Abstract
Objectives
To explore the experiences of family carers who manage technical health procedures at home and describe their learning process.
Design
A qualitative study using grounded theory.
Participants
New Zealand family carers (21 women, 5 men) who managed technical health procedures such as enteral feeding, peritoneal dialysis, tracheostomy care, a central venous line or urinary catheter. In addition, 15 health professionals involved in teaching carers were interviewed.
Methods
Semistructured interviews were coded soon after completion and preliminary analysis influenced subsequent interviews. Additional data were compared with existing material and as analysis proceeded, initial codes were grouped into higher order concepts until a core concept was described. Interviewing continued until no new ideas emerged and concepts were well defined.
Results
The response of carers to the role of managing technical health procedures in the home is presented in terms of five dispositions: (1) Embracing care, (2) Resisting, (3) Reluctant acceptance, (4) Relinquishing and (5) Being overwhelmed. These dispositions were not static and carers commonly changed between them. Embracing care included cognitive understanding of the purpose and benefits of a procedure; accepting a ‘technical’ solution; practical management; and an emotional response. Accepting embrace is primarily motivated by perceived benefits for the recipient. It may also be driven by a lack of alternatives. Resisting or reluctant acceptance results from a lack of understanding about the procedure or willingness to manage it. Carers need adequate support to avoid becoming overwhelmed, and there are times when it is appropriate to encourage them to relinquish care for the sake of their own needs.
Conclusions
The concept of embracing care encourages health professionals to extend their attention beyond simply the practical aspects of technical procedures to assessing and addressing carers’ emotional and behavioural responses to health technology during the training process.
Keywords: QUALITATIVE RESEARCH: Grounded theory, Carer or caregiver, Family or informal care, Technical health care or Complex care, Technology dependence, New Zealand
Strengths and limitations of this study.
The study sheds new light on the experience of family carers managing technical health procedures—an important but often overlooked care role.
Family carers experience and move between five dispositions towards managing technical health procedures.
A constructivist grounded theory approach views interview data as co-constructed by participants and interviewer.
In retrospective interviews, participants may have forgotten or overlooked events or details. No observation was undertaken to confirm reported practice.
The final sample had a preponderance of parent carers over those caring for an adult family member.
Introduction
Caring for a family member who is ill, disabled or frail is a common life experience. Most people are likely to receive and give care within their family at some time in their life. Moreover, health and social systems are dependent on the informal support given by families to enable many people to live at home.1 Informal care thus plays a vital role both for family units and society as a whole.
Since the 1970s, the nature and importance of family care have been increasingly recognised through research, policy development and carer advocacy groups.2 The work of caring has been recognised as having many potential impacts on carers, including their physical and mental health, relationships, social life, employment opportunities and finances.3–10 While many of these impacts are negative and have been framed as caregiver ‘burdens’, attention has also been paid to the positives of caring, including enrichment in the caring relationship and a sense of satisfaction about the caring role.11–13
This study adds to the caregiving literature by centring on a group of carers whose particular needs have not been well considered to date, namely those whose care moves beyond household tasks or personal care, such as bathing and dressing, to taking responsibility for technical health procedures, such as home-based dialysis, nasogastric (NG) tube feeding or intravenous therapy. Typically these procedures have been undertaken by regulated health professionals and usually within hospital settings. A combination of factors have seen such care move from the hospital to the home since the 1970s, including increasing numbers of people living with chronic conditions, through advances in medical care, improved survival of premature babies and those with congenital conditions, and increasing longevity of the population; development of equipment which can be used at home; reduced institutional care and promotion of home or community care; and rising healthcare costs.14–19
New Zealand has followed these trends towards community care through deinstitutionalisation and greater emphasis on the provision of publicly funded health and disability support in the community.20–24 For adults, some long-term residential care is available; eligibility for these services is determined through a needs assessment process, and the cost of care depends on whether a person qualifies for an income and assets-tested Residential Care Subsidy.25 For children, however, there are limited alternatives to family care and children requiring technical healthcare, who might in the past have been cared for in an institution, are generally looked after by their family at home. Some home-based, publicly funded professional nursing (known as district nursing in New Zealand) may also be available, but this is an episodic liaison or procedure-based service rather than full-time nursing in the home, with the accepted model of home care now relying on day-to-day self-management by the patient or, in the case of children or adults needing support, family care. Caring may have a financial impact, both through direct costs and loss of income if paid employment is affected.26
To date, little attention has been given to what it is like for carers to undertake an advanced technical level of care. Levine et al27 argued that there has been an emphasis on activities of daily living and instrumental activities of daily living (ADLs and IADLs, respectively) to measure caregiving tasks, but limited examination of the qualities of the ‘skilled nursing care’ (p.21) role which has developed alongside the shift of technical healthcare from hospital to home. Assessment of the extent of uptake of such roles has also been limited to just the broadest of data collection. For instance, a 1998 US phone survey of 1000 caregivers found 19% changed dressings, 14% helped with equipment and 39% helped administer medications.28 29 A recent online survey with a nationally representative sample of 1677 American caregivers found that 46% performed one or more of 18 ‘medical/nursing tasks’.30 Of these, 78% managed medications, 35% dealt with wound care, 32% used clinical monitors, 25% gave enemas or managed incontinence equipment, and 14% managed medical equipment such as ventilators, tube feeding and home dialysis.30 In addition, 96% of those who managed medical or nursing tasks also assisted with ADLs and/or IADLs. More than half (57%) of those managing medical or nursing tasks did not feel they had had a choice about taking on these responsibilities.
Given that many of these technical health procedures are restricted activities for health professionals, often requiring postgraduate training if not certification prior to becoming part of the scope of practice for individual healthcare providers, there are many sociological and clinical questions about how such procedures are introduced, implemented, and adopted by non-professional carers in the home environment. The aim of this research, therefore, was to explore the experiences of family carers who manage technical health procedures at home and describe their learning process.
Methodology
In seeking to understand participants’ experiences, it was appropriate to take a qualitative, inductive approach.31 Specifically, grounded theory methodology was chosen as it is suitable for studying social processes in areas where little explanatory theory or knowledge currently exists.32 Charmaz’33 constructivist approach to grounded theory was followed because our view accords with hers that researchers are intrinsically part of a study and do not discover theory but construct it through interaction and interpretation with the participants. Grounded theory utilises well-developed methods of purposeful sampling from relevant populations, concurrent data collection and constant comparative analysis which are continued until data saturation is reached along with the development of theoretical concepts.33 The application of these methods in this study are outlined below.
The study took place in New Zealand and there were two sources of data: first, interviews with carers managing technical health procedures, followed by interviews with health professionals who had a role in training carers. A broad range of carers was sought and interviewed: people managing a variety of technical health procedures (including NG or gastrostomy feeding; diabetes management; enemas or bowel washouts; urinary catheter management; central venous line usage; tracheostomy care; peritoneal dialysis and ileostomy management); people caring for their child (n=20), spouse (3), parent or grandparent (3); both women (21) and men (5) and carers from different ethnic groups (20 New Zealand European; one Māori and six of other ethnicities); people living in main urban centres (18) as well as areas further from secondary or tertiary services (8); and those caring short-term and long-term, both early and later in their experience. All were current carers, except one whose parent had recently died. Three carers had been managing a technical health procedure for less than 1 year; 12 for between 1 and 5 years; and 9 for over 5 years (in two cases, the duration was uncertain). However, other aspects of care, such as feeding or personal care, commonly preceded the introduction of a technical health procedure or continued even if the technical aspect of care ceased. The longest duration of overall caring was 29 years.
Recruitment was facilitated by carer networks and, in one area, by district nurses passing on information about the study to potential participants who could then choose to contact the researchers if interested in taking part. Interviews were arranged with those who agreed to participate, starting with further explanation of the study and an opportunity for questions before obtaining written consent. The study was approved by the Multi-region Committee of the New Zealand Health and Disability Ethics Committees (MEC/11/EXP/076).
Interviews with carers took place from November 2011 to September 2012. There were 22 interviews, four of which involved two carers (three sets of parents and a mother-daughter pair), resulting in a total of 26 interviewees. Care recipients were not included in the interviews. All the interviews were conducted by the first author using a semistructured interview schedule which evolved as the study continued. Interviews were conducted in participants’ homes and lasted from 30 min to 2 h (average just under an hour). With permission, all interviews were audio-recorded except one, for which notes were written. The interviews were subsequently transcribed and in line with grounded theory methodology, coding and memoing began with the first interview. An iterative process continued with data collection, coding and analysing, followed by further data collection and analysis until saturation was reached, as evidenced by the last few interviews fitting existing patterns and not generating new ideas.
Data management and coding were aided by use of NVivo software. Initial codes were developed by detailed attention to the transcripts. As subsequent interviews were coded, new examples within each code were compared with existing material for similarities and differences. Additional codes were added for new concepts that arose; some codes were renamed and overlapping codes were condensed, while others were subdivided for more detail. Relationships between codes were noted and memos were written for each code. From the eighth interview, codes began to be grouped into higher level categories as theoretical ideas developed and further coding became more focused. Initial coding and analyses were undertaken by the first author, with discussion between all the authors contributing to shaping the final theory development and contributing to the rigour of the findings.
Following the interviews with carers, a second set of interviews was conducted with the kinds of health professionals that carers had identified as being important in their learning process. Interviews were undertaken with 12 nurses, two dieticians and an occupational therapist, recruited by approaching service leaders in one District Health Board area to pass on information about the study to relevant staff. Ethical approval was also obtained for this part of the study (MEC/12/EXP/047). Interviews took place between February and September 2013, at or close to the participants’ workplaces. They lasted from 46 min to 1.5 h (average just under an hour).
The interviews with health professionals were again audio-recorded and transcribed, then coded de novo rather than assuming the codes from carers’ interviews would apply again. However, it was quickly apparent that much of the health professionals’ description of their teaching process mirrored what family carers had said, and that some identical codes were appropriate. Analysis proceeded as above, with interviews continuing until saturation was again reached. Thereafter, the separate sets of family carer and health professional data and memos were further analysed jointly and the final grounded theory developed and written up. Finally, all the transcripts were reread as whole accounts to confirm they fitted the theory.
Overall, learning to manage technical health procedures at home was theorised as a process of ‘wayfinding’ for family carers. This has two components: a learning process and a process termed ‘embracing care.’ The learning process consisted of three phases: an initial concentrated period of training with professional support; the novice carer taking responsibility for managing a technical procedure at home; and, with sufficient time and experience, the development of carer expertise. For reasons of space, this learning process will be detailed in another article. The focus of this paper is on the second process of embracing care.
Findings: embracing care
The findings presented in this paper describe how the family carers experienced and responded to taking on the role of managing technical health procedures in the home. Presented below are five themes that reflect five dispositions towards the caring role with respect to the management of these technical health procedures. These are the five dispositions: (1) Embracing care, (2) Resisting, (3) Reluctant acceptance, (4) Relinquishing and (5) Being overwhelmed. These titles are intended to be descriptive rather than imply any judgement value or hierarchy among the dispositions. In addition, carers did not remain fixed in one position, but commonly moved between them. Figure 1 presents the relationships between these dispositions in terms of how the family carers described movements between them over time. The overarching label for these results has been taken from the most central of these dispositions, that of ‘Embracing care’.
Figure 1.
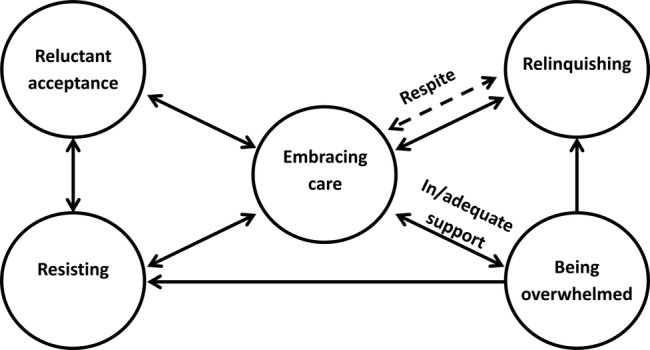
A visual representation of movement between the five dispositions towards caring and management of technical health procedures in the home.
These dispositions were apparent in the initial round of interviews with family carers, and further confirmed and elucidated by the interviews with health professionals. Each of the five dispositions will now be explained, along with movements between them. The findings are illustrated with participants’ quotes, identified as those of a family carer (FC) or health professional (HP). Wording in square brackets [ ] has been added for clarification.
Embracing the care role was about carers’ willingness to take on managing a technical health procedure. Carers might embrace the management of a technical health procedure in whole or in part. There were four components of embracing care: cognitive understanding of the purpose and benefits of a procedure; accepting a ‘technical’ solution; practical management; and an emotional response. Comprehension might be only partial, at least initially. Carers could resist or only reluctantly accept a procedure when they did not understand or acknowledge that its benefits outweighed any perceived disadvantages or they were opposed to ‘unnatural’ treatments (see further below). Carers might choose to learn how to manage some aspects of a procedure but not others (eg, feeding through a NG tube but not replacing it if it came out). Lastly, one's affective response influenced how easy or difficult it was to embrace managing a procedure. In order to be open to embracing a new procedure, carers might also have to let go of existing patterns and expectations which could be associated with a grieving process. This was especially so for parents adjusting to a child with a developmental impairment or who develops a chronic condition.
Embracing care is illustrated by the quote below in which a mother explained how she came to be feeding her child through a NG tube and her expectations about a planned gastrostomy (PEG):
Well basically it was me that said I want the NG…We kind of had her feeding [orally], but it was very, very, hard work and in the end it was just, I was just, ‘No way, I just can't do this.’ It was too hard and she was not gaining weight and that wasn't good for her so we just opted with that [nasogastric feeding]…I'm really excited about getting the PEG [laughs] after all this time because it's not nice having an NG all the time on her face and for her skin and just in general, having to put it down her nose is not very nice for me. And then we can focus on more oral feeding because I think the tube, the tube tends to also, like it affects her swallow and her gag, so I'm looking forward to that next step…I guess when you look at it in the big picture, you're doing it for a good reason. You're doing it so she's going to grow and have the right nutrition, so it is benefiting her. It's not that you're doing something unpleasant for no good reason if you know what I mean. It's not something I enjoy doing, but it's for the better, so I don't really look at it as a negative thing…I just think these [pointing to packets of tubes] have saved my daughter's life. (FC5)
For carers, the primary motivation to embrace managing a technical health procedure was the need and expected benefit for the recipient. The other side of the coin was that the existing situation had become untenable and this could impact on the carer as well as the recipient. Hence accepting a technical procedure could have spin-off advantages for the carer (eg, making feeding quicker and easier); however, at other times, it meant additional work for the carer (such as managing home peritoneal dialysis) and coping with the downsides of the technology (such as responding to a machine alarm in the night or always needing to have equipment when going out). An additional motivation for a family member providing care was that it meant there could be a timely and convenient response to need, rather than having to wait for and fit in with professional assistance.
The health professional participants identified the same motivations for carers embracing care, and added three more which they occasionally saw. The first was a financial imperative. Where the alternative would be residential care, family members might choose to provide care at home to avoid the costs of institutional care not covered by public funding. In this instance, embrace might not be ideal for either the recipient or the carer. Second, some adults with care needs might not want to self-manage and expect another family member to assist them, either from the outset or sometime later. A final motivation, albeit infrequent, was the carer who was perceived to over-embrace their role and, in order to retain this, emphasised the medical needs of the recipient and their own part in providing specialist care. Here, the carer's needs were perceived as having overridden those of the recipient.
By contrast, carers who resisted embracing procedures remained unconvinced of their clinical benefit, did not accept a technical solution, did not believe managing the procedure should be part of their caring role and/or had not (yet) been able to reframe a negative emotional reaction associated with the technology or perhaps with the overall clinical situation:
She had the NG tube in the neonatal unit, and they thought she would have to go home with it, but I was just, I didn't understand what was happening, what had even happened to her, but I was like, ‘No, she's breast-feeding and she's bottle-feeding, why do I need this?’ And she didn't need it in the beginning [but after feeding difficulties and weight loss, began nasogastric tube feeding at six months of age]. But I remember them trying to show me putting it on the litmus and I was just like, I refused to learn it because I didn't want to do anything like that…And I wasn't in the right space to learn it then anyway. (FC10)
Health professional participants also recognised the resistance of carers who were struggling to accept the need for a clinical procedure or who did not want to be the one to manage it. This resistance might be expressed directly, or manifest though passive resistance and a failure to comply with professional directives. At the extreme, it could result in neglecting to provide adequate care.
Being able to resist a caring procedure implies there is an acceptable alternative: the procedure can be safely rejected (at least for a time), or someone else (another family member or a health professional) is available to manage all or some of the procedure at home. However, the necessity for a procedure might become more critical, and a carer might then choose to accept to manage it (willingly or reluctantly); if they remained resistant, this might precipitate their relative moving into alternative care.
Carers were most likely to resist managing aspects of a procedure distressing for the recipient. However, this resistance was sometimes worn down over time by the inconvenience of obtaining outside help or its lack of timeliness, and by familiarity increasing carers’ confidence in their own abilities. A carer's disposition towards a technical procedure could thus shift and the caring role could expand over time.
Health professionals described three responses to carers who were resisting responsibility for a technical procedure. Where this resistance was perceived as legitimate (eg, their work or living situation precluded availability to care), they provided additional professional services if possible or encouraged alternative family care; however, if neither was possible, this could result in a move to residential care. Where they felt a carer could appropriately learn, health professionals attempted to overcome resistance and encourage the carer to embrace the procedure by providing additional information about the need for and benefits of the procedure along with support and reassurance for the carer. In the event of real or potential harm to a patient, they took action to ensure the person's safety.
Another type of disposition towards technical procedures was reluctant acceptance. In this disposition, carers again expressed uncertainty about whether the purported clinical benefits of a procedure outweighed any negatives, or there was a dissonance between their cognitive understanding and their emotional response. However, they reluctantly accepted professional advice because they thought they should, the alternatives appeared even less acceptable, or they felt they had no choice. Alternatively, while accepting the need for a procedure, carers might only reluctantly embrace managing it themselves, doing so because there was no better choice.
Carer: And they also wanted me to add a calorie supplement to the milk, and I was very reluctant to do that because of all the information I'd read about upsetting the baby's gut. But we did it, reluctantly.
Interviewer: What moved the balance for you, that you did do it?
Carer: Because she was still losing weight. And I guess at that stage, the doctors were still in the position that they know best and so we did it, but it took a long time to see any weight gain. (FC22)
Health professionals agreed that lack of alternative care options could compel family members to reluctantly accept a technical procedure, and family expectations might impose the care role on a particular individual. From the health professionals’ perspective, carers could also be reluctant to accept a technical procedure because they were fearful of being left to manage alone, or concerned that becoming involved in one task would inevitably lead to more responsibility. They attempted to counter these concerns with reassurance about their ongoing support.
Relinquishing a technical health procedure, either temporarily or permanently, came about for a number of reasons. First, care might no longer be required: the clinical need for the procedure had resolved (eg, a stoma was reversed), the recipient learned to self-manage (although a carer might continue some supervision) or the recipient died. Second, the carer or recipient might perceive the disadvantages of the procedure as greater than the clinical benefit and choose to cease the treatment. Third, carers might reach a point where they no longer felt able to manage and hence, substitute care arrangements had to be made. This might occur right at the start of a technical health procedure (resistance to managing the procedure becoming the tipping point for the recipient moving to alternative care) or after a period of caring at home. However, while technical healthcare might be relinquished, emotional concern and oversight of the quality of the alternative care continued. Fourth, carers might temporarily relinquish care if their family member was hospitalised or in respite care, or in the case of children, during time at preschool or school. Respite benefited carers by allowing them time for a break and to attend to their own needs, but some found they were expected to continue providing technical care even while their family member was in respite, or chose to because of concerns about safety and quality of alternate care, including a lack of experience with the procedure among health professionals and other staff.
Carer: [Our daughter's] just gone into residential care last month because [my husband] and I are physically buggered … It was basically, we came to a crisis where my back went and I couldn't lift her anymore and we still have this 19 year old ‘baby’. We had become physically, mentally and emotionally exhausted…
Interviewer: And in terms of the service being able to accept her and to set up for her medical needs, how did –
Carer: No, they ring up and say, ‘Take her home, she's sick!’ She sneezes funny and they ring me and say, ‘Take her home.’…They're scared fartless that [she's] going to have a seizure and scare them.
Interviewer: And do they have nursing-qualified staff?
Carer: No nothing, none of them do.
The experience of relinquishing care depends on how carers perceive the reason for relinquishing. Thus, ceasing a procedure because the recipient's improving health renders it unnecessary might bring the carer a sense of freedom and reduced stress, while having a loved one die, or moved into residential care because their needs have increased beyond the carer's capacity to meet them could create more mixed emotions.
Health professionals sometimes encouraged carers to relinquish care for the sake of their own needs. However, they were aware this was difficult when the alternatives were unacceptable to either the carer or recipient, and that there was potential for conflict in relationships. The financial implications sometimes made relinquishment problematic too.
Last, any disposition towards a technical procedure could be replaced by a feeling of being overwhelmed by the demands of the caring role. One participant described this as feeling ‘like a mouse on a running wheel—no matter how fast you run, you're not getting off the running wheel’ (FC20A). When carers were overwhelmed, the care role might overtake other aspects of identity:
Now that she's older, it's definitely just a small part but when she was younger, it seemed all-consuming. It seemed like you weren't the mother, you were the nurse, basically. There was no other time, it seemed, to be doing anything other than toileting. (FC15)
Being overwhelmed by caring could be temporary, particularly during a crisis, or more ongoing where daily care was intensive and there was little support or respite. The environment and social attitudes also contributed to or relieved the sense of being overwhelmed by care. For example, the lack of accessible facilities impeded a family outing, while schools, described by some parents as welcoming and willing to accommodate their children's needs, in other instances imposed obstacles to a child's attendance.
Being overwhelmed could be a catalyst for the carer to seek change and even relinquish care. Though the last straw need not be a technical health procedure, the addition of even an apparently small procedure needed to be considered in the context of the whole family and care situation, as one health professional reflected: ‘I think doing the technical stuff is part of a huge picture and sometimes doing the technical stuff may just be the [point of] tipping [the] balance’ (HP11). Conversely, a technical solution to a problem sometimes relieved carer stress (such as a urinary catheter, making incontinence easier to manage).
Five discrete dispositions towards embracing care have been described, but carers commonly moved between them, for instance, from resistance or reluctant acceptance to embracing a procedure (particularly if post hoc benefits were realised), and from embracing care to being overwhelmed, reluctant acceptance of continuing to care, or relinquishing care. Shifting dispositions was also related to changes in the intensity of caring, and the availability or absence of professional support or respite.
Discussion
To find one's way through managing a technical health procedure involves not only a learning process for carers, but also cognitive and emotional responses to the experience, encapsulated in the phrase ‘embracing care’. In this study, we have described five dispositions towards embracing care, and the movements between them.
Embracing care was primarily motivated by the care recipient's needs and the expectation they would benefit from a technical health procedure. This could be an active choice by the carer, or the naive acceptance of medical advice. Carers might also feel compelled to accept a technical procedure because of social expectations or potential financial consequences. At the extreme of this disposition, some carers may over-embrace their role and seek to retain it even at the expense of what might otherwise be considered to be the recipient's best interests. Twigg and Atkin34 described this last type of caring relationship as ‘symbiotic’ (p.125), being ‘… situations where the carer derives positive benefits from their role, where they have no real wish for it to cease, and where theirs and the cared-for person's needs are mutually reinforcing’ (p.126).
Ethically, embracing care should be a willing choice.35 36 However, health professionals may assume family members will ‘naturally’ take on the role without checking this assumption.37–40 In addition, willingness alone may not lead to the best care situation; health professionals in this study flagged the risks to the recipient of care driven by a financial imperative or over-embrace. Attention therefore needs to be paid to assessing the whole family situation in order to ensure optimal patient care.
By contrast with embracing care, carers who resisted the role of managing technical health procedures had not been persuaded regarding benefits to the recipient. Alternatively, they accepted the need for the procedure but did not want to be the ones to manage some or all of it, particularly aspects which were distressing. Active or passive resistance by a potential carer was problematic for health professionals wanting to teach them; either the carer's resistance had to be overcome or alternative care had to be arranged.
The carer who embraced care largely deflected attention from their own needs to those of the recipient. Resistant carers, on the other hand, draw attention to their own needs. There was some overlap here with Twigg and Atkin's34 ‘balancing/boundary setting mode’ (p.123)—‘The essence of this lies in having an element of separation between the carer and the situation. Carers in this category placed greater value on their own autonomy, and made space for their own interests’ (p.123). Twigg and Atkin34 suggested that this self-interest might take time to develop, could be associated with consciously adopting the title of carer, and not assuming the caring role was simply part of family relationships.
Continuing resistance towards undertaking a technical procedure depended on having the power to resist and the existence of an acceptable alternative. Otherwise, carers might reluctantly accept the caring role. In this disposition, the carer's needs were over-ridden in order to benefit the recipient, yet, continuing in this fashion is likely to be stressful for the carer and less than ideal for the recipient. Reluctant carers may develop sufficient strength to resist the continuing imposition of their role, or they may move to accepting embrace if the benefits experienced by the recipient (or the advantages for their own care-work) overcome their doubts.
Burridge et al41 conducted a systematic review of the concept of reluctance to care, drawing on 17 studies (all but one of which involved care for adults). They defined two dimensions of reluctance: reluctance and resistance/refusal. Many of the indicators of reluctance were similar to those discussed in this study. They included factors such as gender role socialisation, the carer-recipient relationship and other life roles; physical indicators related to the characteristics of the recipient's condition (duration, intensity, predictability) and the carer's own health; psychological indicators under the headings of personal characteristics, perceptions of the role and motivations for it, perceptions of alternatives, and response to the role (including being overwhelmed by it); and finally, social indicators covering expectations of the patient and other family members, expectations of health professionals, where there were problems with preparation for caring, and limited access to resources for support.41 Three important outcomes from reluctance to care were identified in their review: deterioration in the relationship between the carer and recipient, poorer quality of care, and institutionalisation of the recipient.41
Some carers relinquished aspects of the caring role or technical procedure temporarily or permanently if their assistance was no longer required, with some relinquishing the role due to unsustainable demands, physically or psychologically. Relinquishment by a family carer may mean not only a change in care personnel but also in the location of care (eg, a move to residential care for an older person). Being able to relinquish care also depends on the availability and acceptability of alternative care; as noted earlier, carers of adults have greater choice in this regard than those caring for children.
Enabling relinquishment again necessitates viewing carers’ needs as distinct from but equal to those of the recipients. At this point, carers may recognise and advocate, for their own interests, but if they cannot, there may be a place for health professionals encouraging and facilitating their relinquishment.34 42 While relinquishing care focuses on being relieved of the physical work of technical healthcare, other aspects of care, such as monitoring the quality of alternative care, advocacy and providing emotional support to the recipient continue.13 43
Caron and Bowers44 explored how carers decided to continue or relinquish their role in a grounded theory study involving 16 carers of older family members. They found two purposes for caregiving, the first being ‘interrelational’ (protecting and maintaining the recipient's sense of self as well as the relationship between carer and recipient), and the second ‘pragmatic’ provision of good quality care (p.1258). Decisions about getting assistance or relinquishing care were made by considering the purpose of care. When the caregiving had an inter-relational purpose, carers were more concerned with the recipient's needs than their own, and might view any proffered help as unnecessary or interfering with their relationship.44 However, if preserving the relationship became difficult, and the focus shifted to practical care tasks, carers paid more attention to their own needs and were more willing to accept help from service providers.44 This particular pattern of relinquishment may be influenced by their study sample, 10 of whom had cognitive impairments. By contrast, in our study, two mothers who relinquished care of disabled children when they became young adults had done so because of their own health needs and the impact of caring on other family relationships, yet they were also intent on maintaining a close relationship with their child in residential care.
The final disposition towards managing technical health procedures was being overwhelmed by the demands of caring, a state similar to that described as ‘engulfment mode’ by Twigg and Atkin.34 While carers might have some choice about how much they invest themselves in their role and risk being overwhelmed, a very important factor in mitigating this was the degree of external support and alternatives they were offered. The value of professional and community support for carers has been highlighted previously;45–48 conversely, a lack of good quality support and fragmented services is a problem for carers.15
Movement between dispositions towards managing the technical procedure, and the caring role, in general, was influenced by both changing circumstances (particularly the recipient's health and external support) as well as by how carers evaluated the situation. In particular, an initial choice to embrace care might be made hurriedly, with little if any alternative, and limited understanding about what the reality of ongoing care would be like.13 Therefore, it is important to recognise that carers may change their disposition towards technical caregiving procedures. Although context and external support are important, nevertheless, it is the carer's individual experience which needs to be understood.42
A number of important implications for practice can be drawn from the concept of embracing care. First, to embrace technical health procedures, carers need to clearly understand and accept the clinical need for and benefits of the procedure and be assured that they will receive adequate training and ongoing support from the health system. Second, care roles and responsibilities should be openly negotiated, rather than imposed through assumptions, expectations or a lack of alternatives (particularly for parents caring for their children). In encouraging embrace, health professionals may be walking a fine line between meeting the patient's needs and coercing a carer. Further, a carer who embraces a procedure should not be expected to continue to sustain this role indefinitely, or unquestioningly take on more responsibilities in the future. Any additional care tasks should be renegotiated. Carers need to be offered opportunities to affirm their ability to carry on, or be offered alternative support for themselves and their family member in order to avoid becoming overwhelmed. At times, it may be appropriate to encourage carers to prioritise their own needs and relinquish some of the care role. Finally, the concept of embracing care draws attention to the fact that carers’ management of a procedure for a family member is not only a matter of acquiring technical skills, but also one bound up with relationships and emotions. Health professionals need to be aware of and support a carer's emotional adjustment as well as their acquisition of practical expertise.
This study sheds new light on family carers’ experiences of managing technical health procedures—an important but often overlooked care role. Grounded theory methodology has enabled us to attend closely to individual stories and, through comparing and contrasting them, develop a theoretical explanation of their experiences which clinicians can apply when working with other family carers. Our sampling of diverse carers (including those caring for children, a partner or parent, and carers managing a wide range of technical health procedures) strengthens the applicability of the theory to other carers managing technical health procedures.
In relying on retrospective interviews and with no observation to confirm reported practice, participants may have forgotten or overlooked events or details; however, the findings accord with other literature. They could be strengthened by prospectively following carers beginning to manage a technical health procedure and interviewing them at several times to better understand transitions between dispositions towards the caring role. The scope of the theory could also be extended by testing its application to other groups of people who learn to manage technical health procedures, such as school staff, respite carers, and residential care assistants who are not nurses. It could also be tested with carers in non-technical roles to see if it is more generally applicable.
Conclusion
As increasingly complex care continues to move from hospital to home, it is important to consider how family carers learn to manage technical health procedures and their experience of this role. The concept of embracing care highlights five dispositions that carers can take towards technical procedures in the home and will help health practitioners to attend to the needs of carers, in turn benefiting those they care for.
Acknowledgments
The authors thank all the participants and the individuals and organisations (including Mary Potter Hospice) who assisted with recruitment for the study.
Footnotes
Contributors: JMD conceived and designed the study, with supervision from WL and SK. JMD collected the study data through interviews. All authors contributed to analysing and interpreting the data. JMD drafted the initial version of this article and all authors revised it and approved the final version for submission.
Funding: JMD was supported by a Health Research Council of New Zealand Disability Research Placement Programme Career Development Award (grant number 11/129) to undertake this research.
Competing interests: None declared.
Ethics approval: Multi-region Committee of the New Zealand Health and Disability Ethics Committees.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: No additional data are available.
References
- 1.Larkin M. What about the carers? In: Lloyd CE, Heller T, eds. Long-term conditions: challenges in health and social care. London: Sage Publications, 2012:186–98. [Google Scholar]
- 2.Heaton J. The gaze and visibility of the carer: a Foucauldian analysis of the discourse of informal care. Sociol Health Ill 1999;21:759–77. 10.1111/1467-9566.00182 [DOI] [Google Scholar]
- 3.Covinsky KE, Eng C, Lui LY et al. Reduced employment in caregivers of frail elders: impact of ethnicity, patient clinical characteristics, and caregiver characteristics. J Gerontol A Biol Sci Med Sci 2001;56:M707–13. 10.1093/gerona/56.11.M707 [DOI] [PubMed] [Google Scholar]
- 4.Hirst M. Carer distress: a prospective, population-based study. Soc Sci Med 2005;61:697–708. 10.1016/j.socscimed.2005.01.001 [DOI] [PubMed] [Google Scholar]
- 5.Magliano L, Fiorillo A, De Rosa C et al. Family burden in long-term diseases: a comparative study in schizophrenia vs. physical disorders. Soc Sci Med 2005;61:313–22. 10.1016/j.socscimed.2004.11.064 [DOI] [PubMed] [Google Scholar]
- 6.Nepal B, Brown L, Ranmuthugala G et al. Women carers in financial stress report. University of Canberra: National Centre for Social and Economic Modelling, 2009. [Google Scholar]
- 7.Vitaliano PP, Young HM, Zhang J. Is caregiving a risk factor for illness? Curr Dir Psychol Sci 2004;13:13–16. 10.1111/j.0963-7214.2004.01301004.x [DOI] [Google Scholar]
- 8.Vitaliano PP, Zhang J, Scanlan JM. Is caregiving hazardous to one's physical health? A meta-analysis. Psychol Bull 2003;129:946–72. 10.1037/0033-2909.129.6.946 [DOI] [PubMed] [Google Scholar]
- 9.Legg L, Weir CJ, Langhorne P et al. Is informal caregiving independently associated with poor health? A population-based study. J Epidemiol Comm Health 2013;67:95–7. 10.1136/jech-2012-201652 [DOI] [PubMed] [Google Scholar]
- 10.Trivedi R, Beaver K, Bouldin ED et al. Characteristics and well-being of informal caregivers: Results from a nationally-representative US survey. Chronic Ill 2014;10:167–79. 10.1177/1742395313506947 [DOI] [PubMed] [Google Scholar]
- 11.Cohen CA, Colantonio A, Vernich L. Positive aspects of caregiving: rounding out the caregiver experience. Int J Geriatr Psychiatry 2002;17:184–8. 10.1002/gps.561 [DOI] [PubMed] [Google Scholar]
- 12.Mackenzie A, Greenwood N. Positive experiences of caregiving in stroke: a systematic review. Disabil Rehabil 2012;34:1413–22. 10.3109/09638288.2011.650307 [DOI] [PubMed] [Google Scholar]
- 13.Nolan M, Grant G, Keady J. Understanding family care: a multidimensional model of caring and coping. Buckingham: Open University Press, 1996. [Google Scholar]
- 14.Bakewell Sachs S, Porth S. Discharge planning and home care of the technology dependent infant. J Obstet Gynecol Neonatal Nurs 1995;24:77–83. 10.1111/j.1552-6909.1995.tb02382.x [DOI] [PubMed] [Google Scholar]
- 15.Kirk S. Families’ experiences of caring at home for a technology-dependent child: a review of the literature. Child Care Health Dev 1998;24:101–14. 10.1046/j.1365-2214.1998.00043.x [DOI] [PubMed] [Google Scholar]
- 16.Marks L. Home and hospital care: redrawing the boundaries. Research report 9. London: King's Fund Institute, 1991. [Google Scholar]
- 17.Teare J. Defining children with complex needs. In: Teare J, ed. Caring for children with complex needs in the community. Oxford: Blackwell Publishing, 2008:1–20. [Google Scholar]
- 18.Williams AP, Spalding K, Deber RB et al. Prescriptions for pediatric home care: analyzing the impact of the shift from hospital to home and community on children and families. Toronto: Sick Kids Foundation, 2005. [Google Scholar]
- 19.Wong DL. Transition from hospital to home for children with complex medical care. J Pediatr Oncol Nurs 1999;8:3–9. 10.1177/104345429100800102 [DOI] [PubMed] [Google Scholar]
- 20.King A. The New Zealand health strategy. Wellington: Ministry of Health, 2000. [Google Scholar]
- 21.Minister for Disability Issues. The New Zealand disability strategy: making a world of difference Whakanui Oranga. Wellington: Ministry of Health, 2001. [Google Scholar]
- 22.Ministry of Health. Child health strategy. Wellington: Ministry of Health, 1998. [Google Scholar]
- 23.Ministry of Health. Health of older people strategy. Wellington: Ministry of Health, 2002. [Google Scholar]
- 24.Tennant M. Disability in New Zealand: an historical survey. NZ J Disabil Stud 1996;2:3–33. [Google Scholar]
- 25.Ministry of Health. Long-term residential care. Retrieved 23 January 2015 from http://www.health.govt.nz/our-work/life-stages/health-older-people/long-term-residential-care
- 26.Goodhead A, McDonald J. Informal caregivers literature review: a report prepared for the National Health Committee. Wellington: National Health Committee, 2007. [Google Scholar]
- 27.Levine C, Reinhard SC, Feinberg LF et al. Family caregivers on the job: moving beyond ADLs and IADLs. Generations 2003;27:17–23. [Google Scholar]
- 28.Donelan K, Hill CA, Hoffman C et al. Challenged to care: informal caregivers in a changing health system. Health Aff 2002;21:222–31. 10.1377/hlthaff.21.4.222 [DOI] [PubMed] [Google Scholar]
- 29.Gould DA. Family caregivers and the health care system: findings from a national survey. In: Levine C, Murray TH, eds. The cultures of caregiving: conflict and common ground among families, health professionals, and policy makers. Baltimore: The Johns Hopkins University Press, 2004:15–34. [Google Scholar]
- 30.Reinhard SC, Levine C, Samis S. Home alone: family caregivers providing complex chronic care. Washington DC: AARP Public Policy Institute and United Hospital Fund, 2012. [Google Scholar]
- 31.Pope C, Mays N. Reaching the parts other methods cannot reach: an introduction to qualitative methods in health and social services research. BMJ 1995;311:42–5. 10.1136/bmj.311.6996.42 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Birks M, Mills J. Grounded theory: a practical guide. Thousand Oaks, CA: Sage, 2011. [Google Scholar]
- 33.Charmaz K. Constructing grounded theory: a practical guide through qualitative analysis. London: Sage, 2006. [Google Scholar]
- 34.Twigg J, Atkin K. Carers perceived: policy and practice in informal care. Buckingham: Open University Press, 1994. [Google Scholar]
- 35.Arras JD, Dubler NN. Bringing the hospital home: ethical and social implications of high-tech care. Hastings Cent Rep 1994;24:S19–28. 10.2307/3563510 [DOI] [PubMed] [Google Scholar]
- 36.Palm E. Who cares? Moral obligations in formal and informal care provision in the light of ICT-based home care. Health Care Anal 2013;21:171–88. 10.1007/s10728-011-0199-3 [DOI] [PubMed] [Google Scholar]
- 37.Dow B, McDonald J. The invisible contract: shifting care from the hospital to the home. Aust Health Rev 2007;31:193–202. 10.1071/AH070193 [DOI] [PubMed] [Google Scholar]
- 38.Flynn AP, Carter B, Bray L et al. Parents’ experiences and views of caring for a child with a tracheostomy: a literature review. Int J Pediatr Otorhinolaryngol 2013;77:1630–4. 10.1016/j.ijporl.2013.07.020 [DOI] [PubMed] [Google Scholar]
- 39.Kirk S. Negotiating lay and professional roles in the care of children with complex health care needs. J Adv Nurs 2001;34:593–602. 10.1046/j.1365-2648.2001.01788.x [DOI] [PubMed] [Google Scholar]
- 40.Reeves E, Timmons S, Dampier S. Parents’ experiences of negotiating care for their technology-dependent child. J Child Health Care 2006;10:228–39. 10.1177/1367493506066483 [DOI] [PubMed] [Google Scholar]
- 41.Burridge L, Winch S, Clavarino A. Reluctance to care: a systematic review and development of a conceptual framework. Cancer Nurs 2007;30:E9–19. 10.1097/01.NCC.0000265298.17394.e0 [DOI] [PubMed] [Google Scholar]
- 42.Brown J, Nolan M, Davies S. Who's the expert? Redefining lay and professional relationships. In: Nolan M, Davies S, Grant G, eds. Working with older people and their families. Buckingham: Open University Press, 2001:19–32. [Google Scholar]
- 43.Milligan C. Caring for older people in New Zealand: informal carers’ experiences of the transition of care from the home to residential care. Lancaster University: Institute for Health Research, 2004. [Google Scholar]
- 44.Caron CD, Bowers BJ. Deciding whether to continue, share, or relinquish caregiving: caregiver views. Qual Health Res 2003;13:1252–71. 10.1177/1049732303257236 [DOI] [PubMed] [Google Scholar]
- 45.Given BA, Given CW, Kozachik S. Family support in advanced cancer. CA Cancer J Clin 2001;51:213–31. 10.3322/canjclin.51.4.213 [DOI] [PubMed] [Google Scholar]
- 46.Henry P. Negotiating an unstable ladder. N Z Nurs J 2008;14:17–20. 10.1016/j.jnn.2007.11.002 [DOI] [PubMed] [Google Scholar]
- 47.Kirk S, Glendinning C. Supporting ‘expert’ parents: professional support and families caring for a child with complex health care needs in the community. Int J Nurs Stud 2002;39:625–35. 10.1016/S0020-7489(01)00069-4 [DOI] [PubMed] [Google Scholar]
- 48.Sloper P. Models of service support for parents of disabled children. What do we know? What do we need to know? Child Care Health Dev 1999;25:85–99. 10.1046/j.1365-2214.1999.25220120.x [DOI] [PubMed] [Google Scholar]


