Abstract
Tuberculosis caused by Mycobacterium tuberculosis presents a major health challenge in endemic countries and spares no organ in the human body. This infection is a mimicker of various disease processes such as metastasis, lymphoproliferative diseases, and other granulomatous conditions such as sarcoidosis and fungal infections. The most challenging and important differential is metastasis, especially in the disseminated form of tuberculosis. We present a histopathologically proven case of isolated hepatosplenic tuberculosis that was provisionally diagnosed as lymphoma due to its unusual, restricted involvement of the liver and spleen.
Background
Tuberculosis (TB) is caused by Mycobacterium tuberculosis and still remains a major public health problem in India and other developing countries. Recently, there has been a resurgence of TB due to factors such as multidrug resistance, HIV co-infection and intravenous drug abuse.1 Even though the most common presentation is pulmonary TB, extra pulmonary disease accounts for around 15% of all TB.2 Isolated hepatic and splenic TB in the absence of disseminated disease is exceedingly rare and poorly described in the literature.3 The diagnosis is difficult and delayed due to non-specific clinical and imaging features.
Case presentation
A 47-year-old woman with diabetes and hypertension was admitted to our hospital with abdominal pain, early satiety and loss of weight of 2 months duration. There was no history of fever or night sweats. There was neither prior history of treatment for TB nor contact with a patient of TB. Physical examination was unremarkable except for tenderness in the right hypochondrium. There was no jaundice or lymphadenopathy seen.
Investigations
Laboratory examination revealed haemoglobin 11.2 g/dL; haematocrit 38.3%; total white cell count 10 600/mm3; serum urea 11 mg/dL and serum creatinine 0.6 mg/dL. Liver function tests showed total bilirubin of 0.9 mg/dL with a direct component of 0.3 mg/dL; aspartate amino transferase 30 IU/L and alanine transaminase, 13 IU/L. On serology, the patient was non-reactive for HIV types 1 and 2, hepatitis B surface antigen (HBsAg) and antibodies to hepatitis C virus. Fasting and post prandial blood sugar levels were raised, at 193 and 291 mg/dL, respectively. Ultrasonography of the abdomen revealed multiple ill-defined hypoechoic lesions diffusely scattered in the liver and in the spleen. Contrast-enhanced CT revealed multiple small heterogeneously enhancing hypodense lesions in the liver and in the spleen (figure 1). The largest lesion measured 1.6×1.2 cm. Chest radiography was normal. An ultrasound-guided core needle biopsy was performed and submitted for pathological examination. Histopathology revealed mild steatosis and numerous granulomas composed of epithelioid histiocytes, Langhans giant cells and lymphocytes, along with areas of caseous necrosis (figure 2A, B). Ziehl-Neelsen staining revealed acid fast bacilli. A histopathological diagnosis of hepatic TB was made.
Figure 1.
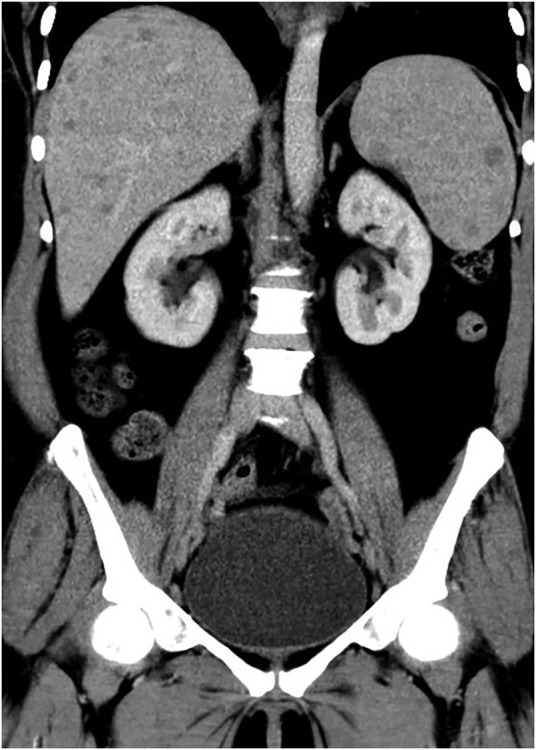
Coronal image from the contrast-enhanced CT of the abdomen of the patient demonstrating multiple, relatively well-defined, hypoenhancing lesions of varying sizes involving the liver and spleen.
Figure 2.
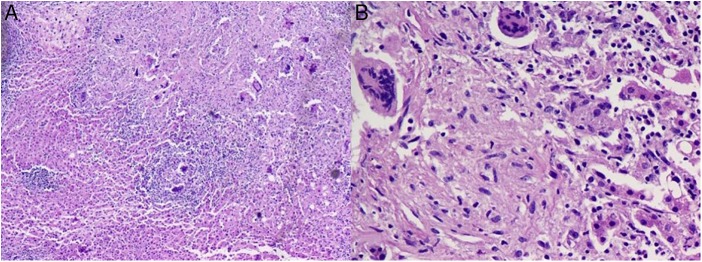
(A) Microscopy showing numerous caseating granulomas along with areas of normal hepatic parenchyma (H&E ×20). (B) High-power view of a granuloma composed of epithelioid histiocytes, Langhans giant cells, caseous necrosis and lymphocytes (H&E ×200).
Differential diagnosis
Clinicoradiological differentials included lymphoma, metastasis and granulomatous conditions such as TB, sarcoidosis and fungal infection.
Treatment
The patient was started on four-drug antitubercular therapy (isoniazid, rifampin, ethambutol and pyrazinamide).
Outcome and follow-up
On 1-month follow-up the patient showed good clinical improvement.
Discussion
The involvement of the liver and the spleen in tuberculous is very rare, and is usually associated with a disseminated or miliary form of the disease and in immunocompromised states such as HIV co-infection.3 4 Isolated hepatic TB is postulated to arise via a minute tubercular focus in the intestine that gains access to the liver via the portal vein.4 Reed et al5 have classified hepatic TB into three morphological types: (1) TB of the liver associated with generalised miliary TB, which is the most common form, noted in 50–80% of patients dying from pulmonary TB, (2) primary miliary TB of the liver and (3) primary tuberculoma or abscess of the liver. Splenic TB similar to hepatic TB can occur either as a part of disseminated disease or in isolated form. Pathomorphologically, splenic TB is of the following five types: miliary TB, nodular TB, tuberculous splenic abscess, calcific TB and mixed type.2 6
The diagnosis of hepatic and splenic TB is challenging, as the clinical presentations are non-specific and range from being asymptomatic to manifesting fever, weakness, weight loss, abdominal pain, hepatosplenomegaly and, rarely, portal hypertension.1 7 8 To add to this dilemma, most patients do not have a history of prior exposure to TB. It is imperative to diagnose this condition early, as mortality rates for untreated abdominal TB is as high as 50%.1
The imaging features of hepatic and splenic TB are non-specific, and have overlapping features with conditions such as metastasis, lymphoproliferative diseases and other granulomatous conditions, including sarcoidosis and fungal infections. The described ultrasound features include well-defined to ill-defined hypoechoic lesions with or without specks of calcification.9 CT features include non-enhancing to heterogeneously enhancing hypodense lesions, with central necrosis in cases of tubercular abscesses. Unusual features include irregular biliary ductal dilation and wall enhancement with stippled wall calcifications. Based on CT findings, hepatic TB has been categorised into three major types, namely: (1) parenchymal, (2) serohepatic and (3) tubercular cholangitis. The parenchymal type is the most common form, comprising of miliary, nodular and mixed variants. Miliary TB presents with multiple discrete non enhancing hypodense lesions, less than 2 cm in size. The nodular form represents lesions more than 2 cm in size, with central non-enhancing necrosis and thick internal septations. The mixed form shows features common to miliary as well as nodular forms. Serohepatic TB refers to peripherally placed miliary TB showing mild peripheral enhancement and causing thickening of the liver capsule. Tubercular cholangitis presents with focal or diffuse irregularly dilated intrahepatic ducts or diffuse calcification along the course of the biliary ducts.10
Needle biopsy or laparotomy may be required for obtaining material for diagnosis, especially if the lesions are small. Histopathological and/or microbiological evidence is a must for establishing a diagnosis of hepatosplenic TB. Histopathology demonstrates characteristic granulomas composed of central caseous necrosis surrounded by epithelioid cells, Langhans giant cells and lymphocytes.3
On the basis of clinicoradiological findings, the initial impression in our patient was suggestive of lymphoma. However, histopathology confirmed the diagnosis of TB. Antitubercular therapy is the primary modality of treatment. Surgery may, rarely, be required in difficult cases.1 6 The present case is unusual in that no other focus of TB was detected in the lung, gastrointestinal tract or lymph nodes, and the disease involvement was restricted to the liver and spleen.
In conclusion, due to its atypical clinicoradiological features, hepatosplenic TB cannot be easily differentiated from its sinister mimics—such as metastasis and lymphoproliferative disorders—and the confirmatory diagnosis can only be made on histopathology. TB should always be considered in the differential diagnosis of multiple hypodense lesions in the liver and in the spleen, especially in endemic areas and in immunocompromised patients.
Learning points.
Isolated hepatic and splenic tuberculosis in the absence of disseminated disease is exceedingly rare.
Apart from lymphoma, metastasis and other granulomatous conditions, such as sarcoidosis and fungal infections, tuberculosis should also be included in the differentials for multiple hypodense lesions in the liver and in the spleen.
Imaging features of isolated hepatic and splenic tuberculosis are non-specific and a high index of suspicion is needed for their early detection and management, as the mortality rate is as high as 50% for untreated abdominal tuberculosis.
Histopathology remains the gold standard for diagnosis of tuberculosis, especially in its atypical presentations, for example, isolated hepatosplenic tuberculosis.
Footnotes
Contributors: RH diagnosed the condition and all the authors contributed equally to the design, the literature search and final editing of the manuscript.
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Wu Z, Wang WL, Zhu Y et al. Diagnosis and treatment of hepatic tuberculosis: report of five cases and review of literature. Int J Clin Exp Med 2013;6:845–50. [PMC free article] [PubMed] [Google Scholar]
- 2.Imani Fooladi AA, Hosseini MJ, Azizi T. Splenic tuberculosis: a case report. Int J Infect Dis 2009;13:e273–5. 10.1016/j.ijid.2008.11.002 [DOI] [PubMed] [Google Scholar]
- 3.Kumar V, Pandey D. Isolated hepatosplenic tuberculosis. Hepatobiliary Pancreat Dis Int 2008;7:328–30. [PubMed] [Google Scholar]
- 4.Singh D, Singh S, Raut SB et al. Isolated liver tuberculosis: a case report. Ped Surgery Int 2004;20:727–8. 10.1007/s00383-002-0878-0 [DOI] [PubMed] [Google Scholar]
- 5.Reed DH, Nash AF, Valabhji P. Radiological diagnosis and management of a solitary tuberculous hepatic abscess. Br J Radiol 1990;63:902–4. 10.1259/0007-1285-63-755-902 [DOI] [PubMed] [Google Scholar]
- 6.Ho PL, Chim CS, Yuen KY. Isolated splenic tuberculosis presenting with pyrexia of unknown origin. Scand J Infect Dis 2000;32:700–1. 10.1080/003655400459685 [DOI] [PubMed] [Google Scholar]
- 7.Mojtahedzadeh M, Otoukesh S, Shahsafi MR et al. Portal hypertension secondary to isolated liver tuberculosis. Am J Trop Med Hyg 2012;87:162–4. 10.4269/ajtmh.2012.11-0643 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Basa JV, Singh L, Jaoude WA et al. A case of isolated splenic tuberculosis. Int J Surg Case Rep 2014;8:117–19. 10.1016/j.ijscr.2014.10.050 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Brauner M, Buffard MD, Jeantils V et al. Sonography and computed tomography of macroscopic tuberculosis of the liver. J Clin Ultrasound 1989;17:563–8. 10.1002/jcu.1870170804 [DOI] [PubMed] [Google Scholar]
- 10.Yu RS, Zhang SZ, Wu JJ et al. Imaging diagnosis of 12 patients with hepatic tuberculosis. World J Gastroenterol 2004;10:1639–42. [DOI] [PMC free article] [PubMed] [Google Scholar]


