Abstract
Background:
around the world health systems constantly face increasing pressures which arise from many factors, such as an ageing population, patients and providers demands for equipment’s and services. In order to respond these challenges and reduction of health system’s transactional costs, referral solutions are considered as a key factor. This study was carried out to identify referral solutions that have had successes.
Methods:
relevant studies identified using keywords of referrals, consultation, referral system, referral model, referral project, electronic referral, electronic booking, health system, healthcare, health service and medical care. These searches were conducted using PubMed, ProQuest, Google Scholar, Scopus, Emerald, Web of Knowledge, Springer, Science direct, Mosby’s index, SID, Medlib and Iran Doc data bases. 4306 initial articles were obtained and refined step by step. Finally, 27 articles met the inclusion criteria.
Results:
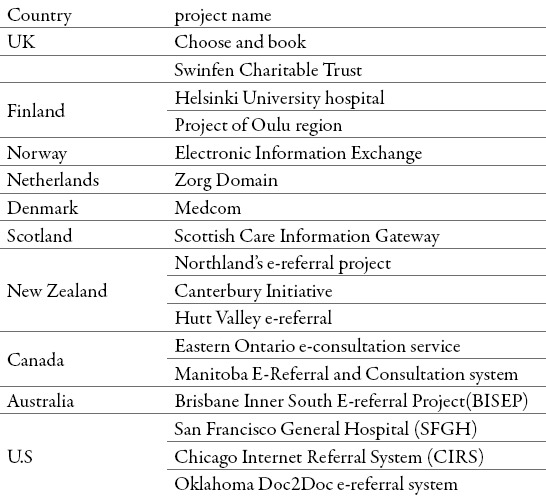
we identified seventeen e-referral systems developed in UK, Norway, Finland, Netherlands, Denmark, Scotland, New Zealand, Canada, Australia, and U.S. Implemented solutions had variant degrees of successes such as improved access to specialist care, reduced wait times, timeliness and quality of referral communication, accurate health information transfer and integration of health centers and services.
Conclusion:
each one of referral solutions has both positive and changeable aspects that should be addressed according to sociotechnical conditions. These solutions are mainly formed in a small and localized manner.
Keywords: referral, consultation, e-referral system, e-booking, health communication, health system
1. INTRODUCTION
Referrals are the link and interface between health care providers in a primary and specialty care settings (1). Referral process is defined as transferring (including sharing) of responsibility of patient care from referring provider to another physician or provider, so that it also includes the transfer back of patient care in an appropriate time (2-4). there is a deep – rooted impression in many countries that higher levels of health services provide the best care. It is essential to make link between health service levels in order to assurance people that they will access specialized services if it is truly needed (5).
Estimations show one third of all patients in US are referred to specialist services annually. It has also reported that 9 million elective referrals from primary to secondary care at a cost of more than £15 billion for the National Health Service(NHS) in England (1, 6).
Referral processes are prone to breakdowns that can result in lack of continuity of care, delays in service delivery and dissatisfaction among practitioners and patients.(3)According to studies%25 to 50% of referrals, have no adequate information for specialists and reason for referrals (7).
Currently, there is a fragmentation in the health system of IRAN. Health services are provided episodic, Conditions are investigated separately. Referral chaos has affected work conditions between primary and secondary health care settings. High proportion of patients is admitted in teaching hospitals without any referrals, resulting in overcrowding in such hospitals. Lack of integration in health system has made difficulties to provide a smooth flow of patient information in a timely and structured manner. Because the close cooperation and communication between general practice and specialty centers is a prerequisite of satisfactory medical care, but this cooperation does not exist in the Iranian health system. There is no appropriate bridging function of referral system and two- way communication among health care’s providers. As a result of the existing referral system, bypassing the primary health care level has become routine, resulting in under utilization and over utilization in lower and upper levels of health care delivery, respectively (8-11).
It appears that achieving cost-effectiveness in health service delivery comes from particular organizational structures. Health systems that have different organizational structures, have different level of costs for the same package of services (12).
Paper based referral processes are known with features such as inadequate information, lost or misplaced paper records, medication errors resulting from illegible handwritings. Addition to limited standardization, lack of the capacity of referral tracking, outcomes and communication in an iterative fashion or feedbacks between referring provider and specialists are other characteristics of paper based referral systems (13, 14).
To resolve these problems, like other sectors, there has been growing interest in using Information and Communication Technologies (ICT) in health systems. ICT has opened new possibilities to health care that is why the ICTs are seen as possible solutions in health care. Therefore, to resolve mentioned problems and meet existing referral related challenges, e-referral has been seen as one of the best solutions to replace paper based referrals (15, 16).
E-referral is an electronically transmitted message such as documents or PDF which can received and viewed by the reviewer (15, 17). Currently e-referrals can be seen as a new model for integration of primary and secondary health care (18). Several countries such as England, Finland, Norway, Netherlands, Denmark, New Zealand, Australia and the US have adopted e-referral systems with a varying levels of success (6, 15, 19).
This study was designed to identify the relatively successful referrals and examine their usability and possibility in creation and modification of developing countries such as Iran.
2. MATERIALS AND METHODS
Databases were searched using keywords that were agreed by the review team. Our search took place between February 2014 to August 2014. Relevant studies were identified using keywords of referrals, consultation, referral system, referral model, referral project, electronic referral, electronic booking, health system, healthcare, health service and medical care.
These searches were conducted using PubMed, ProQuest, Google Scholar, Scopus, Emerald, ISI, Springer, Science direct, Mosby’s index, SID, Medlib and Iran Doc databases. Grey literature was searched in form of reports, books and websites. 4306 initial articles were obtained and refined step by step. Finally, 27 reviewed articles met the inclusion criteria.
We included studies written in English and Persian language that had reported development and implement of referral systems. We also conducted hand searching of reference lists of included studies. Studies that contained introducing, establishing or developing referral solutions were included. Studies that had also covered particular medical specialties and focused on issues outside of introducing, designing or developing of referral systems, were excluded. We also excluded studies which dealt with referral systems in pilot phase. After selecting titles for inclusion, the researchers met to determine which articles were to have abstract review. Following abstract review, a further meeting was held to determine inclusion for full article review. Articles selected for full review were read by researchers and data extracted independently using extraction form.
3. RESULTS
The search for studies resulted in 4306 references, of which 26 articles met the inclusion criteria. (Figure 1) we identified 17 referral solutions in 10 countries. Majority of introduced referral systems have implemented in European countries and United State. Identified referral solutions have been presented in Table 1.
Figure 1.
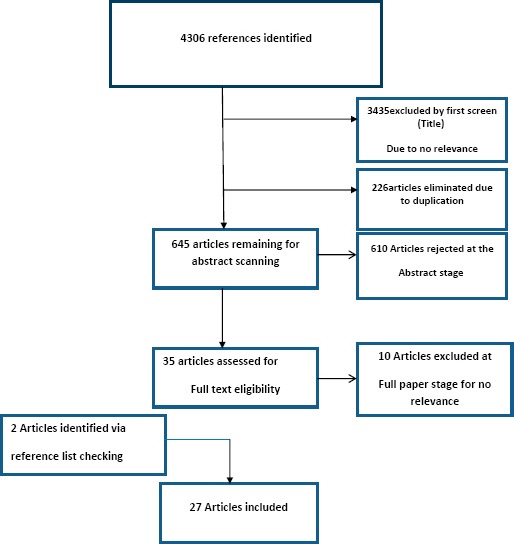
Flowchart of search
Table 1.
Identified e-referral systems
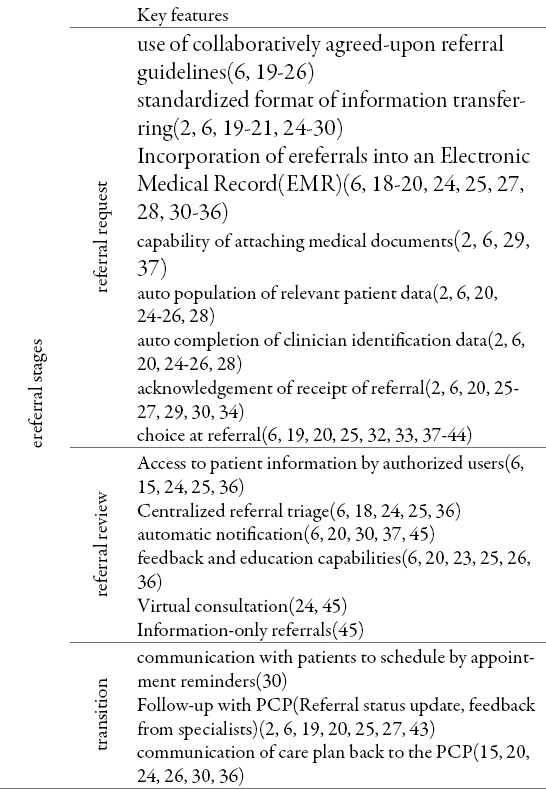
In the next step, key attributes of identified referral systems were extracted based on three main stages of referral process. We collected key features in three separately stages; submission of referral request, referral review and patient transition. These findings are shown in Table 2.
Table 2.
E-referral stages and features
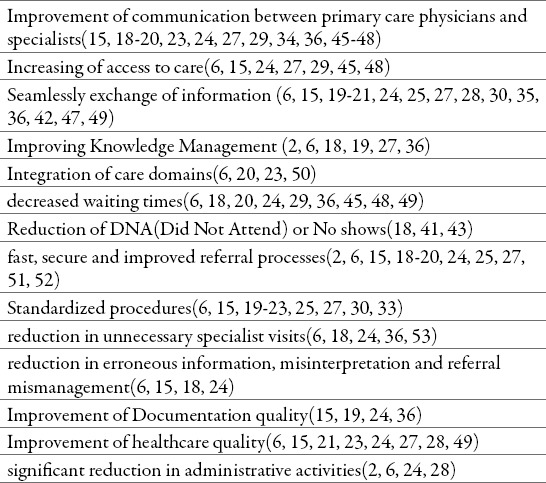
In the next stage, we collected cases of successes that identified referral systems have resulted in those. All of developed systems have the potential capability and benefits that have been listed n in Table 3.
Table 3.
benefits derived from adoption and implementation of e-referral systems
4. DISCUSSION
In this study, we divided all extracted features of e-referrals into three main stages of referral system; referral request, referral review and patient transition. Developed e-referral systems are similar to each other in structure and stages of referrals.
Choose and book as a national electronic referral system in England combines the electronic referrals with the choice of place, date and time of outpatient appointment. This system act as an expanding of patient’s choice such as choice of where, when and how to get medical services had been a key part of Labor government’s strategy for the NHS (1, 6, 19, 27, 31, 32, 38-41) this system is used as a tool to provide commissioning decisions in the ways such as service planning and design, contract Management, commissioning of care pathways, referral management, enhancing quality, Education of referrers (54).
Despite the improvement of patients attendance to appointments and giving opportunities to patients in choosing time and date of appointments in choose and book system (38), Greenhalgh concluded that top down, abstracted and nationally mandated approaches are not the best way in reducing resistance to IT related projects (32). According to Eason unwillingness of patients to choose, more time consuming, anxiety of GPs about security of patient’s information (19), technical problems (39), increased workload and uneven distribution of patients among hospitals can be considered as number of reasons for the limited use of Choose and Book programme (43).
Although reports indicate more patients’ treatment at lower costs, improved cooperation between hospitals and health centers, increased productivity of about threefold in Helsinki referral system, Wootton concluded that careful planning and appropriate implementation is essential for the success of the referral systems (27).
Norwegian electronic booking and referral system as a political instrument for change of health care sector was designed to full utilization of national treatment capacity and dissolve geographical and administrative issues. It seems that inadequate attention was paid on sociotechnical issues in rollout process of the project (19, 42).
ZD in Netherlands addressed the problems of lake of standardized agreements concerning referral process, poor GPs-specialists communications and inappropriate referrals by organizing referrals into defined patient groups (23). Following the re- organization of referral process, the use of standards and guidelines has increased. It is also furthering the integration of primary and secondary domains (20).
Electronic referral in Denmark is a part of Medcom project. Denmark ranks among leading countries in establishment of electronic communication (15). The success of Denmark is based on political support, cross–sector agreements in a country, consensus on national standards, reciprocal professional agreements involving physicians, IT suppliers, counties and the federal government (34, 35).
The success of e-referral project in the New Zealand as an example in Hutt Valley District, arises from key factors such as obligation of superior management, leadership and change management, agreement of participants on information requirements, involvement of multidisciplinary groups in implementation of project, testing and evaluation of the system at every step of its developing (15, 49).
In addition to solving the problems of ineffective information exchange between providers and patient safety issues, developing and implementation of e-consultation service improved access to care, Transmission of high-quality advice securely and PCP- specialists’ communication in Champlain Local Health Integration Network (LHIN), which is one of 14 regional health districts in Ontario, Canada (29, 45, 48).
The success of BISEP is attributed to key factors such as change management approach, excellent cooperation and teambuilding between all vendors, unifying focus to provide timely manner and high quality services to patients (37).
Kim-hwang and colleagues found that referrals made via e-referrals in SFGH resulted in decrease in inappropriate referrals in surgical clinics. Specialists had offered better previsit guidance with e-referrals according to PCPs reports. SFGH e-referral system allows a specialist reviewer to triage and clarify the consultative question. In other words this system can be used to identify knowledge gaps and provide case-based education (18, 36, 55).
Implementation of e-referral in the Chicago area has led to reduction in referral processing time, increasing access to care, improving care quality, and increasing operational efficiency. However, budget cuts within Cook County Health and Hospitals System remains as a main challenge (24).
Limitations of study: There are some challenges and limitations to this study, projects that are not considered as research projects. E-referral projects have limited documentation in English and most of them are available in Northern-European languages.
5. CONCLUSION
This study has identified and introduced relatively successful referral solutions in various countries. The results of this review mainly indicate that e-referral systems have shaped in small and localized manner. Implementation of e-referrals requires political supports and further attention to sociotechnical conditions.
Acknowledgments
This study is a part of PHD thesis that has approved and recorded in a research deputy of Tabriz University of medical sciences in Iran.
Footnotes
CONFLICT OF INTEREST: NONE DECLARED.
REFERENCES
- 1.Mehrotra A, Forrest CB, Lin CY. Dropping the baton: specialty referrals in the United States. Milbank Quarterly. 2011;89(1):39–68. doi: 10.1111/j.1468-0009.2011.00619.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Warren J, White S, Day KJ, Gu Y, Pollock M. Introduction of electronic referral from community associated with more timely review by secondary services. Applied Clinical Informatics. 2011;2(4):546–564. doi: 10.4338/ACI-2011-06-RA-0039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Esquivel A. Characterizing, Assessing and Improving Healthcare Referral Communication. 2008 [Google Scholar]
- 4.Akande T. Referral system in Nigeria: study of a tertiary health facility. 2004 [Google Scholar]
- 5.Organization WH. Hospitals and health for all: report of a WHO Expert Committee on the Role of Hospitals at the First Referral Level [meeting held in Geneva from 9 to 17 December 1985] 1987 [PubMed] [Google Scholar]
- 6.Bouamrane MM, Mair FS. A qualitative evaluation of general practitioners’ views on protocol-driven eReferral in Scotland. BMC medical informatics and decision making. 2014;14(1):30. doi: 10.1186/1472-6947-14-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Patrick GMDMPP, Bisgaier JMSW, Hasham IBS, Navarra TMA, Hickner JMDM. Specialty Care Referral Patterns for the Underserved: A Study of Community Health Centers on the South Side of Chicago. Journal of Health Care for the Poor and Underserved. 2011. 2011 Nov;22(4):1302–1314. doi: 10.1353/hpu.2011.0147. [DOI] [PubMed] [Google Scholar]
- 8.Golalizadeh E, Moosazadeh M, Amiresmaili M, Ahangar N. challenges of second referral level in family physician plan: qualitative study. Journal of Medical Council of Islamic Republic of Iran. 2011;29(4):309–321. in Persian. [Google Scholar]
- 9.Shirvani N, Ashrafian A, Motlagh M. Evaluation of the function of referral system in family physician program in Northern provinces of Iran: 2008. J Babol Univ Med Sci. 2010;11(6):46–52. in Persian. [Google Scholar]
- 10.Rasoulynejad A, Khagani P. Study of rate of self referral and it’s related factors in public and private facilities of Kashan in 2000. Feyz Journal of Kashan University of Medical Sciences. 6(2) in Persian. [Google Scholar]
- 11.Janati A, Jabaribairami H, Golizade M, Gholamzade R, Ghodoosinejad J, Naseriasl M. Regionalization in health care. 2012:176. [Google Scholar]
- 12.Mwabu GM. Referral systems and health care seeking behavior of patients: an economic analysis. World Development. 1989;17(1):85–91. [Google Scholar]
- 13.Thiong’o FK, editor. Framework for the Implementation of a Patient Electronic Referral System: Case Study of Nairobi Province. Scientific Conference Proceedings. 2013 [Google Scholar]
- 14.de Vries J, Pierik E, Nijland E, Bosveld H, MelM Sturkenboom J. Effects of electronic communication on the communication between surgeon and general practitioner for patients suspected of breast cancer: A randomised clinical trial. Effects of Electronic Communication in General Practice. :59. [Google Scholar]
- 15.Tian L. Improving knowledge management between primary and secondary healthcare: an e-referral project. Health Care Inform Rev Online. 2011;15:31–37. [Google Scholar]
- 16.Sadr SMH. A Review of the Impact of E-health on Economic Growth in developed countries and developing countries. Developing Country Studies. 2012;2(7):19–28. [Google Scholar]
- 17.Coleman A. Developing an e-health framework through electronic healthcare readiness assessment: Nelson Mandela Metropolitan University. 2010 [Google Scholar]
- 18.Chen AHMDMPH, Murphy EJMDD, Yee HFJMDP. eReferral - A New Model for Integrated Care. The New England Journal of Medicine. 2013 Jun 27;368(26):2450–2453. doi: 10.1056/NEJMp1215594. [DOI] [PubMed] [Google Scholar]
- 19.Heimly V. Electronic referrals in healthcare: a review. Stud Health Technol Inform. 2009;150:327–331. [PubMed] [Google Scholar]
- 20.Bal R, Mastboom F, Spiers HP, Rutten H. The product and process of referral: optimizing general practitioner-medical specialist interaction through information technology. International journal of medical informatics. 2007;76:S28–S34. doi: 10.1016/j.ijmedinf.2006.05.033. [DOI] [PubMed] [Google Scholar]
- 21.Gu Y, Warren J, Day K, Pollock M, White S, editors. Achieving acceptable structured eReferral forms. Proceedings of the Fifth Australasian Workshop on Health Informatics and Knowledge Management. 2012;129 [Google Scholar]
- 22.Timmins N, Ham C. The quest for integrated health and social care: A case study in Canterbury, New Zealand. The Kings Fund. 2013 [Google Scholar]
- 23.Carrick C. Ann Arbor: University of Manitoba (Canada); 2012. Developing an Optimization Algorithm within an E-Referral Program for Clinical Specialist Selection, Based on an Extensive E-Referral Program Analysis [M.Sc.] [Google Scholar]
- 24.Fischer BS, Martinez E, Driscoll M, Conway T. Chicago: Using Evidence-Based Rules To Make Smarter Referrals Chevy Chase: The People to People Health Foundation, Inc. Project HOPE. 2010. [updated May 2010; cited 29 5]. pp. 972–5. Available from: http://content.healthaffairs.org/content/29/5/972.full.html . [DOI] [PubMed]
- 25.Bouamrane M-M, Mair F. An overview of electronic health systems development & integration in Scotland. Proceedings of the first international workshop on Managing interoperability and complexity in health systems. 2011 [Google Scholar]
- 26.SCI Gateway Product Description. Available from: http://www.sci.scot.nhs.uk/products/gateway/gate_desc.htm .
- 27.Wootton R, Harno K, Reponen J. Organizational aspects of e-referrals. Journal of telemedicine and telecare. 2003;9(suppl 2):76–79. doi: 10.1258/135763303322596354. [DOI] [PubMed] [Google Scholar]
- 28.Warren J, Gu Y, Day K, White S, Pollock M, editors. Electronic referrals: What matters to the users. Studies in Health Technology and Informatics. 2012 [PubMed] [Google Scholar]
- 29.Liddy C, Rowan MS, Afkham A, Maranger J, Keely E. Building access to specialist care through e-consultation. Open Medicine. 2013;7(1):e1. [PMC free article] [PubMed] [Google Scholar]
- 30.Heimly V, editor. Electronic referrals in the health sector in Norway, challenges on the road from standard to high volume use. CTS. 2010 [Google Scholar]
- 31.Boyle S. Health systems in transition: United Kingdom (England) Copenhagen, WHO Regional Office for Europe on behalf of the European Observatory on Health Systems and Policies. 2011 [Google Scholar]
- 32.Greenhalgh T, Stones R, Swinglehurst D. Choose and Book: A sociological analysis of ‘resistance’ to an expert system. Social Science & Medicine. 2014;104(3):210–219. doi: 10.1016/j.socscimed.2013.12.014. [DOI] [PubMed] [Google Scholar]
- 33.Ellingsen G, Obstfelder A. Collective expectations - Individual action implementing electronic booking systems in Norwegian health care. International Journal of Medical Informatics. 2007;76(6 Suppl 1):S104–S12. doi: 10.1016/j.ijmedinf.2006.05.029. [DOI] [PubMed] [Google Scholar]
- 34.Protti D, Johansen I. Further lessons from Denmark about computer systems in physician offices. Electronic Healthcare. 2003;2(2):36–43. [Google Scholar]
- 35.Cannaby S, Westcott D, Pedersen CD, Voss H, Wanscher CE. The cost benefit of electronic patient referrals in Denmark: summary report. Hospitals. 2004;63:100. [PubMed] [Google Scholar]
- 36.Kim YMDMAS, Chen AHMDMPH, Keith EBA, Yee HFJMDP, Kushel MBMD. Not Perfect, but Better: Primary Care Providers’ Experiences with Electronic Referrals in a Safety Net Health System. Journal of General Internal Medicine. 2009. 2009 May;24(5):614–619. doi: 10.1007/s11606-009-0955-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Nicholson C, Jackson CL, Wright B, Mainwaring P, et al. Online referral and OPD booking from the GP desktop. Australian Health Review. 2006. 2006 Aug;30(3):397–404. doi: 10.1071/ah060397. [DOI] [PubMed] [Google Scholar]
- 38.Green J, McDowall Z, Potts H. Does Choose & Book fail to deliver the expected choice to patients? A survey of patients’ experience of outpatient appointment booking. BMC Medical Informatics and Decision Making. 2008;8(1):1–8. doi: 10.1186/1472-6947-8-36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Robertson R, Dixon A. Choice at the point of referral. Report, The King’s Fund, London. 2009 [Google Scholar]
- 40.Pisipati S, Chow K, Payne SR. Choose and Book: An Audit of the Appropriateness of Referrals and Their Effect on Patients’ Attendance to An Inner City Hospital Secondary Care Provider. British Journal of Medical and Surgical Urology. 2009;2(3):111–116. [Google Scholar]
- 41.Dennison J, Eisen S, Towers M, Clark CI. An effective electronic surgical referral system. Annals of the Royal College of Surgeons of England. 2006;88(6):554. doi: 10.1308/003588406X130642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Lotherington AT, Obstfelder A. Contests in virtual space: Power and resistance in electronic booking [Google Scholar]
- 43.Rashid M, Abeysundra L, Mohd-Isa A, Khan Y, Sismeiro C. Two years and 196 million pounds later: where is Choose and Book? Inform Prim Care. 2007;15(2):111–119. doi: 10.14236/jhi.v15i2.649. [DOI] [PubMed] [Google Scholar]
- 44.What is Choose and Book? Available from: http://www.chooseandbook.nhs.uk/patients/whatiscab .
- 45.Keely E, Liddy C, Afkham A. Utilization, benefits, and impact of an e-consultation service across diverse specialties and primary care providers. Telemedicine and e-Health. 2013;19(10):733–738. doi: 10.1089/tmj.2013.0007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Reponen J, Marttila E, Paajanen H, Turula A. Extending a multimedia medical record to a regional service including experiences with electronic referral and discharge letters. Proceedings of 4th International Conference on Successes and Failures in Telehealth, Brisbane. 2004 doi: 10.1258/1357633042614276. [DOI] [PubMed] [Google Scholar]
- 47.Protti D, Bowden T, Johansen I. Adoption of information technology in primary care physician offices in New Zealand and Denmark, part 4: benefits comparisons. Informatics in primary care. 2008;16(4):291–296. doi: 10.14236/jhi.v16i4.705. [DOI] [PubMed] [Google Scholar]
- 48.Liddy C, Maranger J, Afkham A, Keely E. Ten Steps to Establishing an e-Consultation Service to Improve Access to Specialist Care. TELEMEDICINE and e-HEALTH. 2013;19(12):982–990. doi: 10.1089/tmj.2013.0056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Warren J, Gu Y, Day K, Pollock M, White S. Approach to Health Innovation Projects: Learnings from eReferrals. Heal Care Informatics Rev Online. 2012;16(2):17–23. [Google Scholar]
- 50.SCI Gateway Product Overview. Available from: http://www.sci.scot.nhs.uk/products/gateway/gate_desc.htm .
- 51.Will Choose and Book make getting an appointment faster? Available from: http://www.chooseandbook.nhs.uk/patients/wait .
- 52.How secure is Choose and Book? Available from: http://www.chooseandbook.nhs.uk/patients/patient .
- 53.Horner K, Wagner E, Tufano J. Electronic consultations between primary and specialty care clinicians: early insights. Issue Brief (Commonw Fund) 2011;23:1–14. [PubMed] [Google Scholar]
- 54.Choose and Book - A tool to support Clinical Commissioning 2011 [cited 2015] Available from: http://www.chooseandbook.nhs.uk/staff/communications/fact .
- 55.Kim-hwang JE, Chen AH, Bell DS, Guzman D, Yee HF, Kushel MB. Evaluating Electronic Referrals for Specialty Care at a Public Hospital. Journal of General Internal Medicine. 2010. 2010 Oct;25(10):1123–1128. doi: 10.1007/s11606-010-1402-1. [DOI] [PMC free article] [PubMed] [Google Scholar]


