Abstract
Objective
Although multiple studies find that offspring of depressed mothers are at risk for depressive disorders, there is uncertainty about the specific mechanisms that are at work — particularly with respect to modifiable factors that might be targeted for early intervention. The present work examines parenting behaviors may operate as mediators, moderators, or independent influences on the development of youth depressive symptoms.
Methods
One hundred one mothers and their early adolescent children participated in positive and negative interaction tasks. Maternal and youth self-reports of youth depressive symptoms were collected at baseline, nine-month, and eighteen month assessments.
Results
Maternal history of depression was significantly associated with maternal-, but not youth self-reported depressive symptomatology. Maternal positive and negative interaction behaviors in positive contexts were associated with higher youth self-reported depressive symptoms. Maternal positive interaction behaviors in positive contexts and maternal negative interactive behaviors in conflict contexts were associated with higher youth self-reported depressive symptoms. We found no evidence for maternal interaction behaviors serving as a mediator and little evidence of maternal interaction behaviors serving as a moderator of the relationship between maternal and offspring depression.
Conclusions
Low maternal positive engagement tended to be more consistently associated with maternal- and self-reported youth depressive symptoms. The present findings suggest that characteristics of mother-child interactions that are associated with youth depressive symptomatology are pertinent to youth with and without a mother with a history of depression.
Keywords: risk trajectories, depression, adolescence, longitudinal study, parent-child interaction
Extensive data show that offspring of depressed parents are at risk for developing depressive disorders (Goodman, et al., 2011; Klein, Lewinsohn, Rohde, Seeley, & Olino, 2005; Lieb, Isensee, Hofler, Pfister, & Wittchen, 2002) and experiencing multiple adverse psychosocial outcomes (Beardslee, Gladstone, & O’Connor, 2011; Lewinsohn, Olino, & Klein, 2005). While conceptual models have proposed specific mechanisms accounting for the development of depression (e.g., Goodman & Gotlib, 1999), few have been explicitly tested. It has been argued that family interaction behaviors are involved in the development of depression among those at high-risk and are altered in families of depressed youth (Sheeber, Hops, Alpert, Davis, & Andrews, 1997; Sheeber, Hops, & Davis, 2001; Stein, et al., 2000). Here, we examine whether family interaction behaviors serve as mediators or moderators of the relationship between family risk-status and youth depressive symptoms or if family interaction behaviors and family risk-status have independent influences on youth depressive symptoms.
Goodman and Gotlib (1999) articulated a comprehensive conceptual model of mechanisms of risk for youth of depressed mothers. One proposed mechanism suggests that depressed mothers may engage in parenting practices, including affective and behavioral displays that may potentiate risk and these parenting behaviors increase risk for youth depression. Recent work has build support for the possibility that parenting behaviors mediate the relationship between parent and youth depression. A collection of studies have examined differences in parenting behaviors among depressed and healthy parents and another set of studies have examined associations between parenting behaviors and youth depressive symptoms. The former collection of studies have focused on interactions between parents and youth before the youth has experienced clinically significant levels of depression, which provides evidence that adverse parenting behaviors are present before the offspring develops depression. In addition, this prevents interpretations of reverse causality, such that youth depression causes changes in parenting style. A meta-analytic review of 46 observational studies found a small effect size for positive/supportive and a moderate effect size for negative behaviors between mothers with and without a history of depression (Lovejoy, Graczyk, O’Hare, & Neuman, 2000). This work identifies aspects of parenting that differs between depressed and non-depressed parents. More recently, McMakin et al. (2011) examined cross-sectional differences in seven dimensions of maternal behaviors among high- and low-risk parent-child dyads. Mothers and their children completed positive planning and conflict discussion tasks. Depressed mothers displayed lower levels of positive behaviors (e.g., positive affect, problem solving, validation) and higher levels of negative behaviors (e.g., negative affect, dominance, conflict, withdrawal) in positive contexts and lower levels of positive, but not higher levels of negative, behaviors in negative contexts. Thus, differences in negative interaction behaviors appeared to be somewhat context specific.
A number of studies have found cross-sectional associations between parenting and youth depression. A separate meta-analysis found that lower levels of parental warmth and higher levels of parental rejection, control, withdrawal, aversiveness, and over involvement were associated with child depression, with correlations ranging from .20-.33 (McLeod, Weisz, & Wood, 2007). Presence of increased negative interactive behaviors, including aggressive or punitive practices or criticism, may enhance conflict in the family, increase youth negative affectivity, and/or model negative cognitions for youth. Absence of positive interactive behaviors, including warm, accepting, and supportive parenting behavior, may provide contexts where youth are not reinforced for appropriate behavior or are encouraged to pursue goals. This work suggests a link between parenting and child depressive symptoms, with specific dimensions of parenting demonstrating different magnitude of associations with youth depression, which could be obfuscated in aggregate dimensions. Although there are meaningful associations, most of the included studies were cross-sectional and the authors did not report comparisons of effects between cross-sectional and prospective associations. One recent prospective study (Schwartz, et al., 2011) found that maternal dysphoria in response to adolescent aggression was associated with an increased rate of adolescent depressive disorder and suppression of aggression and dysphoria in response to adolescent dysphoria was associated with reduced rates of adolescent depressive disorder.
Taken together, these data provide modest support for one of the proposed mediation mechanisms by Goodman and Gotlib (1999). Ewell-Foster, Garber, and Durlak (2008) reported one of the few studies directly testing this model. The authors found that observed maternal positivity during a positively valenced interaction partially mediated the relationship between maternal depression, defined as either a lifetime history of depression or current symptoms, and child externalizing, but not internalizing problems. The failure to find parenting as a significant mediator for internalizing problems is counter to Goodman and Gotlib’s model. However, this could be due to a number of methodological design characteristics, including relying on a cross-sectional design and focusing solely on a positive interaction task. Additional research, particularly with longitudinal designs, is needed to test the possibility that parenting behaviors mediate the relationship between parent and child depressive symptoms.
Alternatively, the results of Ewell-Foster, Garber, and Durlak (2008) may suggest different conceptual models for examining the relationship between parent and child depression. It is plausible that parenting behaviors may moderate the relationship between parental and youth depression, which would be consistent with a diathesis-stress model. Parental depression may transmit an affective (Durbin, Klein, Hayden, Buckley, & Moerk, 2005) or cognitive (Kujawa, et al., 2011) vulnerability to their offspring (i.e., diathesis) and parental behaviors may serve as an environmental context (i.e., stress) that exacerbates or attenuates the influence of parental depression on offspring. Lastly, parenting behaviors may demonstrate significant associations with child depression that are independent of the effects of parental depression (i.e., unique effects). Lovejoy et al. (2000) suggested that this was a likely possibility, as parenting behaviors accounted for only a modest proportion of variance in youth depressive symptoms.
The Present Study
The present study builds on the cross-sectional comparisons presented by McMakin et al. (2011) and examines processes through which affective parenting behaviors and parental history of depression are associated with the development of youth depressive symptoms over the course of 18 months. As data suggest that the influence of maternal depressive disorder may be stronger than the influences of paternal depression (Connell & Goodman, 2002), we focus on maternal depression and parenting behaviors. We focus on parenting behaviors as youth enter the peak period of risk for depressive disorders (Lewinsohn, Hops, Roberts, Seeley, & Andrews, 1993). Further, rather than relying on a single context to examine mother-child interactions, we assess interactions during positive and negative situations. Most previous studies have compared maternal behaviors during conflict tasks with their children and only some examined positive tasks. As negative contexts are primed for negative affect, the ability to assess variability in positive affect may be limited. In addition, the meaning of behaviors may be more salient when displayed in a congruent or incongruent context. For example, the presence of negative behaviors in a positive context may convey greater risk than negative behaviors in a negative context because, despite being primed for pleasant affect, the behaviors may be more salient and model maladaptive functioning. This is consistent with our previous finding (McMakin et al., 2011) that higher levels of maternal negative interaction behaviors in positive, but not negative, contexts for mothers with a history of depression relative to never depressed mothers. Thus, we explore whether behaviors in negative or positive contexts predict youth depressive symptoms, which was not examined in our previous report. In addition, we consider the utility of both maternal- and self-reports of youth depression symptomatology. Previous work finds that associations between parental and youth depression is stronger when relying on parental reports of youth symptoms (Connell & Goodman, 2002); thus, we anticipate finding a similar pattern of results. Lastly, we examine prospective relationships between maternal depression and interaction behaviors and youth depressive symptoms using a short-term longitudinal design.
As there are compelling conceptual arguments for the role of maternal parenting behaviors mediating the relationship between maternal and child depression and this is supported by empirical work (Lovejoy et al., 2000; McLeod et al., 2007), we anticipate finding support for maternal behavior to partially mediate the relationship between maternal and child depression. However, we also explored interactions between maternal depression and maternal behaviors will be identified, such that for youth of mothers with a history of depression, higher levels of negative and/or lower levels of positive maternal behaviors will be associated with additional elevations in youth depressive symptoms.
Method
Participants
One-hundred and one youth (43 male, 58 female) participated in this study with their biological mothers. At the initial assessment, youth ranged in age from 9 to 14 (M = 11.51, SD = 1.72) and mothers ranged in age from 29 to 55 (M = 42.34, SD = 5.93). Forty-seven youth were offspring of depressed mothers who experienced an episode of Major Depressive Disorder (MDD) within the past two years (High-Risk; HR) and 54 youth were offspring of mothers with no lifetime history of psychiatric disorder (Low-Risk; LR). All HR mothers were required to meet DSM-IV criteria (APA, 1994) for chronic (lasting more than 1 year) or recurrent (minimum of two episodes) MDD, with the most recent episode occurring within two years. Two mothers experienced lifetime dysthymic disorder in addition to meeting lifetime criteria for MDD. Additional exclusion criteria for mothers in the HR group were any history of mania or obsessive-compulsive disorder, psychotic disorder, current substance abuse, or systemic medical illness.
Due to other study procedures (e.g., fMRI, pupilometry), offspring were excluded from the study if they had vision problems not corrected by glasses or contact lenses, motor or other neurological problems, major medical disorders, or were taking psychotropic medications. LR offspring were excluded if they met DSM-IV criteria for any current or past Axis I diagnoses and HR offspring were excluded if they met criteria for a current or past diagnosis of depression, obsessive-compulsive disorder, post-traumatic stress disorder, substance abuse, developmental disorder, or psychotic disorder. HR offspring were included in the study if they had a comorbid anxiety disorder (N = 5) or behavior disorder (N = 5). All analyses were repeated when excluding youth with anxiety and/or behavior disorders and conclusions were identical. HR and LR groups did not differ in race, mother’s education, child age, or child gender.
Procedure
Participants were recruited from the general community in the Pittsburgh area through flyers, newspaper/radio advertisements, and a university-sponsored telephone recruitment service. HR families were also recruited from outpatient clinics at the university hospital. Interested families completed a 15-minute telephone screen to assess maternal and child psychiatric symptomatology and other inclusion and exclusion criteria. A total of 608 families completed a telephone screen, and 420 dyads were screened out based on their responses to the telephone screen. The remaining 188 dyads were invited to the lab to complete diagnostic interviews to confirm parent and child DSM-IV diagnoses. Following these procedures, 103 dyads met full criteria and were enrolled in the study. After obtaining parent consent and child assent, parent-child dyads completed a battery of questionnaires and participated in a series of tasks, including behavioral observation of parent-child interaction. Two dyads did not complete the observation tasks due to technical problems, leading to a final sample of 101.
Instruments
Structured Clinical Interview for DSM-IV (SCID)
The SCID (First & Gibbon, 2004) is a clinician administered interview assessing lifetime and current psychiatric disorders among mothers. The SCID was administered by trained interviewers. Inter-rater reliability for affective and anxiety disorder diagnoses was calculated for a random sample of 18% of interviews and yielded no disagreements (kappa = 1.0).
Schedule for Affective Disorders and Schizophrenia in School-Age Children— Present and Lifetime version (K-SADS-PL)
The KSADS-PL (Kaufman, et al., 1997) assesses lifetime and current psychiatric disorders among youth. Parents and youth were interviewed separately, with trained interviewers integrating data from both to arrive at a final diagnosis. Inter-rater reliability for affective and anxiety disorder diagnoses was calculated for a random sample of 27% of interviews and yielded no disagreements (kappa = 1.0).
Demographics
A demographics questionnaire was used to assess child and parent age, gender, race, and education at baseline.
Child Depressive Inventory
(CDI; Kovacs, 1992). Youth and their mothers independently reported on child depressive symptoms using the CDI in person for the baseline and 18-month assessment. Youth and their mothers independently completed the 9-month assessment over the phone with a trained research assistant. Across all assessments, child- and parent-reported CDI scores were associated (r = .41, p < .01).
Beck Depression Inventory
(BDI; Beck, Steer, & Brown, 1996). Mothers completed the BDI at the time of the baseline, 9-month, and 18-month assessments. The BDI is a widely-used psychometrically sound instrument to assess depression in adults.
Dyadic interactions
Conflict Task
Dyads completed a “hot topics” task designed to elicit conflict and negative emotion (Hetherington & Clingempeel, 1992). First, mothers and youth completed a checklist of common areas of conflict among youth-parent dyads. Dyads were asked to discuss the conflict rated most highly by both members of the dyad during an eight minute videotaped discussion. They were given a card with the conflict listed and asked to address the following points: (1) how recent disagreements started (2) who else was involved (3) how the issue ended, and (4) how the dyad would deal with the issue in the future. The discussion points were included to help dyads that could not think of anything to say.
Plan a Fun Activity Task
Following the conflict task, dyads were asked to jointly plan a fun activity that they could do together in the next week (Hollenstein, Granic, Stoolmiller, & Snyder, 2004). This task was designed to elicit mutual positive affect. Dyads were instructed to choose something that they would both enjoy and plan it in as much detail as possible. The dyad was filmed for 5 minutes while planning the activity. Youth and mothers completed the interactions in a fixed order with the Conflict Task first and the Plan a Fun Activity Task second in order to have dyads return to a more positive state before leaving the session.
Interactional Dimensions Coding System-Revised (IDCS-R)
Interactions were coded using the IDCS-R, which is a macro-analytic observational coding system originally designed to assess couples’ interactions (Julien, Markman, & Lindahl, 1989), and modified for adolescents (Furman & Shomaker, 2008). Trained coders rate observable behavior, facial expressions, and verbal content of interactions for both participants. Here we focus exclusively on maternal behaviors. Mothers are rated on a five-point Likert scale with half-point intervals (1 extremely uncharacteristic to 5 extremely characteristic) for individual affective behaviors. As the present study builds on the cross-sectional work in McMakin et al. (2011), we relied on the same observational codes: Positive Affect, Problem Solving, Support/Validation, Negative Affect, Dominance, Conflict, and Withdrawal. Each code was rated separately in each context. To minimize halo effects, the two contexts were never coded during the same coding session for the same participants. Tasks were randomly assigned to trained coders who were naïve to participant information. Inter-rater agreement was checked on 23% of interactions (for each of three coders relative to the “reliability coder”). Intra-class correlation coefficients for the 10 codes ranged from .71 to .90 (mean = .79; SD = .05).
Rather than rely on individual behavior codes within each context, aggregate scales were computed based on positively and negatively valenced interaction behaviors. A positive interaction behavior construct was computed based on Positive Affect, Problem Solving, Support/Validation, and Withdrawal (reversed) and a negative interaction behavior construct was computed based on the average of Negative Affect, Dominance, and Conflict. The positive and negative aggregates demonstrated good internal consistency in the positive context (αs = .85 and .76, respectively) and the negative context (αs = .85 and .86, respectively).
Data analytic plan
Trajectories of maternal- and self-reported youth depressive symptoms were modeled using Mplus 7.2 (AACAP, 1998). The TWOLEVEL and RANDOM options were used to estimate growth models for youth self- and maternal-reports of youth depression using multilevel models and the MLR estimator was used to compute robust standard errors. Time was centered such that the intercept (i.e., time = 0) was at the 18-month assessment and time of previous assessments was computed in months. This permitted estimating the influence of covariates on depressive symptoms at the last available time (i.e., assessing longitudinal prediction, as opposed to cross-sectional associations) and preserved temporal sequencing of our variables for our mediation analyses.
Unconditional growth models estimate trajectories using intercept and slope parameters with their respective mean and variance estimates. The intercept is the estimated level of the outcome variable at an identified location of the growth trajectory (here, at the 18-month follow-up). The variance estimate of the intercept reflects whether there is significant variation in the outcome variable at the last assessment. The mean value of the slope is the estimated average rate of change over time. The variance estimate of the slope parameter reflects whether significant variation exists in the rate of change in the outcome variable. Thus, this modeling approach examines variability in the outcome at the intercept value and longitudinal variability in the outcome for the slope. Based on observed means of parent- and youth self-reported youth depressive symptoms, we also included a quadratic slope in the model. After identifying the best fitting unconditional model, we examined predictors of intercept and/or slope only when those parameters had significant variance (Raudenbush & Bryk, 2002).
Tests of mediation, when indicated, were implemented using the MODEL CONSTRAINT command in Mplus. This option computed specified indirect effects, including regression weights and standard errors. Tests of moderation followed recommendations by Aiken and West (1991). Continuous predictors were centered before computing the interaction term.
Results
Table 1 displays intercorrelations among child characteristics, maternal depression status, and maternal interaction behaviors. Maternal depression is associated with lower levels of positive and higher levels of negative interaction behaviors in both positive and conflict contexts.
Table 1.
Correlation matrix among all predictor variables
| Positive Context | Negative Context | |||||||
|---|---|---|---|---|---|---|---|---|
| Child Age | Child Sex | Maternal Depression |
Positive Behaviors |
Negative Behaviors |
Positive Behaviors |
Negative Behaviors |
||
| Child Age | -- | |||||||
| Child Sex | .07 | -- | ||||||
| Maternal Depression |
−.14 | −.04 | -- | |||||
| Positive Context | Positive Behaviors |
−.27** | .01 | −.34** | -- | |||
| Negative Behaviors |
.20* | .05 | .32** | −.50** | -- | |||
| Negative Context | Positive Behaviors |
−.15 | .12 | −.27** | .65** | −.48** | -- | |
| Negative Behaviors |
.17 | −.02 | .15 | −.44** | .52** | −.71** | -- | |
p < .05
p < .01
Age = child age; sex = child sex; Mat. Dep. = Maternal history of chronic/recurrent depressive disorder; Positive Context = maternal behaviors assessed during the planning a fun activity discussion; Negative Context = maternal behaviors assessed during the hot topics discussion.
Unconditional Model Fit
Initial models examined included fixed and random effects for the intercept, linear slope, and quadratic slope for maternal-report of youth symptoms. However, this model would not converge. The model was re-estimated removing the random effect for the quadratic slope. This model converged and found a non-significant random effect for the linear slope. Thus, the model was again re-estimated with fixed effects for the intercept, linear slope, and quadratic slope and a random effect for the intercept. The final model found that the parent-reported CDI score differed significantly from 0 (B00 = 8.50, SE = .68, p < .001) and had significant variance (t = 4.60, p < .001) and there were significant effects of the linear and quadratic slopes (B10 = −.26, SE = .12, p < .05; B20 = −.02, SE = .01, p < .05). However, the variance estimate for the linear slope parameter was non-significant. Although negative slope coefficients were identified, the overall growth pattern for depressive symptoms was generally increasing. Based on this model, the data find individual differences in depressive symptoms 18 months after the initial assessment; however, the rate of change in symptoms was similar across all youth.
Similar model fitting procedures were implemented for youth self-reported symptoms. The initial models included fixed and random effects for the intercept, linear slope, and quadratic slope. This model converged. The intercept, linear slope, and quadratic slope all differed significantly from zero and the variance of the intercept differed from zero. However, the variance estimates for the linear and quadratic slope parameters were non-significant. Thus, the models were re-estimated removing these random effects. The resulting model found that the youth self-reported CDI score differed significantly from 0 (B00 = 5.07, SE = .54, p < .001) and had significant variance (t = 4.63, p < .001) and there were significant effects of the linear and quadratic slopes (B10 = .25, SE = .12, p < .05; B20 = .01, SE = .004, p < .05). Thus, both linear and quadratic changes for child self-report were both significant and positive.
Conditional Models
We estimated the influence of child age and sex, maternal history of depressive disorder, and observational ratings of maternal behavior on maternal- and youth-rated depressive symptoms separately at the time of the 18 month follow-up. For maternal reported youth symptoms, analyses (Table 2) found that HR youth demonstrated more depressive symptoms than LR youth. Across both contexts, lower levels of maternal positive and higher levels of negative interactive behaviors were associated with higher level of depressive symptoms.
Table 2.
Influence of Maternal Behaviors on Parent-reported Youth Depressive Symptoms 18-months After Baseline
| Univariate Model | Partly Adjusted Model | Fully Adjusted Model | |||||||
|---|---|---|---|---|---|---|---|---|---|
| B | SE | t | B | SE | t | B | SE | t | |
| Child Age | 0.05 | 0.33 | 0.16 | ||||||
| Child Sex (female) | −1.43 | 1.16 | M.24 | ||||||
| Maternal Depression | 4.56 | 1.05 | 4.34** | 4.66 | 1.02 | 4.57*** | |||
|
| |||||||||
| Positive Context | |||||||||
| Positive | −3.65 | 1.06 | −3.43** | −3.79 | 1.12 | −3.37** | −2.33 | 1.03 | −2.56* |
| Negative | 3.27 | 1.24 | 2.65** | 3.40 | 1.29 | 2.63** | 1.83 | 1.22 | 1.50 |
|
| |||||||||
| Conflict Context | |||||||||
| Positive | −2.64 | .78 | −3.39** | −2.54 | .83 | −3.05** | −1.34 | .79 | −1.70 |
| Negative | 2.24 | .89 | 2.50* | 2.22 | .94 | 2.39* | 1.64 | .76 | 2.15* |
p < .05
p < .01
p < .001
Models estimate associations between covariates, maternal history of depression (Risk Status), and maternal behaviors in the context of the growth models using the intercept (at the 18-month follow-up) as the dependent variable. Univariate Models include only one predictor variable at a time. Partly Adjusted Models include one focal predictor per model and adjusts for child age and sex. Fully Adjusted Models include one parenting behavior per model and adjusts for child age and sex and maternal history of depression.
Parallel analyses were conducted for self-reports of youth depression. As reported by youth (Table 3), lower levels of maternal positive interactive behaviors in both contexts were associated with higher level of depressive symptoms. Maternal negative interaction behaviors and risk-status were not associated with self-reported youth symptoms.
Table 3.
Influence of Maternal Behaviors on Youth Self-reported Depressive Symptoms 18-months After Baseline
| Univariate Model | Partly Adjusted Model | Fully Adjusted Model | |||||||
|---|---|---|---|---|---|---|---|---|---|
| B | SE | t | B | SE | t | B | SE | t | |
| Child Age | 0.20 | 0.24 | 0.84 | ||||||
| Child Sex (female) | 0.20 | 0.92 | 0.21 | ||||||
| Maternal Depression | 1.30 | 0.89 | 1.46 | 1.45 | .87 | 1.67 | |||
|
| |||||||||
| Positive Context | |||||||||
| Positive | −2.34 | .78 | −2.99** | −2.30 | .83 | −2.76** | −2.02 | .85 | −2.68* |
| Negative | 2.77 | .97 | 2.86** | 2.69 | 1.03 | 2.62** | 2.45 | 1.04 | 2.36* |
|
| |||||||||
| Conflict Context | |||||||||
| Positive | −1.59 | .72 | −2.21* | −1.58 | .71 | −2.21* | −1.28 | .79 | −1.63 |
| Negative | 1.44 | .80 | 1.80 | 1.39 | .80 | 1.74 | 1.23 | .81 | 1.51 |
p < .05
p < .01
p < .001
Models estimate associations between covariates, maternal history of depression (Risk Status), and maternal behaviors in the context of the growth models using the intercept (at the 18-month follow-up) as the dependent variable. Univariate Models include only one predictor variable at a time. Partly Adjusted Models include one focal predictor per model and adjusts for child age and sex. Fully Adjusted Models include one parenting behavior per model and adjusts for child age and sex and maternal history of depression.
In our next set of conditional models, we estimated the influence of risk-status and maternal observational ratings on depressive symptoms at the time of the 18 month follow-up after adjusting for child age and sex. For maternal reported youth depressive symptoms, analyses (Table 2) found that, across both contexts, lower levels of maternal positive and higher levels of negative interactive behaviors were associated with higher level of depressive symptoms. As reported by youth, lower levels of maternal positive interactive behaviors in both contexts were associated with higher level of depressive symptoms.
Next, we estimated the influence of maternal observational ratings on depressive symptoms at the time of the 18 month follow-up after adjusting for risk-status, in addition to child age and sex. In all models examining maternal ratings of symptoms, risk-status was a significant predictor, such that high-risk youth demonstrated more depressive symptoms at the 18 month follow-up than low-risk youth. According to maternal reports of youth depressive symptoms, lower levels of maternal positive interaction behaviors in positive contexts and higher levels of negative interactive behaviors in conflict contexts were associated with higher level of depressive symptoms. According to youth reports of depressive symptoms, lower levels of maternal positive interaction behaviors and higher levels of negative interactive behaviors were associated with higher levels of youth reported symptoms.
Finally, we estimated a final set of models for maternal reported youth symptoms to examine whether state-related biases (e.g., maternal depressive state influencing ratings of youth symptoms; De Los Reyes & Kazdin, 2005) were influencing the observed associations. When maternal BDI at each assessment was entered into the models as a time-varying covariate, both maternal history of depression and BDI each predicted youth depressive symptoms. However, maternal negative interaction behaviors during the conflict context were no longer significantly associated with maternal reported youth symptoms and maternal positive interaction behaviors during the positive context were associated with maternal reported youth symptoms at a trend (B = −1.82, SE = .96, t = −1.86, p = .058). Similarly, maternal negative interaction behaviors during the positive context were no longer significantly associated with youth self-reported depression symptoms. However, maternal positive interaction behaviors during the positive context continued to be associated with youth self-reported depression symptoms (B = −1.71, SE = .81, t = −2.10, p < .05).
Tests of Mediation
Our previous analyses demonstrated that youth of depressed mothers demonstrated higher levels of depressive symptoms when assessed via maternal reports. This indicates a direct effect of risk status on youth symptoms. However, since no group differences were found on youth self-reports of depressive symptoms, we did not pursue tests of mediation for this outcome. Maternal depression was associated with lower positive interaction behaviors in both positive and conflict contexts and higher levels of negative interaction behaviors in positive contexts. Finally, lower maternal positive interaction behaviors in positive context and higher negative interaction behaviors in negative context were associated with higher levels of maternal reported youth depressive symptoms. Across this information, it is plausible that the relationship between maternal depression and maternal reports of youth depression may be mediated by maternal positive interaction behaviors in positive context. However, this indirect was not conventionally significant (B = .75, SE = .40, t = 1.86, p = .06).
Tests of Moderation
Finally, we explored whether the relationships between maternal and child depression were moderated by maternal behavior. These models predicted depressive symptoms at the 18-month follow-up within the growth model framework. These models adjusted for child sex and age and included main effects for risk-status and individual observational ratings and individual interaction terms. Based on maternal reports of symptoms, we found that no interactions were significant (or even approached significance; all ps > .53).
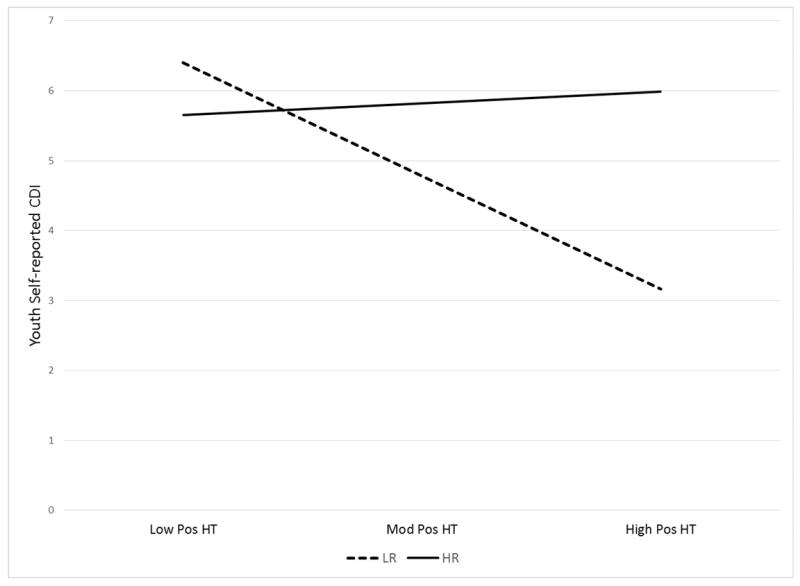
Using youth reports of symptoms, risk-status significantly interacted with maternal positive interaction behavior in negative contexts (B = 3.47, SE = 1.54, p < .05) to predict youth symptoms. Post-hoc analyses found that among youth of mothers without a history of maternal depression, maternal positive interaction behavior in negative contexts was negatively associated with youth reports of depressive symptoms (B = −3.15, SE = 1.20, p < .01). However, among youth of mothers with a history of maternal depression, maternal Positive Affect in both positive and negative contexts was not associated with youth reports of depressive symptoms (B = .32, SE = 93, p = .73). Figure 1 displays the interaction. Although there was no main effect of maternal depression, high-risk youth tended to display higher levels of depressive symptoms and levels of symptoms were unrelated to maternal interactive behaviors. Moderation models were estimated for maternal- and self-reports of depressive symptoms when including maternal BDI as a time-varying covariate. Previously identified interaction effects continued to be significantly associated with maternal- and self-reports of depressive symptoms.
Figure 1.
Maternal interaction behavior X risk status interaction. The x-axis is maternal positive interaction behaviors at low (one standard deviation below the mean), moderate (at the mean), and high (one standard deviation above the mean) levels. HR = high-risk youth; LR = low-risk youth; CDI = Child Depressive Inventory; x-axis: low, moderate, and high maternal positive behaviors during the Hot Topic discussion.
Discussion
Previous work has conceptualized maternal behavior during interactions with their children as potential mediators of the relationship between maternal and child depression (Goodman & Gotlib, 1999). However, much of the empirical literature has relied on cross-sectional methods to examine this possibility (e.g., Dietz, et al., 2008; Ewell-Foster et al., 2008), which limit tests of mediation. Moreover, fewer studies have considered alternative models of the relationship between maternal depression and parenting behaviors for youth depressive symptoms. These alternative possibilities include independent effects or that maternal behaviors may moderate the relationship between maternal and child depression. The present study examined these possibilities in a short-term longitudinal study and examined both maternal- and self-reports of youth depressive symptoms. Overall, the data provided modest support for maternal interaction behaviors mediating or moderating the relationship between maternal and offspring depression. However, the general pattern of results were consistent with past work. Low levels of positive maternal interaction behaviors and high levels of negative interaction behaviors were associated with higher levels of youth symptoms. These results are qualified by specific informants and contexts.
Analyses that relied on maternal- and self-reports of youth depressive symptoms provided some conflicting results. Most strikingly, maternal history of depression was associated with maternal-reports, but not youth self-reports, of youth depressive symptoms. This is fully consistent with past meta-analytic work (Goodman et al., 2011) showing that the associations between parental and offspring psychopathology are stronger when offspring psychopathology is assessed by parent-reports. A plausible explanation would center on informant effects, such that depressed mothers have biases towards over reporting symptoms in their children. However, it is also possible that depressed mothers can identify more subtle signs that their children are displaying emerging, lower levels of depression.
In addition to the relationship between maternal depression and youth symptoms varying as a function of informant of youth symptoms, associations between maternal interaction behaviors and youth symptoms also varied according to context. For both maternal- and youth self-reports, in the positive context, low maternal positive interaction behaviors were associated with higher levels of youth symptoms. However, greater heterogeneity was found for the relationships between maternal negative interaction behaviors and youth symptoms. Maternal negative interaction behaviors in positive contexts were associated with youth-reported symptoms whereas maternal negative interaction behaviors in negative contexts were associated with maternal-reported symptoms. Of particular interest to the present study was that youth self-reported depressive symptoms were associated with maternal interactive behaviors during the positive, but not negative context. This suggests that youth may be more sensitive to the influence of maternal behaviors during positive contexts than negative contexts. In contrast, the maternal-reported youth symptoms were associated with maternal positive behaviors during the positive and negative behaviors during the conflict context. This suggests that maternal reports of youth symptoms are associated with maternal behaviors consistent with the context. These may be important methodological details to note for the planning of future studies. Historically, much attention was paid to increased criticism observed in depressed parents particularly in negative contexts, which limits our ability to determine if our findings are fully consistent with past data.
Theoretical arguments suggest that maternal behavior may mediate the relationship between maternal and child depression (Goodman & Gotlib, 1999). Recent meta-analytic work suggests the plausibility of such a framework (Goodman & Gotlib, 1999; Lovejoy et al., 2000; McLeod et al., 2007). Maternal history of depression was associated with maternal-reports of youth symptoms. Thus, we examined maternal interaction behaviors as mediators of the relationship between maternal and offspring depression. However, consistent with Ewell-Foster et al. (2008), we did not find found a single significant indirect effect of the relationship between maternal depression and maternal report of youth depressive symptoms through maternal interaction behaviors. Perhaps, like Ewell-Foster et al. (2008), there may have been evidence for maternal interaction behaviors mediating the relationship between maternal depression and youth externalizing problems. However, measures of externalizing problems were not examined.
There is a substantial literature indicating that youth of depressed parents are at risk for developing depressive disorders and increases in symptoms and rates of disorders are beginning to be seen in the early adolescent years. However, differences between the high- and low-risk youth were not found on self-reports of youth depressive symptoms. There are several potential explanations for this null result. First, the youth were entering adolescence and the period of risk for depression. The short-term longitudinal follow-up may have been too short to observe increases in symptoms. Second, perhaps the youth self-reported CDI items assess depressive symptoms at a higher level of severity and are insensitive to variation in symptoms at lower severity (Olino, et al., 2012). Further work is needed to evaluate this possibility. Third, although self-reported symptoms did not differentiate between high- and low-risk youth, there may be alternative domains of functioning that are of value, such as neuroticism, stress reactivity, extraversion, or reward seeking/sensitivity (Klein, Kujawa, Black, & Pennock, 2013). Fourth, consistent with current research recommendations, markers of risk may need to be evaluated in other units of analysis, besides self-report. Markers of risk, and developmental changes in risk-related mechanisms, may need to be evaluated using behavioral or neurobiological methods (Patrick, et al., 2013). Thus, additional content would need to be evaluated to determine if other markers of risk may be identified.
We also tested moderation models (i.e., diathesis-stress models), such that maternal history of depression conveys some vulnerability to youth and parenting behaviors act as an environmental stressor to exacerbate risk. Of the eight tests of moderation conducted, we found one significant interaction. Thus, we cautiously interpret this result as a Type I error is possible. Interestingly, the maternal interaction behaviors that moderated the influence of maternal depression on youth depression involved maternal positive interaction behaviors in negative contexts. This interaction found that lower levels of positive maternal behaviors were associated with higher levels of self-reported symptoms among low-risk youth. That is, absence of PA predicted higher levels of depressive symptoms, which is consistent with meta-analytic findings for warmth (McLeod, Weisz, & Wood, 2007). However, these results also suggested that high-risk youth were insensitive to the benefits of experiencing maternal positive behaviors during interactions. Thus, protective effects of positive maternal behaviors during conflict were absent. This pattern stood in contrast to the expected pattern by which absence of positive interaction behaviors would be associated with higher levels of youth symptoms, but the relationship would be particularly strong for high-risk youth.
Finally, we also examined the possibility that maternal history and maternal interaction behaviors have independent influences on youth depressive symptoms. Again, maternal depression was associated with maternal-report, but not self-report of youth depressive symptoms. Most specifically, findings were strongest when considering associations between maternal behaviors in positive contexts when maternal-report of youth depression was examined. As the influence of parenting was no longer associated with maternal reported youth symptoms when state severity of maternal depression was included in the analyses, it is quite possible that maternal reports of youth depression may be biased by their own mood states (De Los Reyes & Kazdin, 2005). Alternatively, youth symptoms may be temporally linked with maternal symptoms (Weissman, et al., 2006), such that there are meaningful associations between mother and offspring depression that are dynamic in nature and account for the association between maternal diagnostic history and offspring state depression.
Consistent with previous work, we found increases in youth-report of depressive symptoms over time. For both maternal and youth reports, model estimation demonstrated the need for a quadratic growth term. However, we cannot be sure whether this result represented a methodological effect of in-person parent-report versus administration over the phone in an interview format or true quadratic changes in depressive symptoms observed in the sample.
In addition, our analytic approach and longitudinal design made it possible to examine the development of symptoms over 18 months. Our results indicate that rate of change of depressive symptoms was similar for all youth included in the study, regardless of risk status. Previous work has found individual differences in rate of change in symptoms (Garber & Cole, 2010; Garber, Keiley, & Martin, 2002; Ge, Lorenz, Conger, Elder, & Simons, 1994). However, these studies have included more youth and over a longer time interval of measurement. These methodological qualities are important to consider when planning future work.
The study had a number of merits, including assessing youth depressive symptoms over time from both mothers and youth, examining prospective relationships between maternal parenting behaviors and youth depressive symptoms, using multiple observational contexts to assess maternal interaction behaviors, and testing competing models of development of depressive symptoms in youth. However, the study should also be considered in light of a number of limitations. First, we focused on maternal behaviors without consideration of how child behaviors may exert an influence on maternal behaviors. An important future direction is to examine micro-analytic dyadic processes that may lead to understanding the ways through which youth influence their experience of interacting with their parents. Second, our global coding system provided an index of broad domains of interactive behaviors. Further work relying on micro-analytic coding may be fruitful in identifying specific targets for prevention efforts (e.g., contingent behaviors). Third, we only considered maternal history of depression and maternal interaction behaviors. Future work would benefit from including data on paternal psychopathology and interaction behaviors (Phares, 1992; Phares & Compas, 1992) as they have been hypothesized to be moderators (Goodman & Gotlib, 1999) of the relationship between maternal and youth depression. Fourth, despite sampling a reasonably large sample of youth and assessing them on three occasions across 18-months, we did not find significant variability in rates of change in depressive symptoms. Thus, we could not address how parental behaviors may have predicted change in symptoms. Future studies with larger samples of youth with a more limited age range may enhance the ability of a study to detect individual differences in rates of symptom increases. Nonetheless, these data are suggestive that the associations found here are consistent over time. Fifth, the order of the observational tasks was not counterbalanced. Thus, we cannot determine whether carryover influences from one task to the other are present and if these have implications for the findings.
The current study provides important new information for understanding the mechanisms by which maternal depression is associated with the development of adolescent depression. By testing competing models of this association, the study contributes to the conceptualization of the effects of maternal depression and points to future directions for developmental psychopathology research. Limited support was found for these complex relationships. However, with some nuance, there was general support for recommending clinical interventions with goals of mothers increasing positive interaction behaviors and reducing negative interaction behaviors. These results also offer important information for forming hypotheses about expected results from studies relying on youth and maternal reports of youth depressive symptoms and contexts in which mother-child interactions are assessed.
Acknowledgments
This work was supported by K01 MH073077 (PI: Silk), K01 MH092603 (PI: Olino), and K23 MH092400 (PI: McMakin).
Contributor Information
Thomas M. Olino, University of Pittsburgh School of Medicine Pittsburg, PA
Dana L. McMakin, University of Pittsburgh School of Medicine Pittsburg, PA
Terri A. Nicely, University of Pittsburgh School of Medicine Pittsburg, PA
Erika E. Forbes, University of Pittsburgh School of Medicine Pittsburg, PA
Ronald E. Dahl, University of California at Berkeley, Berkeley, CA
Jennifer S. Silk, University of Pittsburgh School of Medicine Pittsburgh, PA
References
- AACAP Practice Parameters for the Assessment and Treatment of Children and Adolescents With Obsessive-Compulsive Disorder. Journal of the American Academy of Child & Adolescent Psychiatry. 1998;37:27S–45S. doi: 10.1097/00004583-199810001-00003. [DOI] [PubMed] [Google Scholar]
- Aiken LS, West SG. Multiple regression: Testing and interpreting interactions. Sage Publications, Inc.; 1991. [Google Scholar]
- American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders. 4th edition. Author; Washington, DC: 1994. rev. [Google Scholar]
- Beardslee WR, Gladstone TR, O’Connor EE. Transmission and prevention of mood disorders among children of affectively ill parents: A review. Journal of the American Academy of Child & Adolescent Psychiatry. 2011;50:1098–1109. doi: 10.1016/j.jaac.2011.07.020. [DOI] [PubMed] [Google Scholar]
- Beck A, Steer R, Brown G. Manual for beck depression inventory II (BDI-II) Psychology Corporation; San Antonio, TX: 1996. [Google Scholar]
- Connell AM, Goodman SH. The association between psychopathology in fathers versus mothers and children’s internalizing and externalizing behavior problems: A meta-analysis. Psychological Bulletin. 2002;128:746–773. doi: 10.1037/0033-2909.128.5.746. [DOI] [PubMed] [Google Scholar]
- De Los Reyes A, Kazdin AE. Informant discrepancies in the assessment of childhood psychopathology: a critical review, theoretical framework, and recommendations for further study. Psychological bulletin. 2005;131:483–509. doi: 10.1037/0033-2909.131.4.483. [DOI] [PubMed] [Google Scholar]
- Dietz LJ, Birmaher B, Williamson DE, Silk JS, Dahl RE, Axelson DA, et al. Mother-child interactions in depressed children and children at high risk and low risk for future depression. Journal of the American Academy of Child & Adolescent Psychiatry. 2008;47:574–582. doi: 10.1097/CHI.0b013e3181676595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Durbin CE, Klein DN, Hayden EP, Buckley ME, Moerk KC. Temperamental emotionality in preschoolers and parental mood disorders. Journal of Abnormal Psychology. 2005;114:28–37. doi: 10.1037/0021-843X.114.1.28. [DOI] [PubMed] [Google Scholar]
- Ewell-Foster CJ, Garber J, Durlak JA. Current and past maternal depression, maternal interaction behaviors, and children’s externalizing and internalizing symptoms. Journal of Abnormal Child Psychology. 2008;36:527–537. doi: 10.1007/s10802-007-9197-1. [DOI] [PubMed] [Google Scholar]
- First MB, Gibbon M. The Structured Clinical Interview for DSM-IV Axis I Disorders (SCID-I) and the Structured Clinical Interview for DSM-IV Axis II Disorders (SCID-II). [References] John Wiley & Sons Inc; US; Hoboken, NJ: 2004. [Google Scholar]
- Furman W, Shomaker LB. Patterns of interaction in adolescent romantic relationships: Distinct features and links to other close relationships. Journal of Adolescence. 2008;31:771–788. doi: 10.1016/j.adolescence.2007.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garber J, Cole DA. Intergenerational transmission of depression: A launch and grow model of change across adolescence. Development and Psychopathology. 2010;22:819–830. doi: 10.1017/S0954579410000489. [DOI] [PubMed] [Google Scholar]
- Garber J, Keiley MK, Martin NC. Developmental trajectories of adolescents’ depressive symptoms: Predictors of change. Journal of Consulting and Clinical Psychology. 2002;70:79–95. doi: 10.1037//0022-006x.70.1.79. [DOI] [PubMed] [Google Scholar]
- Ge X, Lorenz FO, Conger RD, Elder GH, Simons RL. Trajectories of stressful life events and depressive symptoms during adolescence. Developmental Psychology. 1994;30:467–483. [Google Scholar]
- Goodman SH, Gotlib IH. Risk for psychopathology in the children of depressed mothers: A developmental model for understanding mechanisms of transmission. Psychological Review. 1999;106:458–490. doi: 10.1037/0033-295x.106.3.458. [DOI] [PubMed] [Google Scholar]
- Goodman SH, Rouse MH, Connell AM, Broth MR, Hall CM, Heyward D. Maternal depression and child psychopathology: A meta-analytic review. Clinical Child and Family Psychology Review. 2011;14:1–27. doi: 10.1007/s10567-010-0080-1. [DOI] [PubMed] [Google Scholar]
- Hetherington EM, Clingempeel W. Coping with marital transitions: A family systems perspective. Monographs of the Society for Research in Child Development. 1992;57:1–242. [Google Scholar]
- Hollenstein T, Granic I, Stoolmiller M, Snyder J. Rigidity in parent-child interactions and the development of externalizing and internalizing behavior in early childhood. Journal of Abnormal Child Psychology. 2004;32:595–607. doi: 10.1023/b:jacp.0000047209.37650.41. [DOI] [PubMed] [Google Scholar]
- Julien D, Markman HJ, Lindahl KM. A comparison of a global and a microanalytic coding system: Implications for future trends in studying interactions: Behavioral Assessment. 1989;11(1):81–100. 1989. [Google Scholar]
- Kaufman J, Birmaher B, Brent D, Rao U, Flynn C, Moreci P, et al. Schedule for Affective Disorders and Schizophrenia for School-Age Children Present and Lifetime version (K-SADS-PL): Initial reliability and validity data. Journal of the American Academy of Child and Adolescent Psychiatry. 1997;36:980–988. doi: 10.1097/00004583-199707000-00021. [DOI] [PubMed] [Google Scholar]
- Klein DN, Kujawa AJ, Black SR, Pennock AT. Depressive disorders. In: Beauchaine TP, Hinshaw SP, editors. Child and adolescent psychopathology. 2nd ed John Wiley & Sons; Hoboken, New Jersey: 2013. pp. 543–576. [Google Scholar]
- Klein DN, Lewinsohn PM, Rohde P, Seeley JR, Olino TM. Psychopathology in the adolescent and young adult offspring of a community sample of mothers and fathers with major depression. Psychological Medicine. 2005;35:353–365. doi: 10.1017/s0033291704003587. [DOI] [PubMed] [Google Scholar]
- Kovacs M. Children’s depression inventory. Multi-Health System; North Tonawanda, N.Y.: 1992. [Google Scholar]
- Kujawa AJ, Torpey D, Kim J, Hajcak G, Rose S, Gotlib IH, et al. Attentional biases for emotional faces in young children of mothers with chronic or recurrent depression. Journal of Abnormal Child Psychology. 2011;39:125–135. doi: 10.1007/s10802-010-9438-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewinsohn PM, Hops H, Roberts RE, Seeley JR, Andrews JA. Adolescent psychopathology: I. Prevalence and incidence of depression and other DSM-III--R disorders in high school students. Journal of Abnormal Psychology. 1993;102:133–144. doi: 10.1037//0021-843x.102.1.133. [DOI] [PubMed] [Google Scholar]
- Lewinsohn PM, Olino TM, Klein DN. Psychosocial impairment in offspring of depressed parents. Psychological Medicine. 2005;35:1493–1503. doi: 10.1017/S0033291705005350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lieb R, Isensee B, Hofler M, Pfister H, Wittchen HU. Parental major depression and the risk of depression and other mental disorders in offspring: a prospective-longitudinal community study. Archives of General Psychiatry. 2002;59:365–374. doi: 10.1001/archpsyc.59.4.365. [DOI] [PubMed] [Google Scholar]
- Lovejoy MC, Graczyk PA, O’Hare E, Neuman G. Maternal depression and parenting behavior: A meta-analytic review. Clinical Psychology Review. 2000;20:561–592. doi: 10.1016/s0272-7358(98)00100-7. [DOI] [PubMed] [Google Scholar]
- McLeod BD, Weisz JR, Wood JJ. Examining the association between parenting and childhood depression: A meta-analysis. Clinical Psychology Review. 2007;27:986–1003. doi: 10.1016/j.cpr.2007.03.001. [DOI] [PubMed] [Google Scholar]
- McMakin DL, Burkehouse KL, Olino TM, Siegle GJ, Dahl RE, Silk JS. Affective functioning among early adolescents at high and low familial risk for depression and their mothers: A focus on individual and transactional processes across contexts. Journal of Abnormal Child Psychology. 2011;39:1213–1225. doi: 10.1007/s10802-011-9540-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olino TM, Yu L, Klein DN, Rohde P, Seeley JR, Pilkonis PA, et al. Measuring depression using item response theory: An examination of three measures of depressive symptomatology. International Journal of Methods in Psychiatric Research. 2012;21:76–85. doi: 10.1002/mpr.1348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patrick CJ, Venables NC, Yancey JR, Hicks BM, Nelson LD, Kramer MD. A construct-network approach to bridging diagnostic and physiological domains: Application to assessment of externalizing psychopathology. Journal of Abnormal Psychology. 2013;122:902–916. doi: 10.1037/a0032807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phares V. Where’s poppa? The relative lack of attention to the role of fathers in child and adolescent psychopathology. American Psychologist. 1992;47:656. doi: 10.1037//0003-066x.47.5.656. [DOI] [PubMed] [Google Scholar]
- Phares V, Compas BE. The role of fathers in child and adolescent psychopathology: Make room for daddy. Psychological Bulletin. 1992;111:387. doi: 10.1037/0033-2909.111.3.387. [DOI] [PubMed] [Google Scholar]
- Raudenbush SW, Bryk AS. Hierarchical linear models: Applications and data analysis methods. Sage Publications; 2002. [Google Scholar]
- Schwartz OS, Dudgeon P, Sheeber LB, Yap MBH, Simmons JG, Allen NB. Observed maternal responses to adolescent behaviour predict the onset of major depression. Behaviour Research and Therapy. 2011;49:331–338. doi: 10.1016/j.brat.2011.02.008. [DOI] [PubMed] [Google Scholar]
- Sheeber L, Hops H, Alpert A, Davis B, Andrews J. Family support and conflict: Prospective relations to adolescent depression. Journal of Abnormal Child Psychology. 1997;25:333–344. doi: 10.1023/a:1025768504415. [DOI] [PubMed] [Google Scholar]
- Sheeber L, Hops H, Davis B. Family processes in adolescent depression. Clinical Child and Family Psychology Review. 2001;4:19–35. doi: 10.1023/a:1009524626436. [DOI] [PubMed] [Google Scholar]
- Stein D, Williamson DE, Birmaher B, Brent DA, Kaufman J, Dahl RE, et al. Parent-child bonding and family functioning in depressed children and children at high risk and low risk for future depression. Journal of the American Academy of Child & Adolescent Psychiatry. 2000;39:1387–1395. doi: 10.1097/00004583-200011000-00013. [DOI] [PubMed] [Google Scholar]
- Weissman MM, Pilowsky DJ, Wickramaratne PJ, Talati A, Wisniewski SR, Fava M, et al. Remissions in maternal depression and child psychopathology. JAMA: Journal of the American Medical Association. 2006;295:1389–1398. doi: 10.1001/jama.295.12.1389. [DOI] [PubMed] [Google Scholar]