Abstract
AIM:
Single-port laparoscopic surgery (SILS) has become increasingly popular during the last decades. This prospective study was undertaken to evaluate the feasibility of single-port laparoscopic splenectomy compared with conventional multiport laparoscopic splenectomy.
MATERIALS AND METHODS:
Between February 2, 2009 and August 29, 2011, a total of 40 patients with the diagnosis of immune thrombocytopenic purpura were included to study. Patients were alienated into two groups according to the procedure type including SILS and conventional multiport splenectomy.
RESULTS:
There were 19 patients in group 1, and 21 in group 2. Operative time was significantly shorter in group 1 versus group 2 (112.4 ± 13.56 vs 71.2 ±18.1 minutes, respectively, P < 0.05). One patient in group 1 had converted to laparatomy due to preoperative bleeding. Postoperative pain analyses (VAS Score) revealed superiority of SILS in the early post-operative days (P < 0.05).
CONCLUSIONS:
SILS splenectomy is a safe and effective alternative to standard laparoscopic splenectomy.
Keywords: Immune thrombocytopenic purpura, single incision laparoscopic surgery, single port, single port access-laparoscopic splenectomy, splenectomy
INTRODUCTION
After the first description of the splenectomy technique in 1910 for hereditary spherocytosis,[1] laparoscopic splenectomy (LS), which was first described by Delaitre and Maignien[2] in 1991 has become the gold standard method in normal size spleens. The most common indication worldwide is immune thrombocytopenic purpura (ITP), and efficacy of the technique is well-known.[3,4,5] During the last two decades many centres around the world performed countless minimally invasive multi-port splenectomies, and experienced teams reported three port techniques as standard approaches. As a consequence of the search to further minimalize the technique, our clinic was first to perform and describe the technique of splenectomy via single incision in the literature.[6] Having gained experience with the technique, this study was undertaken to compare single port access (SPA)-LS with the conventional multi-port LS in terms of duration of the procedure, peri-operative morbidity, pain scores and hospital stay.
MATERIALS AND METHODS
Between February 2, 2009 and August 29, 2011 a total of 40 patients with ITP had undergone minimally invasive splenectomy at our clinic. The patients were divided into two groups according to the procedure type. Group l had SPA-LS and group 2 included three port LS. All the patients had signed informed consent form. The patients were informed about the technique, and the procedure type was selected by patients’ choice. The patient data including age, gender, diagnosis, pre-operative complete blood counts, and operative data including operative time from the first skin incision to the application of wound dresses, estimated blood loss, presence of accessory spleens, morcellated spleen weights, size of spleen, indications for conversion, type of hilar division (either intracorporeal ligation or clipping), vessel sealing system and vascular endoscopic staplers, drainage volume, and duration of hospital stay were collected prospectively. The size of the spleen was measured with computerized tomography (CT) scans and also by a flexible measuring scale, which was introduced via port to the operative field intra-operatively.
Post-operative data were collected from patient charts, computer reviews of surgical clinic database and follow-up charts of haematology clinic. All patients were contacted by phone and engaged in a questionnaire when sufficient data were not found in the survey of the clinics.
All patients were vaccinated with Pneumovax 23 (Merck & Co., Inc., Whitehouse Station, NJ, USA) 2 weeks prior to the operation and received antibiotic prophylaxis (1 g intravenous ampicillin-sulbactam) before operation. All patients underwent an intravenous contrast enhanced total abdominal multislice CT scan for pre-operative splenic measurements and search for susceptible accessory spleens. During their hospital stay, pain complaints of all the patients were scored based on the visual analogue scale (VAS) defined by Wewers and Lowe.[7]
All the patients were enquired for pain analysis starting from the early post-operative time. The 6th and 24th h enquiries revealed superiority of SPA group (P < 0.05 for post-operative 6 and 24 h). Patients were under same post-operative pain medication in both groups.
The patients were operated under general anaesthesia. All the patients were performed by the same senior surgeon (UB). All the patients received the same non-steroid anti-inflammatory agents (8 mg intravenous lornoxicam, twice a day). A suction drain was routinely placed to the operative field in all of the cases and drain amylase was studied on post-operative day 2. Drains were extracted only if the drain amylase was normal, and the amount was <50cc; otherwise kept until the drainage was over.
The Surgical Technique
Laparoscopic splenectomy procedure
The patients were placed in the right lateral decubitus position in a standard fashion as described by different groups,[8,9] tilted at a 15° reverse trendelenburg position and bended at the umbilicus increasing the distance between the iliac crest and costal margin. Three trocars were introduced; two 5 mm trocars, one at the tip of 11th rib laterally and one near the midline medially. A 15 mm trocar was inserted 5 cm below the costal margin. A careful exploration of the abdomen was carried out for detection of accessory spleens. The spleen was mobilized from inferior to superior direction in a standard fashion. The first step of the dissection was the liberation of the inferior pole of the spleen with the dissection of the splenocolic ligament. The next step was the division of short gastric vessels and exploration of the lesser sac in order to expose the splenic hilum. The spleen was fully mobilized except leaving the phrenosplenic ligament partially intact, which was used for a natural countertraction during the preparation of the hilum for division. The splenic hilum was divided by using white cartridge laparoscopic linear vascular stapler (Endo GIA, AutoSuture, Norwalk, CT) in the majority of cases. In two of the patients splenic vein and artery were dissected separately and divided with Ligasure (Valleylab division of Tyco Healthcare, Mansfield, MA) bipolar vessel sealing system. After hilar division a specimen retrieval bag was introduced, placed under the spleen and then the phrenosplenic attachments were divided, letting the spleen fall into the bag. The bag was taken out of the abdominal wall partially from the 15 mm trocar place, and the spleen was morcellated before removal. An aspirative drain was placed in the operative field, and the defect of the 15 mm trocar is closed with fascia closer.
Single port access-laparoscopic splenectomy procedure
The patient position was exactly same as three port laparoscopy technique. We standardly made an umbilical incision and enter the abdominal cavity as in the open technique. Single Incision Laparoscopic Surgery (SILS™) port of Covidien, Mansfield, MA was used in all patients. SILS™ port was introduced with a sponge holder in to the abdomen. The pneumoperitoneum was then obtained via SILS™ port. A 5 mm telescope with 30° angle was introduced, and two articulated hand instruments were used to explore the whole abdominal cavity for accessory spleens. We were used to work with a single articulated instrument for all single port surgeries. The articulated 5 mm grasper was held in the left hand, and 5 mm Ligasure was used by the right hand of the surgeon. The diaphragmatic attachments have significant importance for counter-traction by hanging the spleen upwards with the help of gravity. We obey the inferior to superior dissection rule and start with mobilization of the splenic flexure. After liberation of the lower pole of the spleen, gastro-splenic ligament was divided by Ligasure in order to enter the retro-gastric pouch. The hilum was exposed, and the roticulating grasper was switched with a roticulated dissector, and then the splenic hilum was prepared. After that the table was tilted left, and retrosplenic ligaments were liberated by using Ligasure device.
The first four patients of the SPA-LS group were operated by the technique which was defined by us[6] via three 5 mm ports were introduced through the same umbilical incision from different fascial defects, whereas the latter fifteen patients were operated by using the special SILS™ port (Covidien, Mansfield, MA) introduced from a single 2 cm fascial opening. The patient position was the same with standard laparoscopic technique. In the first four patients a complete umbilical skin incision of 2 cm was made, and pneumoperitoneum was maintained with Veress needle in a closed fashion. After a 12 mmHg CO 2 pneumoperitoneum was obtained, three 5 mm trocars were inserted separately through the umbilical incision. In the latter fifteen patients, a fascial opening was obtained through umbilical incision and the special SILS™ port was introduced with a sponge holder in to the abdomen. The pneumoperitoneum was obtained via SILS™ port. The rest of the procedures were the same in both techniques and all steps in standard LS was followed with roticulated instruments and 5 mm Ligasure (Valleylab division of Tyco Healthcare, Mansfield, MA) probe. A 5 mm telescope with 30° angle was used. An exploration was carried out for exploring the other pathologies and accessory spleens. Following placement of instruments into the abdomen, the basic mechanism was similar to three-port laparoscopic procedures. Ligasure was used during most of the dissection. For stapling of splenic hilum, one of the ports was replaced with a 15 mm port and the operation was resumed. Liberated viscera were put into a special sterile retrieval bag. Spleen in the retrieval bag was morcellated before removal through umbilical incision. An aspirative drain was placed in the operative field routinely after splenectomy. The fascial defect was sutured with non-absorbable suture material.
RESULTS
A total of forty patients underwent minimally invasive splenectomy of whom 19 were in group l and 21 in group 2. There was 1 conversion to open in group l (5%) and none in group 2. One patient from group 1 was also re-laparotomised few hours after the operation in order to control post-operative haemorrhage. There was no mortality in either group.
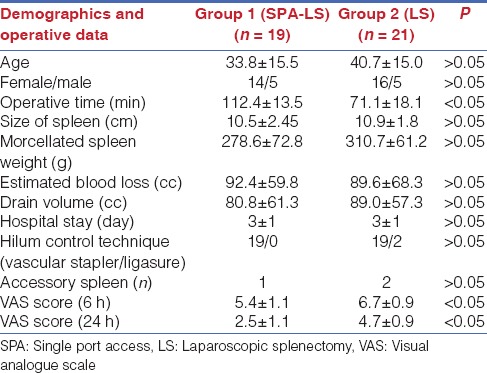
The male/female ratio was similar between study groups with 5/16 in group 2 versus 5/14 in group 1. The mean age of the group 2 was 40.7 ± 15.0 (22–69) years versus 33.8 ± 15.5 in group 1. The weight of morcellated spleen was 310 ± 61 g (range between 220 and 450) in group 2 and 278 ± 72 g (range between 185 and 415), P < 0.05. The mean length of the spleen was similar with 11 ± 2 (range between 8 and 14) in group 2 versus 11 ± 2 (range between 8 and 14) in group 1. Operative time was significantly shorter in group 2 (71 ± 18 [range between 40 and 100]) min compared to the group 1 (112 ± 13 [range between 92 and 145]). Estimated blood loss was similar in both groups (90 ± 68, range 0–400cc vs. 92 ± 60, range 0–300cc, respectively). The amount of drainage was 90 ± 50 cc in group 2 compared to 80 ± 60 cc in group 1. The mean length of hospital stay was same in both groups with 3 days. There were a low-profile pancreatic fistula in one patient in each group. One patient converted to open in group 1, and moreover, there were also one patient who needed laparatomy during the early post-operative period due to bleeding in group 1. The prominent technique for hilum control was the use of vascular stapler in 90% of the cases (n = 19) in group 2. There were 2 accessory spleens in group 2 compared to 1 in group 1. Post-operative pain analyses (VAS score) revealed superiority of SPA-LS in early post-operative days (P < 0.05 for post-operative 6 and 24 h) with. The comparison between study groups were given in detail on Table 1.
Table 1.
Patient demographics and operative data between study groups
DISCUSSION
Surgery in all disciplines dealing in different anatomical regions with all aspects has been in great demand to further minimize its trauma to the patients. With the introduction of video-endoscopy in the last two decades surgeons had the opportunity to perform minimal invasive surgical operations in thorax, abdominal cavity and even in the joints in a wide range of different surgical disciplines without major incisions.
General surgery had the leading role in evaluating techniques and describing the principles of video-endoscopic procedures. Today almost all of the general surgical practices can be done via laparoscopic approaches. As a result of both the technological developments and magnificent patient demands, surgeons are urged to further minimize their techniques. Today's issue in general surgery is to reach the efficient and cheaper way to obtain “scarless” surgery.
Natural orifices are used to reach the abdominal cavity in different procedures in different ways. Cholecystectomies,[10] appendectomies,[11] and nephrectomies[12] have been done via transluminal approaches, but in the majority, due to the flexible body of the video-endoscopes, surgeons needed at least one trans-abdominal port for traction. Pure natural orifice transluminal endoscopic surgery is not feasible yet for any of the procedures and needs further innovation of systems and instruments.
However, procedures can be done via single incision either with single or with multi-channel ports, and the incision could be hidden in the umbilical fold resulting a scarless surgery. The technique had been described and named in many different ways such as laparo-endoscopic single site surgery, SPA, SILS, Single Incision Multi-Port Laparo-Endoscopic Surgery, Natural Orifice Trans Umbilical Surgery and embryologic Natural Orifice Transluminal Endoscopic Surgery. In all of these techniques, trans-umbilical incision is made, and either different ports from different fascial defects or a single port with multiple working channels from a single fascial defect is introduced to perform standard procedures laparoscopically.
Splenectomy via single incision had been reported by different authors in the previous years.[6,13,14,15,16,17,18,19,20,21,22] Most of them were case reports. There is only one small series including eight patients undergoing single port splenectomy for various indications.[13] To the best of our knowledge, this is the first trial to compare SILS with multi-port LS in the literature.
In this study, we only analysed patients with ITP and did not include the hematologic malignancies in order to standardize the patient population. The operative time was significantly longer in SPA group (112 ± 14 min vs. 71 ± 18 min, respectively, P < 0.05). However, post-operative pain analyses (VAS score) revealed superiority of SPA-LS in early post-operative period (P < 0.05 for post-operative 6 and 24 h).
In our opinion, the longer operative time in SPA group was due to the obstacles of single port procedures. We have performed a wide range of procedures via single port[6] and got used to moving properly through the “hole”. However, with the location of the organ, far up and embedded in the left sub-diaphragmatic pouch, spleen has specific obstacles for single port procedures. The most important one was the visualization difficulties, especially during the dissection of the posterior attachments. Some-times we needed a lateral tilt of >20° in order to urge the spleen to fall medially. We have benefited from the long shaft of the 30° camera. This enhances the surgeon's extra-corporal movements preventing the interference with the light-source cable. In two cases, we have used a special 5.4 mm flexible tip camera, Olympus; LTF-VP (Olympus, Australia); as Targarona et al. have described before.-[23] By the help of this technological innovation, a surgical team can easily “see behind the wall”. As the camera assistant pushes the camera shaft downwards out-side the patient, the tip rises up above the operating field leaving the space for the working instruments of the surgeon. This manoeuvre leads to loss of the point of view with 30° standard camera. However, the flexible tip of the device successfully bends over the “peak” of spleen just like the neck of a swine with gently movements and makes the “dark side of the moon” visible. This camera needs a camera operator who has endoscopic experience, but one can easily get used to angulations and movements of the flexible tip through the operation.
The well-known problem of SPA procedures is the clashing of instruments and interference with camera shaft intra-corporally and the light-source extra-corporally. We usually use one articulated and one straight instrument at the same time at the operating field because of the energy devices have straight shafts, and most of the dissection is done by the help of these devices. Surgeon and the camera operator must form a team and get used to each other in order to make complementary movements in and out-side the patient. We surely observed that this results from not only the intra-corporal interference of instruments with each other and camera, but also leads to uncomfortable positioning between camera operator and the surgeon out-side the patient.
The control of hilum is maintained by vascular staplers in most of the laparoscopic splenectomies in our clinic. The artery and vein are not separately dissected and not fully skeletonized. In group 1, the problem at the patient who converted to open was the lack of enough preparation of the hilum. When the patient was explored, the bleeding site was revealed as the stapler line. The staple heights were too short for the tissue which they are grasping. It was not because we chose the wrong stapler size, but lack of peeling off the fat-pad over the hilum itself. Moreover, in group 1, the patient who needed laparatomy during the early post-operative period due to bleeding had multiple parenchymal lacerations due to iatrogenic trauma of the instruments. The parenchymal lacerations can easily dealt with standard three-port laparoscopy. Continuous, but low-profile bleeding suddenly lead to hypotension and a separate port was placed at the left upper quadrant for suction-irrigation. We could not succeed to clean and visualize the hilum from the coagulum for control. An immediate laparotomy was done to securely complete the operation. Both of the patients had platelet counts <50.000 and had pre-operative steroid therapy.
The 2 cm incision enhances the morcellation and extraction of the spleen. We closed the abdominal defect with separate sutures of prolene 0, and no local anaesthetic was done for pain control.
The pain evaluation is a subjective issue varying among different patients. In this study, we used pain charts that were designed in standard VAS type, numbered from 0 to 10, as the pain increases from non to unbearable distress. The charts were given to the patients at the 6th and 24th h. They are told to mark the appropriate colour that represent their actual pain they are feeling, and repeat the test 5 min later to make another mark. After the day of the discharge plenty of charts were given to the patients to fill up at home. Besides that, only the hospital evaluation charts showed a significant difference of the perception of pain in SPA group when compared to multi-port group. We think that this might be due to the pre-operative informative interviews of the surgical team with the patients. Patients in SPA group were informed about the single port procedure, and we assumed to have less pain at the end.
In our opinion, SPA splenectomy is becoming a feasible alternative to standard laparoscopic method with the innovative technologies immerging into the surgical area day by day. We think that the longer operative times and neglectable complications will be fading by time as global experience accumulates. Surgeons are focusing on minimizing operative trauma and patients are demanding minimally invasive procedures as conventional therapies. Single port procedures are gaining wide acceptance and splenectomy through single port seems to be a secure alternative offering good cosmesis and pain control in the early post-operative period.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Sutherland GA, Burghard FF. The treatment of splenic anaemia by splenectomy. Lancet. 1910;2:1819–22. [Google Scholar]
- 2.Delaitre B, Maignien B. Splenectomy by the laparoscopic approach. Report of a case. Presse Med. 1991;20:2263. [PubMed] [Google Scholar]
- 3.Cogliandolo A, Berland-Dai B, Pidoto RR, Marc OS. Results of laparoscopic and open splenectomy for nontraumatic diseases. Surg Laparosc Endosc Percutan Tech. 2001;11:256–61. doi: 10.1097/00129689-200108000-00006. [DOI] [PubMed] [Google Scholar]
- 4.Katkhouda N, Grant SW, Mavor E, Friedlander MH, Lord RV, Achanta K, et al. Predictors of response after laparoscopic splenectomy for immune thrombocytopenic purpura. Surg Endosc. 2001;15:484–8. doi: 10.1007/s004640000355. [DOI] [PubMed] [Google Scholar]
- 5.Rosen M, Brody F, Walsh RM, Tarnoff M, Malm J, Ponsky J. Outcome of laparoscopic splenectomy based on hematologic indication. Surg Endosc. 2002;16:272–9. doi: 10.1007/s00464-001-8150-6. [DOI] [PubMed] [Google Scholar]
- 6.Barbaros U, Dinççag A. Single incision laparoscopic splenectomy: The first two cases. J Gastrointest Surg. 2009;13:1520–3. doi: 10.1007/s11605-009-0869-8. [DOI] [PubMed] [Google Scholar]
- 7.Wewers ME, Lowe NK. A critical review of visual analogue scales in the measurement of clinical phenomena. Res Nurs Health. 1990;13:227–36. doi: 10.1002/nur.4770130405. [DOI] [PubMed] [Google Scholar]
- 8.Park A, Gagner M, Pomp A. The lateral approach to laparoscopic splenectomy. Am J Surg. 1997;173:126–30. doi: 10.1016/S0002-9610(97)89602-X. [DOI] [PubMed] [Google Scholar]
- 9.Walsh RM, Heniford BT. Laparoscopic splenectomy for non-Hodgkin lymphoma. J Surg Oncol. 1999;70:116–21. doi: 10.1002/(sici)1096-9098(199902)70:2<116::aid-jso10>3.0.co;2-y. [DOI] [PubMed] [Google Scholar]
- 10.Dallemagne B, Perretta S, Allemann P, Donatelli G, Asakuma M, Mutter D, et al. Transgastric cholecystectomy: From the laboratory to clinical implementation. World J Gastrointest Surg. 2010;27(2):187–92. doi: 10.4240/wjgs.v2.i6.187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Shin EJ, Jeong GA, Jung JC, Cho GS, Lim CW, Kim HC, et al. Transvaginal endoscopic appendectomy. J Korean Soc Coloproctol. 2010;26:429–32. doi: 10.3393/jksc.2010.26.6.429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kaouk JH, White WM, Goel RK, Brethauer S, Crouzet S, Rackley RR, et al. NOTES transvaginal nephrectomy: First human experience. Urology. 2009;74:5–8. doi: 10.1016/j.urology.2009.03.030. [DOI] [PubMed] [Google Scholar]
- 13.Targarona EM, Pallares JL, Balague C, Luppi CR, Marinello F, Hernández P, et al. Single incision approach for splenic diseases: A preliminary report on a series of 8 cases. Surg Endosc. 2010;24:2236–40. doi: 10.1007/s00464-010-0940-2. [DOI] [PubMed] [Google Scholar]
- 14.Malladi P, Hungness E, Nagle A. Single access laparoscopic splenectomy. JSLS. 2009;13:601–4. doi: 10.4293/108680809X12589999538039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Srikanth G, Wasim MD, Sajjad A, Shetty N. Single-incision laparoscopic splenectomy with innovative gastric traction suture. J Minim Access Surg. 2011;7:68–70. doi: 10.4103/0972-9941.72386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Joshi M, Kurhade S, Peethambaram MS, Kalghatgi S, Narsimhan M, Ardhanari R. Single-incision laparoscopic splenectomy. J Minim Access Surg. 2011;7:65–7. doi: 10.4103/0972-9941.72385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tam YH, Lee KH, Sihoe JD, Chan KW, Cheung ST, Pang KK. Initial experience in children using conventional laparoscopic instruments in single-incision laparoscopic surgery. J Pediatr Surg. 2010;45:2381–5. doi: 10.1016/j.jpedsurg.2010.08.036. [DOI] [PubMed] [Google Scholar]
- 18.Dapri G, Casali L, Bruyns J, Himpens J, Cadiere GB. Single-access laparoscopic surgery using new curved reusable instruments: Initial hundred patients. Surg Technol Int. 2010;20:21–35. [PubMed] [Google Scholar]
- 19.Barbaros U, Sümer A, Tunca F, Gözkün O, Demirel T, Bilge O, et al. Our early experiences with single-incision laparoscopic surgery: The first 32 patients. Surg Laparosc Endosc Percutan Tech. 2010;20:306–11. doi: 10.1097/SLE.0b013e3181f20cf6. [DOI] [PubMed] [Google Scholar]
- 20.Hansen EN, Muensterer OJ. Single incision laparoscopic splenectomy in a 5-year-old with hereditary spherocytosis. JSLS. 2010;14:286–8. doi: 10.4293/108680810X12785289144809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rottman SJ, Podolsky ER, Kim E, Kern J, Curcillo PG., 2nd Single port access (SPA) splenectomy. JSLS. 2010;14:48–52. doi: 10.4293/108680810X12674612014509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Vatansev C, Ece I., Jr Single incision laparoscopic splenectomy with double port. Surg Laparosc Endosc Percutan Tech. 2009;19:e225–7. doi: 10.1097/SLE.0b013e3181c4efab. [DOI] [PubMed] [Google Scholar]
- 23.Targarona EM, Balague C, Martinez C, Pallares L, Estalella L, Trias M. Single-port access: A feasible alternative to conventional laparoscopic splenectomy. Surg Innov. 2009;16:348–52. doi: 10.1177/1553350609353765. [DOI] [PubMed] [Google Scholar]


