Abstract
The intensity of the conflict such as war is one of the determinants of the flow of migrants and refuges with consequence of introducing infectious disease to other countries. This paper investigates the relationship between malaria incidence and forced immigration due to war from neighboring countries in Dezful district, southwestern Iran. All available data and accessible archived documentary records on malaria cases in the period 1988–2011 in Dezful Health Centers were reviewed. Retrospective analysis of routine surveillance data from the Health authority of Dezful district was conducted to assess the trend of malaria incidence and prevalence in the last two decades. Malaria transmission dynamics was described using surveillance indicators viz, Annual Parasite Incidence (API), Slide Positivity Rate (SPR), Annual Blood Examination Rate (ABER) and based on personal information of patients. Two peaks of malaria incidence occurred during past two decades. The first one arisen by Iran-Iraq war due to residential instability in Dezful while the API reached to 8 per 1000. The second peak happened after to civil war of Afghanistan began which caused large immigrates moved into the study area. During the second peak, API reached 1.7 per 1000 at maximum and the majority of patients were immigrants. This study describes the linkage between incidence and prevalence of malaria and immigration due to civil conflict. Therefore, malaria screening of immigrants and early warning programme are effective to prevent outbreak of disease in a potential risk area such Dezful.
Keywords: Imported malaria, Social conflicts, Neighboring countries, Iran
Introduction
Movement of malaria parasites by human migration to a potential country are likely to make epidemic the disease. Migration or population movement is one of the most important forces in modern-day malaria transmission and distribution in large measure due to global socio situation and transportation (1, 2). Some malarious countries, such as those in West Africa and central Asia are much more strongly connected to infection movement while some others such as Ethiopia and Myanmar display significantly greater isolation in terms of likely infection movements in and out (2, 3).
Moreover, many wars take place in countries with a high incidence of malaria. For instance the Afghan civil war takes place in a country where the incidence of malaria is high, and has generated six millions of refugees that, in principles, are at a very high risk of being infected (4, 5). However, the distribution and incidence of malaria, as for often-communicable diseases, can be affected by dispersal of refugees from one country to another in various ways. Refugees may transport malaria parasites from an endemic area to the host country or they may be more vulnerable when coming from a non-endemic area to an endemic area where they may lack natural immunity to local strains. Epidemic conditions may arise when non-immune immigrants are settled onto sites capable of supporting mosquito breeding (6–8). The 23-year conflict in Afghanistan caused one third of the Afghan population (about 6.2 million) fled the war to Pakistan and Iran (9).
Illegal cross border of Afghan refugees became an obsession of health authority regarding to eliminate malaria from Iran (10). Malaria control programs affected by mass movement of Afghani refugees into Pakistan after social conflict occurred in Afghanistan (9, 11, 12).
Since the global malaria eradication campaign ended in 1969, several countries have earmarked on programs aimed at elimination, and some have succeeded in achieving or nearing that goal (13). More recently, a growing number of countries have adopted malaria elimination as a goal and Iran has been listed in these countries to achieve this goal (13–15). Elimination entails reducing to zero the incidence of locally acquired malaria infection in a specific geographic area because of deliberate efforts, with continued measures in place to prevent re-establishment of transmission. Although Iran has been earmarked for elimination of malaria, illegal immigration from east neighbor countries threaten the elimination program. The most of them are immigrant job seekers, which they cause malaria, scatter in the country (16–18).
The present study focuses on malaria prevalence in Dezful district, where has been earmarked for malaria elimination but during 2 decades, malaria situation has been changed by occurring military conflicts in the neighboring countries in east and west. Khuzestan Province, located in southeast of Iran, is classified in strata II where the imported cases are found and the potential risk of malaria transmission exists (19).
Dezful district is situated in west of Khuzestan Province. The area is fertile with large scale of agricultural activities and water source. This district with numerous springs and pounds around Dez River and higher temperatures is expected to have greater malaria prevalence, as these conditions favor breeding of many Anopheline species as well as parasite reproduction within the mosquitoes. Dezful is still threatened by imported malaria, therefore assessment of malaria satiation in Dezful district may be used as a model for zones, which challenge with malaria elimination and straggling against the importation of malaria.
In the present study, we consider civil wars and social conflict as one of the basic reasons behind the observed increase in the incidence of malaria either directly (displacement of native inhabitants) or indirectly (influx of migrants from neighboring countries).
Materials & Methods
Study area
Dezful district is located in southwestern Iran, Khuzestan Province border to Iraq (following map). The area is bordered on the north and east by Zagrus Mountain Chain, south, and west by Khuzestan Plain (Fig.1). It is geographically located between latitude 32° 34′ 8″ N, and longitude 48° 34′ 0″ E. Generally, the area comprises mountainous, hilly regions in the north, with plains regions in the south and west. The region has a mild climate and generally, the temperature reaches to 40 °C during summer and near 10 °C during winter. The water sources are permanent and temporary rivers, wells springs, ponds and pools. The annual rainfall ranged from 100 to 120 mm. The rainfall occasionally received during winter (20).
Fig. 1:

Dezful district location in the map of Iran. Migrant workers across the country to reach to Dezful district which located in west of Iran
Health service
By integrating malaria control activities into Primary Health Care (PHC) in 1988, all rural and urban areas have PHC services. There are 9 Urban Health centers, 9 rural Health Centers and 59 Health Houses in Dezful district.
In addition, there are 3 governmental hospitals and one private as well as ten clinical laboratories in the study area which give clinical services to malaria patients free of charge. In Dezful area, malaria control activities are responsibility of health workers. At the village level, all cases suffering fever are referred to the Health House to have blood smear examination and all malaria positive cases will have antimalaria drugs. Therefore, all malaria diagnosis and treatment of patients’ as well as vector control is undertaken by PHC services free of charge. In addition, Behvaz provide a first point of contact, health education, and a mechanism of referral for local people.
Study design
All available and accessible archived documentary records on malaria cases in the period 1988–2011 in the Health authority of Dezful district were reviewed. Following simple arrangement of archival records, all inclusion and exclusion data such patient details and history of travels, parasite types and treatment were entered in Microsoft Excel sheet, and then the collected documentary records were checked by two researchers. A desk-based retrospective analysis was used to assess the trend of malaria incidence and prevalence in the last two decades. Malaria transmission dynamics was described using surveillance indicators viz, Annual Parasite Incidence (API), Slide Positivity Rate (SPR), Annual Blood Examination Rate (ABER) and also based on personal information of patients.
Data analysis
The dynamics of malaria transmission was analyzed using surveillance indicators viz, API, SPR, ABER as well as age and nationality of cases. Incidence rates of total malaria cases including Plasmodium vivax and P. falciparum malaria were estimated and graphed to describe their transmission dynamics in Dezful district. All diagnosis was based on microscopic examination of a thick and thin blood smear. Malaria surveillance in Dezful District was described using case detection rate as number of malaria cases detected/1000 slides examined/month and number of cases reported positive yearly separately for active and passive surveillance in the period of 1988–2011. Proportionate malaria cases based on their age and nationalities were estimated during the period of study.
Results
Two peaks of malaria incidence occurred during past two decades. Number of malaria cases reached to maximum peak in 1992 while the population of the area was unstable due to Iran/Iraq war. Subsequently, when the health services of Dezful became reorganized and caused malaria control programs especially case finding activities boosted, therefore, the number of malaria cases decreased. Consequently, API declined from 0.84 during 1992–1993 to 0.03 during 1998–1999 (Fig. 2). Once more, by strengthening malaria surveillance system in 2002, more positive cases were found and SPR raised as a small peak of API appeared in 2003.
Fig. 2:

Annual Parasite Index (API), Smear Positive Rate (SPR) and Annual Blood Examination Rate (ABER) in Deful district 1988–2011. Two malaria rate prevalence peaks occurred during two decades. The first peaks emerged after Iran/Iraq post-war period when the residents returned to Dezful and the second peak appeared when the civil conflict began in Afghanistan
The age ratio of malaria patients was also varied during two decades. About 57.4% of total malaria cases were young people (under 15 years old) in period of 1988–1996. Then the prevalence of disease (under 15 years old) rapidly declined as the results of enhancing malaria control programs. Therefore, total cases of young patients reached to 11% in period of 1997–2011 (Fig. 3).
Fig. 3:
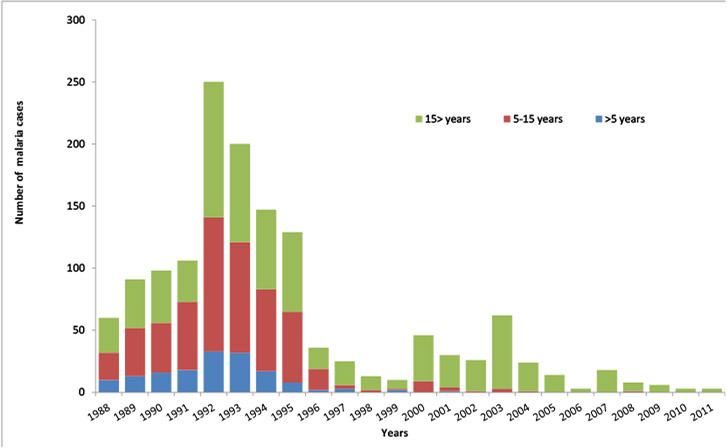
Number of malaria cases based on age category. The incidence of malaria in first decade was very high in young groups in Dezful district. This may be related to unstable condition of residents after war and occurring malaria transmission. Consequently, by supporting case finding and vector control programmes, not only the incidence of malaria declined, also incidence of the disease significantly decreased
Following to enhancement of disease surveillance, no malaria cases under 5 years old reported in last decade.
The number of malaria cases was extremely high among during period of 1988–1995 (Fig. 4). However, it decline rapidly in 1996. During the first decade, the majority of malaria cases were Iranian residents but in second period, the number of Iranian cases rapidly declined. In contrary, the most malaria patients were afghan immigrants (Fig. 4).
Fig 4:
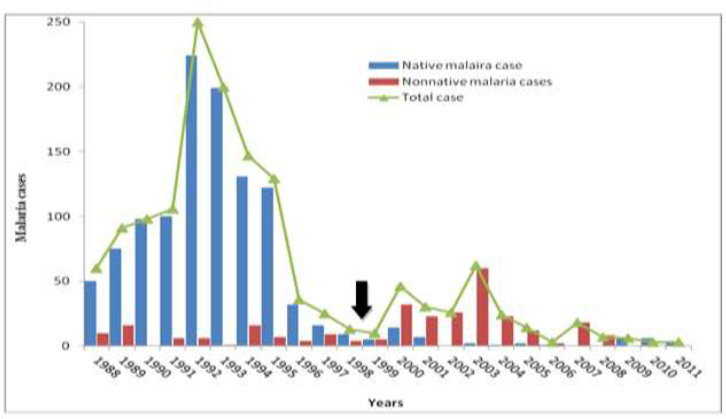
Number of malaria cases based on nationality in Dezful distirct since 1988 up to 2011. In the period 2000–2008, the incidence of malaria among non-Iranian immigrants was distinctly higher than Iranians. In addition all migrant patients were from eastern neighborhood countries. The arrow show when the civil conflict of Afghanistan began
The ratio of indigenous cases was varied during two decades. The most of malaria patients was indigenous during between 1988 and 1996 but this ratio shifted to imported malaria since 1998. The number of imported malaria cases reached to maximum peak in 2003 and then rapidly declined (Fig. 5).
Fig 5:
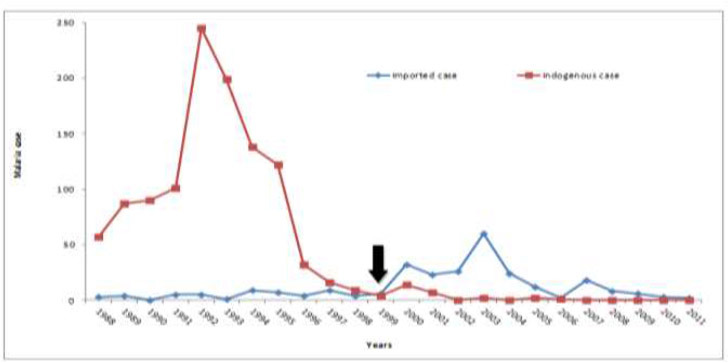
Imported and indigenous malaria cases sine 1988 up to 2011 in Dezful district. The number of imported malaria cases increased from 1999 after civil conflict occurred in Afghanistan. All imported malaria cases had Afghan nationality. The arrow show when the civil conflict of Afghanistan began
Discussion
During two decades, we analyzed data of malaria transmission to elucidate the affect of civil conflicts on the disease incidence. The results of current study can provide new outlook on malaria control planning for not only in any ravaged regions but also neighboring countries. However, the consequence of conflicts and warfare of neighboring countries on Dezful malaria, presented in this paper, provide an important insight into the factors that contribute to increased risk for malaria in certain regions. Malaria risk was found to be dependent on population situation and movement (1, 2). As expected, during unstable social condition during first decade, relatively high malaria infection rate was observed among young populations (under 15 years old). This may indicate that exposure of people to mosquito bites was relatively high due to unfavoured situation of their shelters (Fig. 3).
There are many important consequences related with the health status of people in ravaged regions where suffering war or civil conflict. However, presence of appropriate environment for malaria vectors in Dezful should be considered.
Malariology treaties insist on some social conditions that favor the incidence of malaria (21). Wars, social conflict and therefore force migration had important reasons for increasing risk of malaria in some Asian countries (22, 23). We also observed similar situation in Dezful district due to two wars. Firstly, after Iraq-Iran war which caused displacement of inhabitant population? In addition, by Afghanistan civil war, numerous refugees migrated into Iran as well as Dezful district. The immigrants changed the situation of malaria situation in Dezful. However, migrants and internally displaced populations are particularly vulnerable to the risk of malaria, as the camps in which they live are often in environments prone to vector breeding (11).
Dezful is fertile area with large scale of agricultural activities and water source. The warfare had altered the local ecology of many parts of the District, leaving agricultural fields untended and susceptible to collecting water in which mosquitoes may breed. Therefore, transmission of malaria was relatively high after war when the native people resettled to the area. Subsequently by reorganizing malaria control program and boosting case finding activities in the area, the prevalence of malaria declined until 1999. During post-war period, malaria-control strategies were mainly on malaria cases finding and treatment in Dezful. At the same time, vector control programmes, such as larviciding and residual indoor spraying was only performed in high-risk zones (personal communication).
As data show, malaria situation again increased from 1999 in Dezful and the majority of malaria cases were Afghani (Fig. 4 & 5) but by improvement of socio-economic situation in Dezful, malaria incidence have been noticeably increased. In recent years, south-eastern province of Iran, Sistan-Baluchistan Province straggles with imported malaria (24) and the cross-border movements has a important role for incidence and prevalence of the disease (10, 17, 24). Due to illegal immigration, usually many Afghanis avoided to use health service and the main reason was they were worried about being deported from country therefore the health system was unable to cope malaria among them (10). Similar study was performed on changing the spatial pattern of malaria in the Northwest Frontier Province in Pakistan between 1972 and 1997 and related it to the influx of more than two and a half million Afghan refugees (25).
According to health police of Iranian Ministry of Health, anti-malaria drugs are generally available free of charge in governmental clinics and health authorities. Therefore, all malaria patients including non-Iranian nationalities must attended to governmental malaria clinics for treatment but the immigrants’ apprehension for deporting play as an impact factor for case find activities (10, 17).
According to the records, all Afghanis patients were job seekerwhich passed across the country, reached to Dezful and then settled in unequipped shelters with poor protection condition against mosquito bites. Four malaria vectors exist in Dezful district and therefore local transmission is always possible. In addition, migrants do not carry prophylactic nor protective measures against the mosquito biting because malaria transmission is not their priority (26).
There is no doubt the effect of population movement on malaria is treated widely as infected people who move into malaria-free regions may introduce the parasite into new areas particularly those have appropriate vectors (26). All mobile populations are not usually reached by government malaria control programmes in Iran and many other malarious countries. Most studies upon which these efforts are based treat human groups as stable entities and do not account for possible mobility (8, 27). Thus mobile populations fall out of the loop of most public health efforts since temporary homes often cannot be identified and therefore, do not receive services.
However, the area is earmarked for malaria elimination but presence of illegal migrants with their own treatment seeking behaviour confounds anti-malaria operations. Thus, such as the use of bed nets and access to anti-malarial drugs may be vital for reducing risk in the study area.
Conclusion
In fact, in area such as Dezful district, population movement (caused by political conflicts or civil wars) is potentially the most important factor in the transmission of malaria and this study illustrates attention to the manner in which forced population influx and settlement can alter the ecology of malaria, leading to long-term changes in the geography of malaria.
Ethical considerations
Ethical issues (Including plagiarism, informed consent, misconduct, data fabrication and/or falsification, double publication and/or submission, redundancy, etc.) have been completely observed by the authors.
Acknowledgements
The authors declare that there is no conflict of interests. This work was financially supported by grants from Tehran University of Medical Sciences.
References
- 1. Martens P, Hall L. ( 2000). Malaria on the move: human population movement and malaria transmission. Emerg Infect Dis, 6: 103– 9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Tatem AJ, Smith DL. ( 2010). International population movements and regional Plasmodium falciparum malaria elimination strategies. Proc Natl Acad Sci U S A, 107: 12222– 7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Pichainarong N, Chaveepojnkamjorn W. ( 2004). Malaria infection and life-style factors among hilltribes along the Thai-Myanmar border area, northern Thailand. Southeast Asian J Trop Med Public Health, 35: 834– 9. [PubMed] [Google Scholar]
- 4. Pilsczek FH. ( 1996). A visiting doctor's perspective in Afghanistan: poverty, civil war, and private medicine. Lancet, 348: 1566– 8. [DOI] [PubMed] [Google Scholar]
- 5. Aliev S, Saparova N. ( 2001). [Current malaria situation and its control in Tadjikistan]. Med Parazitol (Mosk): 35– 7. [PubMed] [Google Scholar]
- 6. Gautret P, Schlagenhauf P, Gaudart J, Castelli F, Brouqui P, von Sonnenburg F, Loutan L, Parola P. ( 2009). Multicenter EuroTravNet/GeoSentinel study of travel-related infectious diseases in Europe. Emerg Infect Dis, 15: 1783– 90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Genton B, Loutan L. ( 2007). [Global warming and malaria: a hot debate]. Rev Med Suisse, 3: 1219– 20. [PubMed] [Google Scholar]
- 8. Loutan L. ( 2007). [Migrants: new travelers in a mobile world?]. Rev Prat, 57: 861– 6. [PubMed] [Google Scholar]
- 9. Rowland M, Rab MA, Freeman T, Durrani N, Rehman N. ( 2002). Afghan refugees and the temporal and spatial distribution of malaria in Pakistan. Soc Sci Med, 55: 2061– 72. [DOI] [PubMed] [Google Scholar]
- 10. Basseri HR, Raeisi A, Holakouie K, Shanadeh K. ( 2010). Malaria prevention among Afghani refugees in a malarious area, southeastern Iran. Bull Soc Pathol Exot, 103: 340– 5. [DOI] [PubMed] [Google Scholar]
- 11. Rowland M, Nosten F. ( 2001). Malaria epidemiology and control in refugee camps and complex emergencies. Ann Trop Med Parasitol, 95: 741– 54. [DOI] [PubMed] [Google Scholar]
- 12. Rowland M, Webster J, Saleh P, Chandramohan D, Freeman T, Pearcy B, Durrani N, Rab A, Mohammed N. ( 2002). Prevention of malaria in Afghanistan through social marketing of insecticide-treated nets: evaluation of coverage and effectiveness by cross-sectional surveys and passive surveillance. Trop Med Int Health, 7: 813– 22. [DOI] [PubMed] [Google Scholar]
- 13. Tatem AJ, Smith DL, Gething PW, Kabaria CW, Snow RW, Hay SI. ( 2011). Ranking of elimination feasibility between malaria-endemic countries. Lancet, 376: 1579– 91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. WHO ( 2008) Global malaria action plan for a malaria-free would. In: Partnership WHOTRBM, World Health Organization, Geneva: pp. 274. [Google Scholar]
- 15. Akbari H, Majdzadeh R, Rahimi Foroushani A, Raeisi A. ( 2013). Timeliness of malaria surveillance system in iran. Iran J Public Health, 42: 39– 47. [PMC free article] [PubMed] [Google Scholar]
- 16. Holakouie Naieni K, Malekafzali H, Rashidian A, Vazirian P, Moradi G, Mirzazadeh A, Mirmohammadkhani M, Shamshiri A. ( 2012). Malaria Status in Economic Cooperation Countries; Achievement and Gaps toward United Nations Millennium Development Goals. Iran J Public Health, 41: 7– 13. [PMC free article] [PubMed] [Google Scholar]
- 17. Raeisi A, Gouya MM, Nadim A, Ranjbar M, Hasanzehi A, Fallahnezhad M, Sakeni M, Safari R, Saffari M, Mashyekhi M, Ahmadi Kahnali A, Mirkhani V, Almasian E, Faraji L, Paktinat Jalali B, Nikpour F. ( 2013). Determination of Malaria Epidemiological Status in Iran's Malarious Areas as Baseline Information for Implementation of Malaria Elimination Program in Iran. Iran J Public Health, 42: 326– 33. [PMC free article] [PubMed] [Google Scholar]
- 18. Shahandeh K, Basseri HR, Sharifzadeh Y. ( 2014). An application of cultural model to assess and compare malaria prevention among Afghani migrant and Baluchi resident in the endemic area, southeastern Iran. J Immigr Minor Health, 16: 102– 10. [DOI] [PubMed] [Google Scholar]
- 19. Edrissian GH. ( 2006). Malaria in Iran: Past and Present Situation. Iran J Parasitol, 1: 1– 14 [Google Scholar]
- 20.Khuzestan, meteograms ( 2014) available in: http://www.meteoprog.nl/en/meteograms/Khuzestan/ [Google Scholar]
- 21. Kassebaum NJ, Bertozzi-Villa A, Coggeshall MS, et al. ( 2014). Global, regional, and national levels and causes of maternal mortality during 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 13: 384 (9947): 980– 1004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Kidson C, Indaratna K. ( 1998). Ecology, economics and political will: the vicissitudes of malaria strategies in Asia. Parassitologia, 40: 39– 46. [PubMed] [Google Scholar]
- 23. Bradley DJ. ( 1999). The last and the next hundred years of malariology. Parassitologia, 41: 11– 8. [PubMed] [Google Scholar]
- 24. Ostovar A, Raeisi A, Haghdoost AA, Ranjbar M, Rahimi A, Sheikhzadeh K, Majdzadeh R. ( 2012). Lessons learnt from malaria epidemics in the Islamic Republic of Iran. East Mediterr Health J, 18: 864– 9. [DOI] [PubMed] [Google Scholar]
- 25. Kazmi JH, Pandit K. ( 2001). Disease and dislocation: the impact of refugee movements on the geography of malaria in NWFP, Pakistan. Soc Sci Med, 52: 1043– 55. [DOI] [PubMed] [Google Scholar]
- 26. Montalvo GM, Reynal-Querol M. ( 2006). Discrete polarization with an application to the determinants of genocides. Journal of Asian Economics, 17 448– 477. [Google Scholar]
- 27. Killeen GF, Fillinger U, Knols BG. ( 2002). Advantages of larval control for African malaria vectors: low mobility and behavioural responsiveness of immature mosquito stages allow high effective coverage. Malar J, 1: 8. [DOI] [PMC free article] [PubMed] [Google Scholar]


