Abstract
The relation between the quantity of many healthcare services delivered and health outcomes is uncertain. In January 2004, the Centers for Medicare and Medicaid Services introduced a tiered fee-for-service system for patients on hemodialysis, creating an incentive for providers to see patients more frequently. We analyzed the effect of this change on patient mortality, transplant wait-listing, and costs. While mortality rates for Medicare beneficiaries on hemodialysis declined after reimbursement reform, mortality declined more – or was no different – among patients whose providers were not affected by the economic incentive. Similarly, improved placement of patients on the kidney transplant waitlist was no different among patients whose providers were not affected by the economic incentive; payments for dialysis visits increased 13.7% in the year following reform. The payment system designed to increase provider visits to hemodialysis patients increased Medicare costs with no evidence of a benefit on survival or kidney transplant listing.
1. Introduction
In 2006 Medicare spending in the United States varied more than threefold across different geographic regions. (Fisher, Goodman et al. 2009) Yet, the relation between healthcare spending, the quantity of healthcare used, and health outcomes is uncertain. Studies from the Dartmouth Atlas project comparing regional differences in end-of-life care found no direct association between medical spending and health outcomes, quality of care, or access to care among patients hospitalized for hip fracture, colorectal cancer, or acute myocardial infarction. (Fisher, Wennberg et al. 2003; Fisher, Wennberg et al. 2003) One study found that areas with higher Medicare spending per beneficiary and more physician specialists had lower quality of care. (Baicker and Chandra 2004) In contrast, a state-level study found a positive association between the number of physicians practicing in an area and healthcare quality (Cooper 2009), while an analysis using an instrumental variable approach found that greater Medicare spending was associated with reduced mortality and hospitalizations. (Hadley and Reschovsky 2012).
Observed heterogeneity in the relation between the quantity of healthcare delivered and health outcomes may be due either to differences in methods used among studies or in the populations studied. In the context of a health production function with diminishing marginal returns from additional healthcare production, some patient populations may be at the “flat of the curve,” where additional healthcare does not lead to improved health outcomes. Other patient populations may be at the steep end of the curve, where additional healthcare improves outcomes. (Grossman 1972; Garber and Skinner 2008) An example of a patient population at the steep end of the curve – most likely to benefit from additional healthcare – includes patients with chronic illness who were recently hospitalized. It is not surprising that more intensive healthcare delivery is associated with improved health outcomes in patients recently hospitalized for Chronic Obstructive Pulmonary Disease and Congestive Heart Failure. (Rich, Beckham et al. 1995; Sharma, Kuo et al. 2010)
Because patients with end-stage renal disease (ESRD) receiving hemodialysis suffer from multiple medical co-morbidities and high mortality, they may benefit from more intensive healthcare delivery. Patients with ESRD require life-long renal replacement therapy. The most common form of renal replacement therapy in the United States – in-center hemodialysis – involves patients going to a hemodialysis center for several hours of treatment three or four times per week. Patients receiving hemodialysis are hospitalized an average of twice per year, and suffer from a mortality rate of approximately 20% per year. (USRDS 2013) At the same time, patients with ESRD already receive a disproportionate share of healthcare resources. While patients with ESRD comprise only 1.2 percent of the Medicare population, in 2011 the federal government spent $34 billion, or 6.2% of the total Medicare budget on its ESRD program. (USRDS 2013)
Physician service intensity is closely linked to Medicare fees; higher fees to physicians lead to a greater quantity of care delivered. (Hadley and Reschovsky 2006) Consequently, changes in physician reimbursement that influence physician service intensity can serve as a natural experiment to test the relation between the quantity of care delivered and health outcomes, avoiding many of the biases inherent in cross-sectional comparisons.
In 2004 the Centers for Medicare and Medicaid Services (CMS) fundamentally transformed reimbursement to physicians and advanced practitioners caring for patients receiving hemodialysis from a capitated system to a tiered fee-for-service system (referred to as “G-code” reimbursement). (Centers for and Medicaid Services 2003) The tiered fee-for-service system was structured to encourage more frequent physician visits. While the G-code reimbursement reform applied to all patients with Traditional Medicare coverage, it did not affect reimbursement to providers caring for patients with Medicare Advantage/HMOs, who remained on a capitated system.
In this study we use the incentive to see patients more frequently created by G-code reimbursement reform to assess the relation between quantity of care delivered and health outcomes in patients with ESRD receiving hemodialysis. We use patients covered by Medicare Advantage/HMOs as “controls” in difference-in-difference analyses where we compare the relative change in health outcomes before vs. after G-code reimbursement. Our main study outcome is mortality. We also determine whether reimbursement reform led to improved kidney transplant wait listing, and we examine direct costs associated with reimbursement reform.
This study builds upon past evidence that physician visit frequency to patients on hemodialysis increased in response to G-code reimbursement reform. We verify that visit frequency to patients receiving hemodialysis who were covered by Traditional Medicare increased nationally in the period following G-code reimbursement reform. We demonstrate that the increase in visit frequency was less profound in dialysis facilities with a larger proportion of patients covered by Medicare Advantage HMOs, supporting our assertion that patients covered by Medicare Advantage/HMOs were not affected by the reimbursement policy. Using multivariable Cox models, we show that adjusted mortality was lower in the period after G-code reimbursement reform compared to the period prior to the reform in all Medicare patients (i.e. patients covered by Traditional Medicare and patients covered by Medicare Advantage/HMOs). Then, in a difference-in-difference analysis, we demonstrate that reductions in mortality were not greater (and may have been attenuated) in patients covered by Traditional Medicare who were affected by the reimbursement policy compared to patients not affected by the policy. Likewise, we show that the change in the “hazard” of being placed on the list for a kidney transplant was not different in patients who were affected by the policy compared to those not affected by the policy. Finally, we show that payment to outpatient nephrologists temporarily increased by 13.7% in the period following reimbursement reform.
Our results suggest that, in hemodialysis care, a policy encouraging increased healthcare use did not lead to improved health outcomes, while increasing healthcare costs. This is consistent with findings from the Dartmouth Atlas project that increased healthcare use is not associated with health outcomes.
2. Background
Due to a Federal law passed in 1972, nearly all patients with ESRD are eligible for and receive Medicare coverage regardless of age (Security Amendments of 1972). The Centers for Medicare and Medicaid Services (CMS) uses its role as the predominant payer of dialysis services to influence the behavior of healthcare providers. Before 2004, CMS reimbursed physicians and physician extenders caring for patients on hemodialysis through a capitated payment system; providers received the same amount regardless of the number of times per month patients were seen. In part responding to a presumed benefit from more frequent face-to-face physician visits, in 2004 CMS fundamentally transformed reimbursement for physician-based hemodialysis care by implementing a tiered fee-for-service reimbursement system referred to as “G-codes” (Centers for Medicare & Medicaid Services 2003). Under the new system, providers were remunerated according to how often they saw patients, with a smaller incremental payment for each additional visit up to four or more visits per month. (Table 1)
Table 1.
Tiered Fee-for-service Medicare Reimbursement Schedule Following “G-code” Reform in 2004
| Code | National average fee | |
|---|---|---|
| 1 visit | G0319 | $201 per month |
| 2–3 visits | G0318 | $252 per month |
| 4 or more visits | G0317 | $303 per month |
Source: (Upchurch 2004)
In the past, the delivery of care for patients with end-stage renal disease has been sensitive to economic incentives created by Medicare reimbursement policy. (Iglehart 2011; Swaminathan, Mor et al. 2012) Anecdotal evidence, and one formal analysis, demonstrated that providers also responded promptly to the economic incentive created by G-code reimbursement by seeing patients more frequently (Upchurch 2004; Mentari, DeOreo et al. 2005; Larson 2007; Mueller 2007). A survey of 1,600 patients in 12 hemodialysis facilities conducted by Mentari et al. found that the average number of visits increased from 1.52 to 3.14 immediately following the G-code reimbursement incentive. There was also a trend in visits continuing to increase during the three months following the reimbursement reform. While this payment structure is now a permanent part of the monthly capitation payment to nephrologists, it is unknown whether this incentive for more frequent face-to-face contacts affected healthcare costs and resulted in the anticipated improvements in health outcomes.
3. Data and Patient Selection
For the difference-in-difference analyses, we selected patients in the United States covered by Traditional Medicare Parts A&B and Medicare Advantage/HMOs starting hemodialysis upon ESRD diagnosis in the three years before and after G-code reimbursement (January 1, 2001 to January 1, 2007) from the United States Renal Data System (USRDS). The USRDS is a comprehensive database of all identifiable patients with ESRD in the United States. It contains patient and facility-level data on demographics, comorbidities, treatment modalities, insurance provider, and date of death or transplant. Because ESRD beneficiaries cannot switch to Medicare Advantage after developing ESRD, patients enrolled in Medicare Advantage coverage after developing ESRD were necessarily covered by Medicare Advantage prior to developing ESRD. Consequently, they are generally 65 or older. To balance “treatment” and “control” groups we only included patients 65 and older with Traditional Medicare or Medicare Advantage coverage at the time of dialysis initiation. Patients starting ESRD under age 65 and patients who acquired Medicare coverage 90 days after developing ESRD were excluded from this comparison group.
For analyses of provider response to reimbursement reform and cost of G-code reimbursement, we selected cohorts of prevalent patients receiving hemodialysis. We included patients of all ages and used Medicare claims to determine physician visit frequency and payment for physician visits.
The data in the USRDS database came from the following sources: Medicare Enrollment Database; Medicare inpatient and outpatient claims; ESRD Medical Evidence Report forms (CMS-2728) filled out by healthcare providers upon initiation of hemodialysis; the United Network for Organ Sharing (UNOS) database, and ESRD death notification forms (CMS-2746). Information about dialysis facilities came from the CMS Annual Facility Survey (CMS-2477A). We obtained data on population density from zip-code level Rural Urban Commuting Area (RUCA) codes, a classification system using definitions and work commuting information from the 2000 US census (WWAMI Rural Health Research Center 2005).
4. Provider Response to Reimbursement Reform
4.1 Response to Reimbursement Reform in Patients with Traditional Medicare
Anecdotal evidence, and one formal analysis, demonstrated that providers responded promptly to the economic incentive created by G-code reimbursement. (Upchurch 2004; Mentari, DeOreo et al. 2005; Larson 2007; Mueller 2007) We verify that a similar response occurred in our national cohort by examining visit frequency in the period immediately following G-code reimbursement reform.
Prior to G-code reimbursement, payment to physicians (and advanced practitioners) for outpatient hemodialysis was capitated on a monthly basis. Consequently, Medicare claims data prior to enactment of G-code reimbursement do not contain information on outpatient nephrologist visit frequency. To our knowledge, there is no national-level data on outpatient visit frequency to patients on hemodialysis in the years prior to 2004. While the survey by Mentari et al. demonstrated that most of the provider response to G-code reimbursement occurred immediately at the time of the reimbursement reform, it also illustrated continued visit increases in February and March of 2004. (Mentari, DeOreo et al. 2005) This suggests that some providers exhibited a delayed response to the policy. We used our national data set to examine whether providers continued to respond to the policy in the months following G-code reimbursement.
We constructed a “prevalent hemodialysis cohort” consisting of all prevalent patients receiving in-center hemodialysis who were covered by Medicare Parts A&B in the two years following G-code reimbursement reform (2004 and 2005). We used Medicare claims to determine, for every month, how often patients were seen. We assigned visits according to the G-code claimed each month where: G0319 = one visit, G0318 = two to three visits; G0317 = four or more visits. We assumed patients were not seen by their provider in months when no claims were paid. The focus of this analysis was on provider practice patterns following reimbursement reform. Consequently, we excluded months when patients were hospitalized for more than two days, since patients would not be physically present at their outpatient dialysis facility for as many days in those months which could lead to reduced visits independent of provider practices. We also excluded months when a patient died or changed provider, dialysis modality or insurance type.
For each month, we determined the proportion of patients in the United States seen four or more times and the mean number of visits per month. We assumed that claims for two-to-three visits represented 2.5 visits and claims for four or more visits represented four visits. We plotted monthly visits following reimbursement reform and assessed for an upward trend in the proportion of patients with four-or-more visits and in estimated visits in the three months following enactment of G-code reimbursement.
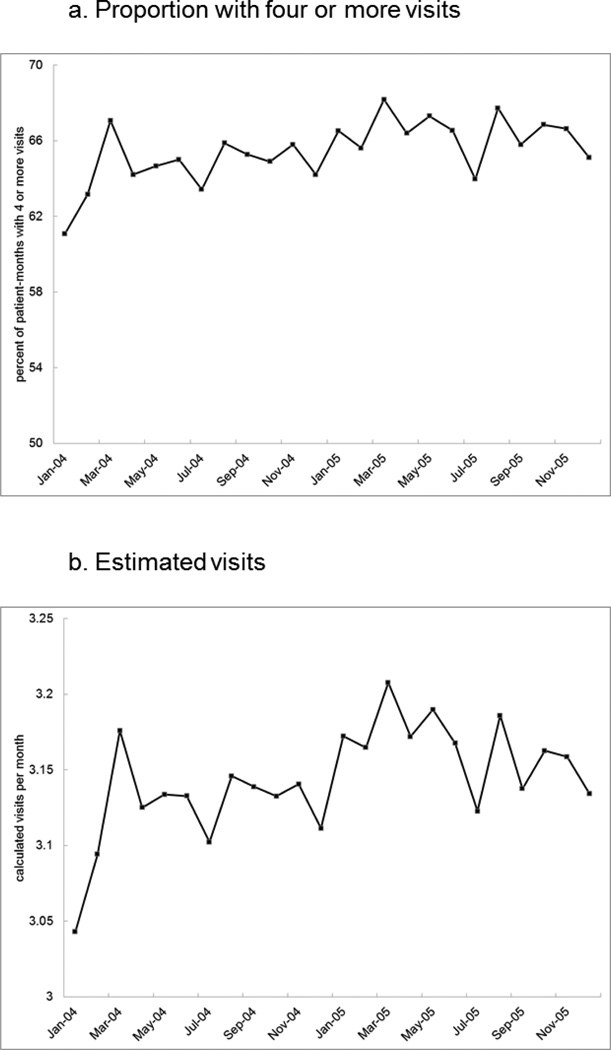
Visit frequency increased as expected following enactment of G-code reimbursement. In January 2004, 61.1% of patients were seen four or more times per month, and patients were seen approximately 3.04 times per month. Two months later, in March 2004, the proportion of months with four or more visits increased by 9.8% to 67.1% of months. Similarly, estimated mean visit frequency increased 4.4% to 3.18 visits per month. Visit frequency remained near these increased levels over the subsequent 21 months. (Figure 1)
Figure 1. Increase in Visit Frequency Following G-code Reimbursement.
Source: United States Renal Data System
Note: Estimates were derived from linear combination of regression coeficients.
Source: USRDS
4.2 Response to Reimbursement Reform in Patients with Medicare Advantage/HMOs
We examined whether patients receiving hemodialysis who were covered by Medicare Advantage/HMOs were less likely to have experienced an increase in visits from their provider following G-code reimbursement reform. Individual Medicare claims are not available for this population. Consequently, we were not able to directly observe visit frequency to patients covered by Medicare Advantage/HMOs. Instead, we developed a method of indirectly observing the change in visit frequency following G-code reimbursement to patients covered by Medicare Advantage/HMOs by measuring visits to patients covered by Traditional Medicare who were dialyzed at the same facilities as patients with Medicare Advantage/HMOs.
Our method has a theoretical basis in our prior work on physician (and advanced practitioner) visit frequency to patients receiving hemodialysis. (Erickson 2013) In that study, we demonstrated that providers tend to see all patients at a given dialysis facility a similar number of times per month, regardless of differences in acuity of illness among individual patients. Additionally, we demonstrated that providers caring for patients on hemodialysis choose how often to visit dialysis facilities based, in part, on economic incentives. In particular, providers were less likely to visit patients dialyzed in more rural areas where, on average, providers have to travel longer distances to see patients on hemodialysis. They were also less likely to see patients at dialysis facilities with fewer patients, presumably due to a higher travel costs to these facilities per patient seen.
Following G-code reimbursement providers had less of an incentive to increase visits to patients in facilities with a larger share of HMO patients. We first consider a scenario where providers choose how often to visit individual dialysis facilities, but once at a given facility, do not selectively see patients according to insurance type. In this scenario, providers would be reimbursed less for traveling to – and seeing patients in – facilities with a larger Medicare Advantage/HMO share. This is because they would only be reimbursed for the Traditional Medicare portion of their total visits to that facility; they would not be reimbursed for additional visits to the HMO patients. This can be expected to lead to fewer visits to all patients dialyzed in facilities with larger Medicare Advantage/HMO populations, as providers will instead visit facilities with a larger share of Traditional Medicare patients.
Next, we consider an alternative scenario where providers choose how often to visit individual dialysis facilities and, once at a given facility, discriminate between patients based on insurance type. In this case, there would still be a financial disincentive to see all patients in facilities with a larger HMO proportion since these facilities would effectively be smaller than their facility size otherwise indicates; for a given dialysis facility size, there would be fewer patients who the provider can be reimbursed for seeing after travel to the facility. Fixed travel costs would be distributed over fewer patients in facilities with a larger share of HMO patients, thereby reducing the incentive to increase visits to all patients in these facilities. In both scenarios, decreased visits to patients covered by Medicare Advantage/HMOs correspond to decreased visits to patients with Traditional Medicare at the same dialysis facility.
We tested whether the economic disincentive to seeing patients with Medicare Advantage/HMOs had its predicted effect by examining visit frequency to patients covered by Traditional Medicare who receive dialysis at facilities with Medicare Advantage/HMO patients. To do this, we constructed a multivariable logistic regression model where the outcome of interest was the proportion of patients with Traditional Medicare coverage seen four or more times in a given month. We used the “prevalent hemodialysis cohort” described above, and included patients receiving dialysis in the first three months following G-code reimbursement (the months when visit frequency continued to increase). The following equation illustrates this model:
Where “PropHMO” represents the proportion of all patients in a facility covered by Medicare Advantage/HMOs in a given month, “Feb04” and “Mar04” are dummy variables representing each month, and “X” are patient and facility characteristics listed in Table 2 (including dialysis facility size), in addition to population density using rural/urban commuting area (RUCA) codes.(WWAMI 2005) We used cluster robust standard errors to account for visit frequency correlation among patients and dialysis facilities.(Huber 1967)
Table 2.
Baseline Characteristics
| Medicare Parts A&B1 | Medicare Advantage1 | |||
|---|---|---|---|---|
| Pre-G-code | Post G-code | Pre-G-code | Post G-code | |
| n = 88,994 | n = 85,258 | n = 16,751 | n = 16,778 | |
| Age - yr (SD) | 75.2 (6.5) | 75.5 (6.7) | 75.2 (6.4) | 75.6 (6.4) |
| Sex - % female | 50.3 | 52.2 | 53.9 | 54.9 |
| Race or ethnic group - % | ||||
| White | 71.8 | 73.7 | 72.9 | 71.9 |
| Black | 22.8 | 21.5 | 20.3 | 21.6 |
| Asian† | 1.8 | 2.2 | 3.5 | 3.9 |
| American Indian | 0.8 | 0.8 | 0.2 | 0.2 |
| Other race2 | 2.8 | 1.8 | 3.1 | 2.4 |
| Hispanic ethnicity† | 8.7 | 8.8 | 12.7 | 14.4 |
| Socioeconomic - % | ||||
| Employed3 | 6.9 | 6.4 | 7.1 | 6.8 |
| Medicaid coverage† | 21.4 | 21.7 | 4.8* | 8.6* |
| Smoking history | 3.2 | 3.6 | 2.6 | 2.9 |
| Alcohol abuse | 0.7 | 0.6 | 0.5 | 0.5 |
| Drug use | 0.1 | 0.1 | 0.1 | 0.1 |
| Comorbid conditions - % | ||||
| EPO prior to HD | 33.9 | 34.8 | 34.1 | 34.5 |
| Peripheral vascular disease | 18.7 | 19.2 | 15.6 | 16.3 |
| Hypertension | 81.3 | 84.0 | 80.2 | 83.1 |
| Cerebral vascular disease | 12.4 | 12.4 | 10.9 | 11.4 |
| Heart failure | 40.7 | 42.3 | 37.3 | 39.5 |
| Malignancy | 8.7 | 10.0 | 8.0 | 8.8 |
| Coronary disease | 37.9 | 34.8 | 34.6 | 31.4 |
| Immobile | 4.9 | 7.1 | 3.9* | 6.1* |
| Pulmonary disease | 10.9 | 12.4 | 9.1 | 10.0 |
| Diabetes | 51.3 | 52.3 | 49.7 | 52.4 |
| Weight - kg (SD) | 73.4 (18.1)* | 75.6 (19.0)* | 72.6 (17.3)* | 74.9 (18.8)* |
| Facility Characteristics | ||||
| Facility size - # of patients (SD)† | 90.5 (60.1) | 89.4 (57.4) | 104.2 (64.7) | 100.8 (63.6) |
| For profit - % | 73.4 | 76.1 | 76.7 | 78.6 |
| Hospital based - % | 18.6 | 16.0 | 15.3 | 13.4 |
≥ 10% standardized difference:
before and after G-codes;
Traditional Medicare vs. Medicare Advantage
Includes patient 65 and older with insurance upon initiation of hemodialysis
Pacific Islander, Mideast, Indian subcontinent, multiracial, and unknown
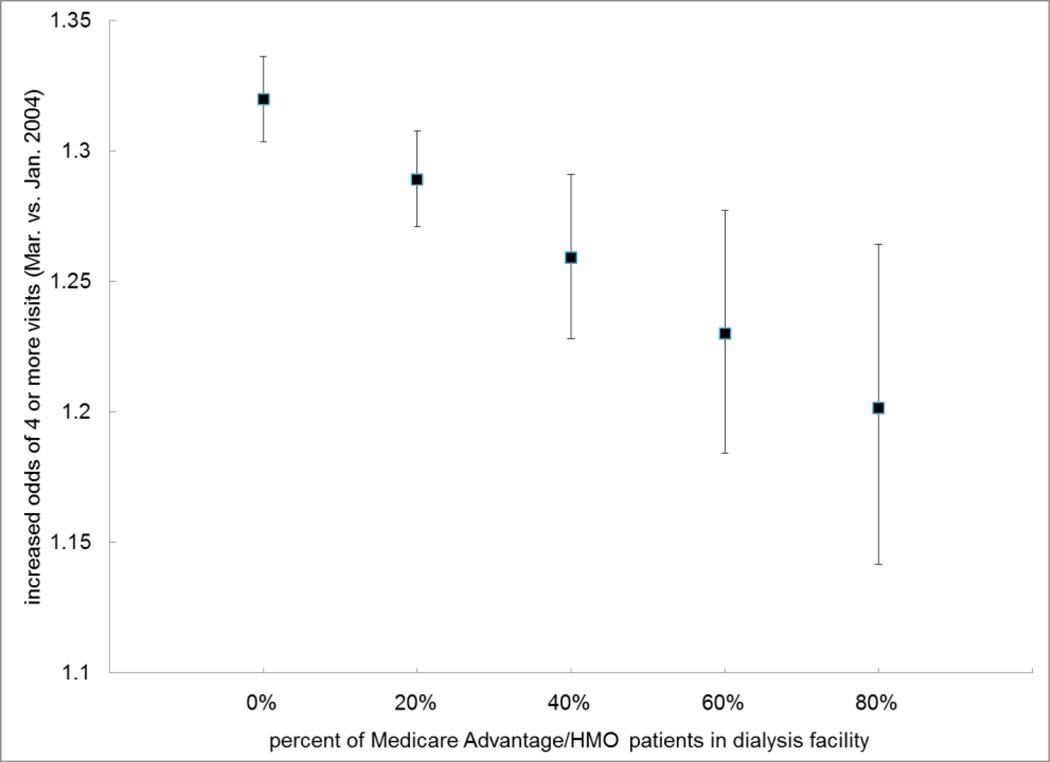
Based on this model, the interaction between the proportion of patients in a facility with HMO coverage and the dummy variables for February and March represent the effect that a larger share of facility HMO patients has on the increase in visit frequency to patients covered by Traditional Medicare. A negative interaction term is consistent with our hypothesis that the increase in visit frequency was diminished in facilities with a larger proportion of HMO patients due to the absence of an economic incentive to see HMO patients more frequently.
After adjusting for patient, facility and geographic characteristics, there was a 27.7% increase in the odds of four or more visits to patients in March 2004 compared to January 2004 (95% CI 26.5%–29.0%). (Table S1) This provides further evidence that some providers continued to respond to G-code reimbursement in the three months following the reform.
Providers responded as expected to the diminished economic incentive to travel to facilities with a larger share of Medicare Advantage/HMO patients. There was a negative interaction between the proportion of Medicare Advantage/HMO patients and the month following G-code reimbursement. This interaction was statistically significant for March 2004 (p=0.001). Figure 2 illustrates how the odds of four or more visits in March 2004 progressively decreased in dialysis facilities with a larger share of patients covered by Medicare Advantage/HMOs. This is consistent with our assertion that the change in visit frequency was less pronounced in patients covered by Medicare Advantage/HMOs.
Figure 2. Estimated Odds of Four or More Visits Varied by Share of Medicare Advantage/HMO Patients.
5. Study Design
The primary outcome was time-to-death in the first two years of hemodialysis as assessed by a proportional hazards regression model. We chose the first two years of hemodialysis since this is a period of high acuity when patients would most likely benefit from increased face-to-face provider visits. We only included patients surviving the transition to ESRD and on dialysis long enough to qualify for Medicare (defined as receiving renal replacement therapy for at least 90 days). This “90 day rule” is commonly used in analyses of the USRDS registry. (USRDS 2013) We censored patients if they changed insurance payer while receiving in-center hemodialysis or after two years of ESRD treatment. We did not censor patients due to change in treatment modality (e.g. hemodialysis to either transplant or peritoneal dialysis) which we considered a potential consequence of more frequent provider visits since more frequent visits could increase the likelihood of discussion about home dialysis therapy or transplantation. A secondary outcome was time-to-wait-listing for kidney transplant, which we hypothesized would decrease as a consequence of more frequent interaction between providers and patients.
We measured the effect of G-code reimbursement on patient mortality using a difference-in-difference survival analysis. We compared survival before and after G-code reimbursement in a Cox regression model adjusting for individual comorbidities, demographics, facility characteristics, and state/territory of residence. We modeled whether a patient received hemodialysis before versus after G-codes as a time-varying covariate. We compared the change in survival following G-code reimbursement reform among patients covered by Traditional Medicare with those covered by Medicare Advantage (who were not affected by the policy). We described baseline characteristics, probability of death, and four year survival functions for each comparison group.
The following equation describes the difference-in-difference model:
Where “Medicare” is a dichotomous variable representing whether patients are enrolled in Traditional Medicare or Medicare Advantage, “Policy Change” is a dichotomous time-varying covariate denoting exposure prior to January 1st 2004 versus after the G-code reimbursement reform, and “Medicare*Policy Change” is a time-varying covariate interaction term identifying patients enrolled in Medicare Parts A&B after the policy change. “X” include facility characteristics, demographic characteristics, and comorbidities listed in Table 2 in addition to state of residence. Within this framework, γ represents the treatment effect of “G-code” reimbursement on hazard of death.
We used this survival model in an identical fashion to assess the effect of G-code reimbursement on time-to-wait-listing for a kidney transplant. In this analysis, an increased “hazard” of transplant wait-listing represents more rapid (i.e. improved) placement on the transplant wait list. In the analysis of time-to-wait-listing for kidney transplant, we restricted the cohort to patients aged 65 to 70 years at the time of ESRD development, due to a small likelihood of receiving a kidney transplant in older patients. Additionally, we excluded patients who were listed for a transplant prior to developing ESRD and with a diagnosis of malignancy at the time of developing ESRD.
This project was approved by the institutional review board of Stanford University School of Medicine.
6. Results
6.1 Baseline Characteristics
Our assessment of the effect of G-code reimbursement on mortality included 207,781 incident patients. The Medicare Advantage group comprised 16.1% of the population. Due to large population size, we used 10% standardized difference as a marker of heterogeneity between groups (Austin 2009). The percent of Asian and Hispanic population, the percent with Medicaid coverage, and facility size, varied according to insurance group. The Medicare Advantage group had proportionately more immobile patients and Medicaid coverage following G-codes. (Table 2)
The probability of death declined after enactment of G-codes in both comparison groups. Patients with Traditional Medicare coverage experienced a probability of death in the first two years of hemodialysis of 46.1% when starting dialysis before enactment of g-codes and 44.7% when starting dialysis after G-codes (difference: −1.4%; p<0.001). Patients with Medicare Advantage experienced a two-year probability of death of 39.5% when starting dialysis prior to G-code reimbursement and 38.9% after the policy (difference: −0.7%; p<0.20).
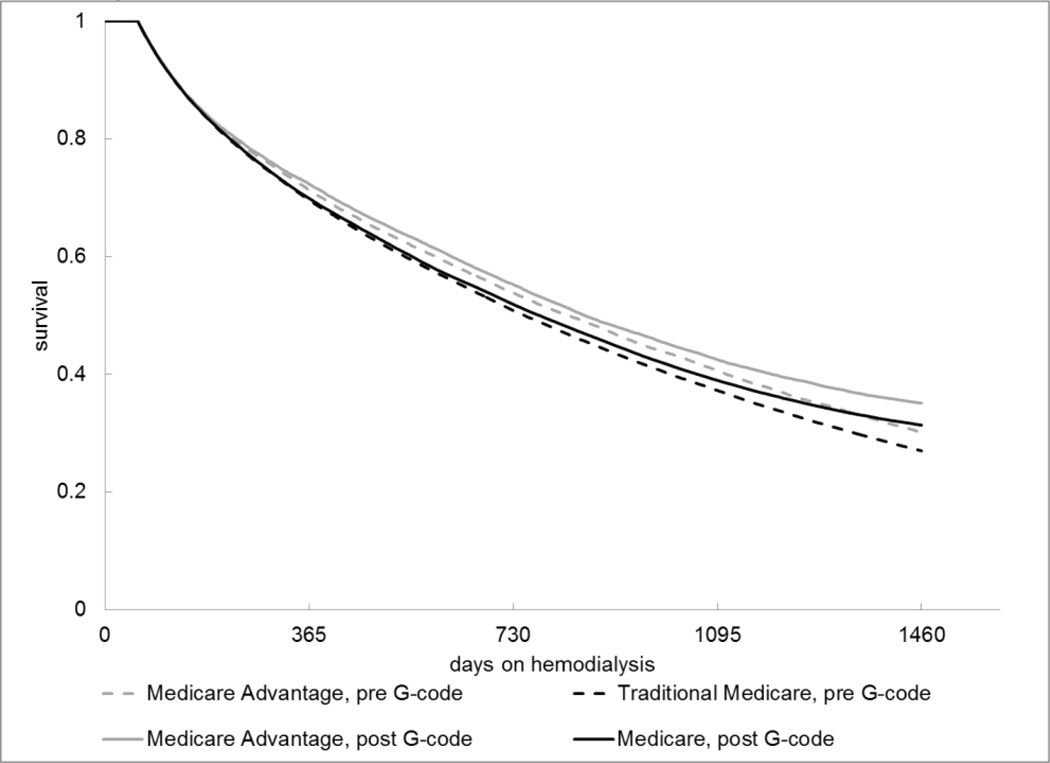
6.2 Survival Plot
Survival plots of each comparison group demonstrate that the first two years (the time interval included in our regression analyses) are a period of high acuity where mortality rates are particularly high. Additionally, unadjusted survival improved in both groups in the period following G-code reimbursement (p<0.001 in a Log Rank test of survival curves for all groups). (Figure 1)
Figure 1. Survival Before and After Reimbursement Reform by Insurance Coverage.
Source: United States Renal Data System Database
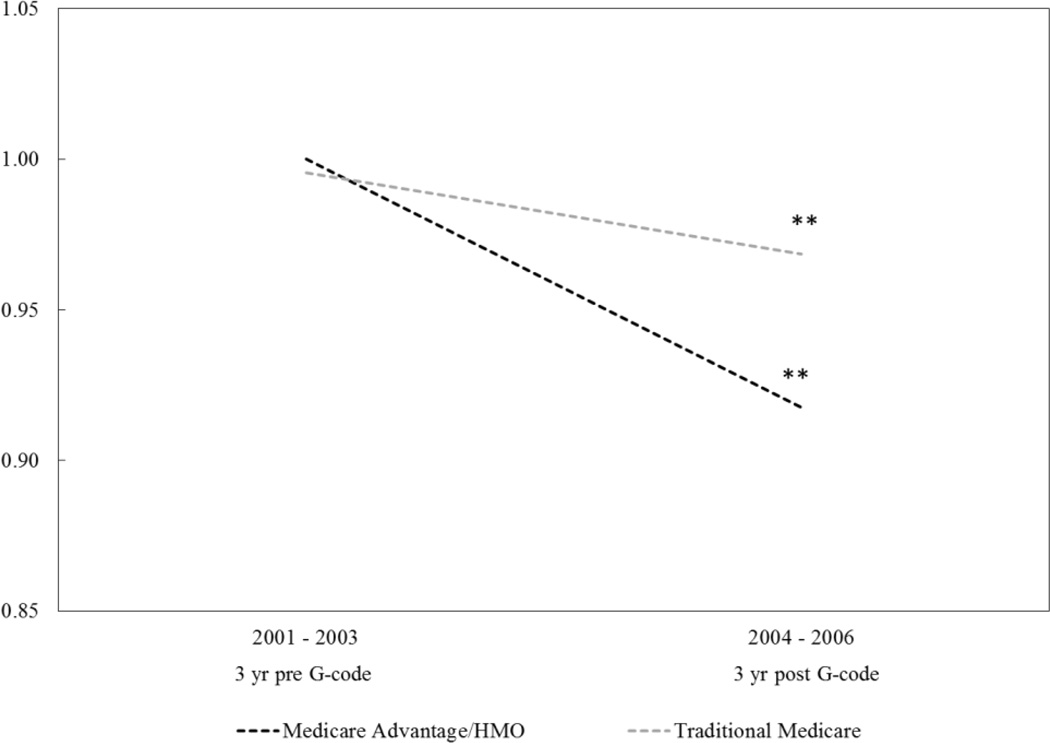
6.3 Effect of Reimbursement Reform on Mortality
A difference-in-difference analysis compared change in survival experienced by Traditional Medicare and Medicare Advantage patients following G-code reimbursement. Adjusted mortality improved (decreased) in patients covered by Traditional Medicare as well as patients covered by Medicare Advantage/HMOs. However, adjusted mortality improved (decreased) more for patients on Medicare Advantage (control group) than it did in patients covered by Traditional Medicare (treatment group). While patients on Traditional Medicare and Medicare Advantage had similar adjusted mortality hazards in the three years prior to 2004 (non-significant difference of 0.5%), patients enrolled in Medicare Advantage experienced an 8.4% decline in adjusted mortality hazard (p<0.001) following G-code enactment while patients enrolled in Traditional Medicare experienced a 2.8% reduction (p<0.001). This difference was statistically significant (p=0.002). (Figure 2)
Figure 2. Change in Relative Mortality Hazards Before and After G-code Enactment.
Note: ** p-value < 0.001 for difference between comparison groups at specified time period. See Tables S2– S3 for full regression results. Regressions adjust for patient, facility, and geographic characteristics in addition to state/territory.
Source: United States Renal Data System
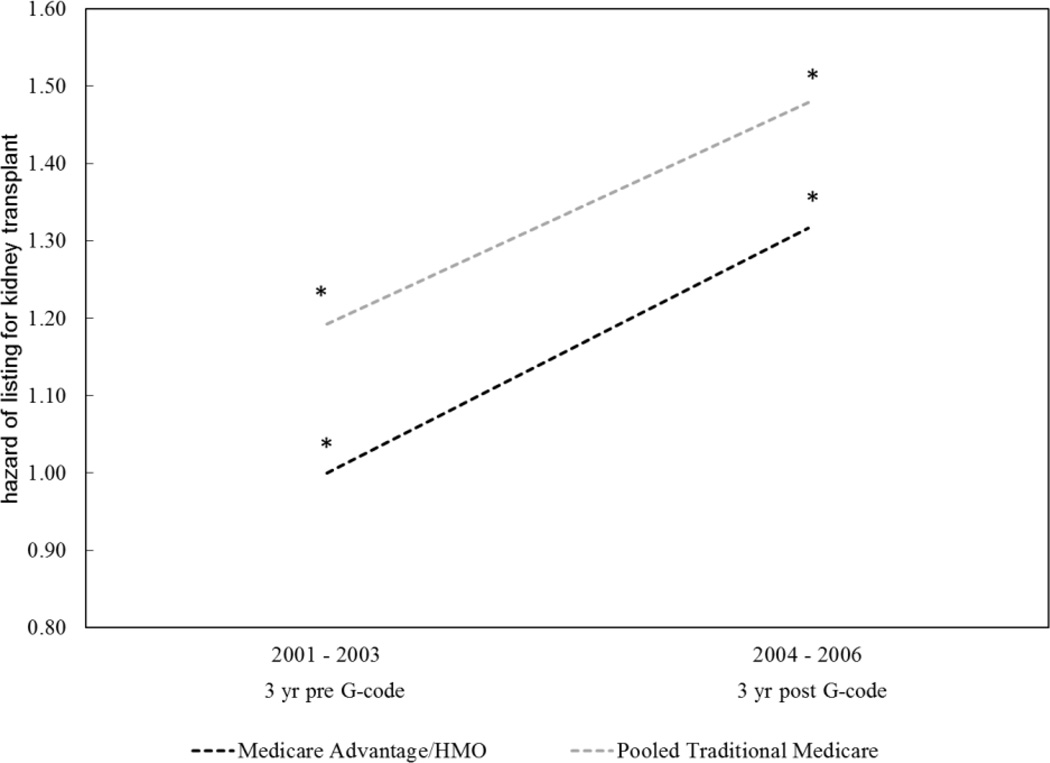
6.4 Effect of Reimbursement Reform on Time-to-wait-listing for Kidney Transplant
A second difference-in-difference analysis compared change in time-to-wait-listing for kidney transplant following G-code reimbursement experienced by patients aged 65–70 upon development of ESRD enrolled in Traditional Medicare versus Medicare Advantage. This analysis included 44,794 patients. Patients enrolled in Traditional Medicare had more rapid listing for kidney transplants in the period prior to G-code reimbursement compared to patients enrolled in Medicare Advantage (hazard ratio 1.19, p=0.03). Patients enrolled in both Traditional Medicare and Medicare Advantage experienced improved time-to-listing for kidney transplant in the period following reimbursement reform (hazard ratios 1.24, p<0.001; 1.32, p=0.002, respectively). The relative difference in the improvement observed in the two groups was not statistically significant (p=0.53). (Figure 3; Table S4)
Figure 3. Change in Relative “Hazard” of Listing for Kidney Transplant Before and After G-code Enactment.
Note: Increased “hazard” of listing means improved (i.e. shorter) listing for kidney transplant.
* p-value < 0.05 for difference between comparison groups at specified time period. See Table S4 for more detailed regression model results. Regressions adjust for patient, facility, and geographic characteristics in addition to state/territory.
Source: United States Renal Data System
6.5 Sensitivity Analyses
We tested the sensitivity of our main study findings to the following parameters: 1) censoring at transplant and due to insurance provider change; 2) duration of follow-up; 3) study period; 4) possible facility fixed effects; 5) inclusion of hemoglobin and albumin as covariates (which were excluded from the primary analysis due to large number of missing values); 6) excluding patients who “bridge” the policy (who were incorporated in the baseline analysis using a time-varying covariate); 5) possibility of underlying trends in treatment and control groups over time. When testing for facility fixed effects, we used difference-in-difference linear probability models where the outcome was the probability of death in the first year of hemodialysis and where patients who develop ESRD in 2003 were excluded since their year of follow-up bridges the policy change. We accounted for the possibility of differences in underlying linear trends in mortality between comparison groups in a difference-in-difference-in-difference model, using data on incident hemodialysis patients dating back to 1995.
All but one of the sensitivity analyses demonstrate either a statistically significant or non-significant trend towards higher (i.e, worse) mortality in patient groups most effected by G-code reimbursement. The exception was the analysis where we excluded patients who “bridge” the policy gap, which found no difference. (Table 3)
Table 3.
Results from Sensitivity Analyses Examining Patient Mortality
| Sensitivity Analysis | "Policy Effect" Coefficient1 | LCI | UCI | p-value |
|---|---|---|---|---|
| Censor patients at transplant - HR | 1.061 | 1.021 | 1.102 | 0.002 |
| Intention to treat insurance group comparison2 -HR | 1.043 | 1.007 | 1.082 | 0.020 |
| Additional (3rd) year of follow-up - HR | 1.043 | 1.007 | 1.081 | 0.019 |
| Extending study period through 2007 - HR | 1.060 | 1.022 | 1.100 | 0.002 |
| Linear probability model of 1-year mortality including facility fixed effects - % change in probability3 | 0.900 | −0.220 | 0.200 | 0.114 |
| Include hemoglobin and albumin as covariates4 - HR | 1.037 | 0.990 | 1.087 | 0.126 |
| Excluding patients who "bridge" the policy - HR | 1.000 | 0.961 | 1.041 | 0.998 |
| Diff-in-diff-in-diff analysis accounting for time trends - one-time policy effect - HR | 1.036 | 0.878 | 1.223 | 0.674 |
| Diff-in-diff-in-diff analysis accounting for time trends - policy effect on annual trend - HR | 1.005 | 0.983 | 1.026 | 0.676 |
(G-code)*(treatment group) interaction term from model representing the effect of the policy change
Does not censor patients who change insurance groups
Measures absolute probability of mortality in 1st year of hemodialysis. Excludes patients who develop ESRD in 2003
Patients with missing hemoglobin and albumin values are excluded from this analysis
HR - Hazard ratio; LCI – Lower 95% confidence interval; UCI – Upper 95% confidence interval.
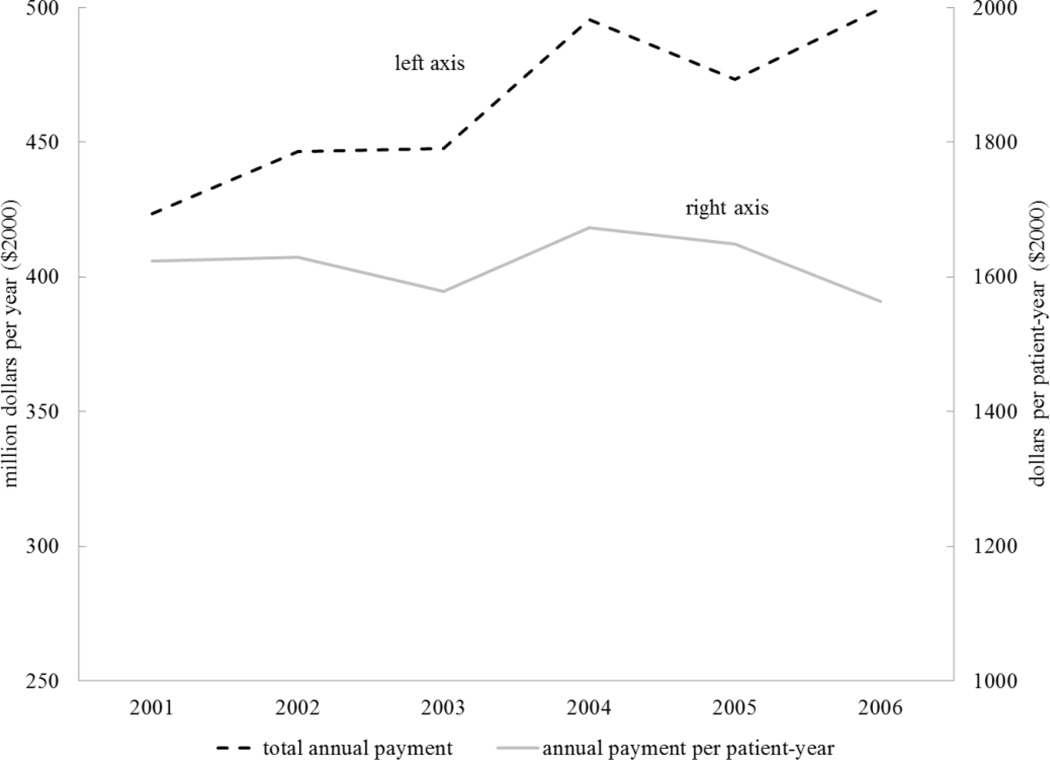
7. Estimating costs of G-codes
We calculated annual physician claims paid by Medicare for outpatient hemodialysis visits during the study period to determine whether direct costs paid to providers changed following G-code enactment. For this analysis we included prevalent patients with Traditional Medicare Parts A&B coverage receiving hemodialysis of all ages. We adjusted costs to 2010 dollars using the General Consumer Price Index (Bureau of Labor Statistics 2011) to account for inflation and presented them as total annual amounts and cost per patient-year of hemodialysis.
Payments to physicians and physician extenders for outpatient hemodialysis care increased by 65.3 million dollars (13.7%) from 2003 to 2004 after G-codes were enacted. After adjusting for inflation and changes in the number patients receiving hemodialysis, payments to providers increased 6.0% per patient-year between 2003 and 2004 (Bureau of Labor Statistics 2011). Provider payments trended back towards their pre G-code levels in 2005 and 2006 as inflation outpaced reimbursement increases and number of claims per patient-month decreased slightly. (Figure 4)
Figure 4. Medicare Payment for Outpatient Hemodialysis Visits.
Note: Data include Medicare claims paid to providers for outpatient care of patients receiving in-center hemodialysis. They include capitation payments and day- based payments (Healthcare Common Procedure Coding System codes 90921, 90925) prior to G-codes and G0317, G0318, G0319 following G- codes; adjusted to constant year 2000 U.S. Dollars using the Consumer Price Index for All Urban Consumers (Bureau of Labor Statistics). Payments for Medicare Advantage/HMO are not included in these estimates.
Source: United States Renal Data System. Bureau of Labor Statistics
8. Discussion
Although survival rates of patients new to hemodialysis improved following the transition to a tiered fee-for-service payment system that promoted more frequent face-to-face provider visits, survival improved in populations directly affected by the policy as well as those whose providers were not affected by the economic incentive. The difference-in-difference analysis of the policy’s effect on mortality demonstrated a larger mortality reduction in patients covered by Medicare Advantage/HMOs, who were not affected by the policy. Likewise, our analysis of time-to-wait-listing for kidney transplant demonstrated no difference in the improvement in transplant wait-listing among patients who were and were not affected by the economic incentive.
These results can be interpreted two ways. One possibility is that the economic incentive to see patients more frequently led to system-wide improvements in practice patterns and a “spill-over” effect that improved survival in all patients regardless of whether their providers were directly influenced by the economic incentive. For example, improved methods of monitoring and closer provider-patient relationships resulting from the policy could have led to the recent aggregate declines in the rate of hospitalization for vascular access failure and more referrals for transplantation. (USRDS 2013) Alternatively, the decline in mortality seen in both groups may have been due to patient or health-system improvements unrelated to the frequency of physician visits, which would suggest that enactment of G-code reimbursements was not the cause of the improved survival rates.
Several findings support the latter argument. First, this study demonstrates that patients whose providers were affected by the incentive to see patients more frequently actually may have experienced comparatively less improvement in mortality than those whose providers were not influenced by the economic incentive. This result would be unlikely if the policy was driving the improvements in survival. Additionally, a reduction in mortality occurred at the same time in populations such as those on peritoneal dialysis whose providers were even less likely to have been influenced by the change in reimbursement (since remuneration for peritoneal dialysis care remained capitated) (USRDS 2013).
More frequent visits could be expected to improve mortality in patients on hemodialysis through a number of mechanisms, including improved achievement of clinical targets, more rapid listing for kidney transplant, and better management of body fluid volume and vascular access. Previous epidemiological analyses assessing whether more frequent physician visits improve outcomes in patients on dialysis have generated mixed conclusions. Analyses conducted in 1995 and 2005 found more frequent physician visits were associated with lower mortality and improved achievement of laboratory-based quality targets (McClellan, Soucie et al. 1998; Plantinga, Jaar et al. 2005). In contrast, a study of visit frequency using a national dataset in the period around enactment of G-code reimbursement found no change in mortality and a slight reduction in hospitalizations in patients seen more frequently (Slinin, Guo et al. 2012), while an analysis in 2003 found frequency of physician contact unassociated with patient survival (Plantinga, Fink et al. 2004). These conflicting results likely come from heterogeneity in the populations studied along with their unique confounders – each population studied may have a unique set of unobserved characteristics associated with both the number of provider visits and patient outcomes, preventing definitive conclusions on whether more visits produce better outcomes.
When CMS changed reimbursement to providers in 2004 to promote more frequent face-to-face provider visits, the policy created a natural experiment testing the causal connection between visit frequency and patient outcomes. Mentari et al. (2005) were the first to study the G-code phenomenon in their survey of 12 hemodialysis facilities and found that, although average visits per month increased from 1.52 to 3.14 following enactment of G-codes, there was no demonstrable improvement in patient outcomes (Mentari, DeOreo et al. 2005). Our study confirms these findings at a national level in several analyses with much greater statistical power and generalizability. Relative benefits were not observed in patients most affected by the G-code economic incentive.
There a several possible explanations for why the incentive to see patients more frequently did not improve mortality or kidney transplant listing. First, providers may have already been seeing patients at an appropriate frequency, such that the additional visits resulting from the policy provided no added value. Second, in an effort to see all patients four times per month, providers may have reduced the attention and time given at each visit. This would have been particularly detrimental to the sickest patients who otherwise would have been accorded the most attention.
There are two notable limitations to this study. First, because we did not have information on the actual number of visits rendered prior to G-code reimbursement, we were unable to test for possible nonlinear relationships between visit frequency and patient outcomes. For example, the difference in mortality and transplant listing between one and two visits per month may be more important than the difference between three and four visits per month. Second, we only examined the effect of G-code reimbursement on patient mortality and kidney transplant listing and did not study other important clinical outcomes (and their associated costs) including rates of infection, hospitalization, health-related quality of life, patient satisfaction and healthcare utilization.
With Medicare costs rapidly rising, it is increasingly important that scarce health care resources are directed towards improving health in cost-effective ways. While some believe that encouraging increased frequency of visits has improved patient-provider relationships, others argue that healthcare providers should determine frequency of patient visits based on patient acuity and need (Larson 2007; Mueller 2007). This study suggests that the incentive for more frequent provider visits did not reduce patient mortality or improve listing for kidney transplants, and may have even attenuated the improvements in survival rates experienced by all patients receiving hemodialysis. To the extent that G-code reimbursement shifted provider incentives and redirected healthcare resources toward more frequent visits to all patients irrespective of “need” and did not improve health outcomes, the associated increase in healthcare utilization and temporary cost increase was wasteful at best, and potentially harmful at worst.
Our conclusions are consistent with findings from the Dartmouth Atlas project in other areas of healthcare delivery demonstrating that more health care does not necessarily lead to improved patient health outcomes. They highlight the importance of critical evaluation of the downstream effects that changes in economic incentives have on health care utilization and patients’ wellbeing. They suggest that efforts to align economic incentives may not always have the intended consequences on health outcomes. This is particularly important as the nation reforms its health care system and the ESRD program.
Supplementary Material
References
- Social Security Amendments of 1972. 1972 [Google Scholar]
- Austin PC. Balance diagnostics for comparing the distribution of baseline covariates between treatment groups in propensity-score matched samples. Statistics in Medicine. 2009;28(25):3083–3107. doi: 10.1002/sim.3697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baicker K, Chandra A. Medicare spending, the physician workforce, and beneficiaries' quality of care. Health Affairs. 2004 doi: 10.1377/hlthaff.w4.184. Suppl Web Exclusives: W4-184–197. [DOI] [PubMed] [Google Scholar]
- BLS. Consumer Price Index. Bureau of Labor Statistics; United States Department of Labor. 2011 [Google Scholar]
- Centers for, M. and H. H. S. Medicaid Services. Medicare program; revisions to payment policies under the physician fee schedule for calendar year 2004. Final rule with comment period. Federal Register. 2003;68(216):63195–63395. [PubMed] [Google Scholar]
- CMS. Medicare Program; Revisions to Payement Policies Under the Physician Fee Schedule for Calendar Year 2004; Proposed Rule. Centers for Medicare & Medicaid Services; Department of Health and Human Services. 2003;68:20–22. [Google Scholar]
- Cooper RA. States with more physicians have better-quality health care. Health Affairs. 2009;28(1):w91–w102. doi: 10.1377/hlthaff.28.1.w91. [DOI] [PubMed] [Google Scholar]
- Erickson KF, Tan KB, Winkelmayer WC, Chertow GM, Bhattacharya J. Variation in Nephrologist Visits to Patients on Hemodialysis across Dialysis Facilities and Geographic Locations. Clinical Journal of The American Society of Nephrology: CJASN. 2013;8(6):987–994. doi: 10.2215/CJN.10171012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fisher ES, Goodman D, et al. Health care spending, quality, and outcomes. Hannover, NH: The Dartmouth Institute for Health Policy and Clinical Practice; 2009. [PubMed] [Google Scholar]
- Fisher ES, Wennberg DE, et al. The implications of regional variations in Medicare spending. Part 1: the content, quality, and accessibility of care. Annals of Internal Medicine. 2003;138(4):273–287. doi: 10.7326/0003-4819-138-4-200302180-00006. [Summary for patients in Ann Intern Med. 2003 Feb 18;138(4):I36; PMID: 12585853]. [DOI] [PubMed] [Google Scholar]
- Fisher ES, Wennberg DE, et al. The implications of regional variations in Medicare spending. Part 2: health outcomes and satisfaction with care. Annals of Internal Medicine. 2003;138(4):288–298. doi: 10.7326/0003-4819-138-4-200302180-00007. [Summary for patients in Ann Intern Med. 2003 Feb 18;138(4):I49; PMID: 12585852]. [DOI] [PubMed] [Google Scholar]
- Garber AM, Skinner J. Is American health care uniquely inefficient? Journal of Economic Perspectives. 2008;22(4):27–50. doi: 10.1257/jep.22.4.27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grossman M. The demand for health: A theoretical and empirical investigation. New york: Columbia University Press; 1972. [Google Scholar]
- Hadley J, Reschovsky JD. Medicare fees and physicians' medicare service volume: beneficiaries treated and services per beneficiary. International Journal of Health Care Finance & Economics. 2006;6(2):131–150. doi: 10.1007/s10754-006-8143-z. [DOI] [PubMed] [Google Scholar]
- Hadley J, Reschovsky JD. Medicare spending, mortality rates, and quality of care. International Journal of Health Care Finance & Economics. 2012;12(1):87–105. doi: 10.1007/s10754-012-9107-0. [DOI] [PubMed] [Google Scholar]
- Huber PJ. The Behavior of Maximum Likelihood Estimates under Nonstandard Conditions. Proceedings of the Fifth Berkeley Symposium on Mathematical Statistics and Probability. 1967;1:221–233. [Google Scholar]
- Iglehart JK. Bundled payment for ESRD--including ESAs in Medicare's dialysis package. New England Journal of Medicine. 2011;364(7):593–595. doi: 10.1056/NEJMp1014187. [Reprint in Minn Med. 2011 May;94(5):38–9; PMID: 21707012]. [DOI] [PubMed] [Google Scholar]
- Larson K. Has the CMS rule of "4 visits per month" influenced patient outcomes? Nephrology healthcare providers should determine the frequency of patient visits. Nephrology Nursing Journal: Journal of the American Nephrology Nurses' Association. 2007;34(3):343–344. [PubMed] [Google Scholar]
- McClellan WM, Soucie JM, et al. Mortality in end-stage renal disease is associated with facility-to-facility differences in adequacy of hemodialysis. Journal of the American Society of Nephrology. 1998;9(10):1940–1947. doi: 10.1681/ASN.V9101940. [DOI] [PubMed] [Google Scholar]
- Mentari EK, DeOreo PB, et al. Changes in Medicare reimbursement and patient-nephrologist visits, quality of care, and health-related quality of life. American Journal of Kidney Diseases. 2005;46(4):621–627. doi: 10.1053/j.ajkd.2005.06.012. [DOI] [PubMed] [Google Scholar]
- Mueller J. Has the CMS rule of "4 visits per month" influenced patient outcomes? Increased frequency of visits has promoted improved patient/provider relationships. Nephrology Nursing Journal: Journal of the American Nephrology Nurses' Association. 2007;34(3):343–344. [PubMed] [Google Scholar]
- Plantinga LC, Fink NE, et al. Frequency of patient-physician contact and patient outcomes in hemodialysis care. Journal of the American Society of Nephrology. 2004;15(1):210–218. doi: 10.1097/01.asn.0000106101.48237.9d. [DOI] [PubMed] [Google Scholar]
- Plantinga LC, Jaar BG, et al. Frequency of patient-physician contact in chronic kidney disease care and achievement of clinical performance targets. International Journal for Quality in Health Care. 2005;17(2):115–121. doi: 10.1093/intqhc/mzi010. [DOI] [PubMed] [Google Scholar]
- Rich MW, Beckham V, et al. A multidisciplinary intervention to prevent the readmission of elderly patients with congestive heart failure. New England Journal of Medicine. 1995;333(18):1190–1195. doi: 10.1056/NEJM199511023331806. [DOI] [PubMed] [Google Scholar]
- Sharma G, Kuo Y-F, et al. Outpatient follow-up visit and 30-day emergency department visit and readmission in patients hospitalized for chronic obstructive pulmonary disease. Archives of Internal Medicine. 2010;170(18):1664–1670. doi: 10.1001/archinternmed.2010.345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slinin Y, Guo H, et al. Association of Provider-Patient Visit Frequency and Patient Outcomes on Hemodialysis. Jounal of American Society of Nephrology. 2012;23 doi: 10.1681/ASN.2012010051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swaminathan S, Mor V, et al. Medicare's payment strategy for end-stage renal disease now embraces bundled payment and pay-for-performance to cut costs. Health Affairs. 2012;31(9):2051–2058. doi: 10.1377/hlthaff.2012.0368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Upchurch LC. Changes to the nephrology monthly capitation payments in the USA. Peritoneal Dialysis International. 2004;24(6):521–525. [PubMed] [Google Scholar]
- USRDS. United States Renal Data System. Bethesda, MD: National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases; 2013. Annual Data Report: Atlas of Chronic Kidney Disease and End-Stage Renal Disease in the United States. [Google Scholar]
- WWAMI. Rural-Urban Commuting Area Codes (RUCA), WWAMI Rural Health Research Center. 2005 [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.