Abstract
Pre-migration and post-migration factors may influence the health of immigrants. Using a cross-national framework that considers the effects of the sending and receiving social contexts, we examined the extent to which pre-migration and post-migration factors, including individual and neighborhood level factors, influence depressive symptoms at a 2-year follow-up time point. Data come from the Boston Puerto Rican Health Study, a population-based prospective cohort of Puerto Ricans between the ages of 45 and 75 y. The association of neighborhood ethnic density with depressive symptomatology at follow-up was significantly modified by sex and level of language acculturation. Men, but not women, experienced protective effects of ethnic density. The interaction of neighborhood ethnic density with language acculturation had a non-linear effect on depressive symptomatology, with lowest depressive symptomatology in the second highest quartile of language acculturation, relative to the lowest and top two quartiles among residents of high ethnic density neighborhoods. Results from this study highlight the complexity, and interplay, of a number of factors that influence the health of immigrants, and emphasize the significance of moving beyond cultural variables to better understand why the health of some immigrant groups deteriorates at faster rates overtime.
Keywords: Immigrant mental health, depressive symptomatology, ethnic density, pre-migration and post-migration factors, acculturation, Latinos/Hispanics
INTRODUCTION
Population health and health patterns are influenced by the growing movement of people across national and local borders (Acevedo-Garcia, Sanchez-Vaznaugh, Viruell-Fuentes, & Almeida, 2012). The health of immigrants over the life course has an important effect on the health patterns of sending and receiving societies (Zimmerman, Kiss, & Hossain, 2011); immigrant health research may inform and enhance knowledge about population health. An emphasis on cultural explanations and the omission of structural factors in immigrant research provides incomplete generalizations about migrant health (Abraido-Lanza, Armbrister, Florez, & Aguirre, 2006; Hunt, Schneider, & Comer, 2004). A broad social determinants of health framework, which underlines social and structural explanations that create and reproduce social and health inequities, and an examination of the interactions between culture and structural inequality, may enhance our understanding of immigrant health (Abraido-Lanza et al., 2006; Acevedo-Garcia et al., 2012; Zambrana & Carter-Pokras, 2010). Using a cross-national framework that considers the effects of the sending and receiving social contexts (Acevedo-Garcia et al., 2012), we examined the extent to which pre-migration and post-migration factors, including individual and neighborhood level factors, influence depressive symptoms in a cohort of Puerto Rican adults in the U.S.--a group at documented disadvantage for a variety of health outcomes (Tucker et al., 2010).
Depression
Major depression is one of the most common mental disorders in the United States. Recent estimates suggest that more than 33 million adults in the United States (16.2%) have experienced an episode of major depression during their lifetime (Kessler et al., 2003; Merikangas et al., 2007). The incidence of depression seems to peak early in adult life and among older adults in their 50s (Eaton et al., 1997). Although some national surveys have reported lower rates of mood and anxiety disorders among Latinos compared to non-Latino whites in the United States; these findings are not homogeneous by ethnic sub-group. The National Latino and Asian American Study (NLAAS) found lifetime prevalence of psychiatric disorders of 37.4% among Puerto Ricans, compared to 29.5% in Mexicans, 28.2% in Cubans and 27.0% among other Latinos (Alegria et al., 2008). Some studies found that U.S.-born and island-born Puerto Ricans had similar risk for psychiatric disorder, relative to the U.S. general population (Alegria et al., 2008; Alegria et al., 2007; J. Breslau, Borges, Hagar, Tancredi, & Gilman, 2009; Ortega, Feldman, Canino, Steinman, & Alegria, 2006), but others suggest that Puerto Ricans living on the U.S. mainland have considerably higher risk than other groups. In Massachusetts, 44 % of Puerto Rican older adults reported high depressive symptomatology vs. 22 % of neighborhood based non-Hispanic white older adults (Falcon & Tucker, 2000).
Neighborhood Ethnic Density
Recent research highlights the critical role of neighborhood context on individual health (Glymour, Mujahid, Wu, White, & Tchetgen, 2010; Osypuk & Acevedo-Garcia, 2010; Roux & Mair, 2010; Sampson, 2003; Truong & Ma, 2006). Among immigrant groups, neighborhoods can significantly shape the process of acculturation (Schwartz, Unger, Zamboanga, & Szapocznik, 2010). The ethnic density effect refers to the protective effect on mental health, in particular, found among immigrants residing in neighborhoods with larger proportions of co-ethnic residents (Becares et al., 2012; Das-Munshi, Becares, Dewey, Stansfeld, & Prince, 2010; Lester, 2010). While neighborhood ethnic density and poverty may be particularly influential to immigrant acculturation, research that examines the interaction between acculturation and neighborhood contexts is limited.
Acculturation
Acculturation is a post-migration process that occurs over the immigrant life course; immigrants engage in a variety of cultural strategies, and adopt behaviors and hold beliefs and values that reflect both the heritage culture and the host culture (Berry, 2006). An understanding of how the process of acculturation may influence immigrant health requires recognition of the context in which it occurs (Schwartz et al., 2010; Zimmerman et al., 2011). This context includes the characteristics of the migrants themselves, the society from which they migrated from, their socioeconomic status and resources, the particular ways in which they are free to adapt and become part of the host culture, and the local community in which they settle (Birman, Trickett, & Buchanan, 2005; Schwartz et al., 2010).
Pre-migration and Post-migration Factors
Experiences in the home country prior to migration may influence the physical and mental health of immigrants later in life (Ornelas & Perreira, 2011). A life course perspective highlights the influential role of physical context early in life in shaping adult health (Braveman & Barclay, 2009; Clarke et al., 2013). However, little is known about the influence of rural vs. urban contexts prior to migration on the health of migrants. Reasons for migration are considered push and pull factors that motivate the migration process and create expectations about the new society (Llácer, Zunzunegui, del Amo, Mazarrasa, & Bolůmar, 2007). Involuntary or forced migration, or negative expectations, may be related to more problems with psychological adaptation. On the other hand, high optimistic but unmet expectations may also generate stress and negatively affect health (Berry, 1997, 2006).
The social context of the places where immigrants settle in may influence how social variables affect health. Communities with high immigrant concentrations have been shown to promote social capital and positive social outcomes that, in turn, have been linked to health outcomes and measures of well-being (Becares & Nazroo, 2013; Kawachi, Kim, Coutts, & Subramanian, 2004). Social variables, including social participation, social support and social networks, are associated with health and well-being in a dynamic process, which is constantly evolving throughout the life course (Berkman & Glass, 2000; Cohen, 2004; Umberson, Crosnoe, & Reczek, 2010). Social participation or social engagement, the involvement in a wide range of social activities, is particularly relevant for individuals settling in new societies because it provides opportunities to adjust to their new social roles, and to develop a sense of community through interactions with their physical and social environments, in productive and meaningful ways (Cohen, 2004; Levasseur, Richard L, Gauvin L, & E., 2010). Engagement in social activities may enhance psychological well-being and overall health by providing emotional support, aiding in management of stressful situations, providing a sense of social and personal control, and assigning social meanings (i.e., connection, belonging, shared culture and religious doctrine) (Umberson et al., 2010). Greater participation in social activities may broaden social capital at the individual level, i.e., individuals’ networks and the access to resources these provide; as well as, social capital at a broader level by supporting the development of social cohesion and social trust at the community level.
Language proficiency allows immigrants to navigate their environment effectively to locate social and economic resources, and may facilitate adaptation to the host society, reducing adaptation related stress (Berry, 1997). Perceived discrimination and length of stay in the host society have been shown to be associated with health outcomes in immigrant groups (D'Anna, Ponce, & Siegel, 2010; Krieger, 2000; Stuber, Meyer, & Link, 2008; Williams & Mohammed, 2009)
Puerto Rican Migrants
Puerto Ricans are the second largest Latino subgroup in the United States (Landale, 1994). Unlike other Latino groups, Puerto Rican migration is officially classified as internal migration, as they enjoy the social and political benefits of U.S. citizenship. However, cultural, linguistic, racial, and socioeconomic differences characterize a migratory process that is more comparable to that of immigrants from Latin America and the Caribbean than to U.S. internal migrants (Landale & Oropesa, 2001).
A growing body of research shows a health disadvantage among Puerto Ricans compared to other Latino groups (Acevedo-Garcia, Bates, Osypuk, & McArdle, 2010; Ortega et al., 2006), and Puerto Ricans on the U.S. mainland tend to reside in neighborhoods with higher racial segregation indices than do other Latino sub-groups (Burgos & Rivera, 2012; Massey, 1989). Studies that examine the interaction of physical context with factors related to the process of acculturation may aid in understanding the health disadvantage of Puerto Ricans in the U.S. mainland.
METHODS
Using data from the Boston Puerto Rican Health Study, a population-based prospective cohort of Puerto Ricans between the ages of 45 and 75 years at baseline, we examined associations of neighborhood ethnic density with depressive symptomatology at approximately two years later before and after adjusting for neighborhood poverty level. We then tested for the modifying effect of pre-migration and post-migration factors on the neighborhood ethnic density and depressive symptomatology at follow-up association.
Following the existing literature, we formulated two main hypotheses:
H1: living in ethnically dense neighborhoods will be initially associated with higher depressive symptomatology, due to the poverty associated with these neighborhoods; but after adjusting for neighborhood poverty level, neighborhood ethnic density will be associated with lower depressive symptomatology.
H2: pre-migration factors (including urbanicity and reason for migration) and post-migration factors (including language acculturation, social activities, perceived discrimination, and length of stay in the U.S. mainland) will have modifying effects on the association of neighborhood ethnic density with depressive symptomatology.
The Institutional Review Boards at Tufts Medical Center and Northeastern University approved the study. All participants provided signed informed consent in their language of choice (Spanish or English). Baseline recruitment occurred between 2004 and 2009. Specifics of the study and recruitment are described in detail elsewhere (Tucker et al., 2010). The initial data collection yielded a baseline cohort of 1,504 participants. Follow-up interviews, conducted approximately two years after baseline, had a high response rate of 84% or 1,265 participants. The lack of availability of valid geocoded data for some of the respondents at baseline, and missing data in some variables (<2%) restricted the final analytical sample to 1142 participants. Results from t-tests and Chi Square tests for descriptive characteristics between included participants and those excluded because of missing data showed no significant differences.
We obtained neighborhood level data from the 2000 U.S. Census data at the tract-level, as a proxy for neighborhood indicators. The tract-level Census variables percent of individuals identified as Puerto Rican, and percent of persons below the poverty level, were used to measure neighborhood ethnic density and neighborhood poverty, respectively.
Measures
Depressive symptoms were measured with the Center for Epidemiologic Studies-Depression Scale (CES-D). This instrument has shown good reliability and discriminating features in Puerto Ricans (Falcon & Tucker, 2000; Mahard, 1988). Participants were asked to indicate how often a list of 20 statements has been true over the past seven days. For example, “I felt depressed,” with responses range from “rarely or never” (0) to “most of the time or all of the time” (3). Items were summed from 0 to 60 with higher scores indicating more frequent depressive symptoms (Radloff, 1977). The Cronbach’s alpha for the CES-D scale components in this sample was high (α=.90). We used the CES-D as a continuous variable.
Neighborhood Ethnic Density was measured using the 2000 U.S. Census indicator of the proportion of Puerto Ricans within the population of a census tract. Ethnic density ranged from 0.1% to 34.4%. Based on this distribution, we performed a median split (0=<15% (ref); 1=≥15%) to create a dichotomous ethnic density variable. Neighborhood poverty level is the proportion of the population of the census tract that lives below the poverty line. The highest rate of neighborhood poverty among our participants was 16.9%, relative to the overall rate of poverty in Massachusetts of 9.6% (Massachusetts Budget and Policy Center, 2008).
Participants were asked about the type of surroundings in their country of birth, and where they spent most of their time while growing up. Responses were categorized as 1=Urban/Suburban (ref), 2=Town, and 3=Rural to create the pre-migration urbanicity variable. Reason for migration, a four-category variable (1=socioeconomic -ref; 2=family reunification; 3=access to health care services; 4=personal or family problems), was created from an open-ended question that asked participants the main reason why they had left Puerto Rico.
Post-migration Factors
Length of residence in the U.S. mainland was categorized into four levels (1=<15y; 2=15-24y; 3=25-34y; 4=>35y) to capture the diverse migrating patterns in this sample of adult migrants. Language acculturation was measured with the Acculturation Scale for Hispanics (ASH) (Marin, Sabogal, Marin, Otero-Sabogal, & Perez-Stable, 1987) modified for the Puerto Rican population (Falcon & Tucker, 2000). The ASH scale scores range from 0-100 with higher scores indicating greater use of English vs. Spanish language in activities such as watching TV or listening to the radio, reading newspapers/books, speaking with neighbors, friends or family, and language use at work. The ASH was categorized into quartiles for analysis. Perceived discrimination due to one’s race, ethnicity, or language was coded as (0=no; 1=yes). Participants were asked to report their engagement in thirteen different social activities within the two weeks preceding the interview. We used principal components analysis to reduce the number of items while preserving the variability of the data. Four component factors, labeled ‘recreational activities’, ‘activities with friends and neighbors’, ‘family activities’, and ‘church and other activities’, were identified (Hamilton, 2009) (Table 1). Factor scores, after varimax rotation, were used in the analysis, standardized to a zero mean and one unit variance (Hamilton, 2009). Demographic variables included sex, age in years, and educational attainment. We categorized years of education into four levels (< 5th grade=ref; vs. 5th-8th grade, 9th-12th grade, or ≥ some college) considering that almost a quarter of the sample reported less than 5th grade and 48% of the sample reported less than 9th grade levels of education.
Table 1.
Factor analysis of social activities
| Items | Loadings | Cummulative Variance |
|---|---|---|
| Factor 1: Recreational Activities | 0.18 | |
| Go to a show or movie, sports event, club meeting, classes or other group event | 0.375 | |
| Participate in any sports or exercises | 0.385 | |
| Work at hobbies | 0.427 | |
| Woork on home maintenance or small repairs around the home | 0.482 | |
| Help friends or neighbors with somethin without being paid | 0.370 | |
| Factor 2: Friends and neighbors Activities | 0.29 | |
| Get together with friends or neighbors | 0.549 | |
| Talk with friends and neighbors | 0.640 | |
| Factor 3: Family Activities | 0.38 | |
| Get together with relatives who doesn't live with you? | 0.662 | |
| Tale with relatives on the telephone | 0.390 | |
| Take care of family members who do not live with you | 0.558 | |
| Factor 4: Church, volunteer, other Activities | 0.46 | |
| Go to church or temple for sercices or other activities | 0.720 | |
| Do volunteer work | 0.521 | |
| Read books, magazines, or newspaper | 0.382 |
Analytical Strategy
Two level hierarchical linear regression models for continuous outcomes were estimated using STATA statistical software version 13.0. Level 1 included study participants and level 2 included census tract-level measures of Puerto Rican ethnic density and neighborhood poverty. We first assessed whether there was significant variance in depressive symptomatology at the neighborhood level. Although, no significant neighborhood variance was found, we continued with a two-level model given the hierarchical structure of our data (individuals nested within neighborhoods). This accounts for the clustering nature of the data, avoids underestimation of standard errors, and reduces type I error (Raudenbush & Bryk, 2002). We examined group differences in outcome, predictors and potential confounders by neighborhood ethnic density (low vs. high) using t-tests and Chi Square tests for continuous and categorical variables, respectively.
Two level hierarchical multivariable linear regression analyses, adjusted for sex, age, education, neighborhood poverty, and baseline depressive symptomatology, were used to test for an association between neighborhood ethnic density and depressive symptomatology at follow-up in model 1. Pre-migration urbanicity, reason for migration, length of stay in the U.S. mainland, language acculturation, perceived discrimination, and social activities were added in model 2. Interactions between neighborhood ethnic density and the pre-migration and post-migration factors were tested and significant interactions were kept in model 3.
RESULTS
Neighborhood ethnic density ranged from 0.1% to 34.4%, with a mean of 14.3% and standard deviation of 9.13. Our final sample included 861 women (71%), and 344 men (29%); the average mean age at baseline was 57 years (SD=7.6); 23% had <5th grade education, 25% had completed middle school, 38% high school, and 14% had at least some college education (Table 2). The average duration between baseline and follow-up was 2.2 years. Mean depressive symptomatology scores were 20.1 (SD=13.1) at baseline, and 18.1 (SD=12.5) at follow-up (p<0.0001, paired t-test). The CES-D provides cutoff scores, e.g., 16 or greater, to identify individuals at risk for clinical depression. More than 60% of participants had CES-D scores greater than 16 at baseline and at follow-up, which indicates high risk for clinical depression in this sample. More than half (51.2%) lived in neighborhoods with high Puerto Rican density (PRD) (≥15%). Those in high PRD neighborhoods were older, less likely to have college education, more likely to be living in poverty, and had higher depressive symptoms, lower language acculturation, and lower scores for recreational activities, but were less likely to report experiences of racial, ethnic or language discrimination (Tables 2a and 2b).
Table 2a.
Puerto Rican adults, aged 45-75y, living in Massachussetts: general characteristics and group comparisons by neighborhood ethnic density (ED)
| All | Ethnic Density Groups | |||||||
|---|---|---|---|---|---|---|---|---|
| Low ED < 15% |
High ED 15%≥ |
T-Test | ||||||
| Means (±SD) | t | Prob>t | ||||||
| Depressive symptomatology (CES-D) at 2-year follow-up | 18.1 | (±12.5) | 17.8 | (±12.6) | 18.3 | (±12.3) | −0.7 | 0.47 |
| Depressive symptomatology (CES-D) at baseline | 20.1 | (±13.1) | 19.0 | (±13.1) | 21.2 | (±13.1) | −2.9 | <0.01 |
| Age (years) | 57.4 | (±7.6) | 56.8 | (±7.4) | 57.9 | (±7.7) | −2.6 | <0.01 |
| Neighborhood population below poverty level Social activities |
7.2 | (±3.0) | 5.6 | (±3.2) | 8.7 | (±3.0) | −17.6 | <0.0001 |
| Recreational activities | −0.02 | (±1.3) | 0.10 | (±1.4) | −0.12 | (±1.3) | 2.8 | <0.01 |
| Friends and neighbors activities | 0.02 | (±1.2) | 0.07 | (±1.2) | −0.03 | (±1.3) | 1.5 | 0.14 |
| Family activities | 0.02 | (±1.1) | 0.06 | (±1.2) | −0.01 | (±1.1) | 1.1 | 0.28 |
| Church related activities | −0.01 | (±1.1) | 0.01 | (±1.1) | −0.02 | (±1.1) | 0.4 | 0.67 |
Table 2b.
Puerto Rican adults, aged 45-75y, living in Massachussetts: general characteristics and group comparisons by neighborhood ethnic density (ED)
| All 1 | Ethnic Density Groups | |||||||
|---|---|---|---|---|---|---|---|---|
| Low ED < 15% |
High ED 15%≥ |
ChiSquare- | ||||||
| η (%) | Chi2 | Prob | ||||||
| Gender | 0.3 | 0.60 | ||||||
| Male | 344 | (29) | 172 | (50) | 172 | (50) | ||
| Female | 861 | (71) | 416 | (48) | 445 | (52) | ||
| Education (categories) | 9.2 | <0.05 | ||||||
| No schooling or <5th grade | 276 | (23) | 130 | (22) | 146 | (24) | ||
| 5th-8th grade | 305 | (25) | 132 | (22) | 173 | (28) | ||
| 9-th-12th grade | 456 | (38) | 230 | (39) | 226 | (37) | ||
| College/graduate | 168 | (14) | 96 | (16) | 72 | (12) | ||
| Pre-migration urbanicity | 5.4 | 0.07 | ||||||
| Urban/suburban | 454 | (38) | 241 | (41) | 213 | (35) | ||
| Town | 177 | (15) | 86 | (15) | 91 | (15) | ||
| Rural | 568 | (47) | 260 | (44) | 308 | (50) | ||
| Reason for migration | 2.6 | 0.45 | ||||||
| Socioeconomic reasons | 556 | (47) | 272 | (47) | 284 | (46) | ||
| Family reunification/to take care of family | 463 | (39) | 224 | (39) | 239 | (39) | ||
| Acces to health care services | 72 | (6) | 29 | (5) | 43 | (7) | ||
| Personal and family problems | 101 | (8) | 53 | (9) | 48 | (8) | ||
| Length of stay in the U.S. mainland-categories | 7.5 | 0.06 | ||||||
| Less 15y | 104 | (9) | 44 | (8) | 60 | (10) | ||
| 15-24y | 136 | (12) | 77 | (13) | 59 | (10) | ||
| 25-34y | 255 | (22) | 134 | (23) | 121 | (20) | ||
| >35y | 686 | (58) | 322 | (56) | 364 | (60) | ||
| Language acculturation quartiles | 46.3 | <0.0001 | ||||||
| Q1 (Mean:1.3 , range: 1.9-4.2) | 362 | (30) | 172 | (24) | 271 | (35) | ||
| Q2 (Mean: 12.9, range: 5.1-20.8) | 298 | (25) | 148 | (21) | 198 | (26) | ||
| Q3 (Mean: 31.6, range:21.4-41.7 ) | 277 | (23) | 172 | (24) | 164 | (21) | ||
| Q4 (Mean: 56.1, range: 42.9-95.8) | 268 | (22) | 223 | (31) | 140 | (18) | ||
| Perceived racial/ethnic/language discrimination | 4.2 | <0.05 | ||||||
| No|no answer | 827 | (69) | 387 | (66) | 440 | (71) | ||
| Yes | 472 | (31) | 201 | (34) | 177 | (29) | ||
Not all categories add to η=1205 due to missing data in some variables
Higher depressive symptomatology was positively associated with neighborhood ethnic density at baseline (β=2.17; SE=0.75; ρ<0.01), and with neighborhood poverty level at baseline (β=0.24; SE=0.11; ρ<0.05) and follow-up (β=−0.24 SE=0.11; ρ<0.05) (Table 3). Women had significantly higher depressive symptomatology than men at baseline (β=5.22; SE=0.82; ρ<0.0001) and follow-up (β=5.35; SE=0.78; ρ<0.0001). Compared to participants who resided in an urban/suburban context while growing up, those growing up in rural areas had lower depressive symptoms at follow-up (Table 3). Participants who migrated for family reunification, access to health care services, or for personal or family problems had higher depressive symptomatology relative to those who migrated for economic reasons at baseline and follow-up (Table 3). Longer length of stay in the U.S. mainland and higher level of language acculturation were associated with lower depressive symptomatology at follow-up (Table 3). Participants who reported discrimination (vs. those who did not) had higher depressive symptomatology at baseline (β=2.63; SE=0.81; ρ=0.001) and follow-up (β=1.65; SE=0.77; ρ<0.05). Engagement in recreational activities, social activities with friends and neighbors, and church activities were inversely associated with depressive symptomatology at both baseline and follow-up (Table 3).
Table 3.
Bivariate associations with depressive symptomatology (CES-D)
| Depressive Symptomatology | ||||||
| at Baseline | at Follow-up | |||||
| β | (SE) | ρ-value | β | (SE) | ρ-value | |
| Neighborhood ethnic density | ||||||
| Low <15% (ref.) | − | − | ||||
| High 15%≥ | 2.17 | 0.75 | <0.01 ** | 0.51 | 0.74 | 0.49 |
| Neighborhood population living below poverty level | 0.24 | 0.11 | 0.03 * | 0.24 | 0.11 | 0.02 * |
| Gender | ||||||
| Male (ref.) | − | − | ||||
| Female | 5.22 | 0.82 | <0.0001 *** | 5.35 | 0.78 | <0.0001 *** |
| Pre-migration urbanicity | ||||||
| Urban/suburban (ref.) | − | − | ||||
| Town | −1.50 | 1.16 | 0.20 | −1.86 | 1.10 | 0.09 + |
| Rural | −0.54 | 0.82 | 0.52 | −1.55 | 0.78 | 0.05 * |
| Reason for migration | ||||||
| Socioeconomic reasons (ref.) | − | − | ||||
| Family reunification/to take care of family | 1.89 | 0.82 | 0.02 * | 2.41 | 0.77 | <0.01 ** |
| Acces to health care services | 6.09 | 1.63 | <0.0001 *** | 3.60 | 1.54 | 0.02 * |
| Personal and family problems | 4.31 | 1.41 | <0.01 ** | 6.11 | 1.33 | <0.0001 *** |
| Length of stay in the U.S. mainland-categories | ||||||
| Less 15y (ref.) | − | − | ||||
| 15-24y | −1.56 | 1.71 | 0.36 | −0.26 | 1.61 | 0.87 |
| 25-34y | −2.00 | 1.53 | 0.19 | −0.66 | 1.44 | 0.65 |
| >35y | −3.47 | 1.38 | 0.01 ** | −3.13 | 1.31 | 0.02 * |
| Language acculturation quartiles | ||||||
| Q1 (Low) (ref.) | − | − | ||||
| Q2 | −0.24 | 1.02 | 0.82 | −1.20 | 0.97 | 0.22 |
| Q3 | −0.85 | 1.05 | 0.42 | −1.42 | 0.99 | 0.15 |
| Q4 (High) | −2.02 | 1.06 | 0.06 + | −2.17 | 1.00 | 0.03 * |
| Perceived racial/ethnic/language discrimination | ||||||
| No|no answer (ref.) | ||||||
| Yes | 2.63 | 0.81 | 0.001 *** | 1.65 | 0.77 | 0.03 * |
| Social activities - Factors | ||||||
| Recreational activities | −1.33 | 0.28 | <0.0001 *** | −1.44 | 0.27 | <0.0001 *** |
| Friends and neighbors activities | −1.41 | 0.31 | <0.0001 *** | −1.26 | 0.30 | <0.0001 *** |
| Family activities | −0.26 | 0.33 | 0.44 | −0.46 | 0.32 | 0.15 |
| Church related activities | −1.42 | 0.33 | <0.0001 *** | −1.41 | 0.31 | <0.0001 *** |
ρ≤0.001;
ρ≤0.01;
ρ≤0.05;
ρ≤0.10
In models adjusting for sex, age, education, neighborhood poverty, depressive symptoms at baseline (Model 1, Table 4) and pre-migration and post-migration factors (Model 2, Table 4), the effect of neighborhood ethnic density on depressive symptomatology at follow-up was non-significant. At follow-up, in the adjusted Model 2, women had higher depressive symptomatology than men (β=2.10; SE=0.70; ρ<0.01); participants who grew-up mostly in rural, vs. urban/suburban, areas had lower depressive symptomatology (β=−1.60; SE=0.65; π<0.05); those who migrated for personal or family problems had higher depressive symptomatology than those who migrated for economic reasons (β=3.07; SE=1.10; π<0.01), and those engaging in recreational (β=−0.51; SE=0.24; π<0.05), or church related activities (β=−0.54; SE=0.27; π<0.05), had lower depressive symptomatology than those who did not. The initially positive association with perceived discrimination became non-significant in the adjusted Model 2 (Table 4).
Table 4.
Effect of neighborhood Puerto Rican density on depressive symptomatology at 2yr-follow-up among participants of the Puerto Rican Health Study
| Model 1 (a) | Model 2 (b) | Model 3 (c) | ||||||||
| β | (SE) | ρ-value | β | (SE) | ρ-value | Coeff | (SE) | ρ-value | ||
| Neighborhood Level | ||||||||||
| Neighborhood ethnic density | ||||||||||
| Low <15% (ref.) | − | − | − | |||||||
| High 15%≥ | −1.17 | 0.64 | 0.07 + | −0.97 | 0.66 | 0.15 | −2.93 | 1.52 | 0.05 * | |
| Individual Level | ||||||||||
| Gender | ||||||||||
| Male (ref.) | − | − | ||||||||
| Female | 2.10 | 0.70 | 0.002 ** | −0.03 | 0.94 | 0.98 | ||||
| Pre-migration urbanicity (PMU) | ||||||||||
| Urban/suburban (ref.) | − | − | ||||||||
| Town | −1.42 | 0.90 | 0.12 | −1.28 | 0.90 | 0.15 | ||||
| Rural | −1.60 | 0.65 | 0.01 * | −1.53 | 0.65 | 0.02 * | ||||
| Reason for migration | ||||||||||
| Socioeconomic reasons (ref.) | − | − | ||||||||
| Family reunification/to take care of family | 0.89 | 0.66 | 0.18 | 0.87 | 0.66 | 0.19 | ||||
| Acces to health care services | −0.05 | 1.37 | 0.97 | −0.16 | 1.37 | 0.91 | ||||
| Personal and family problems | 3.07 | 1.10 | 0.01 ** | 3.20 | 1.10 | 0.004 ** | ||||
| Length of stay in the U.S. mainland | ||||||||||
| Less 15y (ref.) | − | − | ||||||||
| 15-24y | 0.59 | 1.31 | 0.48 | 0.39 | 1.31 | 0.77 | ||||
| 25-34y | 0.24 | 1.22 | 0.85 | 0.10 | 1.21 | 0.93 | ||||
| >35y | −0.26 | 1.17 | 0.82 | −0.33 | 1.17 | 0.78 | ||||
| Language acculturation quartiles | ||||||||||
| Q1 (Low) (ref.) | − | − | ||||||||
| Q2 | −0.59 | 0.80 | 0.46 | 1.34 | 1.23 | 0.27 | ||||
| Q3 | −0.40 | 0.87 | 0.64 | −0.44 | 1.22 | 0.72 | ||||
| Q4 (High) | −0.10 | 0.99 | 0.92 | −0.56 | 1.28 | 0.66 | ||||
| Perceived racial/ethnic/language discrimination | ||||||||||
| No|no answer (ref.) | − | |||||||||
| Yes | 0.54 | 0.64 | 0.40 | − | ||||||
| Recreational activities | −0.51 | 0.23 | 0.03 * | −0.53 | 0.23 | 0.02 * | ||||
| Friends and neighbors activities | −0.13 | 0.26 | 0.60 | − | ||||||
| Family activities | −0.45 | 0.26 | 0.09 + | − | ||||||
| Church related activities | −0.54 | 0.27 | 0.04 * | −0.60 | 0.26 | 0.02 * | ||||
| Neighborhood & Individual Interactions | ||||||||||
| Ethnic density (ED) × Sex | ||||||||||
| Low ED neighborhood & high ED males in (ref.) | − | |||||||||
| High ED females | 3.51 | 1.28 | 0.01 * | |||||||
| Ethnic density (ED) × language acculturation quartiles | ||||||||||
| Low ED residents & High ED in Q1-Low (ref.) | − | |||||||||
| High ED residents in Q2 | −3.41 | 1.60 | 0.03 * | |||||||
| High ED residents in Q3 | −0.0001 | 1.62 | 1.00 | |||||||
| High ED residents in Q4-High | 1.42 | 1.67 | 0.38 | |||||||
| Level-1 (individuals) η | 1204 | 1142 | 1142 | |||||||
| Level-2 (neighborhoods) η | 198 | 196 | 196 | |||||||
| Log Likelihood | −4467.1 | −4214.1 | −4208.6 | |||||||
ρ<0.001;
ρ<0.01;
ρ<0.05;
ρ<0.10
Model 1= sex + age + education + depressive symp. at baseline + neighborhood poverty level + neighborhood ethnic density
Model 2= Model 1 + pre-migration urbanicity + reason for migration + length of stay + language acculturation + perceived rac/eth/lang discrimination + recreational activities + friends&neighbors activities + family activities + church & other activities
Model 3= Model 2 + (ethnic density*sex) + (ethnic density*language acculturation)
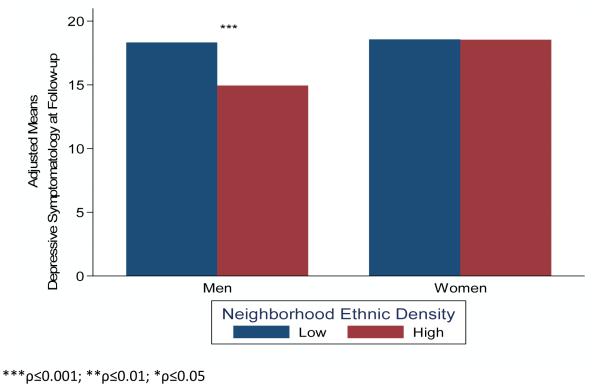
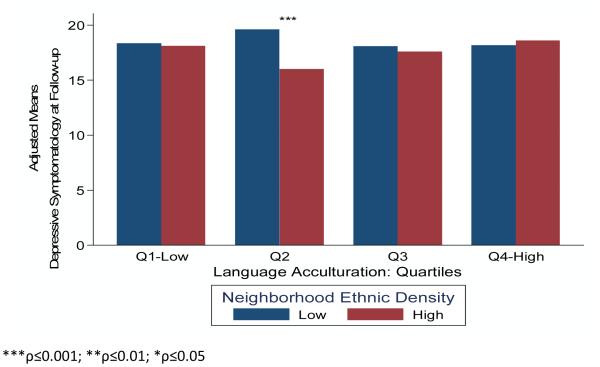
The association of neighborhood ethnic density with depressive symptoms at follow-up was significantly modified by sex and language acculturation (Model 3, Table 4). In stratified analysis, men (β=−3.93; SE=1.18; π=0.001), but not women (β=0.33; SE=0.78; π=0.671), experienced significantly lower depressive symptomatology in high, vs. low ethnic density neighborhoods (Figure 1a). Residing in high ethnic density neighborhoods was significantly associated with lower depressive symptomatology among participants in the second quartile of language acculturation (β=−4.21; SE=1.27; π=0.001), relative to those in the lowest (β=0.51; SE=1.41; π=0.718), third (β=−1.09; SE=1.31; π=0.407) and fourth quartiles (β=0.78; SE=1.43; π=0.585) (Figure 1b).
Figure 1a.
Neighborhood ethnic density and sex interactions on depressive symptoms (interaction p-value<0.01)
Figure 1b.
Neighborhood ethnic density and language acculturation interactions on depressive symptoms (interaction p-value<0.05)
DISCUSSION
The current study addresses research gaps in the immigrant health and ethnic density literature, and extends the Latino health literature by examining the health of Puerto Rican adults, a group with health disadvantages, relative to other Latino groups. Using a population-based cohort, our findings show a small and marginal protective effect of neighborhood ethnic density on depressive symptoms, after adjusting for neighborhood poverty level. These findings extend existing knowledge about the effects of ethnic density on the mental health of Latino immigrants (Gerst et al., 2011; Ostir, Eschbach, Markides, & Goodwin, 2003; Shell, Peek, & Eschbach, 2013), and other ethnic minority groups (Becares & Nazroo, 2013; Das-Munshi et al., 2010; Shaw et al., 2012). Results from this study support the need to adjust for poverty levels when examining the effects of ethnic density on individual health (Das-Munshi et al., 2010). In unadjusted analysis, higher neighborhood percentage of Puerto Ricans was associated with higher depressive symptomatology at baseline, and higher neighborhood poverty rates were significantly associated with higher depressive symptoms, at both baseline and follow-up. We add to this literature by testing ethnic density and mental health associations using longitudinal data to control for baseline depressive symptoms and individual demographics and to control for the high levels of poverty that often accompany immigrant enclaves.
These results also extend knowledge on immigrant health by using a cross-national framework that takes account of the influence of the sending and receiving societies. The significant associations of pre-migration urbanicity and reason for migration with depressive symptoms at follow-up, even though participants have resided in the U.S. mainland for an average of 27 years, indicate the significant influence that life experiences before migration may have on the health of immigrants over time, and how this influence may persist long after initial settlement. Participants who spent most of their growing years in their native country in a rural environment had lower depressive symptoms than participants raised in urban areas. Little is known about the influence of pre-migration urbanicity on immigrant health, and findings from population studies report mixed result. Some studies find lower prevalence of mental health disorders with rural areas of origin (Blazer, George, Landerman, & et al., 1985), while others show slightly higher rates of depression in those with rural (Probst et al., 2006) or small urban and semi-rural origins (Joshua Breslau, Marshall, Pincus, & Brown) relative to large urban areas. The seemingly deleterious effect of growing up in urban areas pre-migration, as seen in our study, may be associated with higher social isolation, adverse living conditions, and stress associated with poverty and unemployment that may be characteristic of urban areas (Moore, Gould, & Keary, 2003; Paykel, Abbott, Jenkins, Brugha, & Meltze, 2000). The established link between nutrition with mental health (Davison & Kaplan, 2012; Exebio, Zarini, Exebio, & Huffman, 2011; Gillen, Markey, & Markey, 2012) supports the possibility that geographic differences in dietary practices between rural and urban areas prior to migration may have conferred a protective effect to participants growing up in rural areas. Significant inverse associations between higher total fat and lower legume intakes and incidence of coronary heart disease were seen in urban, but not rural men in the Puerto Rico Heart Study (Garcia-Palmieri et al., 1980). Physical activity is also associated with mental health (Teychenne, Ball, & Salmon, 2008), and this was higher in rural than urban Puerto Rican men urban men (García-Palmieri et al., 1978). This childhood exposure may have provided long-lasting health benefits to participants in our study, as well. Post-hoc analyses of eating habits and physical activity at baseline by pre-migration urbanicity showed that participants from rural, vs. urban, pre-migration areas had significantly lower intake of saturated fat and alcohol, and marginally lower total energy intake, but no differences in levels of physical activity at the baseline measures for this study. The differences in dietary behavior may be related to behaviors acquired earlier in life during participant’s period of residence in rural areas pre-migration. Additional research is needed to examine the apparent salubrious effect of rural residence pre-migration on the health of immigrants post-migration.
Those who migrated to the U.S. mainland for personal or family related problems had higher depressive symptomatology than those who migrated for economic reasons. Reason for migration can be characterized as push/pull factors that motivate and create expectations about the new society, and involuntary or forced migration may be related to more problems with psychological adaptation (Berry, 1997). Reasons cited under the ‘personal and family problems’ category for migration included: to evade abusive relationships, and legal or political problems. These reasons suggest involuntary migration where support networks may have been left behind. Individual and social problems experienced pre-migration may have been experienced as highly stressful and potentially traumatic life events, which increases risk for later depressive disorders (Avison & Turner, 1988; Eaton, 1978; Esbensen & Benson, 2006). A history of traumatic life events may be prevalent among immigrants groups (Fortuna, Porche, & Alegria, 2008).
Perceived discrimination is a social stressor that affects mental health through psychological responses, including decreased positive emotion (e.g., well-being, positive self-perceptions, and self-esteem) and increased negative emotion (e.g., psychological distress, anger, and negative affect) (Pascoe & Richman, 2009). The non-significant effect of perceived discrimination on depressive symptomatology at follow-up, after controlling for baseline depressive score, suggests that participants’ perceptions of discrimination may be influenced by their mental health status. This finding contrasts with previous prospective studies that found a direct association between perceived discrimination and changes in mental health symptoms (Williams & Mohammed, 2009). A follow up measure of perceived discrimination was not available, which precluded ancillary analysis to test for the prospective effect of depressive symptomatology on perceived discrimination. Prospective studies examining perceived discrimination and health among immigrants, particularly Latino immigrants, are warranted.
Social variables influence health through different mechanisms. Social support is theorized to influence health indirectly by buffering the effects of stress while, in contrast, social integration is proposed to have a direct effect on health, independent of stress (Cohen, 2004). The non-significant effect modification of each of the four types of social activities on the neighborhood ethnic density and depressive symptomatology association supports Cohen’s premise of the direct, rather than indirect or modifying effect, of social integration factors on health (Cohen, 2004). In ancillary analysis we tested the effects of social support, both emotional and instrumental, and found no significant prospective associations with depressive symptomatology.
The protective effect of recreational activities on mental health is consistent with findings of better health outcomes and sense of well-being among adults who engage in greater number and diverse types of social activities throughout their life course (Berkman & Glass, 2000). Enjoyable leisure activities, in particular, have been associated with psychosocial and physical well-being (Pressman et al., 2009). The direct and beneficial effect of recreational and church related activities on depressive symptomatology may operate by promoting a sense of purpose, identity, meaning, belonging, and self-worth, as well as, via social controls and peer pressure that promote health behaviors (e.g., physical activity and healthy eating) (Cohen, 2004; Umberson et al., 2010). Acquiring a sense of community and belonging may be particularly important for immigrant mental health post-migration. In the host society, immigrants establish new social networks and re-define their social roles, which is a life course process influenced by the contextual conditions in the new society and availability of social and material resources. The significantly lower engagement in recreational activities among participants residing in high ethnic density neighborhood parallels recent findings of low physical activity in Latinos residing in immigrant enclaves (Osypuk, Roux, Hadley, & Kandula, 2009). Low physical and recreational activity in high ethnic density communities may be related to a limited availability of recreational facilities. Some studies have shown that Latino neighborhoods were almost nine times less likely to have recreational facilities than white neighborhoods (L. V. Moore, Diez Roux, Evenson, McGinn, & Brines, 2008).
Effect modification
An understanding of how the process of acculturation may influence immigrant health requires recognition of the context, including the local community, in which they settle, and the interactions among acculturation, context and behavioral factors (Schwartz et al., 2010; Zimmerman et al., 2011). Findings from this study show a differential effect of ethnic density on depressive symptomatology that is significantly modified by sex and level of language acculturation.
In contrast to earlier findings (Mair et al., 2010), our findings suggest that the effect of ethnic density is beneficial for men, but may not extend to women. Puerto Rican women had high depressive symptomatology (CES-D > 16) in both low and high ethnic density neighborhoods. Although residing in high ethnic density neighborhoods may provide direct access to social networks and resources, women may experience increased stress related to higher expectations to provide emotional support to others, and higher demands for instrumental support to extended family members residing in the same neighborhood (Parrado, Flippen, & McQuiston, 2005). Higher emotional support demands may provoke psychological distress (Durden, Hill, & Angel, 2007). This is in line with previous findings of a moderating effect of social support between life stressful events and psychological distress that benefited men, but not women in our study (Falcon, Todorova, & Tucker, 2009).
The non-linear modifying effect of quartiles of language acculturation on the association of ethnic density with depressive symptomatology is in contrast with the postulated effects of ethnic density neighborhoods on mental health. Ethnic density has been proposed to be beneficial to the least acculturated or recently arrived immigrants (Halpern & Nazroo, 2000), as ethnic enclaves provide material and functional support, often critical for getting by on a daily basis, as well as social support networks (Halpern & Nazroo, 2000). In contrast, residing in ethnic enclaves may have a potential harmful effect to those who fail to transition into neighborhoods with higher social and economic advantages (Cook, Alegria, Lin, & Guo, 2009; Nicklett & Burgard, 2009), possibly related to stressors associated with feelings of segregation, reduced access to economic opportunities and limited social mobility (Feldmeyer, 2009). In our analyses, participants residing in high ethnic density neighborhoods, and in the second quartile of acculturation group, were more likely to be men, from rural areas pre-migration, and to have higher engagement in family activities. It is possible that the differing effects of gender, the potential exposure to a more salubrious early environment, and greater family engagement on depressive symptomatology may have driven the non-linear associations. The non-linear modifying effects of language acculturation on the ethnic density and depressive symptomatology association may result from unaccounted residual confounding related to structural and institutional factors, host society’s perceptions of migrant populations and policies relevant to immigrant settlement. The contexts of reception influence greatly the process of acculturation and settlement patterns migrants adopt in the host society (Alegria, 2009).
The findings of the present study must be interpreted in light of a number of limitations. The sample included adult Puerto Ricans residing in a Northeast city of the U.S., and their experiences may not reflect those of Puerto Ricans residing in other regions, or to other Latino groups in the U.S. Unlike other Latino subgroups, the migration of Puerto Ricans is officially classified as internal migration as they enjoy the social and political benefits of U.S. citizenship. Future studies including national representative samples of individuals and geographic regions are needed to replicate our findings. Second, despite the longitudinal design, the observational nature of this study limits causal inference due to a threat to internal validity by unmeasured potential confounders.
CONCLUSION
Results from this study highlight the complexity, and interplay, of a number of factors that influence the health of immigrants, and emphasize the significance of moving beyond cultural variables to better understand why the health of some immigrant groups deteriorates at faster rates overtime. Research on immigrant health could benefit by incorporating a social determinants of health framework that incorporates and acknowledges the important influence of pre-migration and post-migration factors, and the interplay of these factors with the communities immigrants settle in. More studies are needed that examine that pathways through which ethnic density may confer health benefits to immigrants, and the relevant role of social engagement in activities other than family and friends activities. Implementation and promotion of leisure and recreational activities, in particular, seem to be a potential intervention strategy to reduce the identified high levels of depression experienced by Puerto Ricans in the U.S. mainland.
Supplementary Material
Research Highlights.
➢ We examined the longitudinal effect of ethnic density (ED) on depressive symptoms
➢ ED was associated with depressive symptoms (DS) at baseline, but not at follow-up
➢ Sex and language acculturation (LA) modified the ED-DS association at follow-up
➢ Men, but not women, experienced protective effects of neighborhood ED
➢ In non-linear interactions, participants in Q2 of LA had lower DS in high ED tracts
Acknowledgements
This study was funded by the National Institute on Aging (P01 AG023394) and National Heart, Lung, and Blood Institute; National Institutes of Health (P50 HL105185). The assistance of our field staff, data management team, and community members who participated in the study is gratefully acknowledged.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Abraido-Lanza AF, Armbrister AN, Florez KR, Aguirre AN. Toward a theory-driven model of acculturation in public health research. Am J Public Health. 2006;96(8):1342–1346. doi: 10.2105/AJPH.2005.064980. doi: Doi 10.2105/Ajph.2005.064980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Acevedo-Garcia D, Bates LM, Osypuk TL, McArdle N. The effect of immigrant generation and duration on self-rated health among US adults 2003-2007. Social Science & Medicine. 2010;71(6):1161–1172. doi: 10.1016/j.socscimed.2010.05.034. doi: DOI 10.1016/j.socscimed.2010.05.034. [DOI] [PubMed] [Google Scholar]
- Acevedo-Garcia D, Sanchez-Vaznaugh EV, Viruell-Fuentes EA, Almeida J. Integrating social epidemiology into immigrant health research: a cross-national framework. Soc Sci Med. 2012;75(12):2060–2068. doi: 10.1016/j.socscimed.2012.04.040. doi: 10.1016/j.socscimed.2012.04.040. [DOI] [PubMed] [Google Scholar]
- Alegria M. The Challenge of Acculturation Measures: What are we missing? A commentary on Thomson & Hoffman-Goetz. Soc Sci Med. 2009;69(7):996–998. doi: 10.1016/j.socscimed.2009.07.006. doi: 10.1016/j.socscimed.2009.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alegria M, Canino G, Shrout PE, Woo M, Duan N, Vila D, Meng XL. Prevalence of mental illness in immigrant and non-immigrant U.S. Latino groups. Am J Psychiatry. 2008;165(3):359–369. doi: 10.1176/appi.ajp.2007.07040704. doi: 10.1176/appi.ajp.2007.07040704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alegria M, Mulvaney-Day N, Torres M, Polo A, Cao Z, Canino G. Prevalence of psychiatric disorders across Latino subgroups in the United States. Am J Public Health. 2007;97(1) doi: 10.2105/AJPH.2006.087205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Avison WR, Turner RJ. Stressful Life Events and Depressive Symptoms: Disaggregating the Effects of Acute Stressors and Chronic Strains. Journal of Health and Social Behavior. 1988;29(3):253–264. doi: 10.2307/2137036. [PubMed] [Google Scholar]
- Becares L, Nazroo J. Social capital, ethnic density and mental health among ethnic minority people in England: a mixed-methods study. Ethn Health. 2013;18(6):544–562. doi: 10.1080/13557858.2013.828831. doi: 10.1080/13557858.2013.828831. [DOI] [PubMed] [Google Scholar]
- Becares L, Shaw R, Nazroo J, Stafford M, Albor C, Atkin K, Pickett K. Ethnic density effects on physical morbidity, mortality, and health behaviors: a systematic review of the literature. Am J Public Health. 2012;102(12):e33–66. doi: 10.2105/AJPH.2012.300832. doi: 10.2105/ajph.2012.300832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berkman LF, Glass T. Social Integration, Social Networks, Social Support, and Health. In: Berkman LF, Kawachi I, editors. Social Epidemiology. Oxford University Press; New York: 2000. [Google Scholar]
- Berry JW. Immigration, acculturation, and adaptation. Applied psychology. 1997;46(1):5–34. [Google Scholar]
- Berry JW. The Cambridge Handbook of Acculturation Psychology. Cambridge University Press; Cambridge: 2006. Contexts of acculturation; pp. 27–42. D. L. S. a. J. W. B. 27-42. [Google Scholar]
- Birman D, Trickett E, Buchanan R. A tale of two cities: replication of a study on the acculturation and adaptation of immigrant adolescents from the former Soviet Union in a different community context. Am J Community Psychol. 2005;35(1-2):83–101. doi: 10.1007/s10464-005-1891-y. [DOI] [PubMed] [Google Scholar]
- Blazer D, George LK, Landerman R, et al. Psychiatric disorders: A rural/urban comparison. Archives of General Psychiatry. 1985;42(7):651–656. doi: 10.1001/archpsyc.1985.01790300013002. doi: 10.1001/archpsyc.1985.01790300013002. [DOI] [PubMed] [Google Scholar]
- Braveman P, Barclay C. Health disparities beginning in childhood: a life-course perspective. Pediatrics. 2009;124(3):S163–175. doi: 10.1542/peds.2009-1100D. [DOI] [PubMed] [Google Scholar]
- Breslau J, Borges G, Hagar Y, Tancredi D, Gilman S. Immigration to the USA and risk for mood and anxiety disorders: variation by origin and age at immigration. Psychol Med. 2009;39(7):1117–1127. doi: 10.1017/S0033291708004698. doi: 10.1017/s0033291708004698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Breslau J, Marshall GN, Pincus HA, Brown RA. Are mental disorders more common in urban than rural areas of the United States? J Psychiatr Res. 56:50–55. doi: 10.1016/j.jpsychires.2014.05.004. doi: 10.1016/j.jpsychires.2014.05.004. [DOI] [PubMed] [Google Scholar]
- Burgos G, Rivera FI. Residential Segregation, Socio-economic Status, and Disability: A Multi-Level Study of Puerto Ricans in the United States. Centro Journal. 2012;24(11):14–46. [Google Scholar]
- Clarke P, Morenoff J, Debbink M, Golberstein E, Elliott MR, Lantz PM. Cumulative Exposure to Neighborhood Context: Consequences for Health Transitions Over the Adult Life Course. Research on Aging. 2013 doi: 10.1177/0164027512470702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen S. Social Relationships and Health. American Psychologist. 2004;59(8):676–684. doi: 10.1037/0003-066X.59.8.676. [DOI] [PubMed] [Google Scholar]
- Cook B, Alegria M, Lin J, Guo J. Pathways and correlates connecting Latinos’ mental health with exposure to the United States. Am J Public Health. 2009;99(12):2247–2254. doi: 10.2105/AJPH.2008.137091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- D'Anna LH, Ponce NA, Siegel JM. Racial and ethnic health disparities: evidence of discrimination's effects across the SEP spectrum. Ethn Health. 2010;15(2):121–143. doi: 10.1080/13557850903490298. [DOI] [PubMed] [Google Scholar]
- Das-Munshi J, Becares L, Dewey ME, Stansfeld SA, Prince MJ. Understanding the effect of ethnic density on mental health: multi-level investigation of survey data from England. BMJ. 2010;341:c5367. doi: 10.1136/bmj.c5367. doi: 10.1136/bmj.c5367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davison KM, Kaplan BJ. Nutrient Intakes Are Correlated With Overall Psychiatric Functioning in Adults With Mood Disorders. Can J Psychiatry. 2012;57(2):85–92. doi: 10.1177/070674371205700205. [DOI] [PubMed] [Google Scholar]
- Durden ED, Hill TD, Angel RJ. Social demands, social supports, and psychological distress among low-income women. Journal of Social and Personal Relationships. 2007;24(3):343–361. [Google Scholar]
- Eaton WW. Life Events, Social Supports, and Psychiatric Symptoms: A Re-Analysis of the New Haven Data. Journal of Health and Social Behavior. 1978;19(2):230–234. doi: 10.2307/2136537. [PubMed] [Google Scholar]
- Eaton WW, Anthony JC, Gallo J, Cai G, Tien A, Romanoski A, Chen L-S. Natural history of Diagnostic Interview Schedule/DSM-IV major depression: The Baltimore epidemiologic catchment area follow-up. Archives of General Psychiatry. 1997;54(11):993–999. doi: 10.1001/archpsyc.1997.01830230023003. [DOI] [PubMed] [Google Scholar]
- Esbensen AJ, Benson BA. A prospective analysis of life events, problem behaviours and depression in adults with intellectual disability. J Intellect Disabil Res. 2006;50:248–258. doi: 10.1111/j.1365-2788.2005.00816.x. Pt 4. doi: 10.1111/j.1365-2788.2005.00816.x. [DOI] [PubMed] [Google Scholar]
- Exebio JC, Zarini GG, Exebio C, Huffman FG. Healthy Eating Index scores associated with symptoms of depression in Cuban-Americans with and without type 2 diabetes: a cross sectional study. Nutrition Journal. 2011;10(135):1–7. doi: 10.1186/1475-2891-10-135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Falcon LM, Todorova I, Tucker K. Social support, life events, and psychological distress among the Puerto Rican population in the Boston area of the United States. Aging Ment Health. 2009;13(6):863–873. doi: 10.1080/13607860903046552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Falcon LM, Tucker KL. Prevalence and correlates of depressive symptoms among Hispanic elders in Massachusetts. J Gerontol B Psychol Sci Soc Sci. 2000;55(2):S108–116. doi: 10.1093/geronb/55.2.s108. [DOI] [PubMed] [Google Scholar]
- Feldmeyer B. Immigration and violence: The offsetting effects of immigrant concentration on Latino violence. Social Science Research. 2009;38(3):717–731. doi: 10.1016/j.ssresearch.2009.03.003. [DOI] [PubMed] [Google Scholar]
- Fortuna L, Porche M, Alegria M. Political violence, psychosocial trauma, and the context of mental health services use among immigrant Latinos in the United States. Ethn Health. 2008;13(5):435–463. doi: 10.1080/13557850701837286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- García-Palmieri M, Costas RJ, Cruz-Vidal M, Cortés-Alicea M, Patterne D, Rojas-Franco L, Kannel W. Urban-rural differences in coronary heart disease in a low incidence area. The Puerto Rico heart study. Am J Epidemiol. 1978;107(3):206–215. doi: 10.1093/oxfordjournals.aje.a112527. [DOI] [PubMed] [Google Scholar]
- Garcia-Palmieri M, Sorlie P, Tillotson J, Costas RJ, Cordero E, Rodriguez M. Relationship of dietary intake to subsequent coronary heart disease incidence: The Puerto Rico Heart Health Program. Am J Clin Nutr. 1980;33(8):1818–1827. doi: 10.1093/ajcn/33.8.1818. [DOI] [PubMed] [Google Scholar]
- Gerst K, Miranda P, Eschbach K, Sheffield K, Peek M, Markides K. Protective neighborhoods: neighborhood proportion of Mexican Americans and depressive symptoms in very old Mexican Americans. J Am Geriatr Soc. 2011;59(2):353–358. doi: 10.1111/j.1532-5415.2010.03244.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gillen MM, Markey CN, Markey PM. An examination of dieting behaviors among adults: Links with depression. Eating Behaviors. 2012;13(2012):88–93. doi: 10.1016/j.eatbeh.2011.11.014. 13, 88–93. [DOI] [PubMed] [Google Scholar]
- Glymour MM, Mujahid M, Wu Q, White K, Tchetgen EJ. Neighborhood Disadvantages and Self-Assessed Health, Disabilty, and Depressive Symptoms: Longitudinal Results From the Health and Retirement Study. Annals of Epidemiology. 2010 doi: 10.1016/j.annepidem.2010.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Halpern D, Nazroo J. The Ethnic Density Effect: Results From a National Community Survey of England and Wales. Int J Soc Psychiatry. 2000;46(1):34–46. doi: 10.1177/002076400004600105. doi: 10.1177/002076400004600105. [DOI] [PubMed] [Google Scholar]
- Hamilton LC. Statistics with STATA. 9 Brooks/Cole; Belmong, CA: 2009. [Google Scholar]
- Hunt LM, Schneider S, Comer B. Should "acculturation" be a variable in health research? A critical review of research on US Hispanics. Social Science & Medicine. 2004;59(5):973–986. doi: 10.1016/j.socscimed.2003.12.009. doi: DOI 10.1016/j.socsimed.2003.12.009. [DOI] [PubMed] [Google Scholar]
- Kawachi I, Kim D, Coutts A, Subramanian S. Commentary: Reconciling the three accounts of social capital. International Journal of Epidemiology. 2004;33(682-690) doi: 10.1093/ije/dyh177. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Berglund P, Demler O, Jin R, Koretz D, Merikangas K, Wang P. The epidemiology of major depressive disorder: results from the National Comorbidity Survey Replication (NCS-R) JAMA. 2003;289(23):3095–3105. doi: 10.1001/jama.289.23.3095. [DOI] [PubMed] [Google Scholar]
- Krieger N. Discrimination and health. In: Berkman L, Kawachi I, editors. Social Epidemiology. Oxford University Press; Oxford: 2000. pp. 36–75. [Google Scholar]
- Landale NS. Migration and the Latino Family: The Union Formation Behavior of Puerto Rican Women. Demography. 1994;31(1):133–157. [PubMed] [Google Scholar]
- Landale NS, Oropesa RS. Migration, Social Support and Perinatal Health: An Origin-Destination Analysis of Puerto Rican Women. Journal of Health and Social Behavior. 2001;42(2):166–183. doi: 10.2307/3090176. [PubMed] [Google Scholar]
- Lester H. Ethnic density and mental health. BMJ. 2010;341:c5252. doi: 10.1136/bmj.c5252. doi: 10.1136/bmj.c5252. [DOI] [PubMed] [Google Scholar]
- Levasseur M, Richard L Gauvin L, E. R. Inventory and analysis of definitions of social participation found in the aging literature: proposed taxonomy of social activities. Soc Sci Med. 2010;71(12):2141–2149. doi: 10.1016/j.socscimed.2010.09.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Llácer A, Zunzunegui MV, del Amo J, Mazarrasa L, Bolůmar F. The contribution of a gender perspective to the understanding of migrants’ health. Journal of Epidemiology and Community Health. 2007;61(Suppl 2):ii4–ii10. doi: 10.1136/jech.2007.061770. http://jech.bmj.com/content/61/Suppl_2/ii4.abstract %U. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mahard RE. The CES-D as a measure of depressive mood in the elderly Puerto Rican population. Journal of Gerontology. 1988;43(1):24–25. doi: 10.1093/geronj/43.1.p24. [DOI] [PubMed] [Google Scholar]
- Mair C, Roux AVD, Osypuk TL, Rapp SR, Seeman T, Watson KE. Is neighborhood racial/ethnic composition associated with depressive symptoms? The multi-ethnic study of atherosclerosis. Social Science & Medicine. 2010;71(3):541–550. doi: 10.1016/j.socscimed.2010.04.014. doi: DOI 10.1016/j.socscimed.2010.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marin G, Sabogal F, Marin BV, Otero-Sabogal R, Perez-Stable EJ. Development of a Short Acculturation Scale for Hispanics. Hisp J Behav Sci. 1987;9(2):183–205. doi: 10.1177/07399863870092005. [Google Scholar]
- Massachusetts Budget and Policy Center Facts at a Glance: Census Bureau shows no change in poverty rate in Massachusetts. 2008 http://www.massbudget.org/reports/pdf/CensusPoverty2007[1].pdf. [Google Scholar]
- Massey DS. Residential Segregation of Mexicans, Puerto Ricans, and Cubans in U.S. Metropolitan Areas. Sociology and Social Research. 1989;73:73–83S. [Google Scholar]
- Merikangas KR, Ames M, Cui L, Stang PE, Ustun TB, Von Korff M, Kessler RC. The Impact of Comorbidity of Mental and Physical Conditions on Role Disability in the US Adult Household Population. Arch Gen Psychiatry. 2007;64(10):1180–1188. doi: 10.1001/archpsyc.64.10.1180. doi: 10.1001/archpsyc.64.10.1180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moore, Gould P, Keary B. Global urbanization and impact on health. Int J Hyg Environ Health. 2003;206(4-5):269–278. doi: 10.1078/1438-4639-00223. [DOI] [PubMed] [Google Scholar]
- Moore LV, Diez Roux AV, Evenson KR, McGinn AP, Brines SJ. Availability of Recreational Resources in Minority and Low Socioeconomic Status Areas. American journal of preventive medicine. 2008;34(1):16–22. doi: 10.1016/j.amepre.2007.09.021. doi: 10.1016/j.amepre.2007.09.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nicklett E, Burgard S. Downward social mobility and major depressive episodes among Latino and Asian-American immigrants to the United States. American Journal of Epidemiology. 2009;170(6):793–801. doi: 10.1093/aje/kwp192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ornelas I, Perreira K. The role of migration in the development of depressive symptoms among Latino immigrant parents in the USA. Social Science & Medicine. 2011;73(8):1169–1177. doi: 10.1016/j.socscimed.2011.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ortega AN, Feldman JM, Canino G, Steinman K, Alegria M. Co-occurrence of mental and physical illness in US Latinos. Soc Psychiatry Psychiatr Epidemiol. 2006;41(12):927–934. doi: 10.1007/s00127-006-0121-8. doi: 10.1007/s00127-006-0121-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ostir G, Eschbach K, Markides K, Goodwin J. Neighbourhood composition and depressive symptoms among older Mexican Americans. J Epidemiol Community Health. 2003;57(12):987–992. doi: 10.1136/jech.57.12.987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Osypuk TL, Acevedo-Garcia D. Beyond individual neighborhoods: A geography of opportunity perspective for understanding racial/ethnic health disparities. Health Place. 2010;16(6):1113–1123. doi: 10.1016/j.healthplace.2010.07.002. doi: DOI 10.1016/j.healthplace.2010.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Osypuk TL, Roux AVD, Hadley C, Kandula NR. Are immigrant enclaves healthy places to live? The Multi-ethnic Study of Atherosclerosis. Social Science & Medicine. 2009;69(1):110–120. doi: 10.1016/j.socscimed.2009.04.010. doi: DOI 10.1016/j.socscimed.2009.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parrado E, Flippen C, McQuiston C. Migration and relationship power among Mexican women. Demography. 2005;42(2):347–372. doi: 10.1353/dem.2005.0016. [DOI] [PubMed] [Google Scholar]
- Pascoe EA, Richman LS. Perceived Discrimination and Health: A Meta-Analytic Review. Psychological bulletin. 2009;135(4):531–554. doi: 10.1037/a0016059. doi: 10.1037/a0016059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paykel ES, Abbott R, Jenkins R, Brugha TS, Meltze H. Urban–rural mental health differences in Great Britain: findings from the National Morbidity Survey. Psychological Medicine. 2000;30(2):269–280. doi: 10.1017/s003329179900183x. [DOI] [PubMed] [Google Scholar]
- Pressman SD, Matthews KA, Cohen S, Martire LM, Scheier M, Baum A, Schulz RL. Association of Enjoyable Leisure Activities With Psychological and Physical Well-Being. Psychosom Med. 2009;71(7):725–732. doi: 10.1097/PSY.0b013e3181ad7978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Probst JC, Laditka SB, Moore CG, Harun N, Powell MP, Baxley EG. Rural-Urban Differences in Depression Prevalence: Implications for Family Medicine. Fam Med. 2006;38(9):653–660. [PubMed] [Google Scholar]
- Radloff LS. The CES-D Scale: A Self-Report Depression Scale for Research in the General Population. Applied Psychological Measurement. 1977;1(3):385–401. doi: 10.1177/014662167700100306. [Google Scholar]
- Raudenbush S, Bryk AS. Hierarchical linear models: Applications and data analysis methods. 2nd Sage Publications; Thousand Oaks, CA: 2002. [Google Scholar]
- Roux AVD, Mair C. Neighborhoods and health. Biology of Disadvantage: Socioeconomic Status and Health. 2010;1186:125–145. doi: DOI 10.1111/j.1749-6632.2009.05333.x. [Google Scholar]
- Sampson RJ. Neighborhood-Level Context and Health: Lessons from Sociology. In: Kawachi I, L. F. Berkman, editors. Neighborhoods and Health. Oxford, University Press; New York, NY: 2003. [Google Scholar]
- Schwartz SJ, Unger JB, Zamboanga BL, Szapocznik J. Rethinking the concept of acculturation: implications for theory and research. Am Psychol. 2010;65(4):237–251. doi: 10.1037/a0019330. doi: 10.1037/a0019330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaw RJ, Atkin K, Becares L, Albor CB, Stafford M, Kiernan KE, Pickett KE. Impact of ethnic density on adult mental disorders: narrative review. Br J Psychiatry. 2012;201(1):11–19. doi: 10.1192/bjp.bp.110.083675. doi: 10.1192/bjp.bp.110.083675. [DOI] [PubMed] [Google Scholar]
- Shell AM, Peek MK, Eschbach K. Neighborhood Hispanic composition and depressive symptoms among Mexican-descent residents of Texas City, Texas. Social Science & Medicine. 2013;99:56–63. doi: 10.1016/j.socscimed.2013.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stuber J, Meyer I, Link B. Stigma, prejudice, discrimination and health. Social Science and Medicine. 2008;67:351–357. doi: 10.1016/j.socscimed.2008.03.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teychenne M, Ball K, Salmon J. Physical activity and likelihood of depression in adults: A review. Preventive Medicine. 2008;2008;46:397–411. doi: 10.1016/j.ypmed.2008.01.009. 46, 397–411. [DOI] [PubMed] [Google Scholar]
- Truong KD, Ma S. A systematic review of relations between neighborhoods and mental health. Journal of Mental Health Policy and Economics. 2006;9:137–154. [PubMed] [Google Scholar]
- Tucker KL, Mattei J, Noel SE, Collado BM, Mendez J, Nelson J, Falcon LM. The Boston Puerto Rican Health Study, a longitudinal cohort study on health disparities in Puerto Rican adults: challenges and opportunities. BMC Public Health. 2010;10:107. doi: 10.1186/1471-2458-10-107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Umberson D, Crosnoe R, Reczek C. Social Relationships and Health Behavior Across Life Course. Annu Rev Sociol. 2010;1(36):139–157. doi: 10.1146/annurev-soc-070308-120011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams DR, Mohammed SA. Discrimination and racial disparities in health: evidence and needed research. Journal of Behavioral Medicine. 2009;32(1):20–47. doi: 10.1007/s10865-008-9185-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zambrana RE, Carter-Pokras O. Role of acculturation research in advancing science and practice in reducing health care disparities among Latinos. Am J Public Health. 2010;100(1):18–23. doi: 10.2105/AJPH.2008.138826. doi: 10.2105/ajph.2008.138826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zimmerman C, Kiss L, Hossain M. Migration and health: a framework for 21st century policy-making. PLoS Med. 2011;8(5):e1001034. doi: 10.1371/journal.pmed.1001034. doi: 10.1371/journal.pmed.1001034. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.