Abstract
Objective
To assess inter-modality variability when evaluating cervical intervertebral disc herniation using 64-slice multidetector-row computed tomography (MDCT) and magnetic resonance imaging (MRI).
Materials and Methods
Three musculoskeletal radiologists independently reviewed cervical spine 1.5-T MRI and 64-slice MDCT data on C2-3 though C6-7 of 51 patients in the context of intervertebral disc herniation. Interobserver and inter-modality agreements were expressed as unweighted kappa values. Weighted kappa statistics were used to assess the extents of agreement in terms of the number of involved segments (NIS) in disc herniation and epicenter measurements collected using MDCT and MRI.
Results
The interobserver agreement rates upon evaluation of disc morphology by the three radiologists were in fair to moderate agreement (k = 0.39-0.53 for MDCT images; k = 0.45-0.56 for MRIs). When the disc morphology was categorized into two and four grades, the inter-modality agreement rates were moderate (k-value, 0.59) and substantial (k-value, 0.66), respectively. The inter-modality agreements for evaluations of the NIS (k-value, 0.78) and the epicenter (k-value, 0.79) were substantial. Also, the interobserver agreements for the NIS (CT; k-value, 0.85 and MRI; k-value, 0.88) and epicenter (CT; k-value, 0.74 and MRI; k-value, 0.70) evaluations by two readers were substantial. MDCT tended to underestimate the extent of herniated disc lesions compared with MRI.
Conclusion
Multidetector-row computed tomography and MRI showed a moderate-to-substantial degree of inter-modality agreement for the assessment of herniated cervical discs. MDCT images have a tendency to underestimate the anterior/posterior extent of the herniated disc compared with MRI.
Keywords: Cervical spine, Disc herniation, MDCT, MRI
INTRODUCTION
Cervical radiculopathy is caused by a combination of compression and inflammation of a spinal nerve. These can be caused by decreased disc height and degenerative changes in the uncovertebral and facet joints (i.e., cervical spondylosis). Herniation of the nucleus pulposus is a relatively rare cause of cervical radiculopathy, which usually occurs in younger age groups than cervical spondylosis (1,2). Magnetic resonance imaging (MRI) is currently considered the imaging modality of choice in patients with cervical radiculopathy, because it does not expose patients to a radiation hazard, has excellent soft-tissue resolution, and can create multi-planar images (3,4,5,6). Additionally, contrast-enhanced CT (7) and CT myelography (8) remain useful imaging tools in the evaluation of cervical radiculopathy, but they carry the risk of anaphylactic reactions and nephrotoxicity with the use of iodinated contrast material.
Non-contrast CT also plays an important role in the preoperational assessment of lumbar disc herniated diseases (9,10,11), with a diagnostic performance similar to that of lumbar spine MRI (10). However, the use of non-contrast CT in the evaluation of disc herniation has been limited due to several disadvantages, including the lack of soft-tissue contrast, radiation exposure, the effects of partial volume averaging, the time required for reformatting multiple thin (1.5-3-mm) sections over multiple vertebral bodies and intervening discs, beam-hardening artifacts in the lower cervical spines caused by the bony structures of the shoulder girdle, and image degradation related to motion artifacts (12).
The recent development of multidetector-row computed tomography (MDCT) allows a scan acquisition time of a few seconds and improvement in spatial resolution using thinner collimation, enhancing improved multi-planar reconstructions and diminishing motion artifacts. MDCT is frequently used as a practical and cost-effective approach to investigating correlative compressive lesions, such as disc herniation or spondylosis, in cervical spine patients who have failed a course of conservative therapy, may be candidates for interventional or surgical treatment, and have a contraindication to MRI (13).
When CT is performed on postoperative patients who have undergone preoperative MRI to evaluate disc herniation, radiologists may find it difficult to compare the views of the herniated disc afforded by MRI and CT.
However, to our knowledge, no comparison of inter-modality agreement in the assessment of cervical herniated disc herniation between non-contrast MDCT and MRI has been reported. The aim of the present study was to investigate the assessment of cervical intervertebral disc herniation using 64-slice MDCT and MRI.
MATERIALS AND METHODS
Patients
The Institutional Review Board approved the research protocol and waived the requirement for patient informed consent because the study was retrospective in nature. From February 2009 to November 2011, 102 patients who underwent 64-slice non-enhanced MDCT and 1.5-T MRI of the cervical spine with a maximum time interval of 5 days between imaging were evaluated. The exclusion criteria were as follows: 1) scoliosis involving a vertebral column curvature greater than 15°, 2) extensive vertebral fractures resulting in difficulty in assessing axial images, 3) severe postoperative infection that could disrupt the border of the dural sac and paraspinal muscle, 4) previous cervical spinal surgery with metallic hardware, 5) ossification of the posterior longitudinal ligament, and 6) metastasis involving the cervical spine.
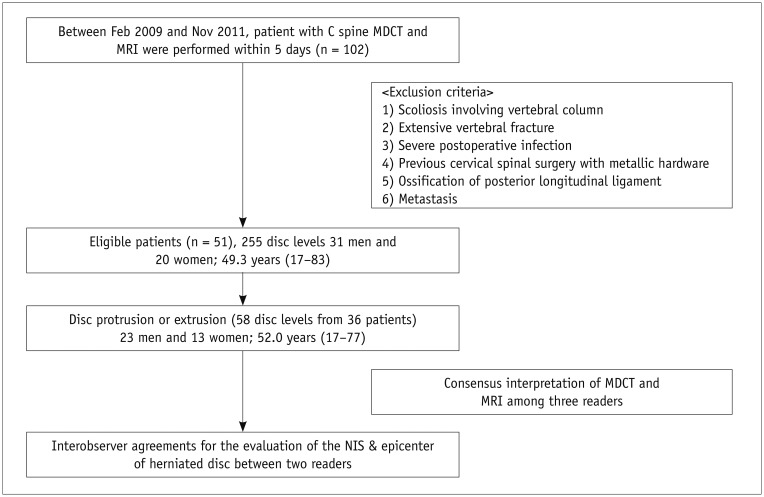
Two hundred and fifty-five segments from 51 patients were included in the current study. There were 31 males and 20 females, and the mean patient age was 49.3 years (range, 17-83 years) (Fig. 1).
Fig. 1. Study flow diagram.
MDCT = multidetector-row computed tomography, MRI = magnetic resonance imaging, NIS = number of involved segments
Imaging Study
CT examinations were performed at one center using a 64-slice MDCT system (Light speed VCT XTe; GE Medical Systems, Milwaukee, WI, USA). Axial scans were acquired at 140 kV and 100 mA for 3-mm-thick sections with a 0.984:1 (mm/rot) table feed and a 512 × 512 matrix. Sagittal reformatted images were obtained based on the transverse images with a 3-mm section thickness. Patients were examined in the supine position with both arms lying flat.
MRI was also performed at the same center using a 1.5-T MR unit (Signa HDxt; GE Medical Systems, Milwaukee, WI, USA) with a dedicated cervical spine surface coil. The protocol included sagittal fast spin-echo T1-weighted (repetition time [TR]/echo time [TE], 583/14 ms) and T2-weighted (TR/TE, 2800/114 ms) images with a 4-mm slice thickness, a 0.1-mm intersection gap, a 448 × 224 matrix, and a 320-mm field of view. Additionally, axial spin-echo T2-weighted (TR/TE, 4400/105 ms) images were obtained from the level of C2 through T1 with a 3.5-mm slice thickness, a 0.1-mm intersection gap, a 288 × 256 matrix, and a 150-mm field of view.
MRI and CT studies were performed with a maximum time interval of 5 days between imagings, and the order in which the imaging study modalities were used was not an issue. Twelve of the 51 patients underwent CT and MRI on the same day. Three of the 51 patients who complained of neurological pain, but who had no obvious trauma history, underwent MRI initially, and CT was performed within 5 days to allow surgical planning. Thirty-six of the 51 patients with trauma histories (minimal to severe) underwent CT first, followed by MRI. Images were stored in the Digital Imaging and Communications in Medicine format and viewed on the same picture archiving and communication system (DEJA-VIEW; Bucheon, Korea).
Image Interpretation
Image analysis was conducted independently in random order by three musculoskeletal radiologists (with 10 years of experience; with 8 years of experience; with 5 years of experience), who were blinded to the patient symptoms and clinical impressions. Prior to this study, to gain experience with the interpretation procedures, each reader independently reviewed and provided pictorial examinations of cervical spine MDCT and MRI for comparison in six patients. The readers independently and randomly analyzed two sets of MDCT and MR images from 51 patients as follows: 1) axial and sagittal images of MDCT and 2) cervical MR images, including axial and sagittal sections. To reduce possible memory of former images, each image set was reviewed with at least a 2-week interval between sessions of interpretation.
Five cervical disc levels were examined per patient at C2-3, C3-4, C4-5, C5-6, and C6-7, and a total of 255 disc levels were included in our study. The image interpretation results were recorded on multiple-choice lists of findings for images of each level. Reviewers were asked to record the disc contour at each level. The modified criteria of the North American Spine Society (NASS) were used to define disc contour features (14).
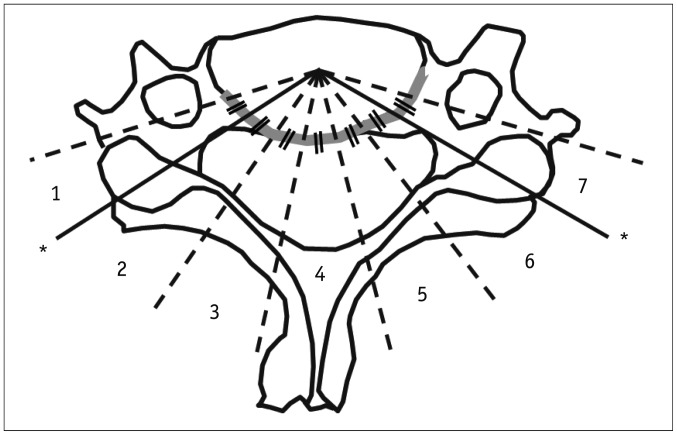
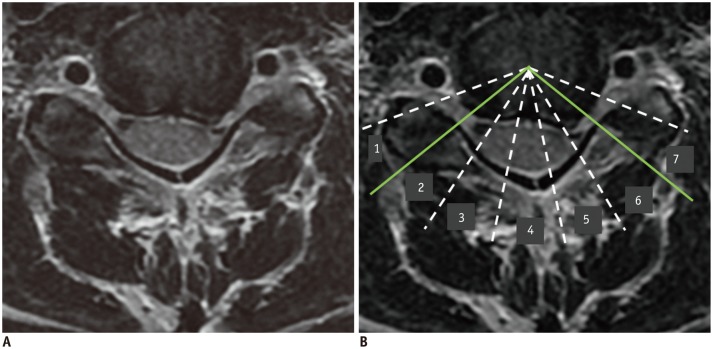
After independent evaluation, the three readers formed consensus interpretations on of the disc morphology on axial and sagittal MDCT images and MRI, and the extent of agreement between the two techniques was determined by reference to these consensus interpretations. Herniated discs (protrusion and extrusion) were selected from 255 disc levels at which the three readers agreed herniation was evident on both MDCT and MRI (Fig. 1). Also, an interpretation agreed upon by two readers was considered to be a consensus. If there were differences in disc morphological evaluation among the three readers, the disc levels were re-evaluated by all readers to attain a consensus interpretation. To evaluate the number of involved segments (NIS) and epicenter of herniated disc materials, the locations of the NIS and epicenter were recorded by two reviewers. Two imaginary lines were drawn by tracing the inner margin of the bilateral pedicles, and an additional four lines that divided the inter-pedicular space evenly were drawn. Furthermore, another two lines that also divided the same space at the lateral aspect of the lines drawn along the inner margin of the pedicles were drawn. As a result, eight virtual lines were drawn on the posterior aspect of the body of the cervical spine, and seven segments were created. Figure 2 shows a schematic of the seven segments. Next, the readers were asked to select the segment that showed the maximal extent of posterior herniation (Fig. 3). For the assessment of inter-modality agreement in terms of the NIS and epicenter of the herniated disc materials, 58 disc levels from 36 patients were selected. Twenty-three patients were males (mean age, 52.5 years; range, 17-77 years), and 13 were females (mean age, 51.23 years; range, 26-76 years); the mean age of all patients was 52.0 years (range, 17-77 years) (Fig. 1).
Fig. 2. Schematic of seven virtual segments of C-spine for evaluation of epicenter and number of involved segments of herniated disc materials.
Two imaginary lines (*) are drawn by tracing inner margin of bilateral pedicles, and additional four lines that divide inter-pedicular space evenly are drawn. Additionally, another two lines that divide same space at lateral aspect of lines drawn along inner margin of pedicles are drawn. As result, eight virtual lines are drawn on posterior aspect of body of cervical spine, and seven segments are created.
Fig. 3. Epicenter and number of involved segments (NIS) of herniated disc on MRI.
45-year-old female with left upper extremity tingling sensation. A. T2-weighted axial imaging shows disc protrusion at C5-6 level. B. Eight virtual lines delimit seven segments, and epicenter (6) and NIS (5, 6, and 7; i.e., three segments) of herniated disc material are determined.
Statistical Analysis
For the assessment of disc morphology according to the four-grade system, interobserver agreement among the three readers was evaluated using kappa statistics. In the evaluation of disc morphology according to the four-grade system, the inter-modality agreements between MDCT and MRI were evaluated by calculating kappa statistics. In addition, agreement between the two modalities was assessed using a two-step system featuring non-pathologic discs (normal and bulging) and truly herniated discs (protrusion and extrusion) (14).
To assess the rate of agreement in the NIS and epicenter measurements between MDCT and MRI, weighted kappa statistics were used. All kappa values were interpreted as proposed in the literature (15), as follows: lower than 0.00, poor agreement; 0.00-0.20, slight agreement; 0.21-0.40, fair agreement; 0.41-0.60, moderate agreement; 0.61-0.80, substantial agreement; and 0.81-1.00, almost perfect agreement. To analyze the inter-modality agreements between the four-grade and two-grade methods, the Z-test was used. Comparison of the inter-modality agreement between MDCT and MRI at each disc level was assessed using the Z-test. All statistical analysis was performed using statistical software (STATA, version 11.0; STATA, College Station, TX, USA). p values less than 0.05 were deemed to indicate a statistically significant difference.
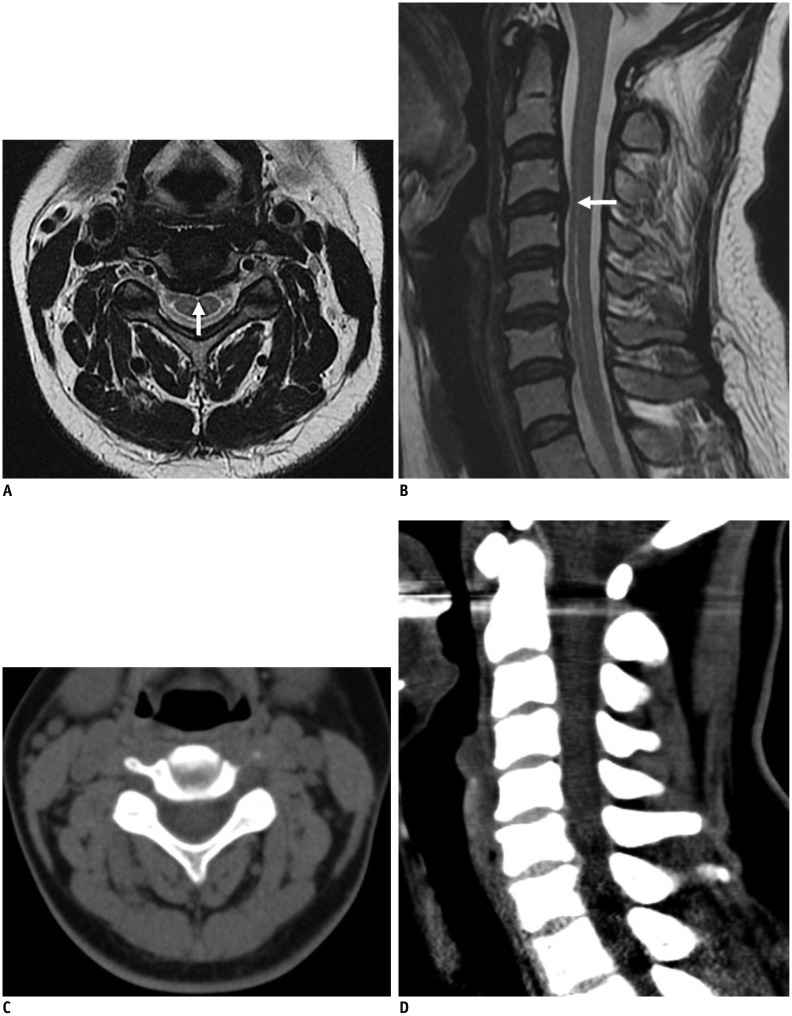
RESULTS
Table 1 shows the interobserver agreement in the evaluation of disc morphology among the three readers, revealing fair to moderate agreement (k = 0.39-0.53 on MDCT images; k = 0.45-0.56 on MRI). When disc morphology was categorized using a two-grade system (normal and bulging vs. protrusion and extrusion), the inter-modality agreement between MDCT and MRI was only moderate (k = 0.59). When disc morphology was categorized using a four-grade system, the inter-modality agreement between MDCT and MRI was substantial (k = 0.66) (Table 2). However, no significant difference in terms of agreement between MDCT and MRI findings was evident when the four- and two-grade systems were compared (p = 0.37). Compared with the MRI findings, 9 of 55 (16.4%) bulging discs, 26 of 79 (32.9%) disc protrusions, and 4 of 6 (66.7%) disc extrusions were underestimated on MDCT images, whereas 11 of 115 (9.6%) normal discs, 12 of 55 (21.8%) bulging discs, and 3 of 79 (3.8%) disc protrusions were overestimated on MDCT images (Table 2). In both the four- and two-grade systems, herniated disc lesions on MDCT images tended to be underestimated compared with MRI imaging findings (Fig. 4). The inter-modality agreement between MDCT and MRI increased slightly, to 82.4% (210/255), when the disc morphology was divided into non-pathologic (normal and bulging) and pathologic (protrusion and extrusion) presentations. Using the two-grade system, 27 of 85 (31.8%) disc herniations on MDCT findings were underestimated, whereas 18 of 160 non-pathologic discs on MDCT were overestimated, compared with MRI.
Table 1. Interobserver Agreement of Disc Morphology Based on MDCT and MRI Findings.
| Reader | MDCT | MRI |
|---|---|---|
| 1 vs. 2 | 0.46 (0.41-0.50) | 0.53 (0.48-0.57) |
| 1 vs. 3 | 0.53 (0.49-0.58) | 0.56 (0.52-0.60) |
| 2 vs. 3 | 0.39 (0.34-0.43) | 0.45 (0.40-0.49) |
Data are presented as k-values with 95% confidence intervals in parentheses. MDCT = multidetector-row computed tomography, MRI = magnetic resonance imaging
Table 2. Inter-Modality Agreement between MDCT and MRI Using Four-Grade System.
| MRI | Total (n) | ||||
|---|---|---|---|---|---|
| Normal (n) | Bulging (n) | Protrusion (n) | Extrusion (n) | ||
| MDCT | |||||
| Normal (n) | 104 | 9 | 8 | 0 | 121 |
| Bulging (n) | 5 | 34 | 18 | 1 | 58 |
| Protrusion (n) | 6 | 11 | 50 | 3 | 70 |
| Extrusion (n) | 0 | 1 | 3 | 2 | 6 |
| Total (n) | 115 | 55 | 79 | 6 | 255 |
k = 0.66 (95% confidence interval, 0.62-0.68). MDCT = multidetector-row computed tomography, MRI = magnetic resonance imaging
Fig. 4. Comparison of cervical MRI and MDCT in 43-year-old female with posterior neck pain.
Central disc protrusion is evident at C3-4 level on MRI (A, B; arrows). However, all readers interpreted disc as normal on MDCT (C, D). MDCT = multidetector-row computed tomography, MRI = magnetic resonance imaging
The inter-modality agreements for evaluation of the NIS and epicenter were substantial (k = 0.78 for the NIS and 0.79 for the epicenter). The interobserver agreements for the NIS and epicenter between two readers were substantial (k = 0.85 for CT and 0.88 for MRI; and k = 0.74 for CT and 0.70 for MRI, respectively).
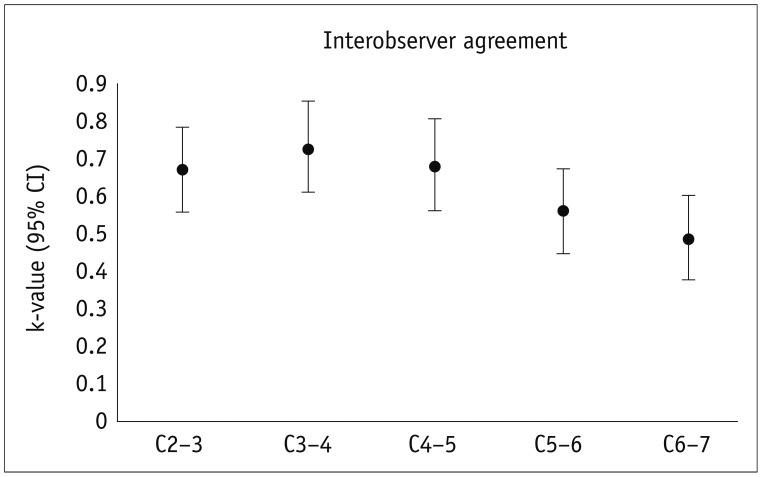
The respective interobserver agreement rates between MDCT and MRI findings according to disc level were determined; the kappa values of the C2-3, C3-4, C4-5, C5-6, and C6-7 disc levels were 0.67, 0.73, 0.68, 0.56, and 0.49, respectively. The highest k-value was for the C3-4 disc level, and the lowest for the C5-6 level, suggesting a decreasing trend from C3-4 to C6-7 (Fig. 5). However, no significant differences among the k-values were noted (p = 0.140-0.710).
Fig. 5. Inter-modality agreement rates between MDCT and MRI findings at five disc levels.
Kappa values of C2-3, C3-4, C4-5, C5-6, and C6-7 disc levels are 0.67, 0.73, 0.68, 0.56, and 0.49, respectively, as depicted by central dot with whiskers, indicating upper and lower limits of 95% CIs. Decreasing trend is observed from C3-4 to C6-7 disc level. CI = confidence interval, MDCT = multidetector-row computed tomography, MRI = magnetic resonance imaging
DISCUSSION
Observer variability is a major hurdle to radiologists in the assessment of discs due to the lack of consensus regarding the nomenclature of disc herniation (16).
MRI is very useful for evaluation of disc herniation, and it does not deliver any radiation to patients who are suffering from cervical radiculopathy (3,4,5,6). However, MRI requires almost 30 minutes to perform and is very sensitive to patient motion. CT requires less time to perform than MRI and is considered superior to MRI for evaluation of disc containment (e.g., bone) (7). We assessed the epicenter locations and the NIS of the herniated disc material on CT or MRI because accurate evaluation of the herniated discs is essential to determine the cause of the radiculopathy. Our results showed moderate and substantial agreement rates between MDCT and MRI findings in the evaluation of disc herniation. Although few similar studies (6,8) have investigated the agreement rate between CT and MRI in the evaluation of cervical disc disease, all of them employed CT myelography, which is rarely used in current clinical practice, making direct comparison between the previous and current studies difficult. Douglas-Akinwande et al. (7) recently compared the diagnostic performance of contrast-enhanced four-slice MDCT and MRI for assessment of the severity and cause of neural foraminal stenosis in patients with cervical radiculopathy. They found that contrast-enhanced MDCT and MRI showed similar diagnostic performance in the evaluation of patients with suspected neural foraminal stenosis.
Although we employed 64-slice MDCT, the agreement rate between the two imaging modalities was lower than that reported previously (7) for contrast-enhanced MDCT and MRI. Additionally, in the lumbar spine, a previous study of observer variation between non-contrast spiral CT and MRI found a moderate interobserver agreement rate in the evaluation of herniation or bulging discs in the lumbar spine based on spiral CT and MRI findings (16); this is consistent with our data. Therefore, we concluded that a moderate-to-substantial agreement rate between MDCT and MRI is acceptable, considering the use of non-contrast enhanced MDCT. In addition, the effect of using advanced MDCT was limited in terms of improving inter-modality agreement.
The morphological analysis using the four-grade and two-grade systems revealed that CT imaging findings were more likely to be underestimated rather than overestimated compared with MRI findings. However, no significant difference was found in the NIS and epicenter of the herniated discs between MDCT and MRI findings.
Our study employed an objective method of assessing the NIS and epicenter of herniated disc materials by dividing the area of the posterior disc material into seven segments, which might supplement a conventional disc grading system. The analysis revealed a substantial inter-modality agreement, similar to that of a conventional disc grading system, thus the modified criteria of the NASS.
Although a significant difference was found at each level of the cervical spine, our data indicated that the inter-modality agreement rates among five disc levels showed a tendency to decrease at the lower level of the cervical spine. Indeed, the k-values were lowest at the C5-6 and C6-7 levels. This may be due to degradation of CT by beam-hardening artifacts and excess attenuation at the base of the neck due to the bulky shoulder girdle (12,17). Even with use of 64-slice MDCT, this beam hardening at the base of neck remains a challenge to radiologists in the evaluation of lower cervical discs.
Our study possessed several limitations. First, it was of a retrospective design. Second, relatively few actual disc pathologies were included. Third, no surgical standard was used to confirm image-based diagnoses, raising the possibility of bias, which would limit generalization of the results. However, because the main purpose of our study was to evaluate the inter-modality agreement between MDCT and MRI, the final surgical result was not necessary to compare the MDCT and MRI findings. Fourth, MDCT is considered superior to MRI for determination of disc containment (e.g., bone) (7). Because we did not obtain the final surgical findings, we could not analyze the containment of herniated disc material on MDCT and MRI. Further investigation is needed to compare the containment of disc material between MDCT and MRI findings. Another limitation is the relatively few patients with disc extrusions, which may reduce the statistical power. Finally, we used the nomenclature of NASS for the evaluation of cervical discs, but this was designed for lumbar disc pathology. Thus, a different result might be obtained using actual disc pathology.
In conclusion, MDCT and MRI show a moderate-to-substantial degree of inter-modality agreement for the assessment of herniated cervical discs. MDCT images have a tendency to underestimate the anterior posterior extent of the herniated discs compared with MRI findings. Recognition of the difference in interpretation of cervical disc pathology between MDCT and MRI findings may provide useful information for clinical work up of patients with cervical radiculopathy.
Footnotes
This work was supported by the Soonchunhyang University Research Fund.
References
- 1.Lunsford LD, Bissonette DJ, Jannetta PJ, Sheptak PE, Zorub DS. Anterior surgery for cervical disc disease. Part 1: Treatment of lateral cervical disc herniation in 253 cases. J Neurosurg. 1980;53:1–11. doi: 10.3171/jns.1980.53.1.0001. [DOI] [PubMed] [Google Scholar]
- 2.Radhakrishnan K, Litchy WJ, O'Fallon WM, Kurland LT. Epidemiology of cervical radiculopathy. A population-based study from Rochester, Minnesota, 1976 through 1990. Brain. 1994;117(Pt 2):325–335. doi: 10.1093/brain/117.2.325. [DOI] [PubMed] [Google Scholar]
- 3.Daniels DL, Grogan JP, Johansen JG, Meyer GA, Williams AL, Haughton VM. Cervical radiculopathy: computed tomography and myelography compared. Radiology. 1984;151:109–113. doi: 10.1148/radiology.151.1.6701298. [DOI] [PubMed] [Google Scholar]
- 4.Shim JH, Park CK, Lee JH, Choi JW, Lee DC, Kim DH, et al. A comparison of angled sagittal MRI and conventional MRI in the diagnosis of herniated disc and stenosis in the cervical foramen. Eur Spine J. 2009;18:1109–1116. doi: 10.1007/s00586-009-0932-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Miyazaki M, Hong SW, Yoon SH, Morishita Y, Wang JC. Reliability of a magnetic resonance imaging-based grading system for cervical intervertebral disc degeneration. J Spinal Disord Tech. 2008;21:288–292. doi: 10.1097/BSD.0b013e31813c0e59. [DOI] [PubMed] [Google Scholar]
- 6.Yousem DM, Atlas SW, Hackney DB. Cervical spine disk herniation: comparison of CT and 3DFT gradient echo MR scans. J Comput Assist Tomogr. 1992;16:345–351. [PubMed] [Google Scholar]
- 7.Douglas-Akinwande AC, Rydberg J, Shah MV, Phillips MD, Caldemeyer KS, Lurito JT, et al. Accuracy of contrast-enhanced MDCT and MRI for identifying the severity and cause of neural foraminal stenosis in cervical radiculopathy: a prospective study. AJR Am J Roentgenol. 2010;194:55–61. doi: 10.2214/AJR.09.2988. [DOI] [PubMed] [Google Scholar]
- 8.Larsson EM, Holtås S, Cronqvist S, Brandt L. Comparison of myelography, CT myelography and magnetic resonance imaging in cervical spondylosis and disk herniation. Pre- and postoperative findings. Acta Radiol. 1989;30:233–239. [PubMed] [Google Scholar]
- 9.Hudgins WR. Computer-aided diagnosis of lumbar disc herniation. Spine (Phila Pa 1976) 1983;8:604–615. doi: 10.1097/00007632-198309000-00006. [DOI] [PubMed] [Google Scholar]
- 10.Modic MT, Masaryk T, Boumphrey F, Goormastic M, Bell G. Lumbar herniated disk disease and canal stenosis: prospective evaluation by surface coil MR, CT, and myelography. AJR Am J Roentgenol. 1986;147:757–765. doi: 10.2214/ajr.147.4.757. [DOI] [PubMed] [Google Scholar]
- 11.Thornbury JR, Fryback DG, Turski PA, Javid MJ, McDonald JV, Beinlich BR, et al. Disk-caused nerve compression in patients with acute low-back pain: diagnosis with MR, CT myelography, and plain CT. Radiology. 1993;186:731–738. doi: 10.1148/radiology.186.3.8267688. [DOI] [PubMed] [Google Scholar]
- 12.Dorwart RH, LaMasters DL. Applications of computed tomographic scanning of the cervical spine. Orthop Clin North Am. 1985;16:381–393. [PubMed] [Google Scholar]
- 13.Wilson DW, Pezzuti RT, Place JN. Magnetic resonance imaging in the preoperative evaluation of cervical radiculopathy. Neurosurgery. 1991;28:175–179. doi: 10.1097/00006123-199102000-00001. [DOI] [PubMed] [Google Scholar]
- 14.Fardon DF, Milette PC, Combined Task Forces of the North American Spine Society, American Society of Spine Radiology, and American Society of Neuroradiology Nomenclature and classification of lumbar disc pathology. Recommendations of the Combined task Forces of the North American Spine Society, American Society of Spine Radiology, and American Society of Neuroradiology. Spine (Phila Pa 1976) 2001;26:E93–E113. doi: 10.1097/00007632-200103010-00006. [DOI] [PubMed] [Google Scholar]
- 15.Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33:159–174. [PubMed] [Google Scholar]
- 16.van Rijn JC, Klemetso N, Reitsma JB, Bossuyt PM, Hulsmans FJ, Peul WC, et al. Observer variation in the evaluation of lumbar herniated discs and root compression: spiral CT compared with MRI. Br J Radiol. 2006;79:372–377. doi: 10.1259/bjr/26216335. [DOI] [PubMed] [Google Scholar]
- 17.Kane AG, Reilly KC, Murphy TF. Swimmer's CT: improved imaging of the lower neck and thoracic inlet. AJNR Am J Neuroradiol. 2004;25:859–862. [PMC free article] [PubMed] [Google Scholar]