms at 27 months above and beyond the control variables added on Step 1. The second step also included BM depressive symptoms to test the main effect for the moderation term in Step 3. Step 3 included the moderation term between AM depressive symptoms at 9 months and BM depressive symptoms. Step 1 of the model was significant, R = 0.59, Adj. R2 = 0.33, F(5, 258) = 27.32, p < 0.001. Prenatal risk factors and AM depressive symptoms at 18 months were significant predictors. Unique variance was not added by Step 2. Neither BM depressive symptoms nor CHNeg to AMNeg were significant predictors. However, unique variance added by Step 3 reached significance. In this final step, the moderation term of CHNeg to AMNeg and BM depressive symptoms was a significant predictor (Table 4).
Table 4. Regression coefficients for the moderation of child negative responses to AM negative behaviors at 18 months predicting AM depressive symptoms at 27 months by BM depressive symptoms.
| β | B | F change | R2 change | |
|---|---|---|---|---|
| Step 1 | ||||
| Child gender | 0.09 | 0.10 | ||
| IBQ fussiness (9 months) | 0.10† | 0.11† | ||
| Prenatal risk factors | 0.11* | 0.12* | ||
| AM depressive symptoms (18 months) | 0.56** | 0.62** | ||
| Child negative response to any AM behaviors | 0.04 | 0.04 | ||
| Step 2 | ||||
| CHNeg to AMNeg | 0.10† | 1.48† | ||
| BM depressive symptoms (4 months) | −0.04 | −0.01 | 2.32† | 0.01† |
| Step 3 | ||||
| CHNeg to AMNeg by BM depressive symptoms (4 months) | 0.12* | 0.15* | 5.12* | 0.01* |
| Total model F and adj. R2 | F = 18.76** | Adj. R2 = 0.35** |
β is the standardized regression coefficient at entry; B is the unstandardized regression coefficient at entry. N = 264.
IBQ, Infant Behavior Questionnaire; AM, adoptive mother; BM, birth, mother; CHNeg to AMNeg, the degree of likelihood that a child responds negatively to AM's negative behavior.
p < 0.10;
p < 0.05;
p < 0.001.
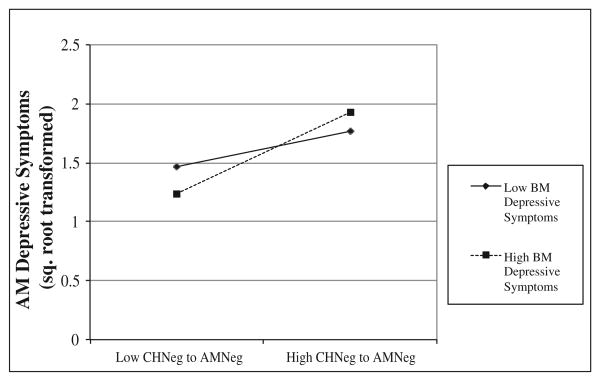
To better understand the significant moderation, simple slopes were tested (Aiken & West, 1991; Dawson, 2014). Simple slope analyses were conducted with a macro (Hayes & Matthes, 2009) in SPSS 20.0. Significance was tested at a value of 19 for the moderator (19 is at least a moderate level of depressive symptoms, as indicated in manual guidelines for interpreting the BDI and accounting for one BDI item not being asked; Beck & Steer, 1993). The simple slope of CHNeg to AMNeg was significant at high levels of BM depressive symptoms (levels of 19 and above), B = 7.79, t = 3.96, p < 0.0001, and nonsignificant at low levels of BM depressive symptoms (18 months and below), B = 0.44, t = 0.54, p = ns. The simple slopes, plotted in Figure 1, show that CHNeg to AMNeg was associated with AM depressive symptoms at 27 months only for children whose BMs reported high levels of depressive symptoms.
Figure 1.
Moderation of CHNeg to AMNeg at 18 months predicting 27-month AM depressive symptoms by BM depressive symptoms. Low and high BM depressive symptoms were determined using a cut-off of 19 (at least moderate depression). BM, birth mother; AM, adoptive mother; CHNeg to AMNeg, the degree of likelihood that a child responds negatively to AM's negative behavior.
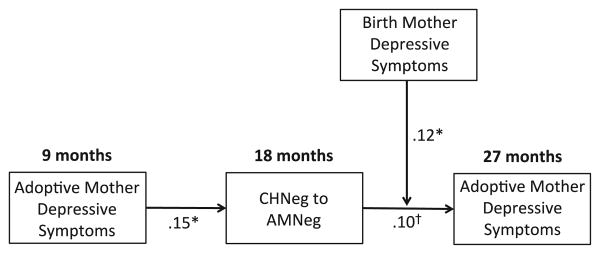
The combined results of the longitudinal associations between AM depressive symptoms and CHNeg to AMNeg are illustrated in Figure 2.
Figure 2.
Representation of two longitudinal hierarchical regressions tested between adoptive mother (AM) depressive symptoms and child negative response to AM negative behavior. CHNeg to AMNeg, the degree of likelihood that a child responds negatively to AM's negative behavior. †p < 0.10, *p < 0.05.
Do Adoptive Mother Depressive Symptoms at 9 Months Predict Adoptive Mother Negative Response to Child Negative Behavior (AMNeg to CHNeg) at 18 Months and is the Effect Moderated by Birth Mother Depressive Symptoms?
We next tested the same regression models as presented earlier, this time examining mothers' negative behavior contingent on prior child negative behavior, that is, AMNeg to CHNeg. We tested whether AM depressive symptoms at 9 months was associated with AMNeg to CHNeg at 18 months after controlling for concurrent depressive symptoms (18 months), perceived child temperament at 9 months, child sex, prenatal risk factors and the degree to which the AM responded negatively to any child behavior. The first step included all controls and the second step added AM depressive symptoms at 9 months to test if it was longitudinally associated with AMNeg to CHNeg over and above the control variables added on the first step. The second step also included BM depressive symptoms in order to include the main effect for the moderation term in Step 3. Only Step 1 of the model had significant unique variance, R = 0.27, Adj. R2 = 0.06, F(5, 271) = 4.38, p < 0.05, with the degree to which the AM responded negatively to any child behavior as the only significant predictor (β = 0.25, p < 0.05). No unique variance was added by any of our variables of interest, suggesting no association between AM depressive symptoms at 9 months and AMNeg to CHNeg.
Does Adoptive Mother Negative Response to Child Negative Behavior (AMNeg to CHNeg) at 18 Months Predict Adoptive Mother Depressive Symptoms at 27 Months and is the Effect Moderated by Birth Mother Depressive Symptoms?
We tested whether AMNeg to CHNeg at 18 months was associated with AM depressive symptoms at 27 months after controlling for concurrent depressive symptoms (18 months), perceived child temperament at 9 months, child sex, prenatal risk factors and the degree to which the AM responded negatively to any child behavior. As before, the first step included all controls and the second step added AMNeg to CHNeg to test if it was longitudinally associated with AM depressive symptoms at 27 months over and above the control variables added on the first step. The second step also included BM depressive symptoms to test the main effect for the moderation term in Step 3. Only Step 1 of the model had significant unique variance, R = 0.59, Adj. R2 = 0.33, F(5, 258) = 27.43, p < 0.001, with depressive symptoms at 18 months (β = 0.55, p < 0.001) and prenatal risk factors (β = 0.11, p < 0.05) as the only significant predictors. No unique variance was added by any of the variables of interest, suggesting no association between AMNeg to CHNeg and AM depressive symptoms at 27 months.
Discussion
Bidirectional associations are often overlooked in the literature, particularly when considering transactional effects on parent well-being (Gross et al., 2008; Pardini, 2008). In particular, the moment-to-moment mutual exchange of negative emotion, which is associated with both maternal depression and child behavior problems (Cole et al., 2003; Field et al., 1990), is an important area for transactional research given its potential as a target for parent–child intervention. This is the first study to examine longitudinal transactional associations between parent depressive symptoms and the qualities of the moment-to-moment parent–child dyadic interaction using a genetically informed adoption design. AM depressive symptoms at 9 months increased the likelihood that, at 18 months, children reacted negatively to their mothers' negative behavior, which in turn predicted higher levels of AM depressive symptoms at 27 months. This finding demonstrates a postulate of the transactional model: that a quality of the dyad, a quality that is determined by both parent and child behaviors, is influenced by earlier parent symptomatology, and vice versa. Moreover, these associations were found in an adoption sample, which demonstrates that the associations were not due to passive gene–environment correlation, that is, that the associations between parent and child are not due to underlying genetic factors that influence the trait in both parent and child.
Specifically, this pattern of findings suggested a direct environmental influence of maternal depressive symptoms on children's tendency to engage in mutually negative interactions, which, in turn, predicted the development of mothers' symptoms of depression 9 months later. The first association replicates well-established correlations in the literature between maternal depressive symptoms and the quality of parent–child interaction (Goodman & Gotlib, 1999). The latter association could also be due to genetically influenced characteristics of the child, unmeasured in this report, on later parent depression symptoms. Overall, the findings highlight the transactional nature of the caregiving environment for both parents and children, pointing to moment-to-moment and longitudinal effects of each partner on the other. Moreover, these findings suggest that targeting the early parent–child relationship for intervention could help reduce the development and impact of maternal depression. The importance of the current findings to understanding the developmental course of maternal depression during the postpartum period and beyond makes a contribution to existing research, which has traditionally examined maternal depression in relation to children's development only (e.g. Bakermans-Kranenburg, van IJzendoorn, & Juffer, 2003; cf. Gross et al., 2008).
A measure of perceived child negative temperament was accounted for in the analyses, indicating that observed patterns of early mother–child mutual negativity predicted maternal depression above and beyond the mothers' perceptions of children's temperamental negativity. Thus, relations were not due to method variance as a function of maternal report. At the same time, moderation by BM depressive symptoms suggests that the association between mother–child mutual negativity at 18 months and later AM depression was not the same for all dyads. AMs' depressive symptoms at 27 months were predicted by the degree to which children negatively responded to their mothers' negative behaviors at 18 months, but only when children had a BM with elevated levels of depressive symptoms. Furthermore, this genetically based sensitivity or reactivity was related to mutual negativity in a manner that led to increased depressive symptoms in mothers.
This is not the first study to find transactional effects only in the context of risk. Ciciolla, Gerstein, and Crnic (2013) found longitudinal bidirectional effects, when children were of preschool age, between maternal psychological distress and child internalizing problems, but only if the children also had developmental delays, the majority of which were in language and cognition. The authors interpreted this moderation as a possible indication of greater vulnerability within the mother–child relationship due to the delay. The presence of the developmental risk could make mothers more susceptible to transactional distress due to child symptoms.
Our findings suggest that the child's genetic make-up, independent of our measure of perceived temperament, may influence the transactional interaction. Perhaps children at genetic risk for depression react with more intensity or more with more negative emotionality when disciplined or restricted by their parents. Offspring of parents with depression have been found to have poorer strategies for regulating emotion (e.g. Silk, Shaw, Skuban, Oland, & Kovacs, 2006), although literature specifying this as a genetic effect, such as identifying candidate genes associated with reactivity to emotions (Hariri et al., 2005), is limited. We also found that obstetric complications significantly predicted AM's depressive symptoms at 27 months. Thus, similar or related to the genetic vulnerability, it seems likely that there is a child characteristic related to perinatal complications that is involved in this transactional interaction that is not captured with our parent-reported measures of early temperament. Previous studies with the EGDS population have found associations between genetic risk, prenatal risk factors and toddler behavior problems through prenatal risk factors (Marceau et al., 2013; Pemberton et al., 2010). Pemberton et al. found that children with more prenatal risk had higher externalizing symptoms at 27 months. It may be that the intensity and/or frequency of children's negative behaviors or negative reactivity is greater in those at genetic risk and/or with obstetric problems. Our coding did not take into account the intensity of the behaviors, which would be an important area for future research.
Notably, we found significant effects of one mutually negative transactional variable on the development of maternal depressive symptoms. Only children's negative responses to their mothers' negative behaviors, and not vice versa, were associated with earlier and later depressive symptoms. The longitudinal association between children reacting negatively to negative parent behaviors and later maternal depressive symptoms, particularly in children who are also at risk genetically, could be explained by parental feelings of inadequacy or rejection that contribute to depressive symptomatology. Mothers who perceive their infants as more reactive (Leerkes & Burnery, 2007) are at higher risk for low feelings of efficacy during infancy, which is associated with maternal depression (Teti & Gelfand, 1991). It may be that the mother restricts the child's play or is disengaged during play and as a result the young child reacts negatively, perhaps in an effort to elicit a response. This may then lead to sustained or exacerbated depressive symptoms later, when the child is 27 months of age. This pattern could be illustrative of a negative cycle of parent and child behaviors, not unlike Patterson's (2002) coercive models of children's aggressive behaviors. Mothers' reactions to their children's negative behaviors may be less associated with earlier and later depressive symptomatology but instead be related to current contextual events or feelings.
Longitudinal data that are observational and microanalytic allow for the objective analysis of the dyad beyond factors associated uniquely with each individual. Data supporting the importance of dyadic interaction, and moving beyond research or interventions that address child problems or parent problems in isolation, call for consideration of relational influences in interventions aimed to improve either parent or child symptoms associated with parental depression. Interventions for at-risk children in early childhood such as the Attachment and Biobehavioral Catch-up (Dozier et al., 2006) and Parent–Child Interaction Therapy (Zizzer & Eyberg, 2010) focus on intervening at the level of the dyad's interaction, not only on changing global qualities of parenting behavior. Such interventions assist parents to tailor responses to their children's specific behaviors and to note how children respond to the parents' behaviors. This study lends support for such an approach, finding that a dyadic quality of mutual negativity characterized by children's negative responses to mothers' negative behaviors has longitudinal effects on the mother's depressive symptoms, emphasizing a need for intervening early to improve patterns of interaction.
A limitation of this study is that it does not include child outcomes in the model. Further analysis, including observed child behaviors, such as emotional negativity, disruptive behavior problems, attention problems, and impulsivity, is warranted and could potentially capture some of the variance suggested by the significance of obstetric risk and moderation by genetic risk. It will be important to observe how child behaviors, maternal depressive symptoms, and characteristics of the dyad change and influence one another over time. The inclusion of observational child outcomes may aid in accounting for more variance in our statistical models. Our models accounted for a small amount of the observed variance, particularly in predicting children's negative response to mothers' negative behavior, and this may be due to the challenge of predicting an observed variable that is not predicted by an earlier measure of the same variable. The first model was predicting the dyadic quality in our 3-min teaching task, a small snapshot of parent–child interaction that we are attempting to generalize to broader parent–child characteristics. Although this measure and this type of observation are used frequently in the literature (e.g. Denham, Renwick, & Holt, 1991; Jacobvitz & Sroufe, 1987), it is also possible that the brief interaction is one reason for the relatively small effects.
An additional limitation is that our genetic findings were with BMs only and were not replicated with depressive symptom data from BFs. We ran our analyses with our smaller sample of BFs for this study (N = 79) and did not find effects in the direction of the moderation we found with the BMs. Replication of the findings using BF data would have provided a strong confirmation of genetic effects because the effects from a BF to a child are not confounded with prenatal environmental factors, although we attempt to control for such factors by including obstetric complications in the model. Without BF data, we are including only half of the child's genetic make-up.
This study is the first that demonstrates transactional patterns between maternal depressive symptoms and mother–child mutual negativity in young children in an adoption sample. Notably, associations between mutual negativity and later maternal depressive symptoms were only found in dyads in which the child was at genetic risk. Findings suggest that the qualities of the rearing mother (depressive symptoms), child (prenatal and genetic risk) and dyad (child's negative behavior contingent on mother's negative behavior) influence one another over time and that intervening to change the dynamics of mother–child interaction could potentially have beneficial effects on later maternal depressive symptoms. Exploration of maternal depressive symptoms and parent–child interactions at the level of the dyad over time, as opposed to static assessment of individuals, provides a more complex and in-depth understanding of mutual influence, both momentary and long-term.
Acknowledgments
This project was supported by grant R01 HD042608 from the National Institute of Child Health and Human Development and the National Institute on Drug Abuse, NIH, U.S. PHS (PI Years 1–5: David Reiss, MD; PI Years 6–10: Leslie Leve, PhD). In addition, this project was supported by grant R01 MH092118 from the National Institute of Mental Health, NIH, U.S. PHS (PIs: Jenae Neiderhiser, PhD and Leslie Leve, PhD), and an individual fellowship F31 MH088015 awarded to the first author. The content is solely the responsibility of the authors and does not necessarily represent the official views of the Eunice Kennedy Shriver National Institute of Child Health and Human Development or the National Institutes of Health.
References
- Aiken LS, West SG. Multiple regression: Testing and interpreting interactions. Newbury Park, London: Sage; 1991. [Google Scholar]
- Bagner DM, Pettit JW, Lewinsohn PM, Seeley JR, Jaccard J. Disentangling the temporal relationship between parental depressive symptoms and early child behavior problems: A transactional framework. Journal of Clinical Child & Adolescent Psychology. 2013;42:78–90. doi: 10.1080/15374416.2012.715368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bakermans-Kranenburg MJ, van IJzendoorn JH, Juffer F. Less is more: Metaanalyses of sensitivity and attachment interventions in early childhood. Psychological Bulletin. 2003;129:195–215. doi: 10.1037/0033-2909.129.2.195. [DOI] [PubMed] [Google Scholar]
- Bates JE, Freeland CA, Lounsbury ML. Measure of infant difficulties. Child Development. 1979;50:794–803. [PubMed] [Google Scholar]
- Beck AT, Steer RA. Manual for the Beck Depression Inventory. San Antonio, TX: Psychological Corporation; 1993. [Google Scholar]
- Bridgett DJ, Gartstein MA, Putnam SP, McKay T, Iddins E, Robertson C, Rittmueller A. Maternal and contextual influences and the effect of temperament development during infancy and parenting in toddlerhood. Infant Behavior and Development. 2009;32:103–116. doi: 10.1016/j.infbeh.2008.10.007. [DOI] [PubMed] [Google Scholar]
- Brownell CA, Kopp CB. Socioemotional development in the toddler years: Transitions and transformations. New York: The Guilford Press; 2007. [Google Scholar]
- Ciciolla L, Gerstein ED, Crnic KA. Reciprocity among maternal distress, child behavior, and parenting: Transactional processes and early childhood risk. Journal of Clinical Child & Adolescent Psychology. 2013 doi: 10.1080/15374416.2013.812038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohn JF, Tronick EZ. Mother-infant face-to-face interaction: Influence is bidirectional and unrelated to periodic cycles in either partner's behavior. Developmental Psycho-pathology. 1988;24:386–392. [Google Scholar]
- Cohn JF, Tronick EZ. Specificity of infants' response to mothers' affective behavior. Journal of American Academy of Child & Adolescent Psychiatry. 1989;28:242–248. doi: 10.1097/00004583-198903000-00016. [DOI] [PubMed] [Google Scholar]
- Cole PM, Teti LO, Zahn-Waxler C. Mutual emotion regulation and the stability of conduct problems between preschool and early school age. Development and Psychopathology. 2003;15:1–18. [PubMed] [Google Scholar]
- Dawson JF. Moderation in management research: What, why, when, and how. Journal of Business and Psychology. 2014;29:1–19. [Google Scholar]
- Deater-Deckard K, Petrill SA. Parent–child dyadic mutuality and child behavior problems: An investigation of gene-environment process. Journal of Child Psychology and Psychiatry. 2004;45:1171–1179. doi: 10.1111/j.1469-7610.2004.00309.x. [DOI] [PubMed] [Google Scholar]
- Denham SA, Renwick SM, Holt RW. Working and playing together: Prediction of preschool social–emotional competence from mother–child interaction. Child Development. 1991;62:242–249. [Google Scholar]
- Dix T. The affective organization of parenting: Adaptive and maladaptive processes. Psychological Bulletin. 1991;110:3–25. doi: 10.1037/0033-2909.110.1.3. [DOI] [PubMed] [Google Scholar]
- Dix T, Meunier LN, Lusk K, Perfect MM. Mothers' depressive symptoms and children's facial emotions: Examining the depression–inhibition hypothesis. Development and Psychopathology. 2012;24:195–210. doi: 10.1017/S0954579411000770. [DOI] [PubMed] [Google Scholar]
- Dozier M, Peloso E, Lindhiem O, Gordon K, Manni M, Sepulveda S, Ackerman J. Developing evidence-based interventions for foster children: An example of a randomized clinical trial with infants and toddlers. Journal of Social Issues. 2006;62:765–783. [Google Scholar]
- Dumas JE, LaFreniere PJ, Serketich WJ. ‘Balance of power’: A transactional analysis of control in mother-child dyads involving socially competent, aggressive, and anxious children. Journal of Abnormal Psychology. 1995;104:104–113. doi: 10.1037//0021-843x.104.1.104. [DOI] [PubMed] [Google Scholar]
- Egeland B, Hiester M. Teaching task rating scales. University of Minnesota: Institute of Child Development; 1993. [Google Scholar]
- Field T, Healy BT, Goldstein S, Guthertz M. Behavior–state matching and synchrony in mother–infant interactions of nondepressed versus depressed dyads. Developmental Psychology. 1990;26:7–14. [Google Scholar]
- Field T, Healy BT, LeBlanc WG. Sharing and synchrony of behavior states and heart rate in nondepressed versus depressed mother–infant interactions. Infant Behavior & Development. 1989;12:357–376. [Google Scholar]
- Fisher AJ, Newman MG, Molenaar PCM. A quantitative method for the analysis of nomothetic relationships between idiographic structures: Dynamic patterns create attractor states for sustained post-treatment change. Journal of Consulting and Clinical Psychology. 2011;79:552–563. doi: 10.1037/a0024069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gelfand DM, Teti DM. The effects of maternal depression on children. Clinical Psychology Review. 1990;10:329–353. [Google Scholar]
- Goodman SH, Gotlib IH. Risk for psychopathology in the children of depressed mothers: A developmental model for understanding mechanisms of transmission. Psychological Review. 1999;106(3):458–490. doi: 10.1037/0033-295x.106.3.458. [DOI] [PubMed] [Google Scholar]
- Goodman SH, Rouse MH, Connell AM, Broth MR, Hall CM, Heyward D. Maternal depression and child psychopathology: A meta-analytic review. Clinical Child and Family Psychology Review. 2011;14:1–27. doi: 10.1007/s10567-010-0080-1. [DOI] [PubMed] [Google Scholar]
- Gross HE, Shaw DS, Burwell RA, Nagin DS. Transactional processes in child disruptive behavior and maternal depression: A longitudinal study from early childhood to adolescence. Development and Psychopathology. 2009;21:139–156. doi: 10.1017/S0954579409000091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gross HE, Shaw DS, Moilanen KL, Dishion TJ, Wilson MN. Reciprocal models of child behavior and depressive symptoms in mothers and fathers in a sample of children at risk for early conduct problems. Journal of Family Psychology. 2008;22:742–751. doi: 10.1037/a0013514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hammen C, Burge D, Stansbury K. Relationship of mother and child variables to outcomes in a high-risk sample: A causal modeling analysis. Developmental Psychology. 1990;26:24–30. doi: 10.1037/0012-1649.26.1.24. [DOI] [Google Scholar]
- Hariri AR, Drabant EM, Munoz KE, Kolachana BS, Mattay VS, Egan MF, Weinberger DR. A susceptibility gene for affective disorders and the response of the human amygdala. Archives of General Psychiatry. 2005;62:146–152. doi: 10.1001/archpsyc.62.2.146. [DOI] [PubMed] [Google Scholar]
- Hayes AF, Matthes J. Computational procedures for probing interactions in OLS and logistic regression: SPSS and SAS implementations. Behavior Research Methods. 2009;41:924–936. doi: 10.3758/BRM.41.3.924. [DOI] [PubMed] [Google Scholar]
- Henderson EN, Jennings KD. Maternal depression and the ability to facilitate joint attention with 18-month-olds. Infancy. 2003;4:27–46. [Google Scholar]
- Jacobvitz D, Sroufe LA. The early caregiver–child relationship and attention-deficit disorder with hyperactivity in kindergarten: A prospective study. Child Development. 1987;58:1496–1504. doi: 10.1111/j.1467-8624.1987.tb03862.x. [DOI] [PubMed] [Google Scholar]
- Kerr D, Leve LD, Harold GT, Natsuaki M, Neiderhiser J, Shaw DS, Reiss D. Influences of biological and adoptive mothers' depression and antisocial behavior on adoptees' early behavior trajectories. Journal of Abnormal Child Psychology. 2013;41:723–734. doi: 10.1007/s10802-013-9711-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kotelchuck M. An evaluation of the Kessner Adequacy of Prenatal Care Index and a proposed adequacy of prenatal care utilization index. American Journal of Public Health. 1994;84:1414–1420. doi: 10.2105/ajph.84.9.1414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laurent HK, Leve LD, Neiderhiser JM, Natsuaki MN, Shaw DS, Harold GT, Reiss D. Effects of birth and adoptive parent depressive symptoms on child HPA regulation: Independent and moderated influences. Developmental Psychology. 2013;49:876–886. doi: 10.1037/a0028800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leadbeater BJ, Bishop SJ, Raver CC. Quality of mother–toddler interactions, maternal depressive symptoms, and behavior problems in preschoolers of adolescent mothers. Developmental Psychology. 1996;32:280–288. [Google Scholar]
- Leerkes EM, Burnery RV. The development of parenting efficacy among new mothers and fathers. Infancy. 2007;12:45–67. doi: 10.1111/j.1532-7078.2007.tb00233.x. [DOI] [PubMed] [Google Scholar]
- Leve LD, Kerr DC, Shaw D, Ge X, Neiderhiser JM, Scaramella LV, Reiss D. Infant pathways to externalizing behavior: Evidence of genotype × environment interaction. Child Development. 2010;81:340–356. doi: 10.1111/j.1467-8624.2009.01398.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leve LD, Neiderhiser JM, Shaw DS, Ganiban J, Natsuaki MN, Reiss D. The Early Growth and Development Study: A prospective adoption study of child behavior from birth through middle childhood. Twin Research and Human Genetics. 2013;16:412–423. doi: 10.1017/thg.2012.126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lipscomb ST, Leve LD, Harold GT, Neiderhiser JM, Shaw DS, Ge X, Reiss D. Trajectories of parenting and child negative emotionality during infancy and toddlerhood: A longitudinal analysis. Child Development. 2011;82:1661–1675. doi: 10.1111/j.1467-8624.2011.01639.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lohaus A, Keller H, Ball J, Elben C, Voelker S. Maternal sensitivity: Components and relations to warmth and contingency. Parenting: Science and Practice. 2001;1:267–284. [Google Scholar]
- Marceau K, Hajal N, Leve LD, Reiss D, Shaw DS, Ganiban JM, Neiderhiser JM. Measurement and associations of pregnancy risk factors with genetic influences, postnatal environmental influences, and toddler behavior. International Journal of Behavioral Development. 2013;37:366–375. doi: 10.1177/0165025413489378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McNeil TF, Cantor-Graae E, Sjöström K. Obstetric complications as antecedents of schizophrenia: Empirical effects of using different obstetric complication scales. Journal of Psychiatric Research. 1994;28:519–530. doi: 10.1016/0022-3956(94)90042-6. [DOI] [PubMed] [Google Scholar]
- McNeil TF, Sjöström K. The McNeil–Sjöström OC Scale: A comprehensive scale for measuring obstetric complications. Sweden: Malmö General Hospital; 1994. [Google Scholar]
- Mesman J. Maternal responsiveness to infants: Comparing micro- and macro-level measures. Attachment and Human Development. 2010;12:143–149. doi: 10.1080/14616730903484763. [DOI] [PubMed] [Google Scholar]
- Molenaar PC. A dynamic factor model for the analysis of multivariate time series. Psychometrika. 1985;50:181–202. [Google Scholar]
- Moore GA, Calkins SD. Infants' vagal regulation in the still-face paradigm is related to dyadic coordination of mother-infant interaction. Developmental Psychology. 2004;40:1068–1080. doi: 10.1037/0012-1649.40.6.1068. [DOI] [PubMed] [Google Scholar]
- Moore GA, Cohn JF, Campbell SB. Infant affective responses to mother's still face at 6 months differentially predict externalizing and internalizing behaviors at 18 months. Developmental Psychology. 2001;37:706–714. [PubMed] [Google Scholar]
- Moore GA, Teti LO, Roben CKP. Early Growth and Development Study (EGDS) microcoding manual for the Parent–Child Teaching Task. University Park, PA: The Pennsylvania State University; 2009. Unpublished manuscript. [Google Scholar]
- Natsuaki MN, Ge X, Leve LD, Neiderhiser JM, Shaw DS, Conger RD, Reiss D. Genetic liability, environment, and the development of fussiness in toddlers: The roles of maternal depression and parental responsiveness. Developmental Psychology. 2010;46:1147–1158. doi: 10.1037/a0019659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Natsuaki MN, Shaw DS, Neiderhiser JM, Ganiban JM, Harold GT, Reiss D, Leve LD. Raised by depressed parents: Is it an environmental risk? Clinical Child and Family Psychology Review. 2014 doi: 10.1007/s10567-014-0169-z. Advance online publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- NICHD Early Child Care Research Network. Infant-mother attachment: Risk and protection in relation to changing maternal caregiving quality over time. Developmental Psychology. 2006;42:38–58. doi: 10.1037/0012-1649.42.1.38. [DOI] [PubMed] [Google Scholar]
- Nicodemus KK, Marenco S, Batten AJ, Vakkalanka R, Egan MF, Straub RE, Weinberger DR. Serious obstetric complications interact with hypoxia-regulated/vascular-expression genes to influence schizophrenia risk. Molecular Psychiatry. 2008;13:874–877. doi: 10.1038/sj.mp.4002153. [DOI] [PubMed] [Google Scholar]
- Pardini DA. Novel insights into longstanding theories of bidirectional parent–child influences: Introduction to the special section. Journal of Abnormal Child Psychology. 2008;36:627–631. doi: 10.1007/s10802-008-9231-y. [DOI] [PubMed] [Google Scholar]
- Patterson GR. Early development of coercive family process. In: Reid JB, Snyder J, editors. Antisocial behavior in children and adolescents: A developmental analysis and model for intervention. Washington, DC: American Psychological Association; 2002. pp. 25–44. [DOI] [Google Scholar]
- Pemberton CK, Neiderhiser JM, Leve LD, Natsuaki MN, Shaw DS, Reiss D, Ge X. Influence of parental depressive symptoms on adopted toddler behaviors: An emerging developmental cascade of genetic and environmental effects. Development and Psychopathology. 2010;22:803–818. doi: 10.1017/S0954579410000477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rhoades KA, Leve LD, Harold GT, Neiderhiser JM, Shaw DS, Reiss D. Longitudinal pathways from marital hostility to child anger during toddlerhood: Genetic susceptibility and indirect effects via harsh parenting. Journal of Family Psychology. 2011;25:282–291. doi: 10.1037/a0022886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sameroff A. Transactional models in early social relations. Human Development. 1975;18:65–79. [Google Scholar]
- Shaw DS, Bell RQ. Developmental theories of parental contributors to antisocial behavior. Journal of Abnormal Child Psychology. 1993;21:493–518. doi: 10.1007/BF00916316. [DOI] [PubMed] [Google Scholar]
- Silk JS, Shaw DS, Skuban EM, Oland AA, Kovacs M. Emotion regulation strategies in offspring of childhood-onset depressed mothers. Journal of Child Psychology and Psychiatry. 2006;47:69–78. doi: 10.1111/j.1469-7610.2005.01440.x. [DOI] [PubMed] [Google Scholar]
- Teti DM, Gelfand DM. Behavioral competence among mothers of infants in the first year: The mediational role of maternal self-efficacy. Child Development. 1991;62:918–929. doi: 10.1111/j.1467-8624.1991.tb01580.x. [DOI] [PubMed] [Google Scholar]
- Tronick EZ, Messinger DS, Weinberg MK, Lester BM, LaGasse L, Seifer R, Liu J. Cocaine exposure is associated with subtle compromises of infants' and mothers' social–emotional behavior and dyadic features of their interaction in the face-to-face still-face paradigm. Developmental Psychology. 2005;41:711–722. doi: 10.1037/0012-1649.41.5.711. [DOI] [PubMed] [Google Scholar]
- Voelker S, Keller H, Lohaus A, Cappenberg M, Chasiotis A. Maternal interactive behavior in early infancy and later attachment. International Journal of Behavioral Development. 1999;23:921–936. [Google Scholar]
- Webster-Stratton C, Eyberg SM. Child temperament: Relationship with child behavior problems and parent–child interactions. Journal of Clinical Child Psychology. 1982;11:123–129. [Google Scholar]
- Zizzer A, Eyberg SM. Treating oppositional behavior in children using parent–child interaction therapy. In: Kazdin AE, Weisz JR, editors. Evidence-based psychotherapies for children and adolescents. New York: Guilford; 2010. pp. 179–193. [Google Scholar]