Key Clinical Message
Differentiating hepatic portal venous gas (HPVG) and pneumobilia on the CT scan can be accomplished by comparing the pattern of intrahepatic air spread. HPVG can be an indicator of significant intra-abdominal pathology and bowel ischaemia is the most common causative etiology for HPVG.
Keywords: Hepatic Portal Venous Gas, Pneumobilia, Bowel toxicity
Case Report
A 49-year-old man presented with a 2-day history of worsening abdominal pain and nonbloody diarrhea. He had undergone his second cycle of radical chemotherapy (Cisplastin, Doxitacel, and 5-fluorouracil) 4 days prior to admission for a newly diagnosed postcricoid esophageal squamous cell carcinoma. On arrival, he was found to be peripherally vasoconstricted, blood pressure was 60/40 mmHg and heart rate was 130 BPM. He was apyrexial and abdominal examination revealed a rigid abdomen with severe generalized rebound tenderness and quiet bowel sounds. A full blood revealed pancytopenia (WCC 0.9, Hb 93, Plt 115) and arterial blood glas showed metabolic acidosis with a lactate of 6.5 mmol/L. He underwent an urgent contrasted CT abdomen and pelvis study (Fig.1), which revealed extensive gas within the portal venous system and in the superior mesenteric branches. This was consistent with a significant ischaemic event within the bowel. A conservative management strategy was adopted and the patient was treated with intravenous piperacillin/tazobactam, intravenous fluids, and analgesia. He made a remarkable recovery over a period of 72 h. A repeat CT study after 2 weeks showed complete radiologic resolution of the gas within the liver. The rapid improvement has led us to suspect that the cause of the reversible bowel ischemia was likely cisplatin-induced bowel toxicity.
Figure 1.
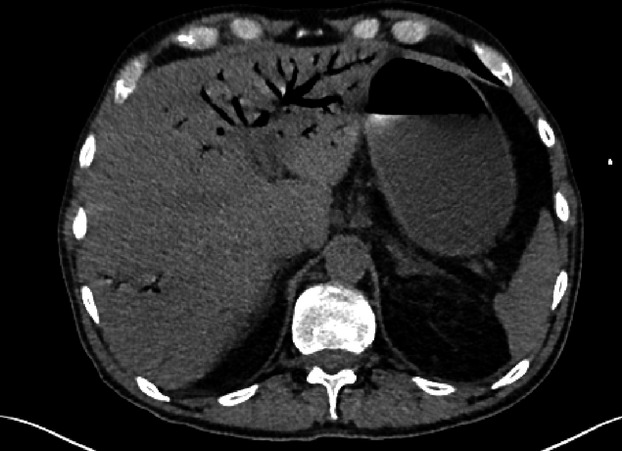
Extensive gas within the portal venous system.
Discussion
Portal venous system is enhanced by the presence of air. The main radiological differential is pneumobilia, air in the biliary tree. Differentiating hepatic portal venous gas (HPVG) and pneumobilia can be accomplished by comparing the pattern of intrahepatic air spread. In HPVG, the branching radiolucency often extends to within 2 cm of the liver capsule due to the centrifugal flow of portal venous blood. In pneumobilia, the air is situated centrally to the liver hilum due to the opposite direction of bile flow 1.
HPVG can be an indicator of significant intra-abdominal pathology and bowel ischemia is the most common causative etiology for HPVG. Traditionally, the detection of HPVG in patients with ischemic bowel is associated highly with transmural necrosis (90% of cases) 2 and predicts a high risk of mortality (up to 85%). With the advent of better imaging techniques, an increasing number of cases of HPVG secondary to various causes such as inflammatory bowel disease, gastric ulcer, and intra-abdominal sepsis can now be detected 3. A study of 182 cases of HPVG revealed an overall mortality rate of 39% 3.
Conflict of Interest
None declared.
References
- Yarze JC. Markowitz DM. Distinguishing Between Hepatic Portal Vein Gas and Pneumo(aero)bilia. Liver Transpl. 2007;13:1476. doi: 10.1002/lt.21239. [DOI] [PubMed] [Google Scholar]
- Abboud B, El Hachem J, Yazbeck T. Doumit C. Hepatic portal venous gas: physiopathology, etiology, prognosis and treatment. World J. Gastroenterol. 2009;15:3585–3590. doi: 10.3748/wjg.15.3585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kinoshita H, Shinozaki M, Tanimura H, Umemoto Y, Sakaguchi S, Takifuji K, et al. Clinical features and management of hepatic portal venous gas: four case reports and cumulative review of the literature. Arch. Surg. 2001;136:1410–1414. doi: 10.1001/archsurg.136.12.1410. [DOI] [PubMed] [Google Scholar]


