Abstract
AIM: To investigate the effects of Japanese apricot (JA) consumption on gastroesophageal reflux disease (GERD)-related symptoms.
METHODS: Participants included individuals living in Minabe-cho, a well-known JA-growing region, who received specific medical check-ups by the local community health service in 2010. GERD-related symptoms were examined in 1303 Japanese individuals using a validated questionnaire, the Frequency Scale for Symptoms of GERD (FSSG), which consists of 7 questions associated with acid reflux symptoms and 5 questions asking about gastrointestinal dysmotility symptoms. Each question was answered using a 4-point scale, with higher scores indicating more severe GERD-related symptoms. Subjects were divided into two groups according to their intake of dried and pickled JA: daily intake (≥ 1 JA daily) (392 subjects) and none or occasional intake (< 1 JA daily) (911 subjects). FSSG scores were compared between subjects who consumed JA daily and those who did not. Next, subjects were stratified by age, gender and Helicobacter pylori (H. pylori) status for subanalyses.
RESULTS: Those who ate JA daily were significantly older than those who did not (60.6 ± 10.5 years vs 56.0 ± 11.0 years, P < 0.001). Total FSSG scores were significantly lower in subjects with daily JA intake than in those with none or only occasional intake (2.13 ± 3.14 vs 2.70 ± 3.82, P = 0.005). In particular, subjects who consumed JA daily showed significantly improved FSSG dysmotility scores compared with subjects who did not (1.05 ± 1.58 vs 1.46 ± 2.11, P < 0.001). In contrast, the FSSG reflux score did not differ between subjects with and without daily intake of JA (1.08 ± 1.90 vs 1.24 ± 2.11, P = 0.177). Subanalysis indicated that improvement in dysmotility by JA intake was specifically observed in non-elderly (1.24 ± 1.68 vs 1.62 ± 2.22, P = 0.005) and H. pylori-negative subjects (0.99 ± 1.58 vs 1.57 ± 2.06, P < 0.001). GERD patients (total FSSG score ≥ 8) were less frequently observed among subjects with daily intake of JA as compared to those without daily intake of JA (6.1% vs 9.7%, P = 0.040).
CONCLUSION: Daily JA intake may improve digestive dysmotility symptoms, resulting in relief of GERD symptoms. The effect is more obvious in non-elderly and H. pylori-negative subjects.
Keywords: Japanese apricot, Umeboshi, Gastroesophageal reflux disease, Frequency Scale for Symptoms of gastroesophageal reflux disease, Dysmotility
Core tip: Japanese apricot (JA), which is eaten as a daily food in Japan, is considered to have medicinal benefits. We focused on the effect of JA on gastroesophageal reflux disease (GERD)-related symptoms in this study. First, GERD-related symptoms were examined in 1303 Japanese individuals using the validated questionnaire, the Frequency Scale for Symptoms of GERD (FSSG). JA was consumed daily by 392 subjects. Then, FSSG scores were compared between subjects who took one or more JA daily and those who did not. This study indicates that daily intake of JA improves digestive dysmotility symptoms, resulting in relief of GERD-related symptoms.
INTRODUCTION
The Japanese apricot (JA) (“ume” in Japanese; Prunus mume, Siebold et Zucc.) enjoys great popularity in Japan. Since ancient times, the JA has been processed into a dried and pickled form (“umeboshi”), and made into liquor and soft drinks. These products have been known to possess various medicinal benefits and have been frequently prescribed as a traditional folk remedy. JA has been reported to possess such beneficial biological activities as improving blood fluidity[1], anti-fatigue effect[2], protection from the human influenza A virus[3], and anti-cancer effect[4]. The biological basis of the efficacy of JA is partly attributable to anti-oxidative and free radical scavenging activities[5], and partly to immune enhancement[6,7].
In Eastern countries, although JA is widely believed to improve various gastrointestinal disorders, including gastrointestinal motility, dyspepsia and gastrointestinal infections, the effect of JA on the gastrointestinal system has scarcely been evaluated in a scientific manner. We previously reported that JA intake exerted a preventive effect on chronic atrophic gastritis by inhibiting Helicobacter pylori (H. pylori) infection and reducing mucosal inflammation[8]. Meanwhile, animal models have suggested that JA or the alimentary fiber provided by it enhances gastrointestinal motility. JA showed laxative effects in the low-fiber diet-induced constipation rat model[9], and the increased alimentary fiber resulting from JA ingestion produced fecal lipid excretion effects and feces bulking effects in adult mice by inducing changes in the composition of intestinal flora[10].
Gastroesophageal reflux disease (GERD) is a common disease in Western countries. Recently, the number of GERD patients has also been increasing in Japan, owing to the Westernization of diets and the decrease in prevalence of H. pylori infection. The main symptoms of GERD can be attributed to reflux of gastric acid and gastrointestinal dysmotility. Subjects with GERD often get heartburn, an unusual sensation in the throat, and bitter liquid coming up into the throat due to reflux of gastric acid, with or without esophageal mucosal injury. Furthermore, they often feel full, sick or heavy during and after meals, and often burp due to gastrointestinal dysmotility[11]. The traditional Japanese folk remedy of ingestion of JA is probably based on its effects on gastric acid secretion and gastrointestinal motility, resulting in improvement of GERD symptoms.
In this study, therefore, we investigated and compared GERD symptoms between Japanese inhabitants who took and did not take JA daily, using a questionnaire that can quantify the severity of GERD symptoms and differentiate between acid-related symptoms and dysmotility-related symptoms.
MATERIALS AND METHODS
Subjects and study design
Participants in this study included adult individuals living in Minabe-cho, Wakayama Prefecture, a well-known JA-growing region, who received specific medical check-ups provided by the local community health service. In Minabe-cho, specific medical check-ups are performed every year for all inhabitants aged 35 years or older. To remind people about the medical check-up program, a guidance postcard is sent from the local community health service to each subject once a year. In Japan, these types of health check-up programs are performed to detect diseases, including cancer, at an early stage. Therefore, subjects who had specific serious symptoms requiring medical care were excluded from the program.
The participation rate in the check-up program in Minabe-cho town in 2010 was about 36%, and a total of 1902 subjects underwent the check-ups. The participants received the following tests and procedures: physical examination, chest X-ray, electrocardiogram, blood laboratory tests, including H. pylori IgG antibody titer, urinalysis, upper gastrointestinal barium X-ray examination, and a fecal occult blood test. H. pylori IgG antibody titers were measured by ELISA (SRL Inc., Tokyo, Japan). Subjects with H. pylori antibody titers ≥ 10 U/mL were considered positive for H. pylori infection and those with titers < 10 U/mL were considered negative.
The subjects also completed a self administered questionnaire and an interview to determine general health status. The questionnaire included an assessment of the daily intake of dried and pickled JA or processed JA, the frequency scale for symptoms of GERD (FSSG)[11], history of therapy for eradication of H. pylori, regular medication, and past history of diseases affecting the gastrointestinal system. Subjects were divided into two groups according to the intake of dried and pickled JA: daily intake (≥ 1 JA daily) and none or occasional intake (< 1 JA daily).
Subjects who had a previous history of surgical resection of gastrointestinal cancer (16 subjects), or H. pylori eradication (167 subjects), and those who had been prescribed a proton pump inhibitor (PPI) or other digestive medicines (167 subjects) that might affect gastrointestinal function were excluded from the study. Those who did not reply to the FSSG questionnaire (12 subjects) were also excluded. In addition, subjects who regularly took processed JA, for example, JA extract, powdered JA or JA juice, other than dried and pickled JA, were excluded (321 subjects) to avoid confounding by additional intake of JA ingredients. Thus, a total of 1303 subjects (589 males and 714 females) were analyzed in this study. The ethics committee of Wakayama Medical University approved the study protocol. Written, informed consent was obtained from all participants.
Assessment of the FSSG questionnaire and the definition of GERD
The FSSG questionnaire for GERD-related symptoms, which was developed by Kusano et al[11] in Japan (Figure 1), was evaluated. The questionnaire consists of 12 questions regarding GERD-related symptoms. Of the 12 FSSG questions, 7 questions (Q1, Q4, Q6, Q7, Q9, Q10, and Q12) are related to acid reflux symptoms, while the remaining 5 questions (Q2, Q3, Q5, Q8, and Q11) pertain to gastrointestinal dysmotility symptoms. Patients assigned each question 0 (never), 1 (occasionally), 2 (sometimes), 3 (often), or 4 (always) points. Acid reflux-related, gastrointestinal dysmotility-related, and total scores were calculated by adding the points for the 7, 5 and 12 questions, respectively. GERD was defined as a total score ≥ 8, which is the recommended cut-off FSSG score for GERD[11,12].
Figure 1.
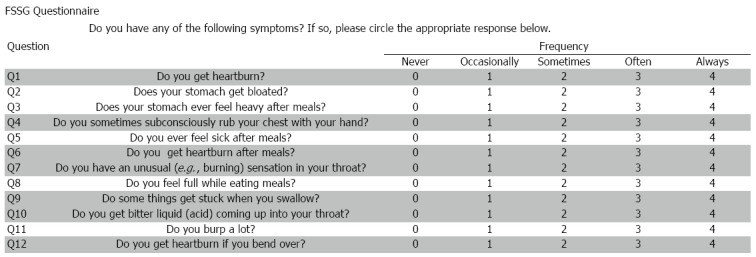
Frequency Scale for Symptoms of gastroesophageal reflux disease questionnaire. Of the 12 FSSG questions, 7 questions (Q1, Q4, Q6, Q7, Q9, Q10, and Q12; shaded lines) deal with acid reflux symptoms, and the other 5 questions (Q2, Q3, Q5, Q8, and Q11, white lines) ask about dysmotility symptoms. FSSG: Frequency Scale for Symptoms of gastroesophageal reflux disease.
Statistical analysis
The data are expressed as mean ± SD. Data were analyzed using the unpaired t-test and Fisher’s exact text. The level of statistical significance was P < 0.05. All analyses were performed using the SPSS 21.0 software package (SPSS Inc., Chicago, IL, United States).
RESULTS
Upper gastrointestinal symptoms according to intake of JA
A total of 1303 subjects (589 men and 714 women, mean age 57.4 (34-79) years old) received the medical check-up and answered the questionnaire. These subjects were analyzed according to intake of JA: daily intake versus none to occasional intake. Of the 1303 subjects, 392 (30%) were categorized into the daily intake group, while 911 (70%) were included in the none or occasional group. The characteristics of subjects in each group are summarized in Table 1. Those who ate one or more JA daily were significantly older than those who did not (60.6 ± 10.5 years vs 56.0 ± 11.0 years, P < 0.001). In addition, the proportion of male subjects was higher in the daily intake group.
Table 1.
Characteristics and Frequency Scale for Symptoms of gastroesophageal reflux disease scores of subjects on the basis of Japanese apricot intake
| Daily intake | None or occasional | P value | |
| (≥ 1 JA daily) | (< 1 JA daily) | ||
| n | 392 | 911 | |
| Age (yr) | 60.6 ± 10.5 | 56.0 ± 11.0 | < 0.001 |
| Sex (male/female) | 201/191 | 388/523 | 0.004 |
| Helicobacter pylori infection rate | 203 (51.8%) | 451 (49.5%) | 0.469 |
| FSSG | |||
| Total score | 2.13 ± 3.14 | 2.70 ± 3.82 | 0.005 |
| Acid reflux score | 1.08 ± 1.90 | 1.24 ± 2.11 | 0.177 |
| Dysmotility score | 1.05 ± 1.58 | 1.46 ± 2.11 | < 0.001 |
| Total FSSG score ≥ 8 | 24 (6.1%) | 88 (9.7%) | 0.040 |
Data are expressed as mean ± SD. JA: Japanese apricot; FSSG: Frequency Scale for Symptoms of gastroesophageal reflux disease.
The total FSSG score was significantly lower in subjects with daily intake of JA than in those with none or occasional intake (2.13 ± 3.14 vs 2.70 ± 3.82, P = 0.005). In particular, those with daily JA intake had significantly better FSSG dysmotility scores than subjects who did not take JA daily (1.05 ± 1.58 vs 1.46 ± 2.11, P < 0.001). In contrast, the FSSG acid reflux score did not differ between subjects with and without daily intake of JA (1.08 ± 1.90 vs 1.24 ± 2.11, P =0.177). GERD patients (total FSSG score ≥ 8) were less frequently observed among subjects with daily intake of JA as compared to those without (6.1% vs 9.7%, P = 0.040) (Table 1).
Table 2 shows the scores for each question according to JA intake. Significant differences were observed in Q2, Q3, Q5, Q8, and Q10 between subjects with and without daily intake of JA. Four of these 5 questions relate to dysmotility symptoms.
Table 2.
Scores of each Frequency Scale for Symptoms of gastroesophageal reflux disease question on the basis of Japanese apricot intake
| Daily intake | None or occasional | P value | |
| (≥ 1 JA daily) | (< 1 JA daily) | ||
| n | 392 | 911 | |
| Q1 score | 0.30 ± 0.62 | 0.33 ± 0.66 | 0.369 |
| Q2 score | 0.31 ± 0.63 | 0.44 ± 0.75 | 0.002 |
| Q3 score | 0.18 ± 0.50 | 0.28 ± 0.62 | 0.001 |
| Q4 score | 0.10 ± 0.37 | 0.13 ± 0.44 | 0.182 |
| Q5 score | 0.08 ± 0.32 | 0.13 ± 0.41 | 0.036 |
| Q6 score | 0.19 ± 0.49 | 0.19 ± 0.49 | 0.865 |
| Q7 score | 0.10 ± 0.43 | 0.11 ± 0.42 | 0.845 |
| Q8 score | 0.11 ± 0.38 | 0.23 ± 0.61 | < 0.001 |
| Q9 score | 0.11 ± 0.41 | 0.14 ± 0.44 | 0.436 |
| Q10 score | 0.18 ± 0.43 | 0.24 ± 0.52 | 0.043 |
| Q11 score | 0.37 ± 0.70 | 0.38 ± 0.75 | 0.792 |
| Q12 score | 0.09 ± 0.36 | 0.11 ± 0.40 | 0.537 |
Data are expressed as mean ± SD. JA: Japanese apricot; FSSG: Frequency Scale for Symptoms of gastroesophageal reflux disease.
Subgroup analysis
Since there was a significant difference in intake of JA according to age and gender, subanalyses were stratified by these factors (Tables 3 and 4). In both male and female subjects, FSSG dysmotility scores were significantly lower in subjects with daily intake of JA than those without (male: 1.00 ± 1.45 vs 1.33 ± 1.99, P = 0.021, female: 0.76 ± 1.38 vs 0.95 ± 1.65, P = 0.005). In contrast, the FSSG acid reflux score did not differ between subjects with and without daily intake of JA (male: 1.01 ± 1.70 vs 1.14 ± 1.89, P = 0.434, female: 1.14 ± 2.08 vs 1.32 ± 2.27, P = 0.338).
Table 3.
Characteristics and Frequency Scale for Symptoms of gastroesophageal reflux disease scores of subjects on the basis of Japanese apricot intake stratified by sex
|
Male |
P value |
Female |
P value | |||
| Daily intake(≥ 1 JA daily) | None or occasional (< 1 JA daily) | Daily intake(≥ 1 JA daily) | None or occasional(< 1 JA daily) | |||
| n | 201 | 388 | 191 | 523 | ||
| Age (yr) | 60.0 ± 10.8 | 56.2 ± 11.6 | < 0.001 | 61.2 ± 10.1 | 55.8 ± 10.5 | < 0.001 |
| Helicobacter pylori infection rate | 103 (51.2) | 192 (49.5) | 0.728 | 100 (52.4) | 259 (49.5) | 0.554 |
| FSSG | ||||||
| Total score | 2.01 ± 2.86 | 2.47 ± 3.53 | 0.091 | 2.26 ± 3.41 | 2.88 ± 4.01 | 0.057 |
| Acid reflux score | 1.01 ± 1.70 | 1.14 ± 1.89 | 0.434 | 1.14 ± 2.08 | 1.32 ± 2.27 | 0.338 |
| Dysmotility score | 1.00 ± 1.45 | 1.33 ± 1.99 | 0.021 | 0.76 ± 1.38 | 0.95 ± 1.65 | 0.005 |
| Total FSSG score ≥ 8 | 9 (4.5) | 34 (8.8) | 0.066 | 15 (7.9) | 54 (10.3) | 0.391 |
Data are expressed as mean ± SD or n (%). JA: Japanese apricot; FSSG: Frequency Scale for Symptoms of gastroesophageal reflux disease.
Table 4.
Characteristics and Frequency Scale for Symptoms of gastroesophageal reflux disease scores of subjects on the basis of Japanese apricot intake stratified by age
|
Non-elderly (34-64 yr) |
P value |
Elderly (65-79 yr) |
P value | |||
| Daily intake | None or occasional | Daily intake | None or occasional | |||
| (≥ 1 JA daily) | (< 1 JA daily) | (≥ 1 JA daily) | (< 1 JA daily) | |||
| n | 239 | 692 | 153 | 219 | ||
| Age (yr) | 54.0 ± 7.7 | 51.5 ± 8.5 | < 0.001 | 70.9 ± 3.7 | 70.2 ± 3.7 | 0.052 |
| Sex (male/female) | 127/112 | 280/412 | 0.001 | 74/79 | 108/111 | 0.916 |
| Helicobacter pylori infection rate | 129 (54.0) | 331 (47.8) | 0.151 | 74 (48.4) | 120 (54.8) | 0.246 |
| FSSG | ||||||
| Total score | 2.50 ± 3.27 | 2.93 ± 3.96 | 0.095 | 1.56 ± 2.82 | 1.98 ± 3.21 | 0.191 |
| Acid reflux score | 1.26 ± 1.99 | 1.31 ± 2.17 | 0.748 | 0.79 ± 1.70 | 1.03 ± 1.91 | 0.211 |
| Dysmotility score | 1.24 ± 1.68 | 1.62 ± 2.22 | 0.005 | 0.76 ± 1.38 | 0.95 ± 1.65 | 0.268 |
| Total FSSG score ≥ 8 | 18 (7.5) | 77 (11.1) | 0.136 | 6 (3.9) | 11 (5.0) | 0.802 |
Data are expressed as mean ± SD or n (%). JA: Japanese apricot; FSSG: Frequency Scale for Symptoms of gastroesophageal reflux disease.
FSSG dysmotility scores in the non-elderly (34-64 years) subgroup of subjects with daily intake of JA were significantly lower than those of subjects without daily intake of JA (1.24 ± 1.68 vs 1.62 ± 2.22, P = 0.005), while in the elderly subgroup (65-79 years), the differences were not significant (0.76 ± 1.38 vs 0.95 ± 1.65, P = 0.268). The FSSG acid reflux scores, on the other hand, did not differ between subjects with and without daily intake of JA regardless of age. These results suggest that JA intake improves upper gastrointestinal dysmotility in both men and women, specifically in non-elderly subjects.
Since H. pylori infection may affect digestive symptoms, subanalysis stratified by H. pylori infection status was also performed (Table 5). Significantly lower total FSSG scores and FSSG dysmotility scores were seen in subjects with daily intake of JA who were negative for H. pylori infection (total FSSG score: 2.03 ± 2.99 vs 2.80 ± 3.69, P = 0.006, FSSG dysmotility score: 0.99 ± 1.58 vs 1.57 ± 2.06, P < 0.001). In contrast, in H. pylori-positive subjects, there was no significant difference in either total FSSG or dysmotility scores between subjects with and without daily intake of JA.
Table 5.
Characteristics and Frequency Scale for Symptoms of gastroesophageal reflux disease scores of subjects on the basis of Japanese apricot intake stratified by Helicobacter pylori infection status
|
Helicobacter pylori infection |
||||||
|
Negative |
Positive |
|||||
| Daily intake(≥ 1 JA daily) | None or occasional(< 1 JA daily) | P value | Daily intake(≥ 1 JA daily) | None or occasional(< 1 JA daily) | P value | |
| n | 189 | 460 | 203 | 451 | ||
| Age (yr) | 60.1 ± 11.5 | 54.0 ± 11.6 | < 0.001 | 61.0 ± 9.3 | 58.1 ± 10.0 | < 0.001 |
| Sex (male/female) | 98/91 | 196/264 | 0.037 | 103/100 | 192/259 | 0.062 |
| FSSG | ||||||
| Total score | 2.03 ± 2.99 | 2.80 ± 3.69 | 0.006 | 2.22 ± 3.27 | 2.60 ± 3.94 | 0.202 |
| Acid score | 1.04 ± 1.80 | 1.23 ± 2.07 | 0.251 | 1.11 ± 1.99 | 1.25 ± 2.16 | 0.435 |
| Dysmotility score | 0.99 ± 1.58 | 1.57 ± 2.06 | < 0.001 | 1.11 ± 1.58 | 1.35 ± 2.16 | 0.116 |
| Total FSSG score ≥ 8 | 11 (5.8) | 42 (9.1) | 0.206 | 13 (6.4) | 46 (10.2) | 0.140 |
Data are expressed as mean ± SD or n (%). JA: Japanese apricot; FSSG: Frequency Scale for Symptoms of gastroesophageal reflux disease.
DISCUSSION
In this study, using a questionnaire, we examined GERD-related symptoms with respect to the intake of JA in a Japanese community cohort. Subjects who took JA daily were less likely to experience GERD-related symptoms than those who did not take JA daily. In addition, there were fewer GERD patients among subjects who took JA daily than those who did not. Moreover, the lower incidence of GERD-related symptoms in subjects with daily intake of JA was mainly attributable to reduced dysmotility of the upper gastrointestinal system. These results suggest that JA facilitates gastric motility and that daily intake of JA can relieve GERD-related symptoms, resulting in improvement in the patients’ quality of life.
The JA tree is a fruit-bearing species belonging to the genus Prunus. Dried and pickled JA, called “umeboshi” in Japanese, is a typical traditional Japanese pickled food, which is made from ripened JA pickled with salt. The taste of umeboshi is extremely sour and salty, and it is usually eaten with rice. This traditional Japanese pickle is considered to have antibacterial activity, and to cause facilitation of salivary secretion and digestion in the gastrointestinal system[1,13-15].
The improvement in gastric motility resulting from intake of JA observed in this study can be attributed to several mechanisms. First, the high acidity of JA may be responsible for this beneficial effect. Dried and pickled JA contains strong acids, including citric acid and malic acid. A previous report showing that JA has laxative effects in a low-fiber diet-induced constipation rat model[9] indicated that citric acid and malic acid accelerate spontaneous contraction of the isolated rat colon. In this regard, such strong acid components may affect gastrointestinal motility. Second, the increased alimentary fiber due to ingestion of JA could also reduce dysmotility. Alimentary fiber increases fecal output and improves gastrointestinal motility by promoting gastrointestinal tract emptying[16-18]. In addition, it has been reported that the fiber contained in JA changes the composition of the intestinal flora, and possesses fecal lipid excretion effects and feces bulking effects in adult mice[10]. Gastrointestinal dysmotility is related to the type of intestinal flora[19,20], and the change in the composition of intestinal flora induced by the fiber in JA may improve gastrointestinal motility. Finally, when we ingest or imagine sour foods, secretion of saliva and gastric juice is facilitated. In this regard, the sour taste of JA, largely resulting from the citric acid content, can induce saliva secretion[14,15,21]. Saliva helps chewing, initial swallowing, and absorption of food particles[22]; hence, increased saliva secretion induced by the sour taste of JA can improve dysmotility.
Daily intake of JA did not improve GERD-related acid reflux symptoms in our study. In addition, improvement of gastric dysmotility by JA intake was observed only in H. pylori-negative subjects. Previously, we reported that JA intake inhibits H. pylori infection and reduces active mucosal inflammation[8]. H. pylori has the ability to neutralize gastric acid, and therefore, suppression of the activity of H. pylori by intake of JA may improve gastric-acid secretion. Conversely, the anti-H. pylori effect of JA may worsen acid reflux symptoms in H. pylori-positive subjects, although the effect of H. pylori suppression on GERD is not well established[23,24]. Meanwhile, gastric emptying is reportedly significantly slower in H. pylori-positive patients than H. pylori-negative patients[25]. Absence of improvement in dysmotility by JA intake in H. pylori-positive subjects suggests that the effect of JA on gastric dysmotility may not overcome the negative effects of H. pylori infection on gastric motility.
Daily intake of JA improved dysmotility symptoms in both men and women. In contrast, improvement of dysmotility by JA intake was seen only in non-elderly subjects. One of the reasons for absence of the effect of JA in elderly subjects may be impaired visceral sensations due to aging[26]. Hence, the effect of JA on improvement of gastrointestinal motility may not surpass the depression of gastrointestinal motility due to aging.
This study has several limitations. First, because JA is considered to be a “healthy” food with curative or beneficial effects, it is possible that those who have a higher intake of JA may also be more likely to have a healthier lifestyle. Such lifestyles, rather than JA intake, may affect GERD-related symptoms. Second, neither smoking habit nor body weight data were collected in this study. Smoking and body weight are factors that are known to affect the GERD condition[27,28]. Third, subjects in this study did not undergo endoscopy to assess for GERD. However, all GERD patients do not show positive endoscopic findings, and therefore, other methods, such as the questionnaire survey used in this study, may also provide sufficient information to make the diagnosis of GERD. Fourth, the presence of diabetes may affect dysmotility-like symptoms, particularly in elderly subjects[29,30]. Although we investigated the presence of diabetes in some of our patients, significant correlations with dysmotility-like symptoms were not observed (data not shown because of the limited number of subjects analyzed). Finally, our cohort included only a few GERD (FSSG ≥ 8) patients. To further demonstrate the effectiveness of JA on improvement of GERD, the correlation between intake of JA and GERD symptoms should be examined in GERD patients in the future.
Daily intake of JA improves digestive dysmotility symptoms, resulting in relief of GERD symptoms. The effect is more obvious in non-elderly and H. pylori-negative subjects. Hence, JA should be recommended as a dietary supplement in young adults in developed countries who have GERD symptoms. Moreover, improvement of hygiene will lower the prevalence of H. pylori infection, particularly in Asian countries, where people eat mainly rice, since intake of JA with rice would alleviate GERD symptoms in susceptible populations. Elucidation of the precise mechanism of improvement in gastric motility by JA may lead to the development of new drugs for GERD.
COMMENTS
Background
Japanese apricot (JA), which is eaten as a daily food in Japan, is considered to have medicinal benefits. Gastroesophageal reflux disease (GERD) is a common disease in Western countries. Recently, the number of GERD patients has also been increasing in Japan. The authors focused on the effect of JA on GERD-related symptoms in this study.
Research frontiers
The authors investigated and compared GERD symptoms between Japanese inhabitants who took and did not take JA daily, using the validated questionnaire, “the Frequency Scale for Symptoms of GERD”, to quantify the severity of GERD symptoms and differentiate between acid-related symptoms and dysmotility-related symptoms.
Innovations and breakthroughs
Daily intake of JA improves digestive dysmotility, resulting in relief of GERD symptoms. The effect is more obvious in non-elderly and Helicobacter pylori-negative subjects. Hence, JA should be recommended as a dietary supplement in young adults in developed countries who have GERD symptoms.
Applications
Elucidation of the precise mechanism of improvement of gastric motility by JA may lead to development of new drugs for GERD.
Terminology
The FSSG questionnaire for GERD related symptoms, which was developed by Kusano et al in Japan, was evaluated. The questionnaire consists of 12 questions regarding GERD-related symptoms, including 7 questions associated with acid reflux symptoms and 5 questions asking about gastrointestinal dysmotility symptoms. Each question was answered on a 4-point scale [0 (never), 1 (occasionally), 2 (sometimes), 3 (often), or 4 (always)], with higher scores indicating more severe GERD-related symptoms. GERD was defined as a total score ≥ 8, which is the recommended cut-off FSSG score for GERD.
Peer-review
This is an interesting manuscript reporting the effect of JA on upper gastrointestinal symptoms using a validated questionnaire. This is a well-written paper, limited by the absence of objective measurement of GERD, limitations already reported by the Authors. Discussion is complete and the limitations of the study have been fully highlighted. Prospective studies are needed to assess the role of JA in the management of GERD and functional hp negative dyspepsia.
Footnotes
Institutional review board statement: The study was reviewed and approved by the Wakayama Medical University Institutional Review Board, Wakayama No.1523.
Informed consent statement: Written, informed consent was obtained from all participants.
Conflict-of-interest statement: There is no conflict of interest in this study.
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/
Peer-review started: January 17, 2015
First decision: March 27, 2015
Article in press: May 21, 2015
P- Reviewer: Ota K, Samiullah S, Vailati C S- Editor: Yu J L- Editor: A E- Editor: Liu XM
References
- 1.Chuda Y, Ono H, Ohnishi-Kameyama M, Matsumoto K, Nagata T, Kikuchi Y. Mumefural, citric acid derivative improving blood fluidity from fruit-juice concentrate of Japanese apricot (Prunus mume Sieb. et Zucc) J Agric Food Chem. 1999;47:828–831. doi: 10.1021/jf980960t. [DOI] [PubMed] [Google Scholar]
- 2.Kim HS, Choi EJ, Park H. The effect of mosapride citrate on proximal and distal colonic motor function in the guinea-pig in vitro. Neurogastroenterol Motil. 2008;20:169–176. doi: 10.1111/j.1365-2982.2007.00996.x. [DOI] [PubMed] [Google Scholar]
- 3.Yingsakmongkon S, Miyamoto D, Sriwilaijaroen N, Fujita K, Matsumoto K, Jampangern W, Hiramatsu H, Guo CT, Sawada T, Takahashi T, et al. In vitro inhibition of human influenza A virus infection by fruit-juice concentrate of Japanese plum (Prunus mume SIEB. et ZUCC) Biol Pharm Bull. 2008;31:511–515. doi: 10.1248/bpb.31.511. [DOI] [PubMed] [Google Scholar]
- 4.Jeong JT, Moon JH, Park KH, Shin CS. Isolation and characterization of a new compound from Prunus mume fruit that inhibits cancer cells. J Agric Food Chem. 2006;54:2123–2128. doi: 10.1021/jf0523770. [DOI] [PubMed] [Google Scholar]
- 5.Kim BJ, Kim JH, Kim HP, Heo MY. Biological screening of 100 plant extracts for cosmetic use (II): anti-oxidative activity and free radical scavenging activity. Int J Cosmet Sci. 1997;19:299–307. doi: 10.1046/j.1467-2494.1997.171726.x. [DOI] [PubMed] [Google Scholar]
- 6.Jung BG, Ko JH, Cho SJ, Koh HB, Yoon SR, Han DU, Lee BJ. Immune-enhancing effect of fermented Maesil (Prunus mume Siebold & amp; Zucc.) with probiotics against Bordetella bronchiseptica in mice. J Vet Med Sci. 2010;72:1195–1202. doi: 10.1292/jvms.09-0555. [DOI] [PubMed] [Google Scholar]
- 7.Tsuji R, Koizumi H, Fujiwara D. Effects of a plum (Prunus mume Siebold and Zucc.) ethanol extract on the immune system in vivo and in vitro. Biosci Biotechnol Biochem. 2011;75:2011–2013. doi: 10.1271/bbb.100886. [DOI] [PubMed] [Google Scholar]
- 8.Enomoto S, Yanaoka K, Utsunomiya H, Niwa T, Inada K, Deguchi H, Ueda K, Mukoubayashi C, Inoue I, Maekita T, et al. Inhibitory effects of Japanese apricot (Prunus mume Siebold et Zucc.; Ume) on Helicobacter pylori-related chronic gastritis. Eur J Clin Nutr. 2010;64:714–719. doi: 10.1038/ejcn.2010.70. [DOI] [PubMed] [Google Scholar]
- 9.Na JR, Oh KN, Park SU, Bae D, Choi EJ, Jung MA, Choi CY, Lee DW, Jun W, Lee KY, et al. The laxative effects of Maesil (Prunus mume Siebold & amp; Zucc.) on constipation induced by a low-fibre diet in a rat model. Int J Food Sci Nutr. 2013;64:333–345. doi: 10.3109/09637486.2012.738648. [DOI] [PubMed] [Google Scholar]
- 10.Tamura M, Ohnishi Y, Kotani T, Gato N. Effects of new dietary fiber from Japanese Apricot (Prunus mume Sieb. et Zucc.) on gut function and intestinal microflora in adult mice. Int J Mol Sci. 2011;12:2088–2099. doi: 10.3390/ijms12042088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kusano M, Shimoyama Y, Sugimoto S, Kawamura O, Maeda M, Minashi K, Kuribayashi S, Higuchi T, Zai H, Ino K, et al. Development and evaluation of FSSG: frequency scale for the symptoms of GERD. J Gastroenterol. 2004;39:888–891. doi: 10.1007/s00535-004-1417-7. [DOI] [PubMed] [Google Scholar]
- 12.Furuta T, Shimatani T, Sugimoto M, Ishihara S, Fujiwara Y, Kusano M, Koike T, Hongo M, Chiba T, Kinoshita Y. Investigation of pretreatment prediction of proton pump inhibitor (PPI)-resistant patients with gastroesophageal reflux disease and the dose escalation challenge of PPIs-TORNADO study: a multicenter prospective study by the Acid-Related Symptom Research Group in Japan. J Gastroenterol. 2011;46:1273–1283. doi: 10.1007/s00535-011-0446-2. [DOI] [PubMed] [Google Scholar]
- 13.Fujita K, Hasegawa M, Fujita M, Kobayashi I, Ozasa K, Watanabe Y. [Anti-Helicobacter pylori effects of Bainiku-ekisu (concentrate of Japanese apricot juice)] Nihon Shokakibyo Gakkai Zasshi. 2002;99:379–385. [PubMed] [Google Scholar]
- 14.Minami S, Suzuki M, Takemura A, Takei Y, Arakawa S, Yoshizawa Y, Matsuura Y, Kawahara K. Optimal timing of MR sialography by use of a simple method of stimulating the salivary gland: a preliminary report. Radiol Phys Technol. 2008;1:208–213. doi: 10.1007/s12194-008-0030-5. [DOI] [PubMed] [Google Scholar]
- 15.Morimoto Y, Ono K, Tanaka T, Kito S, Inoue H, Shinohara Y, Yokota M, Inenaga K, Ohba T. The functional evaluation of salivary glands using dynamic MR sialography following citric acid stimulation: a preliminary study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2005;100:357–364. doi: 10.1016/j.tripleo.2004.11.053. [DOI] [PubMed] [Google Scholar]
- 16.Yang J, Wang HP, Zhou L, Xu CF. Effect of dietary fiber on constipation: a meta analysis. World J Gastroenterol. 2012;18:7378–7383. doi: 10.3748/wjg.v18.i48.7378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Anderson JW, Baird P, Davis RH, Ferreri S, Knudtson M, Koraym A, Waters V, Williams CL. Health benefits of dietary fiber. Nutr Rev. 2009;67:188–205. doi: 10.1111/j.1753-4887.2009.00189.x. [DOI] [PubMed] [Google Scholar]
- 18.Marlett JA, McBurney MI, Slavin JL. Position of the American Dietetic Association: health implications of dietary fiber. J Am Diet Assoc. 2002;102:993–1000. doi: 10.1016/s0002-8223(02)90228-2. [DOI] [PubMed] [Google Scholar]
- 19.Shimizu K, Ogura H, Asahara T, Nomoto K, Morotomi M, Nakahori Y, Osuka A, Yamano S, Goto M, Matsushima A, et al. Gastrointestinal dysmotility is associated with altered gut flora and septic mortality in patients with severe systemic inflammatory response syndrome: a preliminary study. Neurogastroenterol Motil. 2011;23:330–335, e157. doi: 10.1111/j.1365-2982.2010.01653.x. [DOI] [PubMed] [Google Scholar]
- 20.Husebye E, Skar V, Høverstad T, Melby K. Fasting hypochlorhydria with gram positive gastric flora is highly prevalent in healthy old people. Gut. 1992;33:1331–1337. doi: 10.1136/gut.33.10.1331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Durán V, Domínguez P, Morales I, López RO. [Kinetic assessment of salivary secretory response to citric acid. Differences with pilocarpine] Rev Med Chil. 1998;126:1330–1337. [PubMed] [Google Scholar]
- 22.Pedersen AM, Bardow A, Jensen SB, Nauntofte B. Saliva and gastrointestinal functions of taste, mastication, swallowing and digestion. Oral Dis. 2002;8:117–129. doi: 10.1034/j.1601-0825.2002.02851.x. [DOI] [PubMed] [Google Scholar]
- 23.Tan J, Wang Y, Sun X, Cui W, Ge J, Lin L. The effect of Helicobacter pylori eradication therapy on the development of gastroesophageal reflux disease. Am J Med Sci. 2015;349:364–371. doi: 10.1097/MAJ.0000000000000429. [DOI] [PubMed] [Google Scholar]
- 24.Yaghoobi M, Farrokhyar F, Yuan Y, Hunt RH. Is there an increased risk of GERD after Helicobacter pylori eradication?: a meta-analysis. Am J Gastroenterol. 2010;105:1007–1013; quiz 1006, 1014. doi: 10.1038/ajg.2009.734. [DOI] [PubMed] [Google Scholar]
- 25.Fock KM, Khoo TK, Chia KS, Sim CS. Helicobacter pylori infection and gastric emptying of indigestible solids in patients with dysmotility-like dyspepsia. Scand J Gastroenterol. 1997;32:676–680. doi: 10.3109/00365529708996517. [DOI] [PubMed] [Google Scholar]
- 26.Manrique T, Morón I, Ballesteros MA, Guerrero RM, Gallo M. Hippocampus, ageing, and taste memories. Chem Senses. 2007;32:111–117. doi: 10.1093/chemse/bjl042. [DOI] [PubMed] [Google Scholar]
- 27.Nouraie M, Radmard AR, Zaer-Rezaii H, Razjouyan H, Nasseri-Moghaddam S, Malekzadeh R. Hygiene could affect GERD prevalence independently: a population-based study in Tehran. Am J Gastroenterol. 2007;102:1353–1360. doi: 10.1111/j.1572-0241.2007.01208.x. [DOI] [PubMed] [Google Scholar]
- 28.Lee HL, Eun CS, Lee OY, Jeon YC, Sohn JH, Han DS, Yoon BC, Choi HS, Hahm JS, Lee MH, et al. Association between GERD-related erosive esophagitis and obesity. J Clin Gastroenterol. 2008;42:672–675. doi: 10.1097/MCG.0b013e31806daf64. [DOI] [PubMed] [Google Scholar]
- 29.Kong MF, Horowitz M. Diabetic gastroparesis. Diabet Med. 2005;22 Suppl 4:13–18. doi: 10.1111/j.1464-5491.2005.1761e.x. [DOI] [PubMed] [Google Scholar]
- 30.Parkman HP, Hasler WL, Fisher RS. American Gastroenterological Association technical review on the diagnosis and treatment of gastroparesis. Gastroenterology. 2004;127:1592–1622. doi: 10.1053/j.gastro.2004.09.055. [DOI] [PubMed] [Google Scholar]


