Abstract
Objective
To evaluate the increased value of using coronal reformation of a transverse computed tomography (CT) scan for detecting adnexal torsion.
Materials and Methods
This study included 106 woman suspected of having adnexal torsion who underwent CT with coronal reformations and subsequent surgical exploration. Two readers independently recorded the CT findings, such as the thickening of a fallopian tube, twisting of the adnexal pedicle, eccentric smooth wall thickening of the torsed adnexal mass, eccentric septal thickening of the torsed adnexal mass, eccentric poor enhancement of the torsed adnexal mass, uterine deviation to the twisted side, ascites or infiltration of pelvic fat, and the overall impression of adnexal torsion with a transverse scan alone or combined with coronal reformation and a transverse scan. The areas under the receiver operating characteristic curves (AUCs), sensitivity, specificity, and positive predictive value were used to compare diagnostic performance.
Results
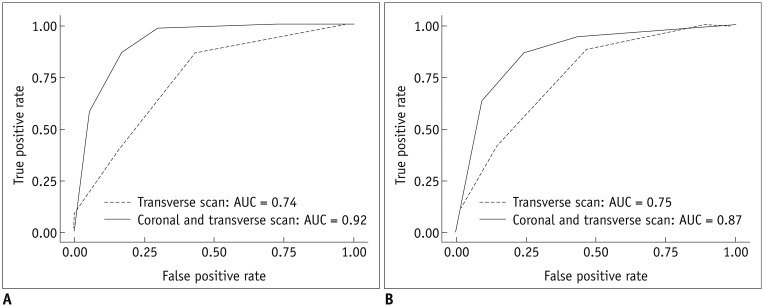
Fifty-two patients were confirmed to have adnexal torsion. The addition of coronal reformations to the transverse scan improved AUCs for readers 1 and 2 from 0.74 and 0.75 to 0.92 and 0.87, respectively, for detecting adnexal torsion (p < 0.001 and p = 0.004, respectively). Sensitivity of CT for detecting twisting of the adnexal pedicle increased significantly for readers 1 and 2 from 0.27 and 0.29 with a transverse scan alone to 0.79 and 0.77 with a combined coronal reformation and a transverse scan, respectively (p < 0.001 and p < 0.001, respectively).
Conclusion
Use of a coronal reformation with transverse CT images improves detection of adnexal torsion.
Keywords: CT, Adnexa, Torsion
INTRODUCTION
Adnexal torsion is a gynecological emergency caused by partial or complete twisting of the ovary, fallopian tube, or both along the vascular pedicle. If the torsion is not relieved, persistent vascular occlusion results in infarction and necrosis of adnexal structures (1). Early recognition is important to preserve the affected ovary and prevent serious complications, such as peritonitis and infertility, but the diagnosis of adnexal torsion poses a challenge because there are no specific clinical signs, manifestations, or biomarkers (2,3). Although gray-scale ultrasonography (US) and Doppler US are the initial imaging modalities of choice when adnexal torsion is suspected (4,5,6), the US findings of adnexal torsion are nonspecific and have not been fully established in a large series (1,7,8).
Use of computed tomography (CT) for evaluating woman presenting with acute pelvic pain in the emergency department has increased to exclude bowel or urologic diseases, such as appendicitis, diverticulitis, or ureter stones. In addition, the innovation of multidetector row CT (MDCT) has led to remarkable improvements in scanning speed, scan volume, and spatial resolution along the z-axis (9). Such technical changes have enabled acquisition of isotropic CT data, and reformations in any desired planes are similar in spatial resolution to those in the transverse plane (10). Several studies have reported that adding a coronal reformation is advantageous to evaluate acute appendicitis, small bowel obstruction, and urinary tract disease (11,12,13,14). Despite promising results obtained with coronal reformations on MDCT in this clinical setting, it remains uncertain whether adding a coronal reformation improves the detection of adnexal torsion. Thus, the purpose of our study was to evaluate the increased value of using a coronal reformation with a transverse CT scan to detect adnexal torsion.
MATERIALS AND METHODS
Study Population
This study was approved by the Institutional Review Board of our medical center. A retrospective analysis of the medical records of patients in our institution from January 1, 2008 to September 30, 2013 was conducted to identify patients who were suspected of having adnexal torsion and who underwent an abdomino-pelvic CT examination and subsequent surgical exploration of the adnexa. Among 110 consecutive patients from our search, four were excluded due to a lack of coronal reformation CT images. Ultimately, 106 patients (age range, 10-80 years; mean age, 34.1 ± 12.3 years) were included in this study. All patients presented with acute pelvic pain for up to 7 days and underwent transabdominal or transvaginal US as first-line imaging. The indications for CT imaging after US included an undetermined ovarian mass, limited US study due to poor sonic window, large ascites volume, or exclusion of bowel disease.
CT Imaging
CT scans were obtained on a MDCT (LightSpeed VCT XT; GE Healthcare, Milwaukee, WI, USA; or LightSpeed Pro 16; GE Healthcare). The scanners were set to the following parameters: detector collimation, 64 × 0.625 mm and 16 × 1.25 mm; helical pitch, 0.984 and 0.938; section thickness/interval, 3.75/3.75 mm and 3.75/3.75 mm; rotation time, 0.5 seconds; 120 kVp/300-500 mA and 120 Kvp/200-400 mA, respectively. Intravenous contrast (iopromide, Ultravist 370; Bayer Healthcare, Berlin, Germany) was injected at a rate of 3 mL/sec in a total volume of 130 mL through the antecubital vein using a mechanical injector. Bolus tracking was not applied, and scanning started 90 seconds after beginning the contrast injection. No oral contrast agent was used. Scanning regularly covered the region from the dome of the liver to the lower vagina. Coronal reformatted images of 3.0 mm section thickness and 3.0 mm reconstruction intervals were generated using the source CT data set and commercially available console software (Volume Viewer; GE Medical Systems, Waukesha, WI, USA). Radiation dose to the patients was monitored for each examination using the volume CT dose index (CTDIvol) and dose length product (DLP), which were calculated by the CT scanner and were automatically saved to a dose report. The mean CTDIvol value was 10.7 ± 2.1 mGy, and the mean DLP value was 530.3 ± 109.1 mGy·cm.
Image Analysis
The CT images were reviewed retrospectively and independently on a picture archiving and communication system workstation (Centricity; GE Healthcare) by two radiologists (with 7 and 5 years experience, respectively, in genitourinary and abdominal imaging). The readers were blinded to all surgical and pathological data. Both readers independently reviewed 1) the transverse CT scan alone and 2) the coronal reformation in combination with the transverse CT scan. The two CT data sets for each patient were randomly interpreted during different sessions at 4-week intervals to minimize recall bias. The CT images were specifically evaluated for the presence or absence of findings related to adnexal torsion, including thickening of a fallopian tube, twisting of the adnexal pedicle, eccentric smooth wall thickening of the torsed adnexal mass, eccentric septal thickening of the torsed adnexal mass, eccentric poor enhancement of the torsed adnexal mass, uterine deviation to the twisted side, ascites, and infiltration of pelvic fat (2,7,15,16). In addition, each reader gave an overall impression of the likelihood of adnexal torsion based on all of the CT findings, using a rating scale of 1 to 5 (1, definitely absent; 2, probably absent; 3, indeterminate; 4, probably present; and 5, definitely present). In patients with bilateral adnexal masses, only the side more likely to be torsed was evaluated because synchronous bilateral adnexal torsion is very rare (17).
Statistical Analysis
Clinical and demographic data are reported with descriptive statistics. Mean, median, and standard deviation are used to summarize continuous variables; frequencies and percentages were used for categorical variables. The Wilcoxon rank-sum test was used to assess the difference between patients with and without adnexal torsion. Receiver operating characteristic curves and the areas under the receiver operating characteristic curves (AUCs) with 95% confidence intervals (CIs) were estimated for overall diagnostic performance of each image set and each reader using nonparametric methods for the 5-point ordinal score assessments. The AUCs for the transverse CT scan alone and the coronal reformation with the transverse CT scan were compared using a nonparametric method (18,19). Sensitivity, specificity, and positive predictive value (PPV) were estimated with an imaging score > 3 as positive for adnexal torsion. Sensitivity and specificity comparisons for the transverse CT scan alone vs. a coronal reformation and the transverse CT scan were calculated using the McNemar test. p-values ≤ 0.05 or less were considered significant.
Inter-reader agreement was assessed using the weighted κ statistic with quadratic weights and was interpreted using the following scale: slight agreement, ≤ 0.20; fair agreement, 0.21-0.40; moderate agreement, 0.41-0.60; substantial agreement, 0.61-0.80; and almost perfect agreement, 0.81-1.0 (20,21). The 95% CIs are reported for the estimated κ statistics.
All statistical analyses were performed with the MedCalc Software 14.10.2 software package (MedCalc, Mariakerke, Belgium).
RESULTS
A total 111 adnexal masses in 106 patients were demonstrated at surgery and during the pathological examinations. An adnexal mass was detected in all patients, and bilateral adnexal masses were demonstrated in five (5/106, 4.7%). Of the five patients with bilateral adnexal masses, three had bilateral endometrioma, one had bilateral corpus luteal cysts, and one had a mucinous cystadenoma and corpus luteal cyst in each adnexa. Of the 106 patients, 52 (52/106, 49.1%) were confirmed to have adnexal torsion, and 54 (54/106, 51.9%) were confirmed not to have adnexal torsion. Table 1 shows the characteristics of the patients with or without adnexal torsion. All cases of adnexal torsion were unilateral, with a slightly right-sided predominance (28:24).
Table 1. Charateristics of Patients with or without Adnexal Torsion.
| Patients with Adnexal Torsion (n = 52) |
Patients without Adnexal Torsion (n = 54) |
P | |
|---|---|---|---|
| Age (years) | 31.0 (22.5-41.5)* | 32.5 (27.0-42.0)* | 0.301 |
| The largest diameter of adnexal mass (cm) | 8.6 (7.0-10.8)* | 6.5 (5.6-8.5)* | 0.002 |
| Hemorrhagic infarction | 20 (38.4) | NA | |
| Histopathologic diagnosis | |||
| Teratoma | 22 (42.3) | 10 (18.5) | |
| Endometrioma | 1 (1.9) | 15 (27.8) | |
| Corpus luteal cyst | 5 (9.6) | 12 (22.2) | |
| Follicular cyst | 10 (19.2) | 7 (13.0) | |
| Mucinous cystadenoma | 3 (5.8) | 4 (7.4) | |
| Serous cystadenoma | 6 (11.5) | 0 | |
| Borderline tumor | 2 (3.8) | 2 (3.7) | |
| Paratubal cyst | 2 (3.8) | 2 (3.7) | |
| Hydrosalpinx | 1 (1.9) | 0 | |
| Tuboovarian abscess | 0 | 1 (1.9) | |
| Fibroma | 0 | 1 (1.9) | |
| Paraovarian cyst | 0 | 1 (1.9) |
Unless otherwise indicated, data are number of patients, with percentages in parentheses. *Data are medians, with ranges in parentheses. NA = not applicable
Adding the coronal reformation to the transverse CT scan improved overall diagnostic performance for detecting adnexal torsion (Table 2, Fig. 1). The AUC for reader 1 increased from 0.74 (95% CI, 0.64-0.82) with a transverse CT scan alone to 0.92 (95% CI, 0.85-0.96) with a coronal reformation and a transverse CT scan (p < 0.001). The AUC for reader 2 increased from 0.75 (95% CI, 0.66-0.83) with a transverse CT scan alone to 0.87 (95% CI, 0.79-0.92) with a coronal reformation and a transverse CT scan (p = 0.004). Interreader agreement for detecting adnexal torsion was moderate (κ = 0.46 for a transverse CT scan alone and κ = 0.57 for a coronal reformation and a transverse CT scan). Sensitivity, specificity, PPV, and accuracy values of each CT finding for diagnosing adnexal torsion using a transverse CT scan alone and a coronal reformation and a transverse CT scan are presented for both readers in Tables 3 and 4 and Figures 2, 3, 4, 5, 6, 7. Sensitivity of reader 1 for the CT finding of a twisted adnexal pedicle increased significantly from 0.27 (95% CI, 0.17-0.40) with a transverse CT scan alone to 0.79 (95% CI, 0.66-0.88) with a coronal reformation and a transverse CT scan (p < 0.001), while sensitivity of reader 2 increased significantly from 0.29 (95% CI, 0.18-0.42) with a transverse CT scan alone to 0.77 (95% CI, 0.64-0.86) with a coronal reformation and a transverse CT scan (p < 0.001).
Table 2. Diagnostic Parameters for Detecting Adnexal Torsion.
| Parameter | Reader 1 | Reader 2 | ||||
|---|---|---|---|---|---|---|
| Transverse Scan | Coronal and Transverse Scans | P | Transverse Scans | Coronal and Transverse Scans | P | |
| AUC | 0.74 (0.64-0.82) |
0.92 (0.85-0.96) |
< 0.001 | 0.75 (0.66-0.83) |
0.87 (0.79-0.92) |
0.004 |
| Sensitivity | 0.35 (0.23-0.48) [18/52] |
0.87 (0.74-0.94) [45/52] |
< 0.001 | 0.42 (0.30-0.56) [22/52] |
0.87 (0.74-0.94) [45/52] |
< 0.001 |
| Specificity | 0.87 (0.75-0.94) [47/54] |
0.83 (0.71-0.91) [45/54] |
0.691 | 0.85 (0.73-0.93) [46/54] |
0.76 (0.63-0.85) [41/54] |
0.181 |
| Positive predictive value | 0.72 (0.52-0.86) [18/25] |
0.83 (0.71-0.91) [45/54] |
0.73 (0.55-0.86) [22/30] |
0.78 (0.65-0.87) [45/58] |
||
| Accuracy | 0.61 (0.52-0.70) [65/106] |
0.85 (0.77-0.91) [90/106] |
0.64 (0.55-0.73) [68/106] |
0.81 (0.73-0.88) [86/106] |
||
Data with 95% confidence intervals in parentheses and numerators and denominators in brackets. AUC = area under receiver operating characteristic curve
Fig. 1. Receiver operating characteristic curves for reader 1 (A) and reader 2 (B) for detecting adnexal torsion.
AUC = areas under receiver operating characteristic curve
Table 3. Diagnostic Performance of CT Findings for Detecting Adnexal Torsion by Reader 1.
| CT Finding | Sensitivity | Specificity | Positive Predictive Value | Accuracy | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Transverse Scan | Coronal and Transverse Scans | P | Transverse Scan | Coronal and Transverse Scans | P | Transverse Scan | Coronal and Transverse Scans | Transverse Scan | Coronal and Transverse Scans | |
| Tubal thickening | 0.73 (0.60-0.83) [38/52] |
0.63 (0.50-0.75) [33/52] |
0.326 | 0.67 (0.53-0.78) [36/54] |
0.81 (0.69-0.90) [44/54] |
0.021 | 0.68 (0.55-0.79) [38/56] |
0.77 (0.62-0.87) [33/43] |
0.70 (0.60-0.78) [74/106] |
0.73 (0.63-0.80) [77/106] |
| Twisting of adnexal pedicle | 0.27 (0.17-0.40) [14/52] |
0.79 (0.66-0.88) [41/52] |
< 0.001 | 0.91 (0.80-0.96) [49/54] |
0.81 (0.69-0.90) [44/54] |
0.221 | 0.74 (0.50-0.89) [14/19] |
0.80 (0.67-0.89) [41/51] |
0.59 (0.50-0.68) [63/106] |
0.80 (0.72-0.87) [85/106] |
| Eccentric smooth wall thickening of adnexal mass | 0.52 (0.39-0.65) [27/52] |
0.58 (0.44-0.70) [30/52] |
0.452 | 0.52 (0.39-0.65) [28/54] |
0.50 (0.37-0.63) [27/54] |
1.000 | 0.51 (0.38-0.64) [27/53] |
0.53 (0.40-0.65) [30/57] |
0.52 (0.42-0.61) [55/106] |
0.54 (0.44-0.63) [57/106] |
| Eccentric septal thickening of adnexal mass | 0.15 (0.08-0.28) [8/52] |
0.15 (0.08-0.28) [8/52] |
NA | 0.87 (0.75-0.94) [47/54] |
0.87 (0.75-0.94) [47/54] |
1.000 | 0.53 (0.30-0.75) [8/15] |
0.53 (0.30-0.75) [8/15] |
0.52 (0.42-0.61) [55/106] |
0.52 (0.42-0.61) [55/106] |
| Eccentric poor enhancement of adnexal mass | 0.12 (0.05-0.23) [6/52] |
0.12 (0.05-0.23) [6/52] |
1.000 | 0.94 (0.84-0.99) [51/54] |
0.94 (0.84-0.99) [51/54] |
NA | 0.67 (0.35-0.88) [6/9] |
0.67 (0.35-0.88) [6/9] |
0.54 (0.44-0.63) [57/106] |
0.54 (0.44-0.63) [57/106] |
| Uterine deviation to side of involved adnexa | 0.08 (0.03-0.19) [4/52] |
0.12 (0.05-0.23) [6/52] |
0.634 | 0.87 (0.75-0.94) [47/54] |
0.89 (0.77-0.95) [48/54] |
1.000 | 0.36 (0.15-0.65) [4/11] |
0.50 (0.25-0.75) [6/12] |
0.48 (0.39-0.58) [51/106] |
0.51 (0.42-0.60) [54/106] |
| Ascites | 0.69 (0.57-0.80) [36/52] |
0.77 (0.64-0.86) [40/52] |
0.132 | 0.31 (0.21-0.45) [17/54] |
0.35 (0.24-0.49) [19/54] |
0.632 | 0.49 (0.38-0.61) [36/73] |
0.53 (0.42-0.64) [40/75] |
0.50 (0.41-0.59) [53/106] |
0.56 (0.46-0.65) [59/106] |
| Infiltration of periadnexal fat | 0.29 (0.18-0.42) [15/52] |
0.37 (0.25-0.50) [19/52] |
0.133 | 0.52 (0.39-0.65) [28/54] |
0.56 (0.42-0.68) [30/54] |
0.501 | 0.37 (0.24-0.52) [15/41] |
0.44 (0.30-0.59) [19/43] |
0.41 (0.32-0.50) [43/106] |
0.46 (0.37-0.56) [49/106] |
Data with 95% confidence intervals in parentheses and numerators and denominators in brackets. NA = not applicable
Table 4. Diagnostic Performance of CT Findings for Detecting Adnexal Torsion by Reader 2.
| CT Finding | Sensitivity | Specificity | Positive Predictive Value | Accuracy | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Transverse Scan | Coronal and Transverse Scans | P | Transverse Scan | Coronal and Transverse Scans | P | Transverse Scan | Coronal and Transverse Scans | Transverse Scan | Coronal and Transverse Scans | |
| Tubal thickening | 0.92 (0.81-0.97) [48/52] |
0.96 (0.86-1.00) [50/52] |
0.502 | 0.48 (0.35-0.61) [26/54] |
0.37 (0.25-0.50) [20/54] |
0.072 | 0.63 (0.52-0.73) [48/76] |
0.60 (0.49-0.69) [50/84] |
0.70 (0.60-0.77) [74/106] |
0.66 (0.57-0.74) [70/106] |
| Twisting of adnexal pedicle | 0.29 (0.18-0.42) [15/52] |
0.77 (0.64-0.86) [40/52] |
< 0.001 | 0.91 (0.80-0.96) [49/54] |
0.74 (0.61-0.84) [40/54] |
0.013 | 0.75 (0.53-0.89) [15/20] |
0.74 (0.61-0.84) [40/54] |
0.60 (0.51-0.69) [64/106] |
0.75 (0.67-0.83) [80/106] |
| Eccentric wall thickening of adnexal mass | 0.71 (0.58-0.82) [37/52] |
0.87 (0.74-0.94) [45/52] |
0.008 | 0.59 (0.46-0.71) [32/54] |
0.54 (0.41-0.66) [29/54] |
0.382 | 0.63 (0.50-0.74) [37/59] |
0.64 (0.53-0.75) [45/70] |
0.65 (0.56-0.74) [69/106] |
0.70 (0.60-0.78) [74/106] |
| Eccentric septal thickening of adnexal mass | 0.19 (0.11-0.32) [10/52] |
0.31 (0.20-0.44) [16/52] |
0.032 | 0.89 (0.77-0.95) [48/54] |
0.87 (0.75-0.94) [47/54] |
1.000 | 0.63 (0.39-0.82) [10/16] |
0.70 (0.49-0.85) [16/23] |
0.55 (0.45-0.64) [58/106] |
0.59 (0.50-0.68) [63/106] |
| Eccentric poor enhancement of adnexal mass | 0 (0-0.08) [0/52] |
0 (0-0.08) [0/52] |
NA | 1.00 (0.92-1.00) [54/54] |
1.00 (0.92-1.00) [54/54] |
NA | NA [0/0] |
NA [0/0] |
0.51 (0.42-0.60) [54/106] |
0.51 (0.42-0.60) [54/106] |
| Uterine deviation to side of involved adnexa | 0.60 (0.46-0.72) [31/52] |
0.71 (0.58-0.82) [37/52] |
0.032 | 0.67 (0.53-0.78) [36/54] |
0.65 (0.51-0.76) [35/54] |
1.000 | 0.63 (0.49-0.75) [31/49] |
0.66 (0.53-0.77) [37/56] |
0.63 (0.53-0.72) [67/106] |
0.68 (0.59-0.76) [72/106] |
| Ascites | 0.85 (0.72-0.92) [44/52] |
0.87 (0.74-0.94) [45/52] |
1.000 | 0.17 (0.09-0.29) [9/54] |
0.15 (0.07-0.27) [8/54] |
1.000 | 0.49 (0.39-0.60) [44/89] |
0.49 (0.39-0.60) [45/91] |
0.50 (0.41-0.59) [53/106] |
0.50 (0.41-0.59) [53/106] |
| Infiltration of periadnexal fat | 0.79 (0.66-0.88) [41/52] |
0.87 (0.74-0.94) [45/52] |
0.214 | 0.61 (0.48-0.73) [33/54] |
0.43 (0.30-0.59) [23/54] |
0.002 | 0.66 (0.54-0.77) [41/62] |
0.59 (0.48-0.70) [45/76] |
0.70 (0.60-0.78) [74/106] |
0.64 (0.55-0.73) [68/106] |
Data with 95% confidence intervals in parentheses and numerators and denominators in brackets. NA = not applicable
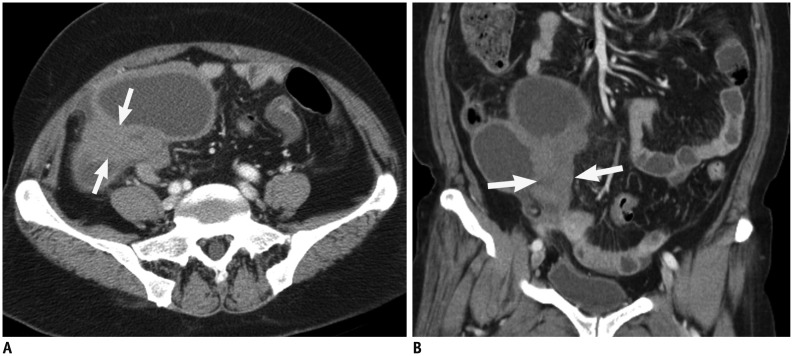
Fig. 2. Contrast-enhanced computed tomography (CT) scan of 66-year-old woman with torsion of follicular cyst in right ovary.
Transverse CT scan (A) and coronal reformation (B) show multilocular cystic mass with homogeneously elongated soft tissue lesion representing tubal thickening (arrows).
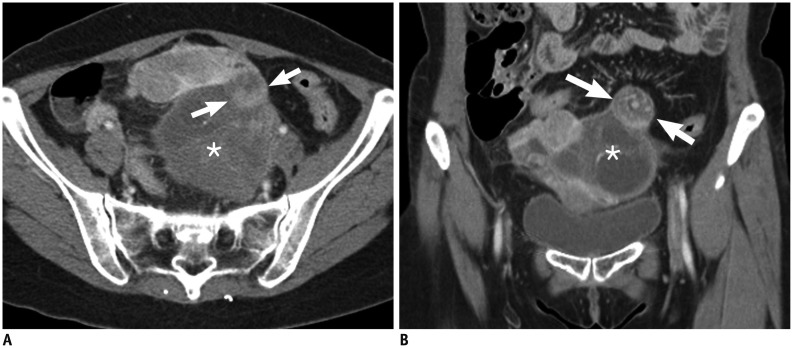
Fig. 3. Contrast-enhanced computed tomography (CT) scan of 53-year-old woman with torsion of follicular cyst in left ovary.
Transverse CT scan (A) and coronal reformation (B) show heterogeneous cystic mass (*) with swirling soft tissue lesion representing twisting of adnexal pedicle (arrows).
Fig. 4. Contrast-enhanced computed tomography (CT) scan of 41-year-old woman with torsion of follicular cyst in right ovary.
Transverse CT scan (A) and coronal reformation (B) show unilocular cystic mass with eccentric smooth wall thickening (arrows).
Fig. 5. Contrast-enhanced computed tomography (CT) scan of 52-year-old woman with torsion of follicular cyst in right ovary.
Transverse CT scan (A) and coronal reformation (B) show eccentric septal thickening (arrow) of cystic mass.
Fig. 6. Contrast-enhanced computed tomography (CT) scan of 49-year-old woman with complaint of acute pelvic pain as false-negative case.
Transverse CT scan (A) and coronal reformation (B) show well-defined cystic mass (*) in pelvic cavity. Both readers provided scores of 2 as level of suspicion for adnexal torsion using 5-point scale. Adnexal mass was serous cystadenoma with torsion in right ovary.
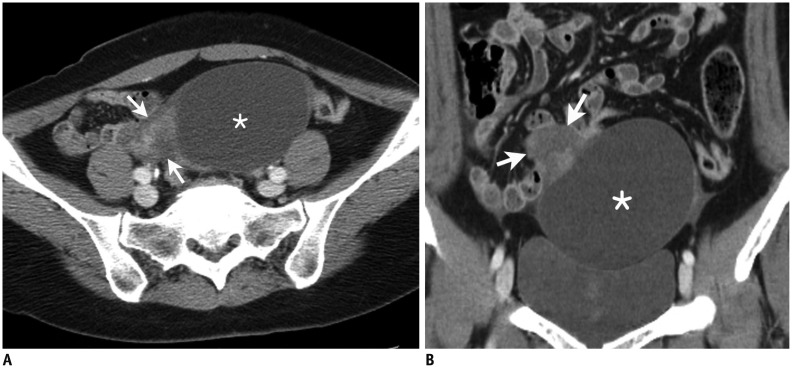
Fig. 7. Contrast-enhanced computed tomography (CT) scan in 38-year-old woman with complaint of acute pelvic pain as false-positive case.
Transverse CT scan (A) and coronal reformation (B) show well-defined cystic mass (*) with eccentric soft tissue lesion (arrows). Both readers provided score of 4 as level of suspicion for adnexal torsion using 5-point scale. Adnexal mass was paratubal cyst without torsion in right ovary.
DISCUSSION
We demonstrated that a coronal reformation added value to a transverse CT scan for detecting adnexal torsion. When the coronal reformation was combined with a transverse CT scan, accuracy for the overall detection of adnexal torsion improved significantly for both readers. In particular, the detection rate of a twisted adnexal pedicle increased significantly for both readers.
The pathophysiological process of adnexal torsion is a sequence of several events. A twisted ovarian pedicle and fallopian tube initially compromise venous and lymphatic outflow resulting in congestion and diffuse ovarian edema, which are likely followed by arterial obstruction and thrombosis. Continued vascular compromise can lead to hemorrhagic infarction and necrosis of the affected ovary.
Ultrasonography is the primary imaging technique most often used in woman with acute pelvic pain suspicious for adnexal torsion. Typical US findings include cystic, solid, or complex ovarian masses, free fluid collection, thickening of the wall, cystic hemorrhage, or follicles at the periphery of an enlarged ovary (3,6,8,22,23). However, low detection rates of 46-74% make distinguishing those from other diseases, such as hemorrhagic cysts, endometriosis, ovarian tumors, or pelvic inflammatory disease, difficult (15). Moreover, given the large variability in Doppler US findings and characteristic dual vascular supply to the ovary, the value of Doppler US is limited for detecting adnexal torsion (8,24,25).
The widespread use of CT for assessing gynecological diseases has led to the view that CT may be useful if the adnexal torsion is equivocal on US or if the lesion is not well depicted sonographically (2,7,15,26). Rha et al. (7) reported that common CT findings of adnexal torsion include tubal thickening, smooth wall thickening of a twisted ovarian cystic mass, ascites, and uterine deviation to the twisted side. A study by Hiller et al. (2) demonstrated that a well-defined adnexal mass with a smooth border or infiltration of periadnexal fat is an important CT sign of adnexal torsion. Chiou et al. (1) also demonstrated that minimal or absent enhancement of a torsed ovary on CT indicates the evolution of ovarian torsion from ischemia to infarction. In the first study that evaluated the diagnostic performance of CT findings for identifying adnexal torsion, Lee et al. (16) found that the accuracy of intra-adnexal or extra-adnexal CT findings, including tubal thickening, eccentric wall or septal thickening of the adnexal mass, eccentric poor enhancement of the adnexal mass, uterine deviation to the side of the involved adnexa, ascites, or infiltration of periadnexal fat ranged from 0.85 to 0.97. However, their data may have been somewhat overestimated because their study population was enrolled regardless of the status or duration of pelvic pain (16). Of note, the aforementioned CT findings may be secondary changes of a torsed ovary and the adjacent genital tract, which reflect edema, congestion, infarction, or necrosis, and are not clear obvious proof of torsion per se (26).
A feature that directly indicates adnexal torsion is twisting of the adnexal pedicle, which shows a characteristic swirling target appearance of the adnexa, and can be a most definitive and pathognomic sign of adnexal torsion (15,25). A twisted pedicle corresponds to the broad ligament, fallopian tube, and ovarian branches of the uterine artery and vein (24). Detecting of this finding varies between 13 and 88% of patients with adnexal torsion on US and in less than one-third of patients with adnexal torsion on CT or magnetic resonance imaging (2,4,24,25). Our results for detecting a twisted adnexal pedicle on a transverse CT scan alone were similar to those of previous studies (2,27). Interestingly, adding a coronal reformation to a transverse CT scan significantly improved the detection rate of this finding from 27-29% to 77-79% and twisting of the adnexal pedicle had the highest accuracy (75-80%) among all CT findings. Similarly, the adding a coronal reformation significantly increased overall accuracy (87-92%) and sensitivity (87%) for detecting adnexal torsion. We suggest that these observations are a clue to validate our hypothesis that additional coronal reformations provide a more intuitive anatomic perspective and help to evaluate an unpredictable tortuous structure, such as an adnexal pedicle, as in previous studies on acute appendicitis (14,28).
We acknowledge the following limitations. First, our study was retrospective. Verification or selection bias may have distorted the true diagnostic performance and limit the applicability of results because we only included patients who underwent preoperative CT and surgery. Second, the relatively high proportion of patients with adnexal torsion in our sample may have affected pretest probability. Third, the readers were instructed to search specifically for adnexal torsion on CT, which may have improved accuracy. Fourth, our results were based on findings obtained from nonuniform CT scanners; however, this reflects actual clinical practice.
In conclusion, adding a coronal reformation to a transverse CT scan improved overall accuracy for diagnosing adnexal torsion and was valuable for detecting a twisted adnexal pedicle.
References
- 1.Chiou SY, Lev-Toaff AS, Masuda E, Feld RI, Bergin D. Adnexal torsion: new clinical and imaging observations by sonography, computed tomography, and magnetic resonance imaging. J Ultrasound Med. 2007;26:1289–1301. doi: 10.7863/jum.2007.26.10.1289. [DOI] [PubMed] [Google Scholar]
- 2.Hiller N, Appelbaum L, Simanovsky N, Lev-Sagi A, Aharoni D, Sella T. CT features of adnexal torsion. AJR Am J Roentgenol. 2007;189:124–129. doi: 10.2214/AJR.06.0073. [DOI] [PubMed] [Google Scholar]
- 3.Kiechl-Kohlendorfer U, Maurer K, Unsinn KM, Gassner I. Fluid-debris level in follicular cysts: a pathognomonic sign of ovarian torsion. Pediatr Radiol. 2006;36:421–425. doi: 10.1007/s00247-005-0104-z. [DOI] [PubMed] [Google Scholar]
- 4.Albayram F, Hamper UM. Ovarian and adnexal torsion: spectrum of sonographic findings with pathologic correlation. J Ultrasound Med. 2001;20:1083–1089. doi: 10.7863/jum.2001.20.10.1083. [DOI] [PubMed] [Google Scholar]
- 5.Auslender R, Shen O, Kaufman Y, Goldberg Y, Bardicef M, Lissak A, et al. Doppler and gray-scale sonographic classification of adnexal torsion. Ultrasound Obstet Gynecol. 2009;34:208–211. doi: 10.1002/uog.6369. [DOI] [PubMed] [Google Scholar]
- 6.Graif M, Shalev J, Strauss S, Engelberg S, Mashiach S, Itzchak Y. Torsion of the ovary: sonographic features. AJR Am J Roentgenol. 1984;143:1331–1334. doi: 10.2214/ajr.143.6.1331. [DOI] [PubMed] [Google Scholar]
- 7.Rha SE, Byun JY, Jung SE, Jung JI, Choi BG, Kim BS, et al. CT and MR imaging features of adnexal torsion. Radiographics. 2002;22:283–294. doi: 10.1148/radiographics.22.2.g02mr02283. [DOI] [PubMed] [Google Scholar]
- 8.Rosado WM, Jr, Trambert MA, Gosink BB, Pretorius DH. Adnexal torsion: diagnosis by using Doppler sonography. AJR Am J Roentgenol. 1992;159:1251–1253. doi: 10.2214/ajr.159.6.1442394. [DOI] [PubMed] [Google Scholar]
- 9.Boone JM. Multidetector CT: opportunities, challenges, and concerns associated with scanners with 64 or more detector rows. Radiology. 2006;241:334–337. doi: 10.1148/radiol.2412060169. [DOI] [PubMed] [Google Scholar]
- 10.Jaffe TA, Nelson RC, Johnson GA, Lee ER, Yoshizumi TT, Lowry CR, et al. Optimization of multiplanar reformations from isotropic data sets acquired with 16-detector row helical CT scanner. Radiology. 2006;238:292–299. doi: 10.1148/radiol.2381050404. [DOI] [PubMed] [Google Scholar]
- 11.Hodel J, Zins M, Desmottes L, Boulay-Coletta I, Jullès MC, Nakache JP, et al. Location of the transition zone in CT of small-bowel obstruction: added value of multiplanar reformations. Abdom Imaging. 2009;34:35–41. doi: 10.1007/s00261-007-9348-4. [DOI] [PubMed] [Google Scholar]
- 12.Jaffe TA, Martin LC, Thomas J, Adamson AR, DeLong DM, Paulson EK. Small-bowel obstruction: coronal reformations from isotropic voxels at 16-section multi-detector row CT. Radiology. 2006;238:135–142. doi: 10.1148/radiol.2381050489. [DOI] [PubMed] [Google Scholar]
- 13.Noroozian M, Cohan RH, Caoili EM, Cowan NC, Ellis JH. Multislice CT urography: state of the art. Br J Radiol. 2004;77 Spec No 1:S74–S86. doi: 10.1259/bjr/13478281. [DOI] [PubMed] [Google Scholar]
- 14.Paulson EK, Harris JP, Jaffe TA, Haugan PA, Nelson RC. Acute appendicitis: added diagnostic value of coronal reformations from isotropic voxels at multi-detector row CT. Radiology. 2005;235:879–885. doi: 10.1148/radiol.2353041231. [DOI] [PubMed] [Google Scholar]
- 15.Duigenan S, Oliva E, Lee SI. Ovarian torsion: diagnostic features on CT and MRI with pathologic correlation. AJR Am J Roentgenol. 2012;198:W122–W131. doi: 10.2214/AJR.10.7293. [DOI] [PubMed] [Google Scholar]
- 16.Lee JH, Park SB, Shin SH, Jang JC, Lee WC, Jeong AK, et al. Value of intra-adnexal and extra-adnexal computed tomographic imaging features diagnosing torsion of adnexal tumor. J Comput Assist Tomogr. 2009;33:872–876. doi: 10.1097/RCT.0b013e31819e41f3. [DOI] [PubMed] [Google Scholar]
- 17.Dunnihoo DR, Wolff J. Bilateral torsion of the adnexa: a case report and a review of the world literature. Obstet Gynecol. 1984;64(3 Suppl):55S–59S. doi: 10.1097/00006250-198409001-00015. [DOI] [PubMed] [Google Scholar]
- 18.Song HH. Analysis of correlated ROC areas in diagnostic testing. Biometrics. 1997;53:370–382. [PubMed] [Google Scholar]
- 19.Molodianovitch K, Faraggi D, Reiser B. Comparing the areas under two correlated ROC curves: parametric and non-parametric approaches. Biom J. 2006;48:745–757. doi: 10.1002/bimj.200610223. [DOI] [PubMed] [Google Scholar]
- 20.Cohen J. Weighted kappa: nominal scale agreement with provision for scaled disagreement or partial credit. Psychol Bull. 1968;70:213–220. doi: 10.1037/h0026256. [DOI] [PubMed] [Google Scholar]
- 21.Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33:159–174. [PubMed] [Google Scholar]
- 22.Shadinger LL, Andreotti RF, Kurian RL. Preoperative sonographic and clinical characteristics as predictors of ovarian torsion. J Ultrasound Med. 2008;27:7–13. doi: 10.7863/jum.2008.27.1.7. [DOI] [PubMed] [Google Scholar]
- 23.Warner MA, Fleischer AC, Edell SL, Thieme GA, Bundy AL, Kurtz AB, et al. Uterine adnexal torsion: sonographic findings. Radiology. 1985;154:773–775. doi: 10.1148/radiology.154.3.3881798. [DOI] [PubMed] [Google Scholar]
- 24.Lee EJ, Kwon HC, Joo HJ, Suh JH, Fleischer AC. Diagnosis of ovarian torsion with color Doppler sonography: depiction of twisted vascular pedicle. J Ultrasound Med. 1998;17:83–89. doi: 10.7863/jum.1998.17.2.83. [DOI] [PubMed] [Google Scholar]
- 25.Vijayaraghavan SB. Sonographic whirlpool sign in ovarian torsion. J Ultrasound Med. 2004;23:1643–1649. quiz 1650-1651. doi: 10.7863/jum.2004.23.12.1643. [DOI] [PubMed] [Google Scholar]
- 26.Chang HC, Bhatt S, Dogra VS. Pearls and pitfalls in diagnosis of ovarian torsion. Radiographics. 2008;28:1355–1368. doi: 10.1148/rg.285075130. [DOI] [PubMed] [Google Scholar]
- 27.Comerci JT, Jr, Licciardi F, Bergh PA, Gregori C, Breen JL. Mature cystic teratoma: a clinicopathologic evaluation of 517 cases and review of the literature. Obstet Gynecol. 1994;84:22–28. [PubMed] [Google Scholar]
- 28.Paulson EK, Jaffe TA, Thomas J, Harris JP, Nelson RC. MDCT of patients with acute abdominal pain: a new perspective using coronal reformations from submillimeter isotropic voxels. AJR Am J Roentgenol. 2004;183:899–906. doi: 10.2214/ajr.183.4.1830899. [DOI] [PubMed] [Google Scholar]