Abstract
Extracorporeal life support (ECLS) is a type of cardiopulmonary bypass. It is an artificial means of supplying oxygen and removing CO2 on behalf of damaged lungs while patients are recovering from underlying diseases. Recently, the use of ECLS is rapidly increasing as this machine becomes smaller, less invasive and easier to use. In addition, the improvement of clinicians' technique and outcome is increasing their application to patients with acute respiratory distress. In this regard, the purpose of this review is to introduce the physiological principles, risk factors, and advantages of ECLS, clinical rationale for using ECLS, ventilatory strategy during ECLS, which are still causing different opinions, the weaning from ECLS, and the use of anticoagulant.
Keywords: Respiratory Distress Syndrome, Adult; Extracorporeal Membrane Oxygenation
What Is Extracorporeal Life Support?
Extracorporeal life support (ECLS), in particular, veno-venous (VV) extracorporeal membrane oxygenation (ECMO) is currently used as rescue therapy on patients with severe acute respiratory distress syndrome (ARDS) or severe hypoxia. Over the last five years, bridge therapy using ECLS has shown good clinical outcomes1,2.
The basic principle of ECLS is that while a pump (from semi-occlusive roller-head device to centrifugal pump) drives blood flow through an oxygenator (from silicone membrane to polymethylpentene fibers) via the extracorporeal circuit, the blood interacts with constant flow of oxygen at a specific speed using sweep-gas flows (Table 1)3. Extracorporeal oxygenation and CO2 removal are determined by three factors: extracorporeal blood flow rate controlled by the centrifugal-pump speed, sweep-gas flow rate controlled by a flow meters, and oxygen tension within the sweep gas controlled by a gas blender (Table 2)3.
Table 1. ECMO vs. ECCO2R.
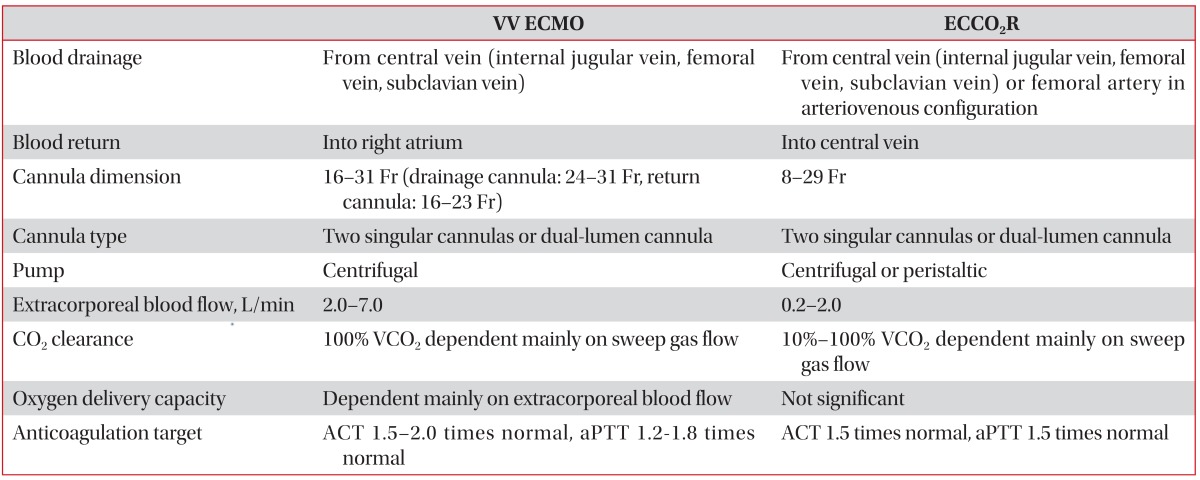
Adopted from Del Sorbo L et al. Lancet Respir Med 2014;2:154-64, with permission of Elsevier3.
ECMO: extracorporeal membrane oxygenation; ECCO2R: extracorporeal CO2 removal; VV: veno-venous; VCO2: CO2 production; ACT: activated clotting time; aPTT: activated partial thromboplastin time.
Table 2. Characteristics of gas exchange and hemodynamic support during ECLS.
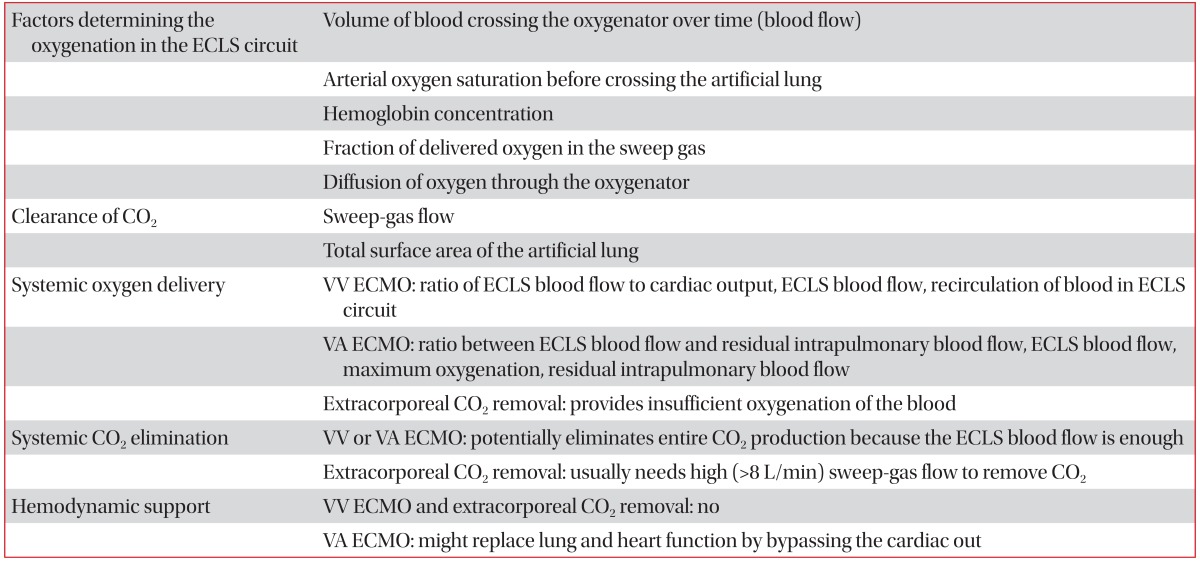
Adopted from Del Sorbo L et al. Lancet Respir Med 2014;2:154-64, with permission of Elsevier3.
ECLS: extracorporeal life support; VV ECMO: veno-venous extracorporeal membrane oxygenation; VA: veno-arterial.
The ECLS strategy which is mostly applied to ARDS patients is VV ECMO, but a switch to veno-arterial ECMO can be considered if reduced cardiac function is accompanied or hypoxia progresses even during the use of VV ECMO4.
As extracorporeal CO2 removal (ECCO2R) requires low blood flow rates (1-2 L/min), small cannulas, and less anticoagulation to remove CO2, it is more convenient to deal with than ECMO5. Because of low blood flow rates, oxygen is supplied by a patient's own lungs. As another type, the pumpless arteriovenous extracorporeal circuit is also used. Here, extracorporeal blood flows are caused by the native arteriovenous pressure gradient (≥60 mm Hg)6.
Considerations in Adult Patients with Respiratory Failure
There are no standardized criteria for the application of ECLS. However, it is mostly applied for rescue therapy on refractory hypoxia or hypercapnia or for ultra-protective ventilator strategies for the prevention of ventilator-induced lung injury (VILI). High ECMO flow rates (3-7 L/min) are required to improve oxygenation, and low flow rates (500-1,500 mL/min) are sufficient to remove CO2 effectively. Indication of ECLS should be decided after considering the risk-benefit ratio by multidisciplinary discussions.
1. Extracorporeal membrane oxygenation
Factors deciding the application of ECLS in patients with respiratory failure are the oxygenation index, PaO2/FiO2, Murray score, and refractory hypercapnia with acidosis (Table 3).
Table 3. VV ECMO for rescue treatment in patients with acute respiratory distress syndrome3.
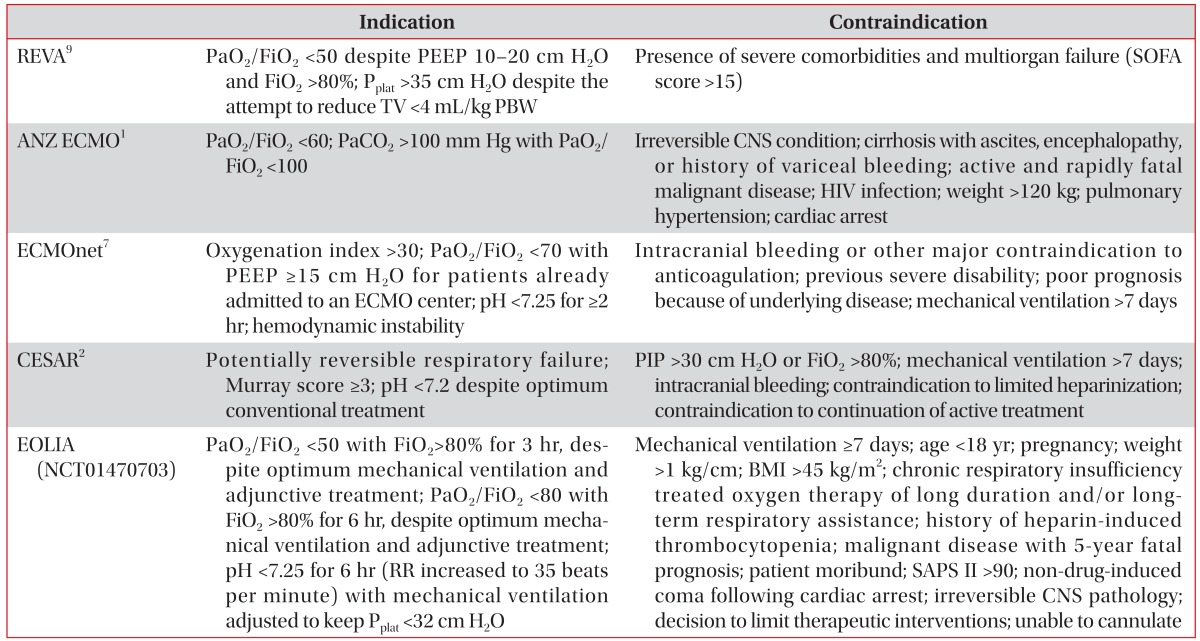
Adopted from Del Sorbo L et al. Lancet Respir Med 2014;2:154-64, with permission of Elsevier3.
VV ECMO: veno-venous extracorporeal membrane oxygenation; PaO2: arterial partial pressure of O2; FiO2: fraction of inspired oxygen; PEEP: positive end-expiratory pressure; TV: tidal volume; PBW: predicted body weight; SOFA: sequential organ failure assessment score; CNS: central nervous system; HIV: human immunodeficiency virus; RR: respiratory rate; BMI: body mass index; SAPS II: Simplified Acute Physiology Score.
In 2009 H1N1 influenza epidemic, many centers applied ECMO to patients with severe ARDS and refractory hypoxia. Australia and New Zealand Extracorporeal Membrane Oxygenation (ANZ ECOMO) Influenza Investigators1 reported a survival rate of 75% in the ECMO treatment group. The Italian ECMO Network also showed a survival rate of 68% in the ECMO treatment group7. The Swine Flu Triage (SWiFT) study, done in the UK showed the lower in-hospital mortality in the ECMO treatment group (24% vs. 53%, p=0.006)8. In the CESAR trial, severe ARDS patients also showed the higher survival rate in the ECMO treatment group (63% vs. 47%, p=0.03)2.
The above results suggested that the implementation of protective mechanical ventilation during ECMO can improve the prognosis.
EOLIA (NCT01470703) should help to define the clinical efficacy of VV ECMO in severe ARDS patients.
2. Extracorporeal CO2 removal
Recent studies reported that the application of ECCO2R in ARDS patients can reduce the lung injury as it enables the ultraprotective strategies of mechanical ventilation (Table 4). Zimmermann et al.6 reported that when pumpless AV ECLS was applied to 51 patients with ARDS, low tidal volume ventilation could be maintained along with the continuous removal of CO2, and the survival rate was 50%.
Table 4. Clinical studies of ECLS to prevent ventilator-induced lung injury3.
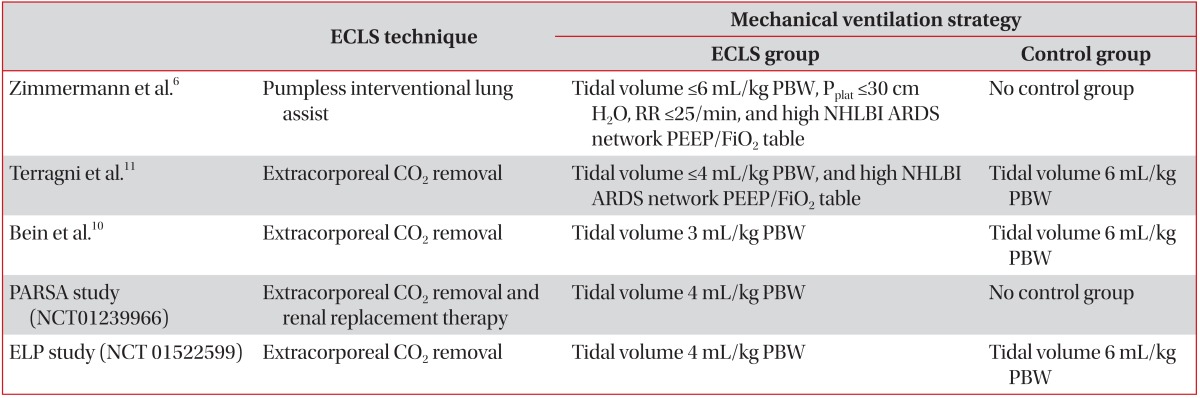
Adopted from Del Sorbo L et al. Lancet Respir Med 2014;2:154-64, with permission of Elsevier3.
ECLS: extracorporeal life support; PBW: predicted bodyweight; Pplat: inspiratory plateau pressure; RR: respiratory rate; NHLBI: National Heart, Lung, and Blood Institute; ARDS: acute respiratory distress syndrome; PEEP: positive end-expiratory pressure; FiO2: fraction of inspired oxygen.
A randomized, controlled study was done to compare an ultra-protective mechanical ventilation (3 mL/kg predicted body weight [PBW] with Pumpless AV ECLS) with low tidal volume ventilation (6 mL/kg PBW) strategies in 79 patients with ARDS. While the two groups did not differ for in-hospital mortality, within the patient group with PF ratio <200, the ultra-protective group showed an improved survival10. At present, studies on the efficacy of very low tidal volumes ventilation strategies during ECCO2R are working in progress.
Controversies
1. Mechanical ventilation strategies
For minimizing VILI, the ventilator settings during VV ECMO should be maintained at low levels to enable the prevention of atelectasis while keeping the alveoli open. However, there are no specific recommendations other than the maintenance of positive end-expiratory pressure (PEEP) at 10 cm H2O or above. As the injured lungs contribute little to oxygenation, lung recruitment using PEEP while maintaining minimal tidal volumes might accelerate lung healing or optimise cardiopulmonary function12,13.
In the CESAR trial, lung rest was induced by limitation of the peak inspiratory pressure to 20 cm H2O with PEEP 10 cm H2O, 10 breaths per minute, and FiO2 of 30%. Another study also showed positive outcomes in patients who maintained a mean plateau pressure of 25 cm H2O9.
After the acute phase of the illness, mechanical ventilation with spontaneous breathing should be considered to reduce the use of sedatives and to improve the diaphragmatic function14,15.
2. Tracheostomy
In the case of applying ECLS due to severe ARDS, mechanical ventilation for a long period of time is predicted. Therefore, the early tracheostomy might be considered. The use of anticoagulants during ECLS is not the contraindication for tracheostomy. In a recent study, a tracheostomy with the percutaneous dilatational technique done by experienced physician is safe with a brief interruption of anticoagulation. In this study, no major complications such as death were observed16.
3. Weaning from ECLS (Table 5)17
Table 5. Weaning from ECMO.
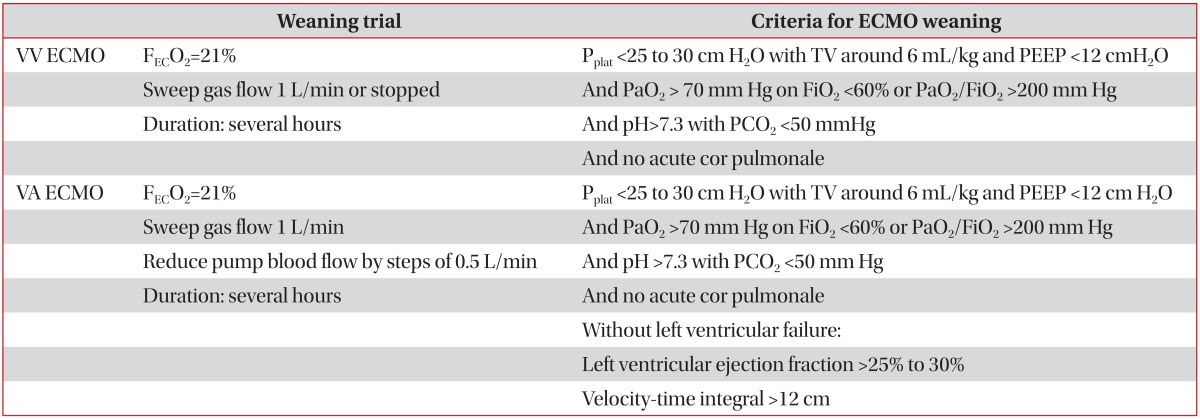
Adopted from Richard C et al. Ann Intensive Care 2014;4:15, according to the Creative Commons License17.
ECMO: extracorporeal membrane oxygenation; VV: veno-venous; FECO2: oxygen fraction delivered by the extracorporeal circuit; Pplat: plateau pressure; TV: tidal volume; PEEP: positive end-expiratory pressure; PaO2: arterial partial pressure of O2; FiO2: fraction of inspired oxygen; PCO2: partial pressure of CO2; VA: venous-arterial.
When mechanical ventilation settings is acceptable (tidal volume <6 mL/Kg PBW, plateau pressure <30 cm H2O, PEEP <12 cm H2O, FiO2 <60%) and respiratory mechanics, gas exchanges, and radiographic findings are improved, weaning from ECLS can be considered. Before weaning, the existence of acute cor pulmonale should be identified. Two main strategies of weaning can be used: reducing sweep-gas flow rates or reducing extracorporeal blood-flow rates. Alternatively, weaning of mechanical ventilation may be considered earlier than weaning from ECLS18,19.
4. Sedation
While deep sedation and neuromuscular blockade might be required in the initial stages to relieve symptoms and reduce oxygen consumption, patients should be kept awake to actively participate in rehabilitation therapy during ECLS. In addition, early mobilization could suppress the progression of weakness and reduce the incidence of delirium.
The indication for the use of awake ECMO, instead of invasive mechanical ventilation is not confirmed in patients with ARDS refractory to non-invasive ventilation. However, the use of awake ECMO as a bridge before lung transplantation has shown promising results20,21,22,23. Mechanical ventilation and sedation might worsen outcomes before and after the transplantation. Awake ECMO enables patients to communicate, eat, and walk and improves physical and physiological conditions.
5. Technological advances
The first technological advances in this field may be the production of bicaval dual-lumen cannulas24. This cannula is inserted via the right internal jugular vein, and then drains blood from the superior and inferior vena cava through one lumen and returns blood into the right atrium through a second lumen. Only one cannulation enables patients to receive intensive physiotherapy more conveniently. Second, reduction in the size of ECLS equipment has enabled patients receiving ECLS to transfer and mobilise25.
6. Anticoagulantion and transfusion
Although the ECLS circuits are engineered with biocompatible materials, the systemic anticoagulants are still required to prevent thrombotic complication. Unfractionated heparin is most commonly used and monitoring is performed using activated partial thromboplastin time (1.2-1.5 times control), anti-Xa activity (0.2-0.4 IU/mL), or the activated clotting time. When heparin-induced thrombocytopenia is suspected, argatroban or bivalirudin can be used as alternatives26.
The guidelines of the Extracorporeal Life Support Organization (ELSO) recommend maintaining normal hemoglobin concentration for tissue oxygenation. However, some centers is more restrictive to transfusion thresholds in critically ill patients (Hb <7 g/dL).
7. Evaluation of prognosis
ELSO has recently announced the Respiratory ECMO Survival Prediction (RESP) score using data extracted from the ELSO international registry. This score can be a good tool to predict survival for patients receiving ECMO for respiratory (Table 6)27.
Table 6. RESP score.
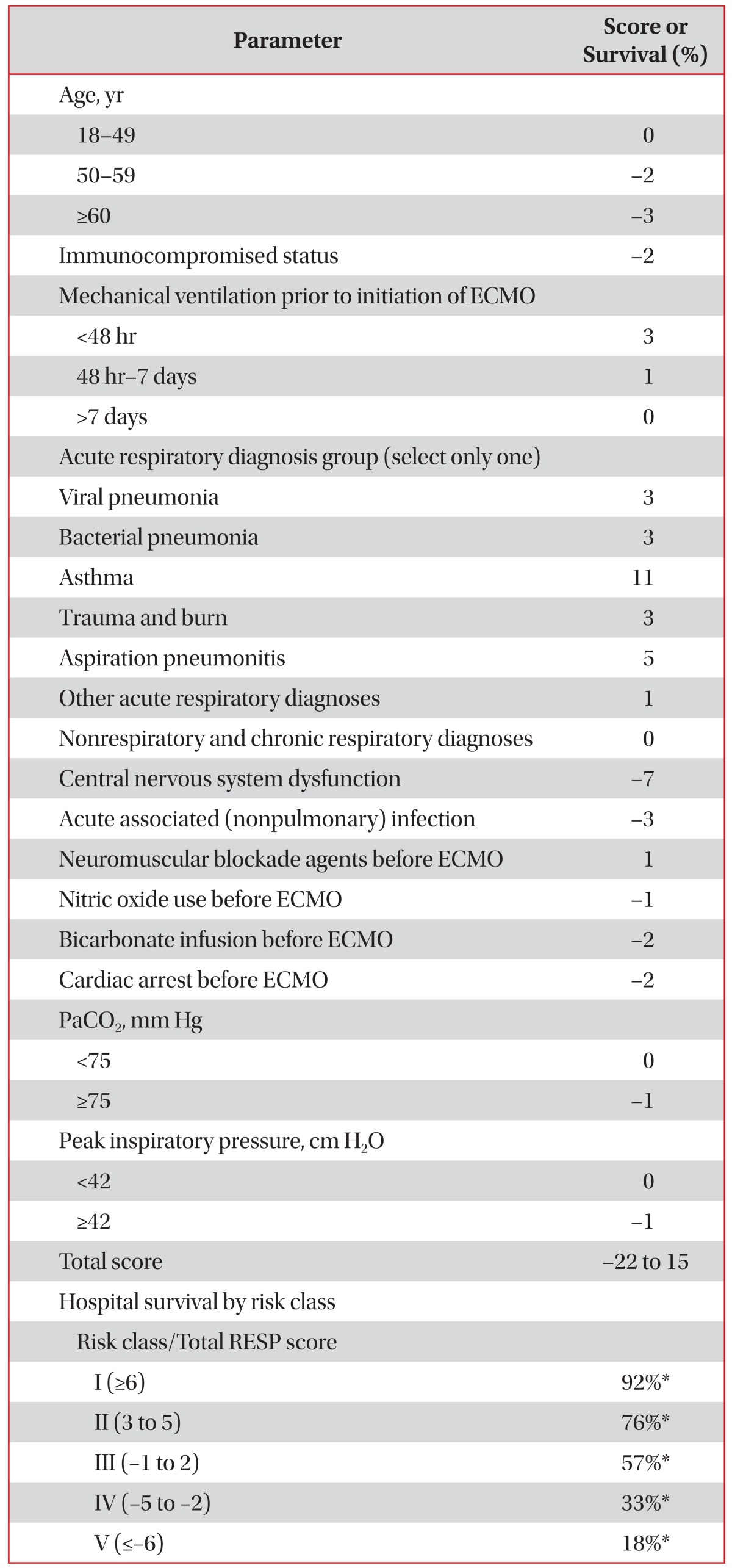
Reprinted with permission of the American Thoracic Society. Copyright © 2015 American Thoracic Society. Schmidt M et al. Predicting survival after extracorporeal membrane oxygenation for severe acute respiratory failure. The Respiratory Extracorporeal Membrane Oxygenation Survival Prediction (RESP) score. Am J Respir Crit Care Med 2014;189:1374-8227. The American Journal of Respiratory and Critical Care Medicine is an official journal of the American Thoracic Society.
*Survival (%).
RESP: Respiratory ECMO Survival Prediction; ECMO: extracorporeal membrane oxygenation; PaCO2:partial pressure of carbon dioxide.
Footnotes
Conflicts of Interest: No potential conflict of interest relevant to this article was reported.
References
- 1.Australia and New Zealand Extracorporeal Membrane Oxygenation (ANZ ECMO) Influenza Investigators. Davies A, Jones D, Bailey M, Beca J, Bellomo R, et al. Extracorporeal membrane oxygenation for 2009 influenza A(H1N1) acute respiratory distress syndrome. JAMA. 2009;302:1888–1895. doi: 10.1001/jama.2009.1535. [DOI] [PubMed] [Google Scholar]
- 2.Peek GJ, Mugford M, Tiruvoipati R, Wilson A, Allen E, Thalanany MM, et al. Efficacy and economic assessment of conventional ventilatory support versus extracorporeal membrane oxygenation for severe adult respiratory failure (CESAR): a multicentre randomised controlled trial. Lancet. 2009;374:1351–1363. doi: 10.1016/S0140-6736(09)61069-2. [DOI] [PubMed] [Google Scholar]
- 3.Del Sorbo L, Cypel M, Fan E. Extracorporeal life support for adults with severe acute respiratory failure. Lancet Respir Med. 2014;2:154–164. doi: 10.1016/S2213-2600(13)70197-8. [DOI] [PubMed] [Google Scholar]
- 4.Gattinoni L, Carlesso E, Langer T. Clinical review: extracorporeal membrane oxygenation. Crit Care. 2011;15:243. doi: 10.1186/cc10490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cove ME, MacLaren G, Federspiel WJ, Kellum JA. Bench to bedside review: extracorporeal carbon dioxide removal, past present and future. Crit Care. 2012;16:232. doi: 10.1186/cc11356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zimmermann M, Bein T, Arlt M, Philipp A, Rupprecht L, Mueller T, et al. Pumpless extracorporeal interventional lung assist in patients with acute respiratory distress syndrome: a prospective pilot study. Crit Care. 2009;13:R10. doi: 10.1186/cc7703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Patroniti N, Zangrillo A, Pappalardo F, Peris A, Cianchi G, Braschi A, et al. The Italian ECMO network experience during the 2009 influenza A(H1N1) pandemic: preparation for severe respiratory emergency outbreaks. Intensive Care Med. 2011;37:1447–1457. doi: 10.1007/s00134-011-2301-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Noah MA, Peek GJ, Finney SJ, Griffiths MJ, Harrison DA, Grieve R, et al. Referral to an extracorporeal membrane oxygenation center and mortality among patients with severe 2009 influenza A(H1N1) JAMA. 2011;306:1659–1668. doi: 10.1001/jama.2011.1471. [DOI] [PubMed] [Google Scholar]
- 9.Pham T, Combes A, Roze H, Chevret S, Mercat A, Roch A, et al. Extracorporeal membrane oxygenation for pandemic influenza A (H1N1)-induced acute respiratory distress syndrome: a cohort study and propensity-matched analysis. Am J Respir Crit Care Med. 2013;187:276–285. doi: 10.1164/rccm.201205-0815OC. [DOI] [PubMed] [Google Scholar]
- 10.Bein T, Weber-Carstens S, Goldmann A, Muller T, Staudinger T, Brederlau J, et al. Lower tidal volume strategy (approximately 3 ml/kg) combined with extracorporeal CO2 removal versus 'conventional' protective ventilation (6 ml/kg) in severe ARDS: the prospective randomized Xtravent-study. Intensive Care Med. 2013;39:847–856. doi: 10.1007/s00134-012-2787-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Terragni PP, Del Sorbo L, Mascia L, Urbino R, Martin EL, Birocco A, et al. Tidal volume lower than 6 ml/kg enhances lung protection: role of extracorporeal carbon dioxide removal. Anesthesiology. 2009;111:826–835. doi: 10.1097/ALN.0b013e3181b764d2. [DOI] [PubMed] [Google Scholar]
- 12.Lachmann B. Open up the lung and keep the lung open. Intensive Care Med. 1992;18:319–321. doi: 10.1007/BF01694358. [DOI] [PubMed] [Google Scholar]
- 13.Vieillard-Baron A, Jardin F. Right level of positive end-expiratory pressure in acute respiratory distress syndrome. Am J Respir Crit Care Med. 2003;167:1576. doi: 10.1164/ajrccm.167.11.952. [DOI] [PubMed] [Google Scholar]
- 14.Putensen C, Zech S, Wrigge H, Zinserling J, Stuber F, Von Spiegel T, et al. Long-term effects of spontaneous breathing during ventilatory support in patients with acute lung injury. Am J Respir Crit Care Med. 2001;164:43–49. doi: 10.1164/ajrccm.164.1.2001078. [DOI] [PubMed] [Google Scholar]
- 15.Marini JJ. Spontaneously regulated vs. controlled ventilation of acute lung injury/acute respiratory distress syndrome. Curr Opin Crit Care. 2011;17:24–29. doi: 10.1097/MCC.0b013e328342726e. [DOI] [PubMed] [Google Scholar]
- 16.Braune S, Kienast S, Hadem J, Wiesner O, Wichmann D, Nierhaus A, et al. Safety of percutaneous dilatational tracheostomy in patients on extracorporeal lung support. Intensive Care Med. 2013;39:1792–1799. doi: 10.1007/s00134-013-3023-8. [DOI] [PubMed] [Google Scholar]
- 17.Richard C, Argaud L, Blet A, Boulain T, Contentin L, Dechartres A, et al. Extracorporeal life support for patients with acute respiratory distress syndrome: report of a Consensus Conference. Ann Intensive Care. 2014;4:15. doi: 10.1186/2110-5820-4-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.MacLaren G, Combes A, Bartlett RH. Contemporary extracorporeal membrane oxygenation for adult respiratory failure: life support in the new era. Intensive Care Med. 2012;38:210–220. doi: 10.1007/s00134-011-2439-2. [DOI] [PubMed] [Google Scholar]
- 19.Brodie D, Bacchetta M. Extracorporeal membrane oxygenation for ARDS in adults. N Engl J Med. 2011;365:1905–1914. doi: 10.1056/NEJMct1103720. [DOI] [PubMed] [Google Scholar]
- 20.Fuehner T, Kuehn C, Hadem J, Wiesner O, Gottlieb J, Tudorache I, et al. Extracorporeal membrane oxygenation in awake patients as bridge to lung transplantation. Am J Respir Crit Care Med. 2012;185:763–768. doi: 10.1164/rccm.201109-1599OC. [DOI] [PubMed] [Google Scholar]
- 21.Rehder KJ, Turner DA, Hartwig MG, Williford WL, Bonadonna D, Walczak RJ, Jr, et al. Active rehabilitation during extracorporeal membrane oxygenation as a bridge to lung transplantation. Respir Care. 2013;58:1291–1298. doi: 10.4187/respcare.02155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Turner DA, Cheifetz IM, Rehder KJ, Williford WL, Bonadonna D, Banuelos SJ, et al. Active rehabilitation and physical therapy during extracorporeal membrane oxygenation while awaiting lung transplantation: a practical approach. Crit Care Med. 2011;39:2593–2598. doi: 10.1097/CCM.0b013e3182282bbe. [DOI] [PubMed] [Google Scholar]
- 23.Hodgson CL, Fan E. A step up for extracorporeal membrane oxygenation: active rehabilitation. Respir Care. 2013;58:1388–1390. doi: 10.4187/respcare.02606. [DOI] [PubMed] [Google Scholar]
- 24.Wang D, Zhou X, Liu X, Sidor B, Lynch J, Zwischenberger JB. Wang-Zwische double lumen cannula-toward a percutaneous and ambulatory paracorporeal artificial lung. ASAIO J. 2008;54:606–611. doi: 10.1097/MAT.0b013e31818c69ab. [DOI] [PubMed] [Google Scholar]
- 25.Foley DS, Pranikoff T, Younger JG, Swaniker F, Hemmila MR, Remenapp RA, et al. A review of 100 patients transported on extracorporeal life support. ASAIO J. 2002;48:612–619. doi: 10.1097/00002480-200211000-00007. [DOI] [PubMed] [Google Scholar]
- 26.Buck ML. Control of Coagulation during extracorporeal membrane oxygenation. J Pediatr Pharmacol Ther. 2005;10:26–35. doi: 10.5863/1551-6776-10.1.26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Schmidt M, Bailey M, Sheldrake J, Hodgson C, Aubron C, Rycus PT, et al. Predicting survival after extracorporeal membrane oxygenation for severe acute respiratory failure. The Respiratory Extracorporeal Membrane Oxygenation Survival Prediction (RESP) score. Am J Respir Crit Care Med. 2014;189:1374–1382. doi: 10.1164/rccm.201311-2023OC. [DOI] [PubMed] [Google Scholar]


