Abstract
Introduction:
Scaphoid fracture is the most common fracture among the bones of the wrist. Plain radiography has a sensitivity of 59 to 79 percent for the diagnosis of scaphoid fracture after injury. Casting is done to avoid complications in patients with suspected fractures with normal radiography. Magnetic resonance imaging (MRI) has a sensitivity of 100% and a specificity of 99%. To avoid unnecessary casting and high costs, we decided to offer a way more efficient than radiography and less costly than MRI.
Material and Methods:
In the present study, 175 patients with suspected scaphoid fracture along with snuff box tenderness and normal radiography were enrolled in the study. On arrival, patients’ pain score were determined using visual analog scale method with anatomical snuffbox tenderness and then MRI was performed on the patients’ wrist and the results were recorded for patient in the check list. The data was then aggregated and analyzed.
Results:
The result of MRI for fracture was negative for 90.9% and positive for 9.1%. The mean pain score was 7.3 in negative MRI group and 8.75 in positive MRI group, considering a significant difference. ROC curve graph showed that the sensitivity and specificity will be 87% and 57%, respectively for scores 7.5 and higher and 75% and 72%, respectively for scores 8.5 and higher.
Conclusion:
It seems that although this method, beside other criteria in the diagnosis of fractures, can be useful in future studies, it would not be helpful in fracture detection.
Keywords: Scaphoid bone fractures, Pain measurement, MRI, Surgery, Diagnosis
1. INTRODUCTION
Scaphoid fracture is the most common fracture among the bones of the wrist (1-11), so that it includes 62 to 87 percent of wrist fractures. This fracture occurs in young adults between 15 and 30 years old and is rare in patients with immature skeletal system, because wrist is completely cartilaginous at birth and its structure remains nearly completely cartilaginous until late childhood and adolescence (7). The most common reason for the fracture is to fall onto an outstretched hand, while the wrist has dorsiflexion or a direct axial pressure is applied in line with thumb metacarpal (2, 7).
According to the fracture site, scaphoid fractures can be divided into three groups: Tuberosity and Distal Pole Fractures, Wrist Fractures and Proximal Pole Fractures. The most common type is wrist fracture that includes 70 to 80% of scaphoid fractures (7). The important point about scaphoid bone is it that it has retrograde blood supply. Among the effects of this type of fracture, avascular necrosis of scaphoid bone and nonunion of the proximal part of the scaphoid are more common (1, 3, 6, 7, 9, 12). Totally, avascular necrosis occurs in 13 to 40% of cases and scaphoid fracture nonunion in 5 to 12% (7). Taking notes as trauma after falling over, with weight pressure on the wrist in the state of wrist dorsiflexion, can be helpful in diagnosis (2, 7). While examining the anatomical snuffbox tenderness, there is a tenderness that is the classic diagnostic finding for this fracture.
Additionally, inflation and filling anatomical snuffbox may also exist. In any case, however, the physical examinations possess high sensitivity in the detection of this fracture, its specificity is relatively low (74 to 80%) (7). Radiographic evaluation of scaphoid fractures includes standard radiography and special scaphoid view (2). This fracture is difficult to be detected with standard radiography and radiography with special scaphoid views should be requested (7). Lucentness of fracture site may be hidden and there may only be some changes, such as fading or moving the scaphoid distal fat. Additionally, this type of fracture is likely not to be detected in the early post-injury radiographs (2, 7).
Numerous studies have reported the sensitivity of plain radiography after injury 59 to 79% (13, 14). According to current issues, immobilization with casting is usually done for a disease with clinically suspected fracture, even if there is no visible sign on radiography. Results from several studies have shown that only 5 to 10 percent of patients with suspected fractures with negative radiography have been reported real fractures after casting and further radiography, causing unnecessary downtimes and medical expenses (casting and re-graphs) imposed to the patient (15, 19). Currently, we have a gold standard for definitive diagnosis of scaphoid fractures with the normal radiography of MRI with a sensitivity of 91% to 99% (average 96%) and a specificity of 96% to 100% (average 99%) (7, 19).
Although MRI has an acceptable sensitivity and specificity to detect a hidden scaphoid fracture with normal radiography, given the high cost of the procedure, the need for lower-cost alternatives for the early detection of this type of fracture is felt. We decided to offer a way more efficient than radiography and less costly than MRI to avoid unnecessary casting and high costs.
2. MATERIALS AND METHODS
Patients diagnosed with suspected scaphoid fracture entered the study based on the findings from the history and physical examination, on arrival to the Emergency Department of Imam Reza (AS) and Hashemi Nejad Hospitals between 2011 – 2012 and with no radiographic signs of fracture, in accordance with the inclusion and exclusion criteria and patient’s satisfaction and sampling was conducted to 175 people. On arrival, patients’ pain score was determined using visual analog scale method with anatomical snuffbox tenderness in the emergency department by two fixed persons (an emergency medicine residents and an Academic Emergency Medicine) and thus recorded in a checklist relevant to patient. It is one of the most common methods of pain assessment in which a 10 cm ruler is used that one side indicates the absence of pain and the other expresses the worst imaginable pain and the patient him/herself specifies the amount of pain by identifying a point of the spectrum and patient’s pain score is characterized based on its distance from the beginning of the ruler. In the following, demographic characteristics of patients were taken and recorded in the checklist. Then, MRI was taken from patient’s wrist without receiving any money and its result was recorded in the checklist. After completion of the study, information on patients was obtained from checklists and given to statistical expertise. Data was analyzed by SPSS software, so that the proper pain cut-off scores to be determined in recognition of this fracture by plotting ROC-curve graph. Inclusion and exclusion criteria are listed in Table 1.
Table 1.
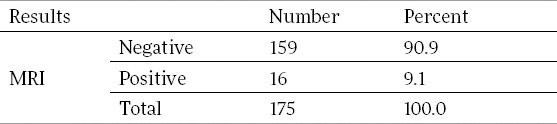
The result of MRI for studied patients in terms of fracture
3. RESULTS
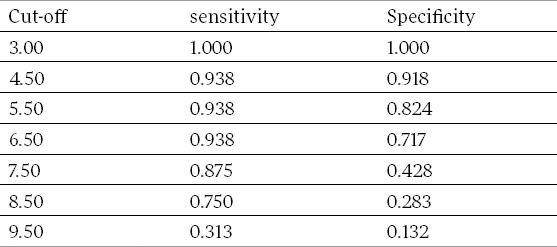
In this study, 175 patients were enrolled based on inclusion and exclusion criteria, including 163 males (93.1%) and 12 females (6.9%). The results of MRI for fractures were negative in 159 patients (90.9%) and positive in 16 patients (9.1%) (Table 1). T-test was done in both groups of patients with negative and positive MRI for the variables of sex and occupation of patients and no significant relationship was observed in any of the variables. In examining t-test results by SPSS software, the mean pain score in negative and positive MIR groups was 7.3 with SD: 1.75 and 8.75 with SD: 1.52, respectively, that was considered significant with P-value: 0.002 and 95%confidence interval. The comparison of age and pain score for both groups are shown in Table 2. ROC-Curve chart was plotted to determine the pain cut-off scores with the best sensitivity and specificity for the diagnosis of scaphoid fractures (Figure 1) and sensitivity and specificity were determined for each point in Table 3. All fractures are diagnosed in pain score 3 (sensitivity 100%), but the false positive rate has increased and specificity reaches zero. The higher the cut-off point, the lower the sensitivity and the more the specificity. The sensitivity and specificity will be 94% and only 8% for scores 4.5 and higher, 94% and 18% for score 5.5 and higher and 94% and 38 for scores 6.5 and higher, respectively. While the sensitivity decreases down to 87% and the specificity increases up to 57% for score 7.5 and the sensitivity and specificity will be 75% and 72% for scores 8.5 and higher, respectively and finally, the sensitivity and specificity will be 31% and 87% for scores 9.5 and higher, respectively.
Table 2.
The comparison of the amount of patients’ age and pain score in both groups
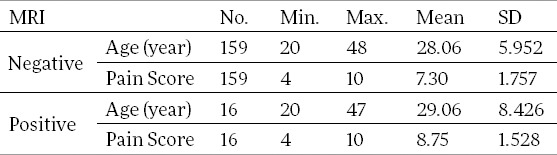
Figure 1.
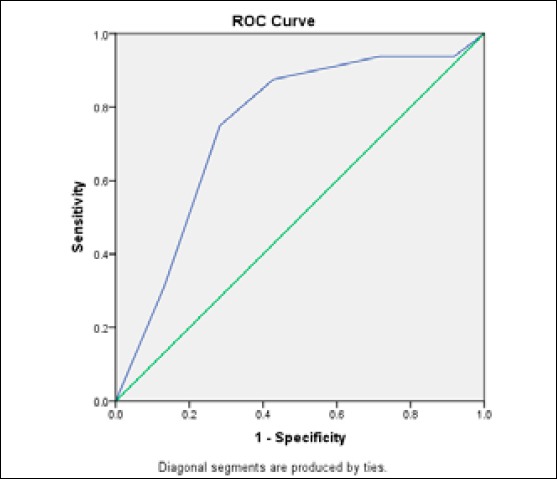
Roc-curve is shown that the sensitivity and specificity will be 87% and 57% for scores 7.5 and higher and 75% and 72% for scores 8.5 and higher, respectively.
Table 3.
The comparison of sensitivity and specificity for different scores as cut-off
4. DISCUSSION
As already mentioned, it is difficult to diagnose the scaphoid fractures with plain radiographs and different studies have cited the sensitivity of plain radiography after injury 59 to 79 percent which is relatively low (13,19,20). MRI is a gold standard for the diagnosis of this type of fracture, but its cost is relatively high (19, 21, 22, 23, 24, 25). Therefore, it is felt the need for other ways with less cost and in order to eliminate additional costs, such as immobilization, referring to the clinic, delayed radiographic examinations, patients’ downtime after casting. The study is aimed to employ a method with time and cost less than MRI, but sensitivity and specificity more acceptable than plain radiography to evaluate patients with suspected fracture with normal radiographs. Accordingly, pain score was defined using Visual Analog Scale and its diagnostic value for the diagnosis of scaphoid fractures was assessed. This method and the same ways have been used in other studies. In 1998, a study was conducted in Canada by MacDermid JC et al in which 64 patients with distal radius fractures and 35 patients with scaphoid fractures participated in reliability survey and 101 patients with distal radius fractures in validity survey to determine the amount of wrist pain and disability. In this study, Patient-Rated Wrist Evaluation (PRWE) questionnaire consisted of 15 items was used to assess the reliability (two times (test-retest)) and the validity (four times at the beginning, 2, 3 and 6 months after the fracture) with doing SF-36 and traditional impairment measures.
The results consider this approach reliable and valid for the study of the amount of pain and disability (with acceptable reliability and validity) (26). According to another study conducted by Ghislain Geurts and his colleagues in Belgium, pain scoring was used to identify the incidence of scaphotrapezial joint arthritis as one of the contributing factors, in an average 6.1 year follow-up of 34 patients with scaphoid fractures without displacement (minimum 307 years), in which the method of assessing pain was visual analog scale. Patients were operated by percutaneous screw fixation with bone (27). Smith JE and his coworkers conducted another study on patients with wrist injury and suspected fracture with a normal CT scan after two weeks of injury in Australia in 2011. Patients were followed up at 3, 6 and 12 months after injury using the Patient Rated Wrist Evaluation questionnaire in where a scale of 0 to 10 was considered for pain and function (28).
5. CONCLUSIONS
Based on statistical analysis in this study, pain score of patients with suspected scaphoid fracture based on symptoms and with normal radiograph of the wrist would not be a good way to help identify. However, this technique can be used combined with other criteria in the diagnosis of fractures in future studies.
Footnotes
CONFLICT OF INTEREST: NONE DECLARED.
REFERENCES
- 1.Bond CD, Shin AY, McBride MT, Dao KD. Percutaneous screw fixation or cast immobilization for nondisplaced scaphoid fractures. The Journal of Bone & Joint Surgery. 2001;83(4):483. doi: 10.2106/00004623-200104000-00001. [DOI] [PubMed] [Google Scholar]
- 2.Brian E. Tintinalli’s Emergency Medicine. 7th ed. New York: McGraw-Hill; 2011. Anorectal disorders; pp. 597–598. [Google Scholar]
- 3.Dias J, Wildin C, Bhowal B, Thompson J. Should acute scaphoid fractures be fixed? A randomized controlled trial. The Journal of Bone & Joint Surgery. 2005;87(10):2160–2168. doi: 10.2106/JBJS.D.02305. [DOI] [PubMed] [Google Scholar]
- 4.Dodds SD, Patterson JT, Halim A. Volar Plate Fixation of Recalcitrant Scaphoid Nonunions With Volar Carpal Artery Vascularized Bone Graft. Techniques in hand & upper extremity surgery. 2014;18(1):2–7. doi: 10.1097/BTH.0000000000000028. [DOI] [PubMed] [Google Scholar]
- 5.Garcia RM, Ruch DS. Management of Scaphoid Fractures in the Athlete: Open and Percutaneous Fixation. Sports medicine and arthroscopy review. 2014;22(1):22–28. doi: 10.1097/JSA.0000000000000008. [DOI] [PubMed] [Google Scholar]
- 6.Haddad F, Goddard N. Acute percutaneous scaphoid fixation A pilot study. Journal of Bone & Joint Surgery, British Volume. 1998;80(1):95–59. doi: 10.1302/0301-620x.80b1.8076. [DOI] [PubMed] [Google Scholar]
- 7.Marx J, Hockberger R, Walls R. Rosen’s Emergency Medicine-Concepts and Clinical Practice: Elsevier Health Sciences. 2013 [Google Scholar]
- 8.Meermans G, Van Glabbeek F, Braem MJ, van Riet RP, Hubens G, Verstreken F. Comparison of Two Percutaneous Volar Approaches for Screw Fixation of Scaphoid Waist Fractures. The Journal of Bone & Joint Surgery. 2014;96(16):1369–1376. doi: 10.2106/JBJS.L.01729. [DOI] [PubMed] [Google Scholar]
- 9.ng H, Tan G, Chew W. Treatment of scaphoid non-union with 1, 2 intercompartmental supraretinacular artery (1, 2 ICSRA) vascularised graft. Singapore Medical Journal. 2011;52(9):658–661. [PubMed] [Google Scholar]
- 10.Saint-Cyr M, Oni G, Wong C, Sen MK, LaJoie AS, Gupta A. Dorsal percutaneous cannulated screw fixation for delayed union and nonunion of the scaphoid. Plastic and reconstructive surgery. 2011;128(2):467–473. doi: 10.1097/PRS.0b013e31821e703b. [DOI] [PubMed] [Google Scholar]
- 11.Taha AMS. Operative Dictations in Orthopedic Surgery. Springer; 2013. Treatment of Scaphoid Nonunion; pp. 327–329. [Google Scholar]
- 12.Chang MA, Bishop AT, Moran SL, Shin AY. The outcomes and complications of 1, 2-intercompartmental supraretinacular artery pedicled vascularized bone grafting of scaphoid nonunions. The Journal of hand surgery. 2006;31(3):387–396. doi: 10.1016/j.jhsa.2005.10.019. [DOI] [PubMed] [Google Scholar]
- 13.Blum A, Sauer B, Detreille R, Zabel J, Pierrucci F, Witte Y, et al. The diagnosis of recent scaphoid fractures: review of the literature. Journal de radiologie. 2007;88(5 Pt 2):741–759. doi: 10.1016/s0221-0363(07)91342-6. [DOI] [PubMed] [Google Scholar]
- 14.Waitayawinyu T, McCallister WV, Katolik LI, Schlenker JD, Trumble TE. Outcome after vascularized bone grafting of scaphoid nonunions with avascular necrosis. The Journal of hand surgery. 2009;34(3):387–394. doi: 10.1016/j.jhsa.2008.11.023. [DOI] [PubMed] [Google Scholar]
- 15.Leung F, Tak-Wingq L. Plate (LCP) Fixation. Mastering Orthopedic Techniques: Intra-articular Fractures. 2013:161. [Google Scholar]
- 16.Lewallen D, Chao E, Kasman R, Kelly P. Comparison of the effects of compression plates and external fixators on early bone-healing. The Journal of Bone & Joint Surgery. 1984;66(7):1084–1091. [PubMed] [Google Scholar]
- 17.Miramini S, Zhang L, Richardson M, Pirpiris M, Mendis P, Oloyede K, et al. Computational simulation of the early stage of bone healing under different configurations of locking compression plates. Computer methods in biomechanics and biomedical engineering. 2013:1–14. doi: 10.1080/10255842.2013.855729. ahead-of-print. [DOI] [PubMed] [Google Scholar]
- 18.Schmal H, Strohm PC, Jaeger M, Südkamp NP. Flexible fixation and fracture healing: do locked plating ‘internal fixators’ resemble external fixators? Journal of orthopaedic trauma. 2011;25:S15–S20. doi: 10.1097/BOT.0b013e31820711d3. [DOI] [PubMed] [Google Scholar]
- 19.Yin ZG, Zhang JB, Kan SL, Wang XG. Diagnosing suspected scaphoid fractures: a systematic review and meta-analysis. Clinical Orthopaedics and Related Research. 2010;468(3):723–734. doi: 10.1007/s11999-009-1081-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Baldassarre RL, Hughes TH. Investigating suspected scaphoid fracture. BMJ. 2013;346 doi: 10.1136/bmj.f1370. [DOI] [PubMed] [Google Scholar]
- 21.Chou YC, Hsu YH, Cheng CY, Wu CC. Percutaneous screw and axial Kirschner wire fixation for acute transscaphoid perilunate fracture dislocation. The Journal of hand surgery. 2012;37(4):715–720. doi: 10.1016/j.jhsa.2012.01.019. [DOI] [PubMed] [Google Scholar]
- 22.Divecha HM, Clarke JV, Barnes SJ. Established non-union of an operatively managed trans-scaphoid perilunate fracture dislocation progressing to spontaneous union. Journal of Orthopaedics and Traumatology. 2011;12(3):159–162. doi: 10.1007/s10195-011-0143-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Forli A, Courvoisier A, Wimsey S, Corcella D, Moutet F. Perilunate dislocations and transscaphoid perilunate fracture - dislocations: a retrospective study with minimum ten-year follow-up. The Journal of hand surgery. 2010;35(1):62–68. doi: 10.1016/j.jhsa.2009.09.003. [DOI] [PubMed] [Google Scholar]
- 24.Komurcu M, Kürklü M, Ozturan KE, Mahirogullari M, Basbozkurt M. Early and delayed treatment of dorsal transscaphoid perilunate fracture-dislocations. Journal of orthopaedic trauma. 2008;22(8):535–540. doi: 10.1097/BOT.0b013e318183eb23. [DOI] [PubMed] [Google Scholar]
- 25.Yildirim C, Unuvar F, Keklikci K, Demirtas M. Bilateral dorsal trans-scaphoid perilunate fracture - dislocation: A case report. International journal of surgery case reports. 2014;5(5):226–230. doi: 10.1016/j.ijscr.2014.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.MacDermid JC, Turgeon T, Richards RS, Beadle M, Roth JH. Patient rating of wrist pain and disability: a reliable and valid measurement tool. Journal of orthopaedic trauma. 1998;12(8):577–586. doi: 10.1097/00005131-199811000-00009. [DOI] [PubMed] [Google Scholar]
- 27.Geurts G, van Riet R, Meermans G, Verstreken F. Incidence of scaphotrapezial arthritis following volar percutaneous fixation of nondisplaced scaphoid waist fractures using a transtrapezial approach. The Journal of hand surgery. 2011;36(11):1753–1758. doi: 10.1016/j.jhsa.2011.08.031. [DOI] [PubMed] [Google Scholar]
- 28.Smith JE, Rickard A, Gay D, Middleton PM. Outcome of wrist injuries with clinical suspicion of scaphoid injury after normal computed tomography. European Journal of Emergency Medicine. 2012;19(3):188–192. doi: 10.1097/MEJ.0b013e32834ad9f9. [DOI] [PubMed] [Google Scholar]


