Abstract
Chrysosplenol C (4′,5,6-trihydroxy-3,3′,7-trimethoxyflavone) isolated from Miliusa balansae has unique structural features as a reversible inotropic agent independent of β-adrenergic signaling and with selective activation of cardiac myosin ATPase. Hence, a series of chrysosplenol analogues were synthesized and explored for identification of pharmacophore that is essential for the increasing contractility in rat ventricular myocytes. Analogue 7-chloro-2-(3-hydroxyphenyl)-3-methoxy-4H-chromen-4-one showed highly potent contractility (54.8% at 10 μM) through activating cardiac myosin ATPase (38.7% at 10 μM). Our systematic structure–activity relationship study revealed that flavonoid nucleus of chrososplenol C appears to be an essential basic skeleton and hydrophobic substituent at position 7 of chromenone such as methoxy or chloro enhances the activity. Additionally, our ATPase study suggested that these chrysosplenol analogues have selectivity toward cardiac myosin activation. Thus, the novel flavonone with 3-/7-hydrophobic substituent and 3′-hydrogen bonding donor function is a novel scaffold for discovery of a new positive inotropic agent.
Keywords: Chrysosplenol C, positive inotrope, myosin activation, contractility
Heart failure (HF) is an enormous health problem worldwide.1 Decreased systolic function is a central factor in the pathogenesis of heart failure.2−4 Systolic dysfunction is better characterized as a decrease in cardiac contractility that can be measured by a reduction in the left ventricular ejection fraction (LVEF).5−9 The contractility function of the cardiac sarcomere mainly depends on the six thin filaments of actin arranged hexagonally around a central thick filament of myosin.10 Actin, which acts as a binding site for myosin heads, is surrounded by a coil of tropomyosin which prevents binding with myosin heads. The three subunits of troponin (troponin I, troponin C, and troponin T)11 and tropomyosin complex regulates actin–myosin binding interaction.12 At the initiation of contraction, intracellular calcium increases. Binding of calcium on the troponin C weakens the troponin I–actin interaction and causes tropomyosin to move to expose the hydrophobic residues on the actin filament. The myosin heads are then able to bind to actin, initiating contraction. The myosin heads latch on to the actin and then rotate at the neck, resulting in fiber shortening. The myosin sliding movement is fueled by chemical energy released from adenosine triphosphate (ATP) during the chemical degradation of ATP to adenosine diphosphate and inorganic phosphate (ADP-Pi) and subsequent release of Pi by myosin ATPase. The power-stroke, velocity, and duration of filament shortening are regulated through the cycle of a weakly actin–myosin bound state to a strongly actin–myosin bound state.
Inotropic agents increase myocardial contractility through different pathways that in most cases lead to a final increment of intracellular cyclic adenylate monophosphate (cAMP) levels, which in turn induces calcium release from the sarcoplasmic reticulum, hence enhancing the contractile force generation by the contractile apparatus.13
There are three classes of inotropic agents that are in use at present: β-agonists, phosphodiesterase inhibitors, and calcium sensitizers. Classical inotropes, such as β-agonists and phosphodiesterase inhibitors, acutely improve the hemodynamic and clinical status of acute decompensated heart failure patients, but frequently promote and accelerate some pathophysiologic mechanisms causing further myocardial injury and leading to increased short- and long-term mortality. However, calcium-sensitizing inotropic agents such as levosimendan14 have been developed to increase the calcium sensitivity of myofibrils without increasing calcium transients for treating systolic heart failure. Unfortunately, in the later stages, it was found that levosimendan also has significant phosphodiesterase inhibition activity.15 This mixed mechanism may be the reason for levosimendan failure in improvement on mortality. A recent breakthrough came from identifying omecamtiv mecarbil (Figure 1)16,17 as a selective cardiac myosin adenosine triphosphatase (ATPase) activator, which is currently completing late phase II trials on the verge of phase III trials for treatment of systolic heart failure, demonstrating the enormous potential of myosin-targeting drugs.
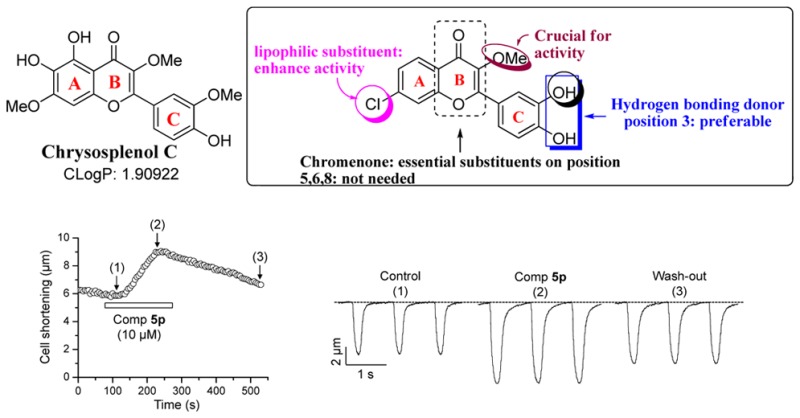
Figure 1.
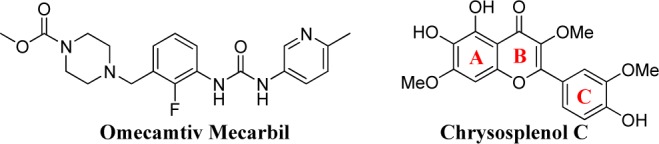
Known myosin activators.
Thus, on the basis of ATPase activation concept, we screened18 compounds from the natural sources. Our efforts brought to light chrysosplenol C19 (4′,5,6-trihydroxy-3,3′,7-trimethoxyflavone, Figure 1), a known flavonoid isolated from Miliusa balansae and Pterocaulon sphacelatum, which induced positive inotropic effect in rat ventricular myocytes by reversibly increasing ventricular cell shortening with an EC50 value of about 45 ± 7.8 μM independent of β-adrenergic signaling20 and showed the activation (28.1% at 10 μM) of cardiac myosin ATPase as presented in Table 1. Thus, the positive inotropic effect of Chrysosplenol C was considered to be originated from the activation of cardiac myosin ATPase. Chrysosplenol C possesses flavonoid scaffold, which is the unique structural feature of an inotropic agent. Therefore, to explore the pharmacophore responsible for its contractile activity, we systematically studied the structure–activity relationship of chrysosplenol C using cell contractility test of myocytes. Later, the activation of the cardiac myosin ATPase of its potent analogues was demonstrated.
Table 1. Summary of the Changes in Ventricular Cell Contractility and Cardiac Myosin ATPase Activity by Chrysosplenol C Analoguesa.
| ventricular
cell contractility (% of change) |
|||||||
|---|---|---|---|---|---|---|---|
| compd | R1 | R2 | R3 | R4 | 10 μM | 50 μM | cardiac myosin ATPase % activation at 10 μM |
| 5a | 5-OH | OMe | OMe | OH | 4.20 ± 2.10 (3) | 12.3 ± 4.02 (3) | 0 |
| 5b | 6-OH | OMe | OMe | OH | 3.90 ± 2.30 (3) | 9.30 ± 1.89 (3) | |
| 5c(23) | 7-OMe | OMe | OMe | OH | 60.7 ± 3.10c (3) | 45.3 ± 2.09c (3) | 33.7 ± 2.64 |
| 5d | 7-Cl | OMe | OMe | OH | 43.9 ± 6.83 (3)c | 41.8 ± 5.25 (3)b | 36.4 ± 1.32 |
| 5e | H | OMe | OMe | OH | 30.5 ± 5.10 (3)c | 44.9 ± 4.27 (3)c | |
| 5f | 5-OH | OH | OMe | OH | 0.00 ± 0.00 (3) | 0 (1) | |
| 5g | 6-OH | OH | OMe | OH | 0.00 ± 0.00 (3) | 0 (1) | |
| 5h(23) | 7-OMe | OH | OMe | OH | 8.17 ± 3.17 (3) | 3.98 ± 2.28 (3) | 0 |
| 5i | 7-Cl | OH | OMe | OH | 23.5 ± 2.40c (3) | 57.3 ± 9.65 (3)b | |
| 5j | H | OH | OMe | OH | 10.5 ± 3.10 (3) | 10.3 ± 2.08 (3) | |
| 5k | 7-Cl | H | OMe | OH | 0.00 ± 0.00 (3) | 0 (1) | |
| 5l(24) | 7-OMe | OMe | H | OH | 42.1 ± 2.54 (3)c | 38.6 ± 5.49 (3)c | 30.9 ± 1.01 |
| 5m(24) | 7-Cl | OMe | H | OH | 49.6 ± 4.67 (3)c | 62.1 ± 4.75 (3)b | 28.9 ± 2.29 |
| 5n | 7-OMe | OMe | H | Cl | 0.00 ± 0.00 (3) | 0 (1) | |
| 5o(24) | 7-Cl | OMe | H | Cl | 0 (1) | 0 (1) | |
| 5p | 7-Cl | OMe | OH | H | 54.8 ± 2.76c (3) | 53.9 ± 2.79 (3)c | 38.7 ± 1.09 |
| 5q(25) | 7-OMe | OH | H | OH | 8.87 ± 3.87 (3) | 23.10 ± 3.17 (3)b | |
| 5r(26) | 7-Cl | OH | H | OH | 0.00 ± 0.00 (3) | 11.0 ± 2.51 (3) | |
| 5s | 7-Cl | OMe | OMe | H | 16.6 ± 4.30 (3)b | 23.6 ± 3.29 (3)b | |
| 5t | 7-Cl | OH | OMe | H | 0.00 ± 0.00(3) | 0.00 ± 0.00(3) | |
| 6 | chalcone | 0 (1) | 0.00 ± 0.00 (3) | ||||
| 7(27) | methylated chrysosplenol C | 8.70 ± 3.00 (3) | 21.6 ± 3.90 (3)c | ||||
| chrysosplenol C | 5-OH,6-OH,7-OMe | OMe | OMe | OH | 16.6 ± 3.05 (3)b | 53.0 ± 4.07 (3)c | 28.1 ± 1.20 |
| omecamtiv mecarbil | 400 nM | 1 μM | 80.4 ± 2.89 | ||||
| 59.3 ± 2.60d (6) | 33.8 ± 4.10 (5)b | ||||||
Values represent mean ± SEM.
*P < 0.05.
**P < 0.01.
***P < 0.001 vs control (one sample t test). The number in the parentheses indicates number of cells tested. ATPase activation measurements were done twice.
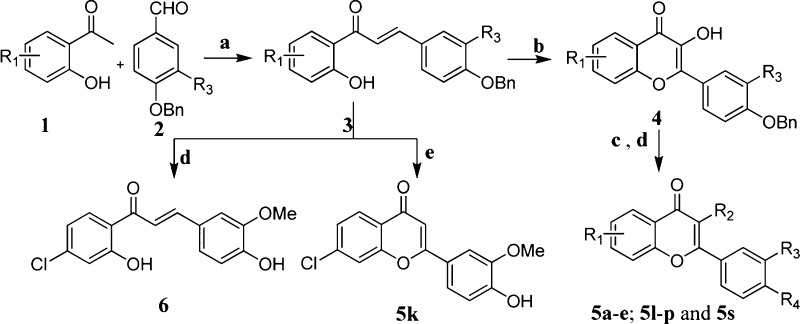
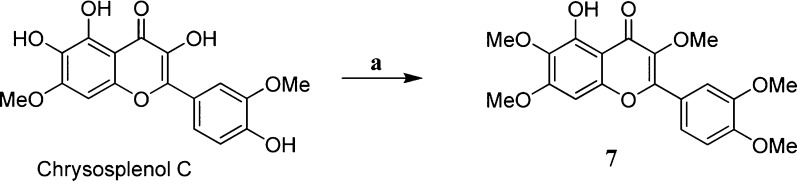
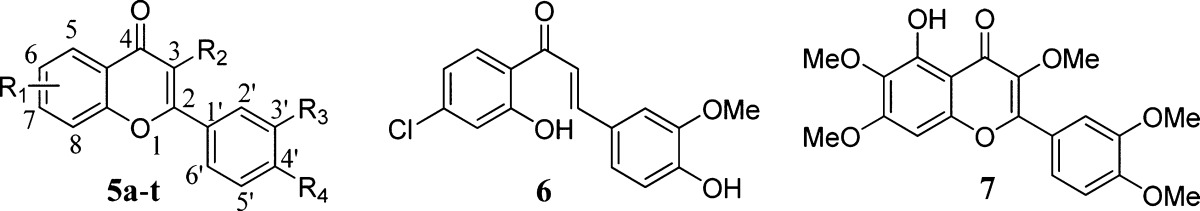
Designed chrysosplenol C analogues 5 and 6 (Table 1) were synthesized as outlined in Scheme 1. The key intermediate chalcones 3(21) were prepared in excellent yields by aldol condensation of substituted hydroxyacetophenones 1 with corresponding substituted benzaldehydes 2 in the presence of KOH in aqueous ethanol under reflux conditions. Chalcone intermediates 3 were cyclized using Algar–Flynn–Oyamada reaction22 in the presence of hydrogen peroxide in aq. NaOH in a mixture of ethanol and dioxane solution at 5–10 °C, which afforded chromenones 4. Then, methylation of chromenones 4 using methyl iodide and NaH in DMF followed by deprotection of benzyl group using thioanisole as a catalyst in trifluoroacetic acid furnished desired compounds 5a–e, 5l–p, and 5s. Analogues 5f–j, 5q, 5r, and 5t were prepared by deprotection of benzyl group of the corresponding 4 as shown in Scheme 2. Compound 5k was obtained by the treatment of chalcone 3 with iodine in DMSO at 100 °C. Chalcone 6 was obtained by debenzylation of the corresponding 3.
Scheme 1. Synthesis of Chrysosplenol C Analogues 5.
Reagents and conditions: (a) KOH,90% EtOH, reflux; (b) H2O2,10% NaOH, dioxane/ethanol (1:1) 5 °C–rt; (c) CH3I, NaH, DMF; (d) TFA/thioanisole at rt; (e) I2, DMSO, 1 h/100 °C.
Scheme 2. Synthesis of Compounds 5f–j; 5q,r,t.
Reagents and conditions: (a) TFA/thioanisole at rt.
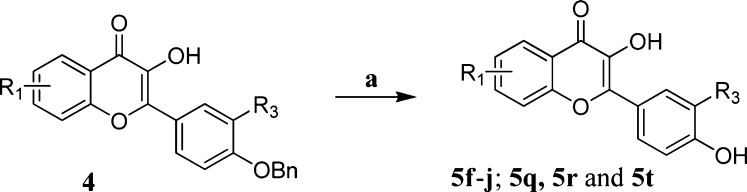
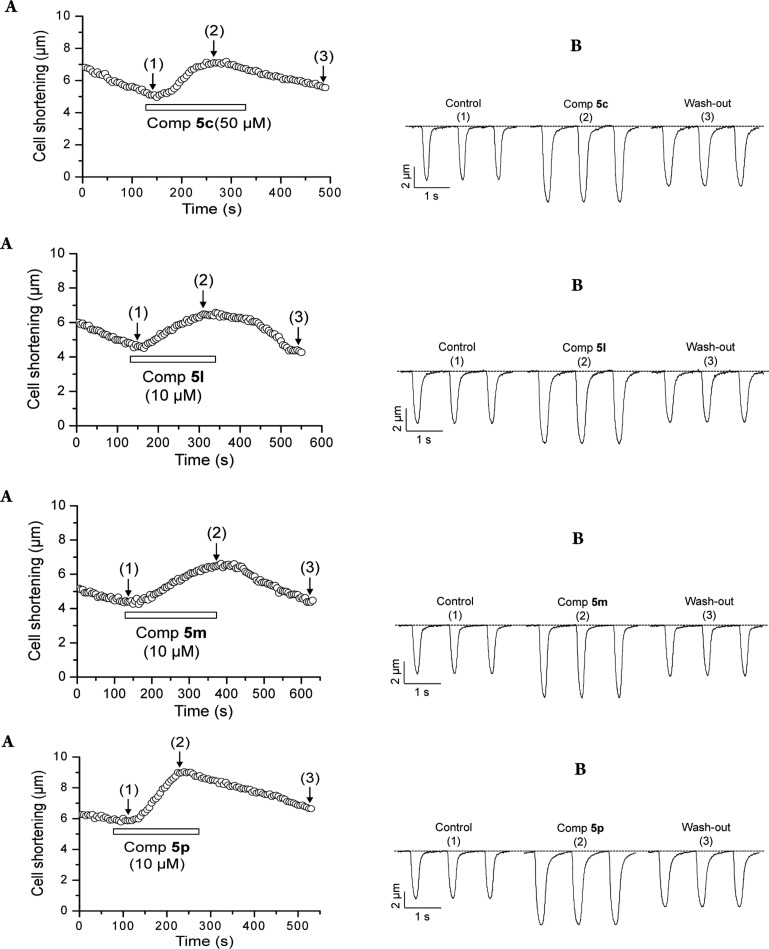
Compound 7 was prepared as shown in Scheme 3 by methylating chrysosplenol C using methyl iodide in the presence of NaH in DMF solvent. The structures of the compounds were confirmed by physical and spectral analysis (see synthesis and characterization of compounds in the Supporting Information). All the synthesized compounds were measured for cell shortening activity,18 and the results are listed in Table 1. The time courses of induced positive inotropic effect and the effect of the kinetics of contraction and relaxation for potent compounds 5c, 5l, 5m, and 5p are illustrated in Figure 2.
Scheme 3. Synthesis of Compound 7.
Reagents and conditions: (a) CH3I, NaH, DMF at 5–10 °C.
Figure 2.
Time course of chrysosplenol C analogue-induced positive inotropic effect and the effect of kinetics of contraction and relaxation. (A) Time course of change in the peak values of cell shortenings in the presence of corresponding compounds. (B) Traces recorded at the time periods indicated by (1), (2), and (3) in panel A.
In order to identify a potential pharmacophore of chrysosplenol C, our attempt was begun by investigating the effect of substituents on A ring (Figure 1) of chrysosplenol C. Accordingly, 5-hydroxy (5a, % change in contractility 4.23 ± 2.13, ClogP = 2.782), 6-hydroxy (5b, % change in contractility 3.91 ± 2.27, ClogP = 1.882), and 7-methoxy (5c, % change in contractility 60.7 ± 3.10, ClogP = 2.298) analogues were prepared and studied for their rat ventricular cell contractility activity (assay briefed in the Supporting Information). Among these derivatives, 7-methoxy analogue 5c (solubilty in DMSO/tyrode solution, 17.06 μg/mL) showed the strong contractility activity and improved aqueous solubility profile compared with chrysosplenol C (solubilty in DMSO/tyrode solution, 14.08 μg/mL, and unlike 5c chrysosplenol C was partially precipitated on long-standing in in vitro DMSO/tyrode stock solution), while 5a and 5b remarkably diminished the activity. The above results implicated that hydroxy functional groups on positions 5 and 6 of chromenone ring of chrysosplenol C are not essential.
To further understand the role of electronic effect of substituent on A ring, methoxy group of 5c was replaced with mild electron withdrawing chloro group as shown in 5d (% change in contractility 43.9 ± 6.83, ClogP = 3.043), and the activity was retained. However, omission of all the substituents on A ring as shown in 5e decreased (% change in contractility 30.5 ± 5.10, ClogP = 2.294) the activity. These results indicate that lipophilic substituents on position 7 of chromenone ring enhanced the activity.
Next our attention was turned to explore the role of methoxy group on B ring. This prompted the synthesis and evaluation of analogues 5f–j. Compounds 5f, 5g, 5h (% change in contractility 8.2 ± 3.2), and 5j (% change in contractility 10.5 ± 3.1) with 3-hydroxy group on the B ring did not show any activity or showed negligible activity. However, 3-hydroxy analogue 5i with 7-chloro group exhibited moderate potency (% change in contractility 23.5 ± 2.40; ClogP = 3.033). Elimination of 3-methoxy group as shown in the compound 5k on the B ring did not show any inotropic activity. These results indicate that 3-methoxy group is preferred.
Compounds 5c and 5d were considered as lead compounds for further optimization on the C ring of chrysosplenol C. Removal of the methoxy group on the C ring of lead compounds 5c and 5d provided compounds 5l (% change in contractility 42.1 ± 2.54, ClogP = 2.455) and 5m (% change in contractility 49.6 ± 4.67, ClogP = 3.216), respectively. Both compounds 5l and 5m showed nearly 3-fold greater potency (Table 1) than chrysosplenol C and comparable activity to 5c and 5d. These results implied that the methoxy substituent is not necessary for the activity.
Replacement of the hydroxy group on the C ring of 5c and 5d with chloro gave inactive compounds 5n and 5o, respectively. These results implicate that the hydrogen bonding donor at C ring should be very important for the activity.
Encouraged by these findings, we pursued further to find the effect of the substituents on ring C. Hence we prepared compound 5p by changing the position of the hydroxy of C ring in 5m from position 4′ to 3′. This compound showed more potent activity (% change in contractility 54.8 ± 2.75, ClogP = 3.216) than 5m. This result indicates that hydrogen bonding donor at position 3′ of C ring may be ideal for the activity. Even though compounds have a hydroxy group at position 4′ of the C ring, the existence of hydroxyl group on B ring resulted in very weak activity as shown in compounds 5q and 5r. Once again, these confirm that methoxy group on B ring is very crucial. Replacement of hydroxyl function on position 3′ of C ring in 5p with methoxy as shown in 5s (% change in contractility 16.60 ± 4.27) markedly reduced the activity. This result indicates that the hydrogen bonding donating property of the hydroxy group on C ring is important. Replacement of the methoxy group of 5s with hydroxy on position 3 of chromenone ring as shown in 5t completely demolished the activity. This again proves that 3-methoxy function of chromenone ring of these analogues is important for the activity.
Methylation of all hydroxy groups in chrysosplenol C gave compound 7 (% change in contractility 8.73 ± 3.00), which showed less activity. This might be due to masking of hydrogen bonding donor capability of hydroxyl group at C ring of chrysosplenol C.
The next set of experiments studied the importance of chromenone backbone by mimicking it into chalcone 6, which resulted in complete loss of activity. This might indicate that planar chromenone with α,β-unsaturated ketone combination is very important for the activity.
To find the mechanism of action of cardiac contractility of chrysosplenol C and its analogues, active compounds 5c, 5d, 5l, 5m, and 5p were assessed by sarcomere ATPase assay,28 and the results are listed in Table 1. All of these analogues showed significant myosin activation activity compared to chrysosplenol C. The compound 5c exhibiting the best contractile activity showed moderate ATPase activation activity and better than chrysosplenol C. The chloro substituted compound 5d exhibited most potent activity in ATPase activation as well as highly potent contractility. Even though 5l and 5m with only 4-hydroxy substituent on C ring showed the highest level of cardiac contractility activity, their ATPase activities were moderate. Interestingly, the compound 5p showed the best performance in contractility activity as well as ATPase activation. Although the ATPase activation of chrysosplenol C analogues are not entirely parallel to their activity in cell contractilities, cardiac myosin ATPase activation of these analogues might be the potential mode of action of their positive inotropic effect. Thus, chrysosplenol C analogues are quite unique scaffolds for finding a novel inotropic agent.
The compounds that showed good cell contractility and myosin activity were analyzed for selectivity in myosins at 10 μM concentration18 (Results are presented in the Supporting Information). The experiment was done in duplicate and repeated twice, none of the tested compounds showed significant activity for myosin ATPase using skeletal and smooth myosin S1. Thus, from these results it can be assumed that these compounds are selective for Cardiac myosin S1. However, more detailed in vivo studies are required for the same.
γ
For defining the pharmacophore of chrysosplenol C, a number of analogues of chrysosplenol C have been investigated for their ventricular contractility and activation of cardiac myosin ATPase activity. Among them analogue 7-chloro-2-(3-hydroxyphenyl)-3-methoxy-4H-chromen-4-one (5p) showed highly potent contractility with activation of cardiac myosin ATPase. The structure–activity relationship of chrysosplenol C could be summarized as illustrated in Figure 3. Flavonoid scaffold of chrososplenol C appears to be a basic skeleton, and hydroxy groups of A ring in chrososplenol C are not necessary for the activity. Introduction of hydrophobic substituent at position 7 of chromenone such as methoxy or chloro enhances the activity. The methoxy group at position 3 appears to be crucial for the activity; however, hydroxyl group abolishes or decreases the activity. The hydrogen bonding donor capability at position 3′ or 4′ of C ring is important for the activity; however, position 3′ is more effective than position 4′. Thus, the flavonone with 3-/7-hydrophobic substituent and 3′-hydrogen bonding donor function is a novel scaffold for discovery of a new positive inotropic agent.
Figure 3.
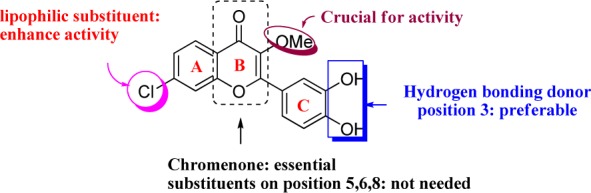
Identified pharmacophore of chrysosplenol C.
Supporting Information Available
Experimental details and spectroscopic data for the compounds described in this Letter. The Supporting Information is available free of charge on the ACS Publications website at DOI: 10.1021/acsmedchemlett.5b00043.
Author Contributions
All authors have given approval to the final version of the manuscript.
This work was supported by Priority Research Centers Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Education, Science and Technology (2009-0093815).
The authors declare no competing financial interest.
Supplementary Material
References
- Man J. P.; Jugdutt B. I. Systolic heart failure in the elderly: optimizing medical management. Heart Fail. Rev. 2012, 17, 563–571. [DOI] [PubMed] [Google Scholar]
- Gottdiener J. S.; McClelland R. L.; Marshall R.; Shemanski L.; Furberg C. D.; Kitzman D. W.; Cushman M.; Polak J.; Gardin J. M.; Gersh B. J.; Aurigemma G. P.; Manolio T. A. Outcome of congestive heart failure in elderly persons: influence of left ventricular systolic function. The cardiovascular health study. Ann. Int. Med. 2002, 137, 631–639. [DOI] [PubMed] [Google Scholar]
- Berry C.; Hogg K.; Norrie J.; Stevenson K.; Brett M.; McMurray J. Heart failure with preserved left ventricular systolic function: a hospital cohort study. Heart 2005, 91, 907–913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teerlink J. R. A novel approach to improve cardiac performance: cardiac myosin activators. Heart. Fail. Rev. 2009, 14, 289–298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lenzen M. J.; Scholte op Reimer W. J. M.; Boersma E.; Vantrimpont P. J. M. J.; Fallath F.; Swedberg K.; Cleland J.; Komajda M. Differences between patients with a preserved and a depressed left ventricular function: a report from the EuroHeart failure survey. Eur. Heart J. 2004, 25, 1214–1220. [DOI] [PubMed] [Google Scholar]
- Hobbs F. D. R; Kenkre J. E.; Roalfe A. K.; Davis R. C.; Hare R.; Davies M. K. Impact of heart failure and left ventricular systolic dysfunction on quality of life. Eur. Heart J. 2002, 23, 1867–1876. [DOI] [PubMed] [Google Scholar]
- Malki Q.; Sharma N. D.; Afzal A.; Ananthsubramaniam K.; Abbas A.; Jacobson G.; Jafri S. Clinical presentation, hospital length of stay, and readmission rate in patients with heart failure with preserved and decreased left ventricular systolic function. Clin. Cardiol. 2002, 25, 149–152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Philbin E. F.; McCullough P. A.; Dec G. W.; DiSalvo T. G. Length of stay and procedure utilization are the major determinants of hospital charges for heart failure. Clin. Cardiol. 2001, 24, 56–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen-Solal A.; Desnos M.; Delahaye F.; Emeriau J. P.; Hanania G. A national survey of heart failure in French hospitals. Eur. Heart J. 2000, 21, 763–769. [DOI] [PubMed] [Google Scholar]
- Bragadeesh T. K. M.; Mathur G.; Clark A. L.; Cleland J. G. F. Novel cardiac myosin activators for acute heart failure. Expert Opin. Invest. Drugs 2007, 16, 1541–1548. [DOI] [PubMed] [Google Scholar]
- Greaser M. L.; Gergely J. Purification and properties of the components from troponin. J. Biol. Chem. 1973, 248, 2125–2133. [PubMed] [Google Scholar]
- Tobacman L. S. Thin filament-mediated regulation of cardiac contraction. Annu. Rev. Physiol. 1996, 58, 447–481. [DOI] [PubMed] [Google Scholar]
- Felker G. M.; O’Connor C. M. Inotropic therapy for heart failure: an evidence-based approach. Am. Heart J. 2001, 142, 393–401. [DOI] [PubMed] [Google Scholar]
- Moiseyev V. S.; Poder P.; Andrejevs N.; Ruda M. Y.; Golikov A. P.; Lazebnik L. B.; Kobalava Z. D.; Lehtonen L. A.; Laine T.; Nieminen M. S.; Lie K. I. Safety and efficacy of a novel calcium sensitizer, levosimendan, in patients with left ventricular failure due to an acute myocardial infarction. A randomized, placebo-controlled, double-blind study (RUSSLAN). Eur. Heart J. 2002, 23, 1422–1432. [DOI] [PubMed] [Google Scholar]
- Orstavik O.; Ata S. H.; Riise J.; Dahl C. P.; Andersen G. Ø.; Levy F. O.; Skomedal T.; Osnes J. B.; Qviqstad E. Inhibition of phosphodiesterase-3 by levosimendan is sufficient to account for its inotropic effect in failing human heart. Br. J. Pharmacol. 2014, 171, 5169–5181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morgan B. P.; Muci A.; Lu P.-P.; Qian X.; Tochimoto T.; Smith W. W.; Garard M.; Kraynack E.; Collibee S.; Suehiro I.; Tomasi A.; Valdez S. C.; Wang W.; Jiang H.; Hartman J.; Rodriguez H. M.; Kawas R.; Sylvester S.; Elias K. A.; Godinez G.; Lee K.; Anderson R.; Sueoka S.; Xu D.; Wang Z.; Djordjevic N.; Malik F. I.; Morgans D. J. Jr. Discovery of omecamtiv mecarbil the first, selective, small molecule activator of cardiac myosin. ACS Med. Chem. Lett. 2010, 1, 472–477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Malik F. I.; Hartman J. J.; Elias K. A.; Morgan B. P.; Rodriguez H.; Brejc K.; Anderson R. L.; Sueoka S. H.; Lee K. H.; Finer J. T.; Sakowicz R.; Baliga R.; Cox D. R.; Garard M.; Godinez G.; Kawas R.; Kraynack E.; Lenzi D.; Lu P. P.; Muci A.; Niu C.; Qian X.; Pierce D. W.; Pokrovskii M.; Suehiro I.; Sylvester S.; Tochimoto T.; Valdez C.; Wang W.; Katori T.; Kass D. A.; Shen Y.-T.; Vatner S. F.; Morgans D. J. Cardiac Myosin Activation: A potential therapeutic approach for systolic heart failure. Science 2011, 331, 1439–1443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Please see the Supporting Information for the contraction assay procedure.
- Huong D. T.; Kamperdick C.; Sung T. V. Homogentisic acid derivatives from Miliusa balansae. J. Nat. Prod. 2004, 67, 445–447. [DOI] [PubMed] [Google Scholar]
- Son M. J.; Kim H. K.; Thu Huong D. T.; Kim Y. H.; Sung T. V.; Cuong N. M.; Woo S. H. Chrysosplenol C increases contraction in rat ventricular myocytes. J. Cardiovasc. Pharmacol. 2011, 57, 259–262. [DOI] [PubMed] [Google Scholar]
- Pouget C.; Fagnere C.; Basly J.-P.; Besson A.-E.; Champavier Y.; Habrioux G.; Chulia A.-J. Synthesis and aromatase inhibitory activity of flavanones. Pharm. Res. 2002, 19, 286–291. [DOI] [PubMed] [Google Scholar]
- Bennett M.; Burke A. J.; O’Sullivan W. I. Aspects of the Algar-Flynn-Oyamada (AFO) reaction. Tetrahedron 1996, 52, 7163–7178. [Google Scholar]
- Yamaguchi S. Sulfuric acid esters III-IV. III. Sulfuric Acid esters of flavonoids. (part 2). Synthesis of sulfuric acid esters of polyhydroxyflavonols. Nippon Kagaku Zasshi 1960, 81, 1332–1336. [Google Scholar]
- Meyer N. D.; Haemers A.; Mishra L.; Pandey H. K.; Pieters L. A. C.; Vanden Berghe D. A.; Vlietinck A. J. 4′-Hydroxy-3-methoxyflavones with potent antipicornavirus activity. J. Med. Chem. 1991, 34, 736–746. [DOI] [PubMed] [Google Scholar]
- Simpson T. H.; Garden L. Chelate systems. Part I. J. Chem. Soc. 1952, 4638–4644. [Google Scholar]
- Kidd D. Potential bronchodilators in the flavanoid series. J. Chem. Soc. 1962, 5121–5125. [Google Scholar]
- Wei G.-J.; Sheen J.-F.; Lu W.-C.; Hwang L. S.; Ho C.-T.; Lin C.-I. Identification of sinensetin metabolites in rat urine by an isotope-labeling method and ultra high performance liquid chromatography-electrospray ionization mass spectrometry. J. Agric. Food Chem. 2013, 61, 5016–5021. [DOI] [PubMed] [Google Scholar]
- Pollard T. D. Myosin purification and characterization. Methods Cell Biol. 1982, 24, 333–371. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.