The occurrence of a giant hepatic artery aneurysm (GHAA) in a patient with systemic vasculitis is very rare. Herein, we describe our endovascular treatment experience of a GHAA associated with immunoglobulin G4-related disease (IgG4-RD) consisting primarily of a liquid embolic injection and deployment of a vascular plug.
A 69-year-old man underwent a contrast-enhanced abdominal computed tomography scan due to abdominal pain during a re-acutized phase of IgG4-related kidney Editordisease. The examination revealed a 10 × 4 cm giant aneurysm extending from the common hepatic artery to the proximal tract of the right and left hepatic arteries. Moreover, an ectatic celiac trunk measuring 2.2 cm in diameter was also detected (Fig. 1). The decision was made to treat the GHAA with an endovascular technique, given the patient's hemodynamic stability. Color Doppler ultrasound was performed and detected reduced and demodulated blood flow through the giant aneurysm, whereas intrahepatic portal flow was normal in direction and velocity. A selective common hepatic arteriogram was arranged, the double inflow-outflow blockage technique was performed, and a non-adhesive liquid embolic ethylene-vinyl alcohol agent (Onyx® LES, Covidien, Paris, France) was injected selectively at the origin of the right hepatic, left hepatic, and gastroduodenal arteries. Onyx was also injected inside the sac, followed by inserting 20 cm fragments cut from a Teflon-coated standard angiographic guidewire with the inner core removed. In-flow was stopped at the proximal neck using a detachable vascular plug (Amplatzer vascular plug-AVP; AGA Medical, Golden Valley, MN, USA) (Fig. 2). The procedure was uneventful, and the patient was discharged within a few days with improved renal function. He has been monitored for IgG4-RD, celiac trunk diameter, and GHAA thrombosis and evolution for 7 months.
Fig. 1. Computed tomography angiography: volume rendering reconstruction showing 10 × 4 cm giant aneurysm involving common, proper, right and left hepatic arteries, with short proximal neck at origin from celiac trunk.

Fig. 2. Celiac trunk angiography showing complete exclusion of giant hepatic artery aneurysm.
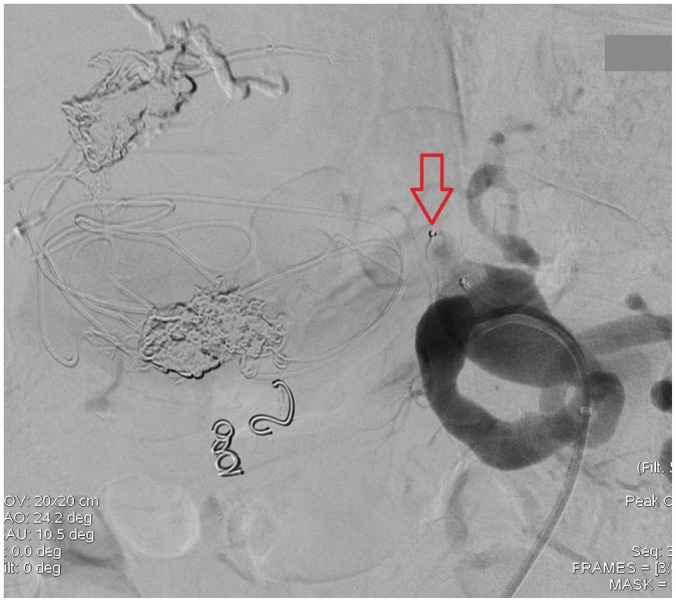
Liquid agent (Onyx) used for embolization is evident at origin of right hepatic, left hepatic, and gastroduodenal arteries. Red arrow indicates Amplatzer vascular plug occluding proximal neck of aneurysm.
A visceral aneurysm occurring in a patient with IgG4-RD is extremely rare, except those in the aorta and coronary arteries. As of 2015, only two cases have been described involving the hepatic artery and neither was classified as giant (1). Endovascular or surgical treatment is recommended for hepatic artery aneurysms (HAAs) > 2 cm because of their high tendency to rupture (2). GHAA is a more life-threatening condition than HAA, and a rupture leading to certain death can occur if left untreated (2). Several types of treatment have been described for GHAAs (3,4,5). Open aneurysmectomy without vascular reconstruction is performed most frequently for GHAAs in a hemodynamically unstable patient or one with vascular anatomy anomalies. Arterial reconstruction is mandatory if ischemia of a visceral organ occurs. Furthermore, liver transplantation has been conducted in rare and selected cases of GHAAs. Otherwise, endovascular techniques are becoming a cogent option to treat GHAAs. Among these, endovascular exclusion with a stent graft or an Amplatzer vascular plug has been successful (3,4,5). In contrast to an HAA, coil embolization or coil packing appears to be a less reliable procedure for GHAAs, as a complete thrombosis occurred in an enlarged GHAA on a post-embolization angiogram in a case reported previously (3). Applying a liquid embolic agent, such as ethylene-vinyl alcohol (Onyx), to manage a visceral artery aneurysm is a safe and minimally invasive technique but its use for a GHAA has not been reported previously. However, we recommend considering use of a liquid embolic agent for giant visceral aneurysms of the abdominal cavity, provided the patient is hemodynamically stable, the aneurysm is crackless, the interventional radiologist is experienced, and the operating room has been alerted.
References
- 1.Vlachou PA, Khalili K, Jang HJ, Fischer S, Hirschfield GM, Kim TK. IgG4-related sclerosing disease: autoimmune pancreatitis and extrapancreatic manifestations. Radiographics. 2011;31:1379–1402. doi: 10.1148/rg.315105735. [DOI] [PubMed] [Google Scholar]
- 2.Rebonato A, Rossi M, Rebonato S, Cagini L, Scialpi M. Giant hepatic artery aneurysm: a fatal evolution. J Emerg Med. 2013;45:e217–e219. doi: 10.1016/j.jemermed.2013.05.069. [DOI] [PubMed] [Google Scholar]
- 3.Cavalcante RN, Couto VA, da Fonsecaa AV, de Miranda RB, Costa AJ, Correa JA. Endovascular treatment of a giant hepatic artery aneurysm with Amplatzer vascular plug. J Vasc Surg. 2014;60:500–502. doi: 10.1016/j.jvs.2013.06.077. [DOI] [PubMed] [Google Scholar]
- 4.Rossi M, Rebonato A, Citone M, La Torre M, David V. Common hepatic artery aneurysm successfully treated with a celiac axis stent graft. Two years of follow up. Eur J Radiol Extra. 2010;75:e125–e128. [Google Scholar]
- 5.Rossi M, Rebonato A, Greco L, Citone M, David V. Endovascular exclusion of visceral artery aneurysms with stent-grafts: technique and long-term follow-up. Cardiovasc Intervent Radiol. 2008;31:36–42. doi: 10.1007/s00270-007-9167-6. [DOI] [PubMed] [Google Scholar]


