Abstract
Objective
Systematically review frequency and quality of adverse event (AE) reports in randomized clinical trials (RCTs) of Tai Chi (TC).
Data Sources
Electronic searches of PubMed/MEDLINE and additional databases from inception through March 2013 of English-language RCTs. Search terms were tai chi, taiji, tai chi chuan. Data were independently extracted by two investigators.
Study Selection
We included all available randomized controlled trials (RCTs) that were published in English and used Tai Chi as an intervention. Inclusion and exclusion of studies were reported in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines.
Data Extraction
Eligible RCTs were categorized with respect to AE reporting: 1) No mention of protocols for monitoring AEs or reports of AEs; 2) Reports of AEs either with or without explicit protocols for monitoring AEs.
Data Synthesis
153 eligible RCTs were identified, most targeting older adults. Only 50 eligible trials (33%) included reporting of AEs, and of these, only 18 trials (12% overall) also reported an explicit AE monitoring protocol. Protocols varied with respect to rigor of systematic monitoring in both Tai Chi and comparison groups. Reported AEs were typically minor and expected, and primarily musculoskeletal related (e.g., knee and back pain); no intervention-related serious AEs were reported.
Conclusions
Tai Chi is unlikely to result in serious adverse events, but may be associated with minor musculoskeletal aches and pains. However, poor and inconsistent reporting of AEs greatly limits the conclusions that can be drawn regarding the safety of Tai Chi.
Keywords: Tai Chi, Safety, Adverse Event, Randomized Controlled Trial
Paralleling the rapidly expanding adult population in the U.S. is a growing appreciation for the benefits of exercise and physical activity in the prevention and rehabilitation of age-related disease. 1, 2Abbreviations Poor adherence to exercise programs, especially in older adults,3 has motivated research to identify novel, cost-effective, and sustainable exercises––including complementary and alternative therapies––to address this population need. Tai Chi is a low-impact, mind-body exercise originating in China that has become increasingly popular 4-6 and has become a recognized therapeutic tool by the Western medical community. One of the key features that has made Tai Chi a promising intervention, especially for older and rehabilitating adults, is its purported safety. However, to our knowledge, there has not been a formal review of the literature that has specifically and comprehensively evaluated the reporting of adverse events and the safety of Tai Chi.
Adverse event (AE) reporting within clinical trials is an important source for evaluating the safety of new therapies. An AE is broadly defined as any unfavorable or unintended event that occurs during the course of a study. Typically, identification and reporting of AEs is not restricted to events believed a priori to be directly related to the intervention; in some studies, relatedness is only appreciated after review of all events during a trial.7 Monitoring of safety and AEs during clinical trials is required by Institutional Review Boards, and international research guidelines for all human research involving the delivery of treatment interventions have been developed. The CONSORT has suggested that AEs should be described in the results section of published articles.8 However, even in pharmacological trials, where guidelines are well developed and definitions of AEs are relatively clear, reporting is inconsistent.9-12 Complete and consistent reporting of AEs in trials of non-pharmacological interventions can be even more problematic, due to less developed guidelines.13, 14
The main purpose of this systematic review is to evaluate the frequency and type of AE occurrences in RCTs of Tai Chi for all populations. A secondary aim is to evaluate the consistency and quality of AE monitoring protocols used in the included trials. We conclude with recommendations for improving our understanding of the safety of Tai Chi, including guidelines for reporting AEs in future trials of Tai Chi and related mind-body exercises.
Methods
Literature Search
Electronic literature searches were conducted using PubMed/MEDLINE, EBSCOhost and the Cochrane Library from inception through March 2013. Search terms were tai chi, taiji, tai chi chuan; searches were limited to English-language RCTs. Hand searches were performed of retrieved articles for additional references.
Eligibility Criteria
We first included all available randomized controlled trials (RCTs) that were published in English and used Tai Chi as an intervention. No exclusions were made on the basis of population, type of Tai Chi intervention or intervention controls. Inclusion and exclusion of studies were reported in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines.
All identified RCTs were then categorized into two groups with respect to their reporting of adverse events. Group I studies did not report AEs in the results or discussion and did not include any formal protocols for monitoring and reporting and were thus excluded from further analysis. Group II studies did report AEs in the results or discussion, with or without a formal protocol for monitoring and reporting AEs.
Data Extraction and Synthesis
Data pertinent to AE reporting and AE monitoring protocols, as well as study design, location, duration, subject population, and Tai Chi and control interventions were independently extracted by two reviewers in a standardized manner. Discrepancies were resolved through discussion, and a third arbiter when needed. Synthesis of data on AEs is summarized for all Group II studies in narrative form, including explicit report and detail of an AE monitoring protocol, details of study design, and types and frequencies of AE's. Our analytic methods were based on descriptive statistics which were calculated within an Excel database. The methodological quality of reporting for the subset of studies that included an explicit AE reporting protocol was further assessed using criteria from the CONSORT extension checklist of ten recommendations when reporting harms in randomized controlled trials.8 Key criteria are: defining adverse events (#3), clarifying how harms-related information was collected (#4), describing plans for presenting and analyzing information on harms (#5), and describing information on harms for all treatment arm s (#6).
Reporting of Adverse Events
Adverse events were defined according to the National Institutes of Health (NIH) as follows:15 “Unfavorable changes in health … that occur in trial participants during the clinical trial or within a specified period following the trial.” Using NIH guidelines, adverse events were further divided into two types, “Serious” and “Other (not including Serious).” Serious Adverse Events include adverse events that result in death, require either in-patient hospitalization or the prolongation of hospitalization, are life-threatening, result in a persistent or significant disability/incapacity or result in a congenital anomaly/birth defect. Other important medical events, based upon appropriate medical judgment, may also be considered Serious Adverse Events if a trial participant's health is at risk and intervention is required to prevent an outcome mentioned. Other Adverse Events are those that are not Serious Adverse Events.
For the present systematic review, to qualify as a reported AE an incident had to be explicitly referred to as AE. However, to provide context for interpreting quality of reporting, we also systematically quantified all health events reported in publications, including explicit or implicit references to health related drop-outs in CONSORT flow diagrams, study results and discussion sections. For a study to qualify as having an AE reporting protocol, there had to be explicit mention of methods associated with monitoring, soliciting, and recording AE's (e.g., direct observation, during outcome visits, regular surveys or phone calls), either directly from participants or from staff or intervention instructors.
Results
Literature Search
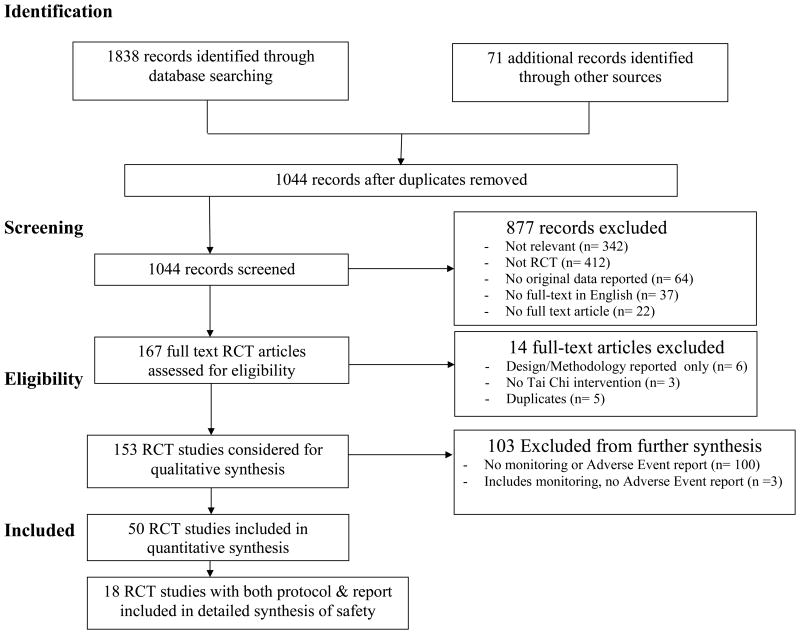
Figure 1 summarizes the flow of our literature search and selection process. Our initial search resulted in 1,909 studies. Eight hundred and sixty-five publications were excluded because they were duplicate articles in different databases. Eight hundred and seventy-seven publications were further excluded for the following reasons: 342 irrelevant to the search (e.g., author last name “Tai”); 412 not randomized controlled trials; 64 did not report original data, 37 non-English language; 22 not full text articles (i.e., abstracts). Of the remaining 167 articles: 6 included only information on design methodology; 3 did not utilize Tai Chi as an intervention; and 5 reported identical duplicate data. This resulted in a total of 153 publications. Of these, 100 were excluded because they did not have a monitoring protocol or adverse event reports. Three additional studies included a monitoring protocol, but did not have adverse event reports. Fifty trials mentioned AE reporting and were included for quantitative synthesis.
Figure 1. PRISMA.
Participant characteristics and study setting
The 50 trials identified by our search that included an AE report are summarized in Table 1. The average age of study participants was 65y (median= 69y, range 11-102y). Forty-two studies included men and women, 7 women only, and 1 men only. One trial was in adolescents. Twentysix studies recruited community dwelling individuals, 18 were based in hospital settings, 5 were based in independent or assisted senior living facilities, and 1 in a university setting. Twelve studies targeted individuals with balance impairments, musculoskeletal weakness, or reduced physical function; 20 with metabolic, cardiovascular, or immune disorders; 9 with chronic pain; and 4 with cognitive deficits or mood disorders. The remaining studies included healthy individuals that ranged from young to older adults (n= 5). One half of the studies were conducted in the United States (n = 25).
Table 1. Randomized controlled trials of Tai Chi (TC) that include reporting of adverse events (Aes) (n= 50).
| Population Author last name (Year) |
Interventions type; dose; sample size (n) |
AE Protocol included (Y/N)? If Y,
|
AEs reported by author | AEs reported for all groups (Y/N)? |
|---|---|---|---|---|
| Healthy adults | ||||
| Irwin et al (2008)56 |
|
|
|
|
| Li et al (2004)32 |
|
|
|
|
| Liu et al (2012)20 |
|
|
|
|
| Nedeljkovic et al (2012)21 |
|
|
|
|
| Wolfson et al (1996)19 |
|
|
|
|
| Impaired balance, musckuloskeletal health, reduced physical function | ||||
| Day et al (2012)22 |
|
|
|
|
| Dechamps et al (2009)57 |
|
|
|
|
| Dechamps et al (2010)42 |
|
|
|
|
| Li et al (2004)33 |
|
|
|
|
| Li et al (2005)43 |
|
|
|
|
| Li et al (2012)58 |
|
|
|
|
| Ming-Chien et al (2010)23 |
|
|
|
|
| Sattin et al (2005)59 |
|
|
|
|
| Shen et al (2010)45, 67 |
|
|
|
|
| Taylor et al (2012)53 |
|
|
|
|
| Wayne et al (2012)49 |
|
|
|
|
| Wolf et al (2003)55 |
|
|
|
|
| Adults with chronic pain | ||||
| Abbott et al (2006)41 |
|
|
|
|
| Brismee et al (2007)17 |
|
|
|
|
| Fransen et al (2007)24 |
|
|
|
|
| Hall et al (2011)16 |
|
|
|
|
| Jones et al (2012)44 |
|
|
|
|
| Ni et al (2010)30 |
|
|
|
|
| Song et al (2003)25 |
|
|
|
|
| Wang et al (2009)54 |
|
|
|
|
| Wang et al (2010)31 |
|
|
|
|
| Metabolic, cardiovascular, and immune disorders | ||||
| Barrow et al (2007)60 |
|
|
|
|
| Caminiti et al (2011)61 |
|
|
|
|
| Chan et al (2010)34 |
|
|
|
|
| Chen et al (2010)35 |
|
|
|
|
| Dechamps et al (2008)36 |
|
|
|
|
| Hart et al (2004)62 |
|
|
|
|
| Jung et al (2012)26 |
|
|
|
|
| Leung et al (2012)27 |
|
|
|
|
| Sato et al (2010)37 |
|
|
|
|
| Taylor-Piliae et al (2012)28 |
|
|
|
|
| Tsai et al (2003)29 |
|
|
|
|
| Tsang et al (2007)46, 47 |
|
|
|
|
| Tsang et al (2010)48 |
|
|
|
|
| Wang et al (2008)63 |
|
|
|
|
| Wang et al (2010)38 |
|
|
|
|
| Yeh et al (2004)50 |
|
|
|
|
| Yeh et al (2010)51 |
|
|
|
|
| Yeh et al (2011)52 |
|
|
|
|
| Yeh et al (2012)39 |
|
|
|
|
| Zhang et al (2008)64 |
|
|
|
|
| Adults with cognitive deficites or mood disorders | ||||
| Lam et al (2011)66 |
|
|
|
|
| Lavretsky et al (2011)40 |
|
|
|
|
| Tsai et al (2012)65 |
|
|
|
|
| Yeung et al (2012)18 |
|
|
|
|
Intervention and control group characteristics
Tai Chi interventions varied greatly in content, dosage, duration and intensity. The majority of studies (n= 30) employed interventions described as ‘simplified’ research protocols, and/or included a subset of movements typically learned in traditional Tai Chi choreographed sets; 13 employed complete traditional Tai Chi sets (e.g., Yang style 24-form); 1 integrated Tai Chi exercises within a multi-component intervention including other cognitive or physical exercises; 1 utilized community-based pragmatic interventions; and 5 studies did not provide Tai Chi intervention details.
Individual Tai Chi sessions varied in duration from 20 to 120 minutes. The frequency of sessions varied from 1 to 5 times per week, with overall training programs lasting 6 weeks to 1 year. Qualifications of instructors were mentioned in only 22 of 50 studies.
Twenty trials used active exercise control groups (e.g., resistance training, aerobics, flexibility, and balance training), 1 employed non-exercise activities (e.g., dietary supplements); 10 studies utilized group education and support programs; and 19 employed a non-intervention control including waitlist and usual care.
Patterns of Adverse Events Reporting
Of the 153 identified publications evaluating Tai Chi, 100 (65%) included no mention of either AE monitoring protocols or AEs, and an additional 3 studies only mentioned an AE protocol but no AE report. Of the 50 eligible studies that included an explicit AE report, only 18 trials included an explicit monitoring protocol, which provides a more reliable framework for interpreting the validity of AE reports. Information for all 50 trials is summarized in Table 1.
Reported AEs varied in scope and detail (Table 1). Fourteen studies16-29 (28%) solely reported on intervention-related AEs; 15 studies30-44 (30%) did not specify between groups; 20 studies45-65 (40%) more comprehensively reported other AEs including non-intervention related hospitalizations and new medical diagnoses (e.g. cancer). One study66 (2%) reported AEs only in the control group.
Among the 50 studies in Table 1, no serious AEs related to Tai Chi was reported, and 32 studies 18, 20, 21, 26-29, 31-34, 36-39, 41-44, 50-52, 55-57, 59-65 reported no occurrence of any AEs related to intervention. Fifteen 16, 17, 19, 23-25, 30, 45, 47-49, 53, 54, 58, 59 of the 50 studies specifically reported occurrences of minor musculoskeletal aches and pain, with complaints of lower extremity pain (knee and ankle) being most common. Six studies16, 19, 24, 47, 49, 58 mentioned a report of back/spine related pain. In one47 of these back pain reports, pain was severe leading to study withdrawal; subsequent analysis revealed a pre-existing condition of stenosis missed during screening. Falls were not consistently reported as AEs, in part because falls were considered as outcomes in many studies. Four48, 52, 58, 66 studies reported falls.
AE monitoring protocols varied greatly among the studies in Table 1. Of the 18 studies that included an explicit AE monitoring protocol, slightly more than half included explicit tracking of AEs in both the Tai Chi intervention group and the control16, 30, 31, 45-52, 67 (n = 10; 56%); 2 studies17, 18 (11%) only reported monitoring protocols for Tai Chi and 6 studies19, 32, 33, 53-55 (33%) did not explicitly state which groups were monitored. Details regarding how AEs were monitored also varied, with 7 studies17, 19, 32, 33, 45, 48, 49, 67 (39%) including multiple methods (e.g., study staff queries, instructor observation), 9 studies 16, 18, 31, 46, 47, 50-54 (50%) reported only one source of information, and 2 studies30, 55 (11%) did not explicitly indicate how AE information was collected. Similarly, frequency of monitoring AEs also varied, with 5 studies17-19, 32, 33 (28%) querying participants after each intervention session; 9 studies30, 31, 45-52, 67 (50%) collecting AE reports at regular assessments (e.g., weekly or monthly); 1 (6%) study53 relying on recall at the end of the intervention period; 3 studies16, 54, 55 (17%) did not explicitly describe frequency of monitoring.
When evaluated according to the CONSORT extension checklist for reporting harms in randomized controlled trials,10 studies (56%)listed addressed adverse events with definitions for each (recommendation #3), 13 (72%) clarified how harms-related information was collected (#4), 1 (6%) described plans for presenting and analyzing harms (#5), 7 (39%) described for each arm the participant withdrawals due to harms (#6), and 6 (33%) provided a balanced discussion of benefits and harms (#10) (see Table 2).
Table 2. CONSORT extension checklist of ten recommendations when reporting harms in randomized controlled trials (n = 18).
| Author (Year) | 1 | 2 | 3 | 4 | 5 | 6 | 7* | 8** | 9 | 10 |
|---|---|---|---|---|---|---|---|---|---|---|
| Brismee et al (2007)17 | X | X | X | |||||||
| Hall et al (2011)16 | X | |||||||||
| Li et al (2004)33 | X | |||||||||
| Li et al (2004)32 | X | X | X | |||||||
| Ni et al (2010)30 | X | X | X | X | ||||||
| Shen et al (2010)45, 67 | X | X | X | X | X | X | X | |||
| Taylor et al (2012)53 | X | X | X | |||||||
| Tsang et al (2007)46, 47 | X | X | X | X | X | |||||
| Tsang et al (2010)48 | X | X | X | X | X | |||||
| Wang et al (2009)54 | X | X | X | |||||||
| Wang et al (2010)31 | X | X | X | X | X | |||||
| Wayne et al (2012)49 | X | X | X | |||||||
| Wolf et al (2003)55 | X | X | X | |||||||
| Wolfson et al (1996)19 | X | X | X | |||||||
| Yeh et al (2004)50 | X | X | X | X | ||||||
| Yeh et al (2010)51 | X | X | X | X | X | |||||
| Yeh et al (2011)52 | X | X | X | X | X | |||||
| Yeung et al (2012)18 | X | X | X | X | X |
We considered study to have addressed recommendation 7 if the denominator for harms could be easily inferred from the CONSORT flow diagram or other text describing 'what follow up-time counts towards overall exposure'
We considered study to have addressed recommendation 8 if adverse events were further categorized per arm by type, grade, OR seriousness (where we included relatedness to the intervention as a type). If there were no events in the control arm, this needed to be stated.
Discussion
Tai Chi is increasingly recognized by the Western medical community as an effective exercise for rehabilitation and prevention of multiple medical conditions, and Tai Chi programs are now offered through academic medical centers, assisted living facilities, and community senior centers across the United States.68 Tai Chi's purported safety, along with evidence of its clinical effectiveness and cost-effectiveness, has likely contributed to growth in its health-related use, especially among older adults and those deconditioned by chronic illnesses.
Our systematic review has identified significant flaws in the reporting of adverse events in trials of Tai Chi, which greatly limits the conclusions that can be drawn to date regarding Tai Chi's safety. Based on 153 randomized trials of Tai Chi published between 1977 and 2013, we found highly inconsistent, and overall, very poor reporting of AE monitoring protocols and AEs. Sixty five percent of these trials (n = 100) included no mention whatsoever of either monitoring protocols or AEs, and an additional 23% (n = 35) did not include the adequate information required for evaluating the validity of AE reports (i.e., information on the monitoring protocols used to solicit information on AEs, or the AEs themselves). Of note, 39% of the 100 studies that included no explicit mention of an AE included reports of health-related drop-outs in either the study's CONSORT diagram or in the publication text, suggesting that AEs were under-reported. Only 18 of the 50 trials included in Table 1 (representing < 12% of all 153 trials) reported both an AE monitoring protocol and explicit AE reports, and the quality of reporting in these studies was variable with only a small proportion of studies adequately meeting important CONSORT recommendations for reporting harms in RCTs. Some studies53 relied on monitoring procedures with a high risk of bias (e.g., recall of AEs at a single time point at the end of the study), or only monitored and reported AEs for the Tai Chi group making it impossible to assess if the frequency or types of events observed in a group learning Tai Chi differs from control interventions or natural history. By comparison, the less biased studies included monitoring protocols applied repeatedly throughout the study (e.g., weekly or monthly), and/or solicited information from multiple sources (e.g., patient self-reports, instructor reports), and monitored and documented AEs in both the intervention and control groups. Additionally, reports of AEs in more reliable studies were more comprehensive, not limited to intervention-related events, and provided quantitative data (e.g. frequency of event types). Based on this small subset of more reliable studies, there were no reports of serious AEs, the majority of the reported AEs were unrelated to study interventions, and AEs that were deemed related to the Tai Chi intervention were minor and anticipated musculoskeletal aches and pains.
Reports of minor musculoskeletal pain related to Tai Chi training are consistent with AEs reported in other exercise studies,69, 70 including studies of mind-body therapies like yoga,71, 72 but lower than AEs reported in more combat-oriented martial arts. 73-75 Of note, lower extremity, and especially knee pain, was reported in 9 17, 19, 23, 25, 30, 48, 54, 58, 59 of the 50 trials in Table 1. Biomechanic studies support that during Tai Chi training, practitioners experience higher shear force and frontal plane torques at the ankle, knee, and hip joints, as compared to natural walking.76-79 A recent commentary on Tai Chi safety emphasized that Tai Chi practice requires the knee joint to regularly conform to a semi-flexed position, thus incurring high mechanical load and putting it at risk for injury.80 The commentary cites two observational studies from China with reports of knee injury higher than those observed in our study. In one study, 32 of 219 (15%) novice Tai Chi practitioners experienced some form of knee complication after 3 to 6 months of training.81 In another study of 200 longer-term Tai Chi practitioners, 23% had a history of knee joint injury, 8.5% had patella strain, 7% had meniscus injury, 3.0% had knee fat pad injury, 2.0% had medial collateral ligament injury, 1.5% had cruciate ligament injury, and 1% had lateral collateral injury. The commentary concluded that to minimize knee injuries, Tai Chi training requires careful attention to appropriate load, biomechanics, and overall effort.80 However, these results are difficult to interpret as the prevalence of these injuries in age-matched individuals in the same population is not known. Nevertheless, these observations reflect more widespread concerns expressed in the lay literature about Tai Chi's safety for knees and other musculoskeletal conditions80, 82, 83 especially in those with pre-existing conditions. Of note, no intervention-related cardiovascular adverse events were reported, including in the higher quality studies of heart failure and COPD patients, although these studies are relatively small. Finally, our review also found no reports of psychological AEs, which have been reported in related mind-body exercises including qigong and meditation.84, 85
There is a rich literature highlighting a long history of poor reporting of AEs in clinical trials of both pharmacological and non-pharmacological interventions.86, 87 To address these concerns, the CONSORT Statement extension with recommendations on the reporting of harms was published in 2004. Nevertheless, a recent review of orthopedic physical therapy studies found AE reporting poorly complied with CONSORT guidelines, and like our study, observed that 58% of all studies did not show evidence of any AE monitoring whatsoever.88, 89 Similarly, a Cochrane review on exercise for reducing osteoporosis-related fractures found that none of the 7 reviewed RCTs included AE reporting.90
In keeping with the broad guidelines of the CONSORT Statement Extension of the reporting of harms statement, we emphasize the following guidelines for the reporting of AEs in Tai Chi studies. First, protocols for defining and monitoring AEs should be clearly defined in the methods section of all studies. Second, protocols should include assessments repeated throughout the course of the entire trial. Third, AEs should be assessed using multiple sources of information, including self-reports by patients, pro-active queries by study staff, physician report (if appropriate) and observations by teachers or intervention administrators, as relying on individual sources can be limited. Fourth, monitoring of AEs should take place in all groups (intervention and control) using equivalent protocols. Fifth, all unfavorable changes in medical conditions should be reported as potential AEs, not just those deemed to be intervention related. Finally, reports should be made quantitatively, with information on frequency of occurrence.
While the above recommendations will greatly improve our estimates of potential shorter-term AEs in clinical settings, they will not inform longer-term potential adverse effects in more typical community-based settings where Tai Chi is typically practiced. Thus, the study of AEs in Tai Chi should also include systematic cross-sectional and longitudinal surveys and audits of short- and long-term practitioners in community-based settings as has been done in other emerging integrative medical therapies.91, 92
Study Limitations
There are a number of limitations to this study. First, our study only included trials published in the English language. Future studies might include other languages for a better global estimate of AE reporting. Asian language journals, for example, may be more likely to publish Tai Chi research. Second, because of the small number of studies as well as the heterogeneity of both interventions and controls, our study only employed descriptive statistics and narrative summaries of AE reports. As the literature evolves, future studies with more formal meta-analyses for assessing relative harms of Tai Chi when compared to other control interventions may be helpful. Finally, our study only included AEs reported in randomized trials. As noted above, data from audits and cross-sectional studies, especially of longer-term practitioners, as well as uncontrolled longitudinal studies may better inform long-term effects in the community.
Conclusions
Estimates of potential harm related to any novel therapy is a critical component of the evidence required by the medical community for informing policy and referrals. Similarly, patient concerns regarding exercise safety and injury may limit broader compliance with recommendations for exercise and more active lifestyles.6 Poor and inconsistent reporting of AEs greatly limits the conclusions that can be drawn regarding the safety of Tai Chi. Based on a small number of less biased studies, Tai Chi is unlikely to result in serious adverse events, but may be associated with minor musculoskeletal aches and pains. Until AE reporting in Tai Chi trials is improved, we cannot draw more definitive conclusions regarding its safety. Already existing CONSORT guidelines for comprehensive monitoring and reporting of AEs in future trials of Tai Chi should be enforced. Additionally, these guidelines should be supplemented by systematic audits of short- and long-term practitioners in community based setting.
Acknowledgments
This publication was made possible by grant number R21 AT005501-01A1 from the National Center for Complementary and Alternative Medicine (NCCAM) at the National Institutes of Health (NIH). Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the NCCAM or the NIH.
List of Abbreviations
- AE
Adverse Event
- TC
Tai Chi
Footnotes
Conflicts of Interest: We certify that no party having a direct interest in the results of the research supporting this article has or will confer a benefit on us or on any organization with which we are associated AND, if applicable, we certify that all financial and material support for this research (eg, NIH or NHS grants) and work are clearly identified in the title page of the manuscript. (Wayne PM, Berkowitz DL, Litrownik DE, Yeh GY, Buring JE)
Author contributions: PW conceived the idea for this study. In addition, PW wrote the first draft, extracted data, evaluated studies, and interpreted results. DB contributed to the first draft, conducted literature searches, extracted data, and evaluated studies. DL conducted literature searches, extracted data, and contributed to the manuscript. GY extracted data, and contributed to the manuscript. JB contributed to the manuscript. All authors contributed to the revision and approval of the final version.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Gremeaux V, Gayda M, Lepers R, Sosner P, Juneau M, Nigam A. Exercise and longevity. Maturitas. 2012;73(4):312–7. doi: 10.1016/j.maturitas.2012.09.012. [DOI] [PubMed] [Google Scholar]
- 2.Garber CE, Blissmer B, Deschenes MR, Franklin BA, Lamonte MJ, Lee IM, Nieman DC, Swain DP. American College of Sports Medicine position stand. Quantity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuromotor fitness in apparently healthy adults: guidance for prescribing exercise. Med Sci Sports Exerc. 2011;43(7):1334–59. doi: 10.1249/MSS.0b013e318213fefb. [DOI] [PubMed] [Google Scholar]
- 3.Simek EM, McPhate L, Haines TP. Adherence to and efficacy of home exercise programs to prevent falls: a systematic review and meta-analysis of the impact of exercise program characteristics. Preventive medicine. 2012;55(4):262–75. doi: 10.1016/j.ypmed.2012.07.007. [DOI] [PubMed] [Google Scholar]
- 4.Birdee GS, Wayne PM, Davis RB, Phillips RS, Yeh GY. T'ai chi and qigong for health: patterns of use in the United States. J Altern Complement Med. 2009;15(9):969–73. doi: 10.1089/acm.2009.0174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Barnes PM, Bloom B, Nahin RL. Complementary and alternative medicine use among adults and children: United States, 2007. National health statistics reports. 2008;(12):1–23. [PubMed] [Google Scholar]
- 6.Chodzko-Zajko WBL, Chow R, Firman J, Jahnke R, Park CH, Rosengren K, Sheppard L, Yang Y. National Expert Meeting on Qi Gong and Tai Chi Consensus Report. Urbana, IL: 2005. [Google Scholar]
- 7.Ory M, Resnick B, Jordan PJ, Coday M, Riebe D, Ewing Garber C, Pruitt L, Bazzarre T. Screening, safety, and adverse events in physical activity interventions: collaborative experiences from the behavior change consortium. Ann Behav Med. 2005;29(Suppl):20–8. doi: 10.1207/s15324796abm2902s_5. [DOI] [PubMed] [Google Scholar]
- 8.Ioannidis JP, Evans SJ, Gotzsche PC, O'Neill RT, Altman DG, Schulz K, Moher D. Better reporting of harms in randomized trials: an extension of the CONSORT statement. Annals of internal medicine. 2004;141(10):781–8. doi: 10.7326/0003-4819-141-10-200411160-00009. [DOI] [PubMed] [Google Scholar]
- 9.Raisch DW, Troutman WG, Sather MR, Fudala PJ. Variability in the assessment of adverse events in a multicenter clinical trial. Clinical therapeutics. 2001;23(12):2011–20. doi: 10.1016/s0149-2918(01)80153-3. [DOI] [PubMed] [Google Scholar]
- 10.Breau RH, Gaboury I, Scales CD, Jr, Fesperman SF, Watterson JD, Dahm P. Reporting of harm in randomized controlled trials published in the urological literature. The Journal of urology. 2010;183(5):1693–7. doi: 10.1016/j.juro.2010.01.030. [DOI] [PubMed] [Google Scholar]
- 11.Chowers MY, Gottesman BS, Leibovici L, Pielmeier U, Andreassen S, Paul M. Reporting of adverse events in randomized controlled trials of highly active antiretroviral therapy: systematic review. The Journal of antimicrobial chemotherapy. 2009;64(2):239–50. doi: 10.1093/jac/dkp191. [DOI] [PubMed] [Google Scholar]
- 12.Shukralla AA, Tudur-Smith C, Powell GA, Williamson PR, Marson AG. Reporting of adverse events in randomised controlled trials of antiepileptic drugs using the CONSORT criteria for reporting harms. Epilepsy research. 2011;97(1-2):20–9. doi: 10.1016/j.eplepsyres.2011.06.015. [DOI] [PubMed] [Google Scholar]
- 13.Peterson AL, Roache JD, Raj J, Young-McCaughan S. The need for expanded monitoring of adverse events in behavioral health clinical trials. Contemporary clinical trials. 2013;34(1):152–4. doi: 10.1016/j.cct.2012.10.009. [DOI] [PubMed] [Google Scholar]
- 14.Liu CJ, Latham N. Adverse events reported in progressive resistance strength training trials in older adults: 2 sides of a coin. Arch Phys Med Rehabil. 2010;91(9):1471–3. doi: 10.1016/j.apmr.2010.06.001. [DOI] [PubMed] [Google Scholar]
- 15.(NIH) NIoH. [cited 2013 October 28];Further resources for nih grantees. 2011 May 26; Available from: URL: http://grants.nih.gov/clinicaltrials_fdaaa/definitions.htm.
- 16.Hall AM, Maher CG, Lam P, Ferreira M, Latimer J. Tai chi exercise for treatment of pain and disability in people with persistent low back pain: a randomized controlled trial. Arthritis care & research. 2011;63(11):1576–83. doi: 10.1002/acr.20594. [DOI] [PubMed] [Google Scholar]
- 17.Brismee JM, Paige RL, Chyu MC, Boatright JD, Hagar JM, McCaleb JA, Quintela MM, Feng D, Xu KT, Shen CL. Group and home-based tai chi in elderly subjects with knee osteoarthritis: a randomized controlled trial. Clin Rehabil. 2007;21(2):99–111. doi: 10.1177/0269215506070505. [DOI] [PubMed] [Google Scholar]
- 18.Yeung A, Lepoutre V, Wayne P, Yeh G, Slipp LE, Fava M, Denninger JW, Benson H, Fricchione GL. Tai Chi Treatment for Depression in Chinese Americans: A Pilot Study. American journal of physical medicine & rehabilitation / Association of Academic Physiatrists. 2012;91(10):863–70. doi: 10.1097/PHM.0b013e31825f1a67. [DOI] [PubMed] [Google Scholar]
- 19.Wolfson L, Whipple R, Derby C, Judge J, King M, Amerman P, Schmidt J, Smyers D. Balance and strength training in older adults: intervention gains and Tai Chi maintenance. J Am Geriatr Soc. 1996;44(5):498–506. doi: 10.1111/j.1532-5415.1996.tb01433.x. [DOI] [PubMed] [Google Scholar]
- 20.Liu J, Wang XQ, Zheng JJ, Pan YJ, Hua YH, Zhao SM, Shen LY, Fan S, Zhong JG. Effects of Tai Chi versus Proprioception Exercise Program on Neuromuscular Function of the Ankle in Elderly People: A Randomized Controlled Trial. Evidence-based complementary and alternative medicine : eCAM. 2012;2012:265486. doi: 10.1155/2012/265486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Nedeljkovic M, Ausfeld-Hafter B, Streitberger K, Seiler R, Wirtz PH. Taiji practice attenuates psychobiological stress reactivity--a randomized controlled trial in healthy subjects. Psychoneuroendocrinology. 2012;37(8):1171–80. doi: 10.1016/j.psyneuen.2011.12.007. [DOI] [PubMed] [Google Scholar]
- 22.Day L, Hill KD, Jolley D, Cicuttini F, Flicker L, Segal L. Impact of tai-chi on impairment, functional limitation and disability among pre-clinically disabled older people. A randomised controlled trial Arch Phys Med Rehabil. 2012 Aug;93(8):1400–07. doi: 10.1016/j.apmr.2012.03.018. [DOI] [PubMed] [Google Scholar]
- 23.Ming-Chien C, James CR, Sawyer SF, Brismée JM, Xu KT, Poklikuha G, Dunn DM, Chwan-Li S. Effects of tai chi exercise on posturography, gait, physical function and quality of life in postmenopausal women with osteopaenia: a randomized clinical study. Clin Rehabil. 2010;24(12):1080–90. doi: 10.1177/0269215510375902. [DOI] [PubMed] [Google Scholar]
- 24.Fransen M, Nairn L, Winstanley J, Lam P, Edmonds J. Physical activity for osteoarthritis management: a randomized controlled clinical trial evaluating hydrotherapy or Tai Chi classes. Arthritis Rheum. 2007;57(3):407–14. doi: 10.1002/art.22621. [DOI] [PubMed] [Google Scholar]
- 25.Song R, Lee EO, Lam P, Bae SC. Effects of tai chi exercise on pain, balance, muscle strength, and perceived difficulties in physical functioning in older women with osteoarthritis: a randomized clinical trial. J Rheumatol. 2003;30(9):2039–44. [PubMed] [Google Scholar]
- 26.Jung S, Lee EN, Lee SR, Kim MS, Lee MS. Tai chi for lower urinary tract symptoms and quality of life in elderly patients with benign prostate hypertrophy: a randomized controlled trial. Evidence-based complementary and alternative medicine : eCAM. 2012;2012:624692. doi: 10.1155/2012/624692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Leung RW, McKeough ZJ, Peters MJ, Alison JA. Short-form Sun-style Tai Chi as an exercise training modality in people with COPD. The European respiratory journal : official journal of the European Society for Clinical Respiratory Physiology. 2012;41(5):1051–57. doi: 10.1183/09031936.00036912. [DOI] [PubMed] [Google Scholar]
- 28.Taylor-Piliae RE, Coull BM. Community-based Yang-style Tai Chi is safe and feasible in chronic stroke: a pilot study. Clin Rehabil. 2012;26(2):121–31. doi: 10.1177/0269215511419381. [DOI] [PubMed] [Google Scholar]
- 29.Tsai JC, Wang WH, Chan P, Lin LJ, Wang CH, Tomlinson B, Hsieh MH, Yang HY, Liu JC. The beneficial effects of Tai Chi Chuan on blood pressure and lipid profile and anxiety status in a randomized controlled trial. J Altern Complement Med. 2003;9(5):747–54. doi: 10.1089/107555303322524599. [DOI] [PubMed] [Google Scholar]
- 30.Ni GX, Song L, Yu B, Huang CH, Lin JH. Tai chi improves physical function in older Chinese women with knee osteoarthritis. Journal of clinical rheumatology : practical reports on rheumatic & musculoskeletal diseases. 2010;16(2):64–7. doi: 10.1097/RHU.0b013e3181cf344f. [DOI] [PubMed] [Google Scholar]
- 31.Wang C, Schmid C, Rones R, Kalish R, Yinh J, Goldenberg D, Lee Y, McAlinden T. A randomized trial of tai chi for fibromyalgia. The New England journal of medicine. 2010;363(8):743–54. doi: 10.1056/NEJMoa0912611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Li F, Fisher KJ, Harmer P, Irbe D, Tearse RG, Weimer C. Tai chi and self-rated quality of sleep and daytime sleepiness in older adults: a randomized controlled trial. J Am Geriatr Soc. 2004;52(6):892–900. doi: 10.1111/j.1532-5415.2004.52255.x. [DOI] [PubMed] [Google Scholar]
- 33.Li F, Harmer P, Fisher K, McAuley E. Tai Chi: improving functional balance and predicting subsequent falls in older persons. Med Sci Sports Exerc. 2004;36(12):2046–52. doi: 10.1249/01.mss.0000147590.54632.e7. [DOI] [PubMed] [Google Scholar]
- 34.Chan AW, Lee A, Suen LK, Tam WW. Effectiveness of a Tai chi Qigong program in promoting health-related quality of life and perceived social support in chronic obstructive pulmonary disease clients. Quality of life research : an international journal of quality of life aspects of treatment, care and rehabilitation. 2010;19(5):653–64. doi: 10.1007/s11136-010-9632-6. [DOI] [PubMed] [Google Scholar]
- 35.Chen SC, Ueng KC, Lee SH, Sun KT, Lee MC. Effect of t'ai chi exercise on biochemical profiles and oxidative stress indicators in obese patients with type 2 diabetes. J Altern Complement Med. 2010;16(11):1153–9. doi: 10.1089/acm.2009.0560. [DOI] [PubMed] [Google Scholar]
- 36.Dechamps A, Gatta B, Bourdel-Marchasson I, Tabarin A, Roger P. Pilot study of a 10-week multidisciplinary Tai Chi intervention in sedentary obese women. Clinical journal of sport medicine : official journal of the Canadian Academy of Sport Medicine. 2008;19(1):49–53. doi: 10.1097/JSM.0b013e318193428f. [DOI] [PubMed] [Google Scholar]
- 37.Sato S, Makita S, Uchida R, Ishihara S, Masuda M. Effect of Tai Chi training on baroreflex sensitivity and heart rate variability in patients with coronary heart disease. International Heart Journal. 2010;51(4):238–41. doi: 10.1536/ihj.51.238. [DOI] [PubMed] [Google Scholar]
- 38.Wang W, Sawada M, Noriyama Y, Arita K, Ota T, Sadamatsu M, Kiyotou R, Hirai M, Kishimoto T. Tai Chi exercise versus rehabilitation for the elderly with cerebral vascular disorder: a single-blinded randomized controlled trial. Psychogeriatrics. 2010;10(3):160–6. doi: 10.1111/j.1479-8301.2010.00334.x. [DOI] [PubMed] [Google Scholar]
- 39.Yeh GY, Wood MJ, Wayne PM, Quilty MT, Stevenson LW, Davis RB, Phillips RS, Forman DE. Tai Chi in Patients With Heart Failure With Preserved Ejection Fraction. Congestive heart failure. 2012;19(2):77–84. doi: 10.1111/chf.12005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lavretsky H, Alstein LL, Olmstead RE, Ercoli LM, Riparetti-Brown M, Cyr NS, Irwin MR. Complementary use of tai chi chih augments escitalopram treatment of geriatric depression: a randomized controlled trial. The American Journal Of Geriatric Psychiatry: Official Journal Of The American Association For Geriatric Psychiatry. 2011;19(10):839–50. doi: 10.1097/JGP.0b013e31820ee9ef. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Abbott RB, Hui KK, Hays RD, Li MD, Pan T. A randomized controlled trial of tai chi for tension headaches. Evidence-based complementary and alternative medicine : eCAM. 2007;4(1):107–13. doi: 10.1093/ecam/nel050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Dechamps A, Diolez P, Thiaudiere E, Tulon A, Onifade C, Vuong T, Helmer C, Bourdel-Marchasson I. Effects of exercise programs to prevent decline in health-related quality of life in highly deconditioned institutionalized elderly persons: a randomized controlled trial. Archives of internal medicine. 2010;170(2):162–9. doi: 10.1001/archinternmed.2009.489. [DOI] [PubMed] [Google Scholar]
- 43.Li F, Harmer P, Fisher K, McAuley E, Chaumeton N, Eckstrom E, Wilson N. Tai Chi and fall reductions in older adults: a randomized controlled trial. J Gerontol A Biol Sci Med Sci. 2005;60(2):187–94. doi: 10.1093/gerona/60.2.187. [DOI] [PubMed] [Google Scholar]
- 44.Jones K, Sherman C, Mist S, Carson J, Bennett R, Li F. A randomized controlled trial of 8-form Tai chi improves symptoms and functional mobility in fibromyalgia patients. Clinical rheumatology. 2012;31(8):1205–14. doi: 10.1007/s10067-012-1996-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Shen C, Chyu M, Pence B, Yeh J, Zhang Y, Felton C, Xu K, Wang J. Green tea polyphenols supplementation and Tai Chi exercise for postmenopausal osteopenic women: safety and quality of life report. BMC Complem Alt Med. 2010;10:76. doi: 10.1186/1472-6882-10-76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Tsang T, Orr R, Lam P, Comino E, Singh MF. Effects of Tai Chi on glucose homeostasis and insulin sensitivity in older adults with type 2 diabetes: a randomised double-blind sham-exercise-controlled trial. Age and ageing. 2007 doi: 10.1093/ageing/afm127. [DOI] [PubMed] [Google Scholar]
- 47.Tsang T, Orr R, Lam P, Comino EJ, Singh MF. Health benefits of Tai Chi for older patients with type 2 diabetes: the "Move It For Diabetes study"--a randomized controlled trial. Clinical interventions in aging. 2007;2(3):429–39. [PMC free article] [PubMed] [Google Scholar]
- 48.Tsang TW, Kohn MR, Chow CM, Fiatarone Singh MA. Kung fu training improves physical fitness measures in overweight/obese adolescents: the “martial fitness” study. Journal of obesity. 2010;2010 doi: 10.1155/2010/672751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Wayne P, Kiel D, Buring J, Connors E, Bonato P, Yeh G, Cohen C, Mancinelli C, Davis R. Impact of Tai Chi exercise on multiple fracture-related risk factors in post-menopausal osteopenic women: a pilot pragmatic, randomized trial. BMC complementary and alternative medicine. 2012;12(1):7. doi: 10.1186/1472-6882-12-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Yeh G, Wood M, Lorell B, Stevenson L, Eisenberg D, Wayne P, Goldberger A, Davis R, Phillips R. Effects of tai chi mind-body movement therapy on functional status and exercise capacity in patients with chronic heart failure: a randomized controlled trial. Am J Med. 2004;117(8):541–8. doi: 10.1016/j.amjmed.2004.04.016. [DOI] [PubMed] [Google Scholar]
- 51.Yeh GY, Roberts DH, Wayne PM, Davis RB, Quilty MT, Phillips RS. Tai Chi Exercise for Patients With Chronic Obstructive Pulmonary Disease: A Pilot Study. Respiratory Care. 2010;55(11):1475–82. [PMC free article] [PubMed] [Google Scholar]
- 52.Yeh GY, McCarthy EP, Wayne PM, Stevenson LW, Wood MJ, Forman D, Davis RB, Phillips RS. Tai chi exercise in patients with chronic heart failure: a randomized clinical trial. Archives of internal medicine. 2011;171(8):750–7. doi: 10.1001/archinternmed.2011.150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Taylor D, Hale L, Schluter P, Waters DL, Binns EE, McCracken H, McPherson K, Wolf SL. Effectiveness of tai chi as a community-based falls prevention intervention: a randomized controlled trial. J Am Geriatr Soc. 2012;60(5):841–8. doi: 10.1111/j.1532-5415.2012.03928.x. [DOI] [PubMed] [Google Scholar]
- 54.Wang C, Schmid C, Hibberd P, Kalish R, Roubenoff R, Rones R, McAlinden T. Tai Chi is effective in treating knee osteoarthritis: a randomized controlled trial. Arthritis Rheum. 2009;61(11):1545–53. doi: 10.1002/art.24832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Wolf SL, Sattin RW, Kutner M, O'Grady M, Greenspan AI, Gregor RJ. Intense tai chi exercise training and fall occurrences in older, transitionally frail adults: a randomized, controlled trial. Journal of the American Geriatrics Society. 2003;51(12):1693–701. doi: 10.1046/j.1532-5415.2003.51552.x. [DOI] [PubMed] [Google Scholar]
- 56.Irwin MR, Olmstead R, Motivala SJ. Improving sleep quality in older adults with moderate sleep complaints: A randomized controlled trial of Tai Chi Chih. Sleep. 2008;31(7):1001–8. [PMC free article] [PubMed] [Google Scholar]
- 57.Deschamps A, Onifade C, Decamps A, Bourdel-Marchasson I. Health-related quality of life in frail institutionalized elderly: effects of a cognition-action intervention and Tai Chi. Journal of aging and physical activity. 2009;17(2):236–48. doi: 10.1123/japa.17.2.236. [DOI] [PubMed] [Google Scholar]
- 58.Li F, Harmer P, Fitzgerald K, Eckstrom E, Stock R, Galver J, Maddalozzo G, Batya SS. Tai chi and postural stability in patients with Parkinson's disease. The New England journal of medicine. 2012;366(6):511–9. doi: 10.1056/NEJMoa1107911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Sattin R, Easley K, Wolf S, Chen Y, Kutner M. Reduction in fear of falling through intense tai chi exercise training in older, transitionally frail adults. J Am Geriatr Soc. 2005;53(7):1168–78. doi: 10.1111/j.1532-5415.2005.53375.x. [DOI] [PubMed] [Google Scholar]
- 60.Barrow DE, Bedford A, Ives G, O'Toole L, Channer KS. An evaluation of the effects of Tai Chi Chuan and Chi Kung training in patients with symptomatic heart failure: a randomised controlled pilot study. Postgraduate medical journal. 2007;83(985):717–21. doi: 10.1136/pgmj.2007.061267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Caminiti G, Volterrani M, Marazzi G, Cerrito A, Massaro R, Arisi A, Franchini A, Sposato B, Rosano G. Tai chi enhances the effects of endurance training in the rehabilitation of elderly patients with chronic heart failure. Rehabilitation research and practice. 2011;2011:761958. doi: 10.1155/2011/761958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Hart J, Kanner H, Gilboa-Mayo R, Haroeh-Peer O, Rozenthul-Sorokin N, Eldar R. Tai Chi Chuan practice in community-dwelling persons after stroke. Int J Rehabil Res. 2004;27(4):303–4. doi: 10.1097/00004356-200412000-00008. [DOI] [PubMed] [Google Scholar]
- 63.Wang C. Tai Chi improves pain and functional status in adults with rheumatoid arthritis: results of a pilot single-blinded randomized controlled trial. Medicine and sport science. 2008;52:218–29. doi: 10.1159/000134302. [DOI] [PubMed] [Google Scholar]
- 64.Zhang Y, Fu FH. Effects of 14-week Tai Ji Quan exercise on metabolic control in women with type 2 diabetes. The American journal of Chinese medicine. 2008;36(4):647–54. doi: 10.1142/S0192415X08006119. [DOI] [PubMed] [Google Scholar]
- 65.Tsai PF, Chang JY, Beck C, Kuo YF, Keefe FJ. A Pilot Cluster-Randomized Trial of a 20-Week Tai Chi Program in Elders With Cognitive Impairment and Osteoarthritic Knee: Effects on Pain and Other Health Outcomes. Journal of pain and symptom management. 2012;45(4):660–9. doi: 10.1016/j.jpainsymman.2012.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Lam LC, Chau RC, Wong BM, Fung AW, Lui VW, Tam CC, Leung GT, Kwok TC, Chiu HF, Ng S, Chan WM. Interim follow-up of a randomized controlled trial comparing Chinese style mind body (Tai Chi) and stretching exercises on cognitive function in subjects at risk of progressive cognitive decline. International journal of geriatric psychiatry. 2011;26(7):733–40. doi: 10.1002/gps.2602. [DOI] [PubMed] [Google Scholar]
- 67.Shen CL, Chyu MC, Yeh JK, Zhang Y, Pence BC, Felton CK, Brismee JM, Arjmandi BH, Doctolero S, Wang JS. Effect of green tea and Tai Chi on bone health in postmenopausal osteopenic women: a 6-month randomized placebo-controlled trial. Osteoporosis international : a journal established as result of cooperation between the European Foundation for Osteoporosis and the National Osteoporosis Foundation of the USA. 2012;23(5):1541–52. doi: 10.1007/s00198-011-1731-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Wayne PM, Foster ML. The Harvard Medical School Guide to Tai Chi. United States of America: Shambhala Publications, Inc.; 2013. [Google Scholar]
- 69.Messier SP, Mihalko SL, Legault C, Miller GD, Nicklas BJ, DeVita P, Beavers DP, Hunter DJ, Lyles MF, Eckstein F, Williamson JD, Carr JJ, Guermazi A, Loeser RF. Effects of intensive diet and exercise on knee joint loads, inflammation, and clinical outcomes among overweight and obese adults with knee osteoarthritis: the IDEA randomized clinical trial. JAMA : the journal of the American Medical Association. 2013;310(12):1263–73. doi: 10.1001/jama.2013.277669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Morey MC, Snyder DC, Sloane R, Cohen HJ, Peterson B, Hartman TJ, Miller P, Mitchell DC, Demark-Wahnefried W. Effects of home-based diet and exercise on functional outcomes among older, overweight long-term cancer survivors: RENEW: a randomized controlled trial. JAMA : the journal of the American Medical Association. 2009;301(18):1883–91. doi: 10.1001/jama.2009.643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Cramer H, Lauche R, Hohmann C, Ludtke R, Haller H, Michalsen A, Langhorst J, Dobos G. Randomized-controlled trial comparing yoga and home-based exercise for chronic neck pain. The Clinical journal of pain. 2013;29(3):216–23. doi: 10.1097/AJP.0b013e318251026c. [DOI] [PubMed] [Google Scholar]
- 72.Sherman KJ, Cherkin DC, Wellman RD, Cook AJ, Hawkes RJ, Delaney K, Deyo RA. A randomized trial comparing yoga, stretching, and a self-care book for chronic low back pain. Archives of internal medicine. 2011;171(22):2019–26. doi: 10.1001/archinternmed.2011.524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Zetaruk MN, Violan MA, Zurakowski D, Micheli LJ. Injuries in martial arts: a comparison of five styles. British journal of sports medicine. 2005;39(1):29–33. doi: 10.1136/bjsm.2003.010322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Pieter W. Martial arts injuries. Medicine and sport science. 2005;48:59–73. doi: 10.1159/000084283. [DOI] [PubMed] [Google Scholar]
- 75.Kujala UM, Taimela S, Antti-Poika I, Orava S, Tuominen R, Myllynen P. Acute injuries in soccer, ice hockey, volleyball, basketball, judo, and karate: analysis of national registry data. BMJ (Clinical research ed) 1995;311(7018):1465–8. doi: 10.1136/bmj.311.7018.1465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Mao de W, Li J, Hong Y. Plantar pressure distribution during Tai Chi exercise. Arch Phys Med Rehabil. 2006;87(6):814–20. doi: 10.1016/j.apmr.2006.02.035. [DOI] [PubMed] [Google Scholar]
- 77.Mao DW, Hong Y, Li JX. Characteristics of foot movement in Tai Chi exercise. Phys Ther. 2006;86(2):215–22. [PubMed] [Google Scholar]
- 78.Wu G, Liu W, Hitt J, Millon D. Spatial, temporal and muscle action patterns of Tai Chi gait. Journal of electromyography and kinesiology : official journal of the International Society of Electrophysiological Kinesiology. 2004;14(3):343–54. doi: 10.1016/j.jelekin.2003.09.002. [DOI] [PubMed] [Google Scholar]
- 79.Mao DW, Li JX, Hong Y. The duration and plantar pressure distribution during one-leg stance in Tai Chi exercise. Clinical biomechanics (Bristol, Avon) 2006;21(6):640–5. doi: 10.1016/j.clinbiomech.2006.01.008. [DOI] [PubMed] [Google Scholar]
- 80.Chen HL, Liu K, You QS. Attention should be paid to preventing knee injury in tai chi exercise. Injury prevention : journal of the International Society for Child and Adolescent Injury Prevention. 2011;17(4):286–7. doi: 10.1136/injuryprev-2011-040027. [DOI] [PubMed] [Google Scholar]
- 81.Zhao SYZX, Qi WH. Reasons for Knee Joint Pain Caused by Yang's Shadowboxing. J Chin Clin Rehabil. 2005;9:182–3. [Google Scholar]
- 82.Foster B. Knee Problems and the Tai Chi Player. T'ai Chi The International Magazine of T'ai Chi Ch'uan. 2006:44–6. [Google Scholar]
- 83.Lam P. Safety First. [cited 2013 Nov 18];2013 Available from: URL: http://www.taichiforhealthinstitute.org/articles/individual_article.php?id=41.
- 84.Ng BY. Qigong-induced mental disorders: a review. The Australian and New Zealand journal of psychiatry. 1999;33(2):197–206. doi: 10.1046/j.1440-1614.1999.00536.x. [DOI] [PubMed] [Google Scholar]
- 85.Xu SH. Psychophysiological reactions associated with qigong therapy. Chinese medical journal. 1994;107(3):230–3. [PubMed] [Google Scholar]
- 86.Papanikolaou PN, Churchill R, Wahlbeck K, Ioannidis JP. Safety reporting in randomized trials of mental health interventions. The American journal of psychiatry. 2004;161(9):1692–7. doi: 10.1176/appi.ajp.161.9.1692. [DOI] [PubMed] [Google Scholar]
- 87.Ioannidis JP, Lau J. Completeness of safety reporting in randomized trials: an evaluation of 7 medical areas. JAMA : the journal of the American Medical Association. 2001;285(4):437–43. doi: 10.1001/jama.285.4.437. [DOI] [PubMed] [Google Scholar]
- 88.Carlesso LC, Macdermid JC, Santaguida LP. Standardization of adverse event terminology and reporting in orthopaedic physical therapy: application to the cervical spine. The Journal of orthopaedic and sports physical therapy. 2010;40(8):455–63. doi: 10.2519/jospt.2010.3229. [DOI] [PubMed] [Google Scholar]
- 89.Carlesso LC, Gross AR, Santaguida PL, Burnie S, Voth S, Sadi J. Adverse events associated with the use of cervical manipulation and mobilization for the treatment of neck pain in adults: a systematic review. Manual therapy. 2010;15(5):434–44. doi: 10.1016/j.math.2010.02.006. [DOI] [PubMed] [Google Scholar]
- 90.Giangregorio LM, Macintyre NJ, Thabane L, Skidmore CJ, Papaioannou A. Exercise for improving outcomes after osteoporotic vertebral fracture. The Cochrane database of systematic reviews. 2013;1:CD008618. doi: 10.1002/14651858.CD008618.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.MacPherson H, Thomas K, Walters S, Fitter M. A prospective survey of adverse events and treatment reactions following 34,000 consultations with professional acupuncturists. Acupuncture in medicine : journal of the British Medical Acupuncture Society. 2001;19(2):93–102. doi: 10.1136/aim.19.2.93. [DOI] [PubMed] [Google Scholar]
- 92.Ernst E, White AR. Prospective studies of the safety of acupuncture: a systematic review. Am J Med. 2001;110(6):481–5. doi: 10.1016/s0002-9343(01)00651-9. [DOI] [PubMed] [Google Scholar]