Abstract
Background
Self-reported hypertension has not been validated in specific Hispanic subgroups (Puerto Ricans, Dominicans) and in Asian Americans. The objectives were to assess validity of self-reported hypertension in Hispanic and Asian American adults, and to recalibrate self-reported hypertension with measured values.
Methods
Data were from the New York City Community Health Survey 2005-08 and the Heart Follow-Up Study (HFUS) 2010 (included measured hypertension). Sensitivity and specificity were calculated in the HFUS data; recalibration was conducted using a previously described method by Mentz et al.
Results
Sensitivity was similar in Puerto Ricans and Dominicans versus whites. The differences in hypertension prevalence after recalibration were largest in Hispanics. No substantial differences occurred among Asian Americans.
Discussion
Factors such as low health literacy or insurance status are potential explanations for bias in self-reported hypertension among Hispanic subgroups. Surveillance systems may consider recalibration, potentially in areas with a high percentage of Hispanics or uninsured.
Keywords: Hypertension, Validation, Surveillance, Immigrant Populations
Background
Cardiovascular disease is the leading cause of death both nationally(1) and in New York City (NYC),(2) and hypertension (HTN) is a leading modifiable risk factor affecting approximately 1 in 4 NYC adults.(3) Since the Immigration Act of 1965, immigration from Latin America and Asian countries has increased steadily,(4) with many individuals settling in metropolitan areas such as NYC.(5, 6) Population-level surveillance of HTN in these populations is critical for understanding health patterns, identifying health disparities, and developing targeted interventions.
Self-reported HTN has been validated in white, black, and Mexican-American populations using national data with the lowest sensitivity and specificity values observed in Mexican-American men.(7) Validity was also lower among those who reported no medical visits compared to those with at least one visit in the past year, implying that access to care may have bearing on the ability to accurately self-report HTN. To date, only one other study on validation of self-reported HTN has been performed in a diverse population living in an urban area using local data.(8) The study used representative data from Detroit (~80% black or Hispanic), and found few differences between racial/ethnic groups in terms of validity of self-reported HTN. The racial/ethnic composition of NYC, differs from Detroit and from the nation; 2.7 million NYC adults (44%) are foreign-born, and foreign-born adults are more likely to be uninsured than U.S.-born adults (22% vs. 9%).(9) Further, the majority of Hispanics in NYC are from the Dominican Republic (18.8%) or Puerto Rico (36.5%) rather than from Mexico (3.5%), and there is also a substantial Asian American population(13%).(10-13) Given that limited access to health care and language barriers may impact a respondent's ability to report HTN accurately, validation in these recent immigrant groups is important for ensuring the accuracy of chronic disease surveillance in diverse populations.
The objective of this analysis was 1) to assess validity of self-reported HTN in foreign-born, Hispanic, and Asian American adults living in NYC and 2) to recalibrate the prevalence of self-reported HTN to clinically measured HTN in a representative NYC sample.
Methods
Data Collection
Data were obtained from the NYC Community Health Survey (CHS) 2005-08 and the 2010 Heart Follow-Up Study (HFUS). The CHS is a random-digit dial, cross-sectional survey of 8,000 to 10,000 adult New Yorkers that has been conducted annually since 2002 in English, Spanish, Russian and Chinese. The CHS uses a disproportionate stratified (by age, racial/ethnicity, sex, and neighborhood) random sample design to allow for estimates at the city, borough, and neighborhood levels.(14) The data are weighted to account for probability of selection and nonresponse, and post-stratified using population control totals for age, race/ethnicity, sex, and neighborhood. Data from 2005-08 were combined; observations were excluded if self-report of HTN was missing (n=123), resulting in an unweighted sample size of 36,550.
The HFUS was a cross-sectional survey conducted to assess sodium intake in a representative sample of NYC adults, aged 18 years and older. CHS 2010 participants were randomly selected (n=6,799), and for those who agreed to participate in the HFUS (n=2,305), we asked survey questions related to cardiovascular disease and nutrition, and sent a urine collection kit with written instructions to their homes to collect their urine for 24 hours. Following the collection period, a medical technician made a home visit for those who signed the informed consent form to pick up urine samples, measure anthropometry (height and weight), and take 3 seated, consecutive blood pressure (BP) measurements (according to the National Health and Nutrition Examination [NHANES] protocol).(16) The technicians used validated, clinic-grade BP monitors and standardized arm and body positions to measure BP.(17) Participants were instructed not to consume caffeine or to exercise 30 minutes prior to the visit, and they rested for 5 minutes prior to measurement. From all analyses of the HFUS data, those with incomplete urine samples (n=119) were excluded.(15, 18) The observations from one technician were excluded (n=86) because of an error that systematically produced low readings. Those missing measured blood pressure and data on anti-hypertensive medication use were additionally excluded (n=2). The final analytic sample size was 1,568. Further details about sampling and measurement have been described elsewhere.(15) The Institutional Review Board of the NYC Health Department approved this study.
Measures
Self-reported HTN status in the CHS and HFUS was defined as an affirmative response to the question: “Have you ever been told by a doctor or other health care professional that you have hypertension, also called high blood pressure?” Variables required to define clinical HTN for population surveillance: a) 3 seated, consecutive blood pressure measurements and b) self-report of current anti-HTN medication use (19) came from the HFUS data. “Measured HTN” was defined by the average of three BP measurements (systolic ≥ 140 mm Hg; diastolic ≥ 90 mm Hg) or self-reported antihypertensive medication usage.
Race/ethnicity was assessed using two questions on Hispanic origin and race group, and was categorized as non-Hispanic white, non-Hispanic black, Hispanic, non-Hispanic Asian and non-Hispanic other (hereafter referred to as ‘white’, ‘black’, and ‘Asian’). Due to small sample size, results from the non-Hispanic other race category are not presented. Hispanic was additionally broken down into those who reported being born in Puerto Rico or the Dominican Republic. Participants could select from different types of insurance (employer, self-purchase, Medicare, Medicaid/Family Health+, Military/CHAMPUS/Tricare, COBRA/Other, uninsured); responses were collapsed to create a dichotomous variable coded ‘insurance’ or ‘no insurance’. Nativity was defined as self-reported birthplace and was categorized as either being born in the U.S. or elsewhere. Puerto Ricans and those born in U.S. territories were defined as being U.S.-born. Languages spoken at home were English, Spanish, or other (includes Russian, Chinese, and Indian language speakers). Poverty status was assessed as combined household income, grouped according to the 2010 federal poverty guidelines determined by the U.S. Department of Health and Human Services.(20)
Analysis
All estimates except for sensitivity and specificity were weighted to be representative of the NYC population. We first described demographic characteristics for both the HFUS and CHS. Sensitivity and specificity of self-reported HTN were calculated in the clinical HTN estimates in the HFUS data, and confidence intervals (CI) were calculated using Fisher's exact test.(21) Differences in sensitivity and specificity, and between self-reported HTN and recalibrated HTN, were evaluated based on the overlap of 95% CIs. The prevalence of self-reported HTN was estimated using the CHS and age-adjusted to the U.S. 2000 standard population.
Self-reported HTN from the CHS was recalibrated using measured HTN based on the method developed by Mentz and colleagues.(8) The method requires population-based representative estimates of the prevalence of self-reported HTN in the geographic area of interest (i.e., NYC), and contemporaneous data on measured HTN from a representative survey restricted to the same area of interest (i.e., HFUS 2010 data).
The steps were as follows:
- Two logistic regression models with clinical HTN as the dependent variable were estimated using HFUS data; independent variables in the model were chosen based on the literature as likely predictors of clinical HTN and were age, sex, race/ethnicity, poverty group, education and insurance status. The regression equation used for both models was as follows:
The first model was fitted in the HFUS sample for those who had self-reported HTN (SRi=1); the second model was fitted in those who did not have self-reported HTN (SRi=0). Analyses (and therefore resulting β coefficients) were weighted to the overall NYC population using weights developed for the HFUS subsample.Equation 1 - The regression coefficients from the first model (restricted to those with self-reported HTN, SRi=1), were plugged into Equation 2 (shown below) from Mentz et al. to obtain a recalibrated estimate of sensitivity.
The regression coefficients from the second model (restricted to those without self-reported HTN, SRi=0), were plugged into Equation 3 (shown below) to obtain a recalibrated estimate of specificity.Equation 2
Where and are the vectors of point estimates from the two logistic regression models fitted in the HFUS sample. CHi is equal to clinical HTN.Equation 3 A threshold value of 0.50(8) was applied to the recalibrated sensitivity and specificity values for each individual; anyone with a recalibrated sensitivity or specificity of >0.50 was considered to have predicted clinical HTN, those with a sensitivity or specificity of ≤0.50 were considered not to have predicted clinical HTN. Hereafter we refer to the predicted clinical HTN as ‘recalibrated HTN’.
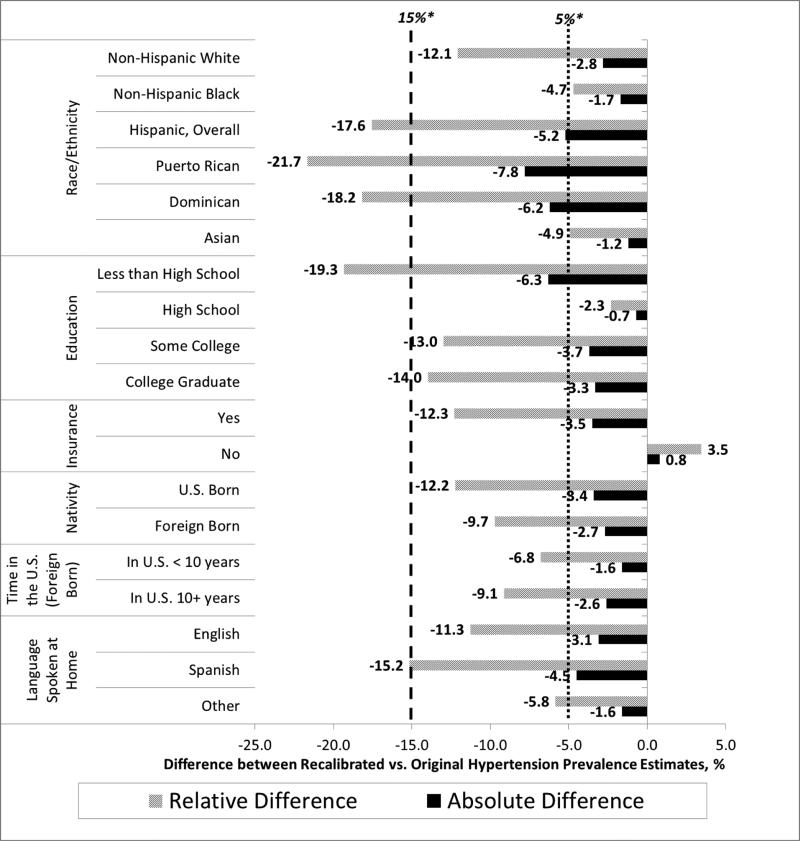
Comparisons between the self-reported and recalibrated HTN prevalence estimates were conducted using cutoffs of a 5% absolute difference and a 15% relative difference.
All analyses (validation and HTN prevalence estimates) were performed overall and stratified by covariates (race/ethnicity, education, insurance status, nativity, length of time in the U.S. among foreign-born, language spoken at home). Analyses were conducted using SUDAAN (version 10.0; Research Triangle Institute, Research Triangle Park, North Carolina) and SAS (version 9.2; SAS Inc., Cary, North Carolina).
Results
The participant characteristics for the HFUS and CHS samples displayed in Table 1 were similar overall. Those who agreed to participate in the HFUS, compared with those who did not, were slightly more likely to be Hispanic, <65 years of age, lower income, and obese; there were no meaningful differences in self-reported general health status between CHS and HFUS participants.(15) About half of both samples were female (54%), black or Hispanic (47%), had an education level of high school or less (41-46%), and were foreign-born (43%). The majority had insurance (82-83%); spoke English at home (70-72%); and of those who were foreign born, had been in the U.S. for 10+ years (76-79%). For self-reported HTN among the 1,568 HFUS participants, 449 were labeled as true positive, 918 as true negative, 88 as false positive, and 109 as false negatives. The sensitivity and specificity were 80% (95% CI: 77, 84) and 91% (95% CI: 89, 93), respectively (Table II). A lower sensitivity was observed in men (74%, [95% CI: 67, 79]) compared to women (85%, [95% CI: 88, 93]). Sensitivity was also lower in those without insurance compared to those with insurance (67% [95% CI: 54, 79] vs. 82% [95% CI: 78, 85]) and in those in the US for <10 years compared to 10+ years (63% [95% CI: 41, 81] vs. 85% [95% CI: 78, 89]), though the confidence intervals overlapped with referent groups. Specificity was lower in those with a less than high school education compared to those with a college education (80% [95% CI: 73, 87] vs. 94% [95% CI: 92, 96]). Though the confidence intervals overlapped, blacks had a slightly lower specificity than whites (88% [95% CI: 83, 92] vs. 94% [95% CI: 91, 96]. No meaningful differences for sensitivity and specificity measures were observed for Puerto Ricans, Dominicans or Asians compared to whites, or between acculturation-related factors overall
Table I.
Select Characteristics in the Heart Follow-Up Study 2010 and the Community Health Survey 2005-08
| HFUS 2010 | CHS 2005-08 | |||||
|---|---|---|---|---|---|---|
| n | Weighted n | weighted % | n | Weighted n | weighted % | |
| Overall | 1568 | 5,906,000 | 100.0 | 36,550 | 6,059,061 | 100.0 |
| Sex | ||||||
| Male | 659 | 2,716,000 | 46.0 | 14,158 | 2,793,000 | 46.2 |
| Female | 909 | 3,190,000 | 54.0 | 22,392 | 3,256,000 | 53.8 |
| Race/Ethnicity | ||||||
| Non-Hispanic White | 584 | 2,279,000 | 38.6 | 14,745 | 2,351,000 | 38.9 |
| Non-Hispanic Black | 413 | 1,363,000 | 23.1 | 9,299 | 1,386,000 | 22.9 |
| Hispanic, Overall | 456 | 1,419,000 | 24.0 | 8,868 | 1,496,000 | 24.7 |
| Puerto Rican | 79 | 196,000 | 3.3 | 1,622 | 182,000 | 3.0 |
| Dominican | 114 | 305,000 | 5.2 | 1,887 | 299,000 | 5.0 |
| Asian | 81 | 624,000 | 10.6 | 2,585 | 623,000 | 10.3 |
| Education | ||||||
| Less than High | ||||||
| School | 248 | 1,224,000 | 20.8 | 6,123 | 975,000 | 16.3 |
| High School | 308 | 1,577,000 | 26.7 | 8,892 | 1,475,000 | 24.7 |
| Some College | 374 | 1,251,000 | 21.2 | 7,437 | 1,258,000 | 21.1 |
| College Graduate | 635 | 1,846,000 | 31.3 | 13,613 | 2,261,000 | 37.9 |
| Insurance | ||||||
| Yes | 1342 | 4,780,000 | 82.0 | 30,899 | 4,905,000 | 82.8 |
| No | 213 | 1,048,000 | 18.0 | 4,959 | 1,016,000 | 17.2 |
| Nativity | ||||||
| U.S. Born | 986 | 3,328,000 | 56.4 | 22,260 | 3,427,000 | 56.8 |
| Foreign Born | 581 | 2,573,000 | 43.6 | 14,205 | 2,609,000 | 43.2 |
| In U.S. < 10 years | 97 | 543,000 | 21.1 | 1,938 | 464,000 | 24.5 |
| In U.S. 10+ years | 482 | 2,025,000 | 78.9 | 8,472 | 1,427,000 | 75.5 |
| Language Spoken at Home | ||||||
| English | 1184 | 4,216,000 | 71.5 | 26,954 | 4,213,000 | 70.0 |
| Spanish | 251 | 904,000 | 15.3 | 5,306 | 932,000 | 15.5 |
| Other | 129 | 774,000 | 13.1 | 4,097 | 873,000 | 14.5 |
Table II.
Sensitivity and Specificity, by Select Covariates, HFUS 2010
| Sensitivity % (95% CI) | Specificity % (95% CI) | |||
|---|---|---|---|---|
| Overall | 81 | (77, 84) | 91 | (89, 93) |
| Sex | ||||
| Male | 74 | (67,79) | 92 | (89, 94) |
| Female | 85 | (81, 89) | 91 | (88, 93) |
| Race/Ethnicity | ||||
| Non-Hispanic White (Ref) | 81 | (74, 86) | 94 | (91, 96) |
| Non-Hispanic Black | 87 | (81, 91) | 88t | (83, 92) |
| Hispanic, Overall | 73 | (66, 80) | 89 | (85, 93) |
| Puerto Rican | 81 | (66, 91) | 89 | (74, 97) |
| Dominican | 81 | (67, 91) | 91 | (81, 97) |
| Asian | 79 | (54, 94) | 94 | (84, 98) |
| Education | ||||
| Less than High School | 86 | (78, 92) | 80* | (73, 87) |
| High School | 80 | (72, 86) | 95 | (90, 98) |
| Some College | 79 | (71, 86) | 89 | (85, 93) |
| College Graduate (Ref) | 78 | (72, 84) | 94 | (92, 96) |
| Insurance | ||||
| Yes (Ref) | 82 | (78, 85) | 91 | (89, 93) |
| No | 67† | (54, 79) | 92 | (87, 96) |
| Nativity | ||||
| U.S. Born (Ref) | 80 | (75, 84) | 92 | (89, 94) |
| Foreign Born | 82 | (76, 87) | 91 | (87, 93) |
| In U.S. < 10 years | 63t | (41, 81) | 96 | (88, 99) |
| In U.S. 10+ years (Ref) | 85 | (78, 89) | 89 | (85, 93) |
| Language Spoken at Home | ||||
| English (Ref) | 82 | (78, 85) | 91 | (89, 93) |
| Spanish | 77 | (67, 85) | 92 | (85, 95) |
| Other | 77 | (63, 88) | 95 | (88, 99) |
95% confidence intervals do not overlap with estimates in referent group
Meaningful difference vs. referent group although 95% CI overlap
The prevalence of HTN in the CHS was 27.8 (95% CI: 27.3, 28.3), while the recalibrated HTN prevalence was 24.7 (95% CI: 24.2, 25.1). In men, HTN prevalence before and after recalibration did not differ (27.2, [95% CI: 26.4, 28.0] vs. 27.0, [95% CI: 26.2. 27.7], respectively), while in women, the self-reported prevalence was higher than the recalibrated value (28.1, [95%CI: 27.5, 28.8] vs. 22.6, [95%CI: 22.1, 23.2], respectively). The prevalence estimates of HTN in the CHS in Hispanics overall, Puerto Ricans, Dominicans and Asians were 29.6, 34.1, 36.0, and 24.4, respectively; and the recalibrated estimates were 24.4, 28.2, 27.9 and 23.2, respectively (Supplemental Table). The self-reported and recalibrated HTN prevalence estimates stratified by the remaining covariates are displayed in the Supplemental Table.
Overall the absolute difference between the recalibrated and the self-reported HTN prevalence was 3.1%; the relative difference was 11.0%. The difference between the recalibrated and self-reported prevalence estimates was largest in Hispanics overall (4.7% absolute, 17.6% relative differences); Puerto Ricans (7.8% absolute, 21.7% relative); Dominicans (6.2% absolute, 18.2% relative); those with less than a high school education (6.3% absolute, 19.3% relative); and in those speaking Spanish at home (4.5% absolute, 15.2% relative; Figure 1). Large differences were also observed but were similar across categories by insurance status, nativity, length of time in the U.S., and in those with higher education. Recalibration did not produce substantial changes for HTN estimates in Asian Americans.
Figure 1.
Absolute and Relative % Differences in Recalibrated vs. Self-reported Hypertension Prevalence Estimates, CHS 2005-08 and HFUS 2010
Discussion
Validity of self-reported HTN was good-to-fair in this ethnically diverse sample. Sensitivity was lowest among Hispanics, the uninsured, those who spoke Spanish at home, and foreign-born adults who had been in the U.S. for <10 years. Specificity did not differ markedly across groups. Interestingly, sensitivity and specificity in Puerto Ricans, Dominicans (but not in Hispanics overall), Asians and foreign-born NYC residents were similar to whites and those who were U.S.-born. Previously published analyses in national samples have demonstrated that self-reported HTN is the least accurate in the Mexican American subgroup.(7) Similarly in the current analysis, Hispanics who were not Dominican or Puerto Rican had the lowest likelihood of reporting HTN when clinical HTN was present. Lack of health insurance or limited access to care may help explain some of these differences since Puerto Ricans and Dominicans are more likely to have health insurance than other Hispanic subgroups.(22)
After applying the recalibration methodology, self-reported HTN prevalence in the CHS tended to be slightly overestimated in all groups, with the largest differences observed in women; in Hispanics (overall, Puerto Ricans, and Dominicans); and in those with less than a high school education. Low health literacy related to HTN and health in general might have also led to reporting errors in these groups; previous studies have shown that underreporting is less likely due to misreporting and more related to a lack of diagnosis.(23). These findings also suggest that cultural differences in the definition of HTN may lead to misreporting, and may be a factor that affects HTN self-reporting. In addition to misreporting, those who self-reported HTN but did not have clinical HTN according to the study definition may have been able to achieve control through lifestyle modification (e.g., physical activity, reducing sodium intake, quitting smoking, etc.). The sample size of false positives (n=88) and false negatives (n=109) precluded meaningful exploration of these factors. This may be an important consideration when using self-reported HTN as the definition for tracking and surveillance in Hispanics.
The similarity in validity of self-reported HTN for Asians compared to whites is a novel contribution to the current understanding of these population surveillance measures. The ability to accurately self-report HTN may be linked to having health insurance. Overall, health insurance coverage among Asians is similar, or slightly lower, than that among whites in NYC;(24) however this access differs widely when data are stratified by specific Asian subgroups (e.g., Chinese, Korean, Asian Indians), with Koreans being the least likely to have health insurance.(25) We were unable to explore Asian American subgroup in this analysis due to limited sample size. Thus, it is critical to conduct validation studies of self-reported HTN by specific Asian subgroups and health insurance status where data are available.
The current analysis contributes to understanding the validity of self-reported hypertension in rapidly growing, yet understudied minority subgroups. Among this study's strengths is that clinical hypertension was assessed using measured values derived from a rigorous clinical protocol that was based on the NHANES blood pressure measurement methods using validated BP monitors.(16, 17) Also, results were weighted to be representative of the NYC non-institutionalized adult population as a whole. Limitations include the potential misclassification of HTN from BP measured at one time point, although an average of three BP measurements was used at that one time point. The small sample size of Asians restricted the ability to explore specific Asian subgroups.
Self-reported HTN performed relatively well in this diverse urban population. Practical consideration of health literacy, access to health care and HTN control by lifestyle modification are critical to the use of self-reported HTN for surveillance. In the absence of annually recurring measured data, surveillance measures can be recalibrated to help improve the individual-level validity of estimates in a given year, potentially in areas with a high percentage of Hispanics. More recent acknowledgement to these smaller subgroups have been reflected to changes to the sampling strategy of NHANES, the primary national surveillance system for health and related behaviors; oversampling of Hispanics other than Mexican-Americans began in 2007, and of Asian Americans in 2011. Local or urban areas with racial/ethnic population distributions that differ markedly from the national distribution may consider recalibrating self-reported HTN in their populations to ensure valid estimates.
New Contribution to the Literature
Immigration patterns in the last 50 years have introduced large numbers of Hispanic and Asian adults to the U.S. population. Surveillance of chronic disease is critical for program planning and in understanding health disparities. Self-reported hypertension, a commonly used measure on surveys has only been validated in white, black and Mexican-Americans in the U.S. The current analysis demonstrated that Hispanics and Asians have similar validity (sensitivity, specificity) for self-report of hypertension compared to measured hypertension, but Hispanics may overreport more than other race/ethnicities. Insurance status was associated with more valid reporting, and this may be a meaningful factor when considering racial/ethnic differences in self-report of hypertension.
Supplementary Material
Acknowledgements
The HFUS was made possible by funding from the Robert Wood Johnson Foundation, the New York State Health Foundation, the National Association of County & City Health Officials and the Centers for Disease Control and Prevention [Grant Number 5U38HM000449-02], the W.K. Kellogg Foundation, the U.S. Department of Health and Human Services, and New York City tax levy dollars. This funding is administered by the Fund for Public Health in New York, a private non-profit organization that supports innovative initiatives of the NYC DOHMH. The New York University Center for the Study of Asian American Health is supported by the NIH/NIMHD cooperative agreement number 2P60MD000538-10.The contents of this article are solely the responsibility of the authors and do not necessarily represent the official view of the funders.
References
- 1.National Vital Statistics Reports Deaths: Final Data for 2009. 60(3) http://www.cdc.gov/nchs/data/nvsr/nvsr60/nvsr60_04.pdf. [PubMed] [Google Scholar]
- 2.Summary of Vital Statistics 2010: The City of New York, Population and Mortality. The New York City Department of Health and Mental Hygiene; 2012. http://www.nyc.gov/html/doh/downloads/pdf/vs/vs-population-and-mortality-report.pdf. [Google Scholar]
- 3.Angell SY, Garg RK, Gwynn RC, Bash L, Thorpe LE, Frieden TR. Prevalence, awareness, treatment, and predictors of control of hypertension in New York City. Circ Cardiovasc Qual Outcomes. 2008;1(1):46–53. doi: 10.1161/CIRCOUTCOMES.108.791954. [DOI] [PubMed] [Google Scholar]
- 4.America's Foreign Born in the Last 50 Years. United States Census Bureau; [June 10, 2014]. http://www.census.gov/how/infographics/foreign_born.html. [Google Scholar]
- 5.Frey W. The New Metropolitan Minority Map: Regional Shifts in Hispanics, Asians, and Blacks from Census 2010. Metropolitan Policy Program, Brookings; 2011. http://www.brookings.edu/research/papers/2011/08/31-census-race-frey. [Google Scholar]
- 6.Hirschman C. Immigration and the American century. Demography. 2005;42(4):595–620. doi: 10.1353/dem.2005.0031. [DOI] [PubMed] [Google Scholar]
- 7.Vargas CM, Burt VL, Gillum RF, Pamuk ER. Validity of self-reported hypertension in the National Health and Nutrition Examination Survey III, 1988-1991. Prev Med. 1997;26(5 Pt 1):678–85. doi: 10.1006/pmed.1997.0190. [DOI] [PubMed] [Google Scholar]
- 8.Mentz G, Schulz AJ, Mukherjee B, Ragunathan TE, Perkins DW, Israel BA. Hypertension: development of a prediction model to adjust self-reported hypertension prevalence at the community level. BMC Health Serv Res. 2012;12:312. doi: 10.1186/1472-6963-12-312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kim MVW, Kerker G, Thorpe B, Frieden L, TR . The Health of Immigrants in New York City. New York City Department of Health and Mental Hygiene; New York: 2006. [March 17, 2014]. Available at: http://www.nyc.gov/html/doh/downloads/pdf/episrv/episrv-immigrant-report.pdf. [Google Scholar]
- 10. [Jan 9, 2014];New York City Census Query. https://sasebiweb200.health.dohmh.nycnet/epiquery/Census/index2010.html.
- 11.NYC . Results from the 2000 Census, Demographic/Household Characteristics & Asian and Hispanic Subgroups. New York City Department of City Planning; 2000. [June 10, 2014]. http://www.nyc.gov/html/dcp/pdf/census/nyc20002.pdf. [Google Scholar]
- 12.U.S. Hispanic Country of Origin Counts for Nation, Top 30 Metropolitan Areas. Pew Research Center; [June 10, 2014]. http://www.pewhispanic.org/2011/05/26/us-hispanic-country-of-origin-counts-for-nation-top-30-metropolitan-areas/. [Google Scholar]
- 13.Hoeffel EM, Rastogi S, Kim MO, Shahid H. [Jan 9, 2014];The Asian Population: 2010 Census Briefs. Issued March 2012; https://www.census.gov/prod/cen2010/briefs/c2010br-11.pdf.
- 14. [Jan 9, 2014];The New York City Community Health Survey. http://www.nyc.gov/html/doh/html/survey/survey.shtml.
- 15.Sanderson M, Yi S, Bartley K, Quitoni K, Curtis C, Angell S, et al. The Community Health Survey, Heart Follow-Up Study Methodology Report. The New York City Department of Health and Mental Hygiene; 2012. http://www.nyc.gov/html/doh/html/diseases/hfus.shtml. [Google Scholar]
- 16.National Health and Nutrition Examination Survey (NHANES) Health Tech/Blood Pressure Procedures Manual. http://www.cdc.gov/nchs/data/nhanes/nhanes_09_10/BP.pdf.
- 17.Ostchega Y, Nwankwo T, Sorlie PD, Wolz M, Zipf G. Assessing the validity of the Omron HEM-907XL oscillometric blood pressure measurement device in a National Survey environment. J Clin Hypertens (Greenwich) 2010;12(1):22–8. doi: 10.1111/j.1751-7176.2009.00199.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Angell SY, Yi S, Eisenhower D, Kerker BD, Curtis CJ, Bartley K, et al. Sodium Intake in a Cross-Sectional, Representative Sample of New York City Adults. Am J Public Health, e-View Ahead of Print. 2014 doi: 10.2105/AJPH.2013.301542. doi: 102105/AJPH2013301542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Crim MT, Yoon SS, Ortiz E, Wall HK, Schober S, Gillespie C, et al. National surveillance definitions for hypertension prevalence and control among adults. Circ Cardiovasc Qual Outcomes. 2012;5(3):343–51. doi: 10.1161/CIRCOUTCOMES.111.963439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Poverty guidelines for the remainder of 2010. US Department of Health and Human Services; [February 1, 2014]. Available at: http://aspe.hhs.gov/poverty/10poverty.shtml. [Google Scholar]
- 21. [Jan 9, 2014];SAS Usage Note 24170: Estimating sensitivity, specificity, positive and negative predictive values, and other statistics. http://support.sas.com/kb/24/170.html.
- 22.Daviglus ML, Talavera GA, Aviles-Santa ML, Allison M, Cai J, Criqui MH, et al. Prevalence of major cardiovascular risk factors and cardiovascular diseases among Hispanic/Latino individuals of diverse backgrounds in the United States. JAMA. 2012;308(17):1775–84. doi: 10.1001/jama.2012.14517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bowlin SJ, Morrill BD, Nafziger AN, Jenkins PL, Lewis C, Pearson TA. Validity of cardiovascular disease risk factors assessed by telephone survey: the Behavioral Risk Factor Survey. J Clin Epidemiol. 1993;46(6):561–71. doi: 10.1016/0895-4356(93)90129-o. [DOI] [PubMed] [Google Scholar]
- 24.Pulsford RM, Stamatakis E, Britton AR, Brunner EJ, Hillsdon MM. Sitting behavior and obesity: evidence from the Whitehall II study. Am J Prev Med. 2013;44(2):132–8. doi: 10.1016/j.amepre.2012.10.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Katzmarzyk PT, Church TS, Craig CL, Bouchard C. Sitting time and mortality from all causes, cardiovascular disease, and cancer. Medicine & Science in Sports & Exercise. 2009 doi: 10.1249/MSS.0b013e3181930355. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.